Abstract
Objectives
A high body mass index (BMI) is associated with risk of type 2 diabetes mellitus (DM). The United Arab Emirates (UAE) is experiencing a marked increase in obesity. Nonetheless, no data are available regarding the incidence of type 2 DM in the high-risk adult UAE population. Therefore, this study aimed to evaluate the incidence rate and risk of developing type 2 DM among individuals with above-normal BMI in the UAE.
Design
A retrospective cohort study.
Setting
Outpatient clinics at a tertiary care centre in Al Ain, UAE.
Participants
Three hundred and sixty-two overweight or obese adult UAE nationals who visited outpatient clinics between April 2008 and December 2008.
Primary outcome measure
Patients with type 2 DM were identified based on diagnosis established by a physician or through glycated haemoglobin (HbA1c) levels ≥6.5% during the follow-up period (until April 2018).
Results
The overall incidence rate of type 2 DM during the median follow-up time of 8.7 years was 16.3 (95% CI 12.1 to 21.4) cases per 1000 person-years. Incidence rates in men and women were 17.7 (95% CI 11.6 to 25.9) and 15.0 (95% CI 9.8 to 22.2) cases per 1000 person-years, respectively. Multivariable Cox proportional hazard analysis determined older age and obesity in women and pre-diabetes in men to be independent risk factors for developing type 2 DM.
Conclusions
The incidence rate of type 2 DM in overweight and obese UAE nationals is high. In addition to screening, current strategies should strongly emphasise lifestyle modifications to decrease HbA1c and BMI levels in this high-risk population.
Keywords: diabetes & endocrinology, epidemiology, internal medicine
Strengths and limitations of this study.
This long-term longitudinal cohort study determines the incidence rate and risk factors of type 2 diabetes mellitus in overweight and obese United Arab Emirates (UAE) nationals.
Anthropometric and laboratory data were obtained instead of self-reported information for the classification of risk factors and identification of incident cases.
The study’s subjects were recruited from a single large public hospital’s ambulatory clinics; therefore, our findings may not apply to the general UAE population.
No data were available for review regarding additional confounders, such as family history and changes in weight and physical activity.
Introduction
A rapid worldwide increase has been observed regarding the prevalence of type 2 diabetes mellitus (DM) and obesity. The United Arab Emirates (UAE) is one of the epicentres of this epidemic. In a 2007 study, the age-standardised rates for pre-diabetes and type 2 DM among UAE nationals were 24.2% and 29%, respectively.1 However, in a 2019 study of young Emirati men, the age-adjusted prevalence of pre-diabetes was much higher at 41.3%.2 By contrast, the prevalence of type 2 DM in North America and Western European countries is well below 12%.3–6 Notably, the number of people with type 2 DM in the UAE is estimated to reach over two million by 2040.7
Overweight, defined as body mass index (BMI) between 25 and 29.99 kg/m2, and obesity, defined as BMI ≥30 kg/m2,8 are known risk factors of type 2 DM.9 More recently, the age-adjusted prevalence of overweight and obesity among Emirati men between the ages of 18 and 30 years was noted to be 27% and 30%, respectively.2 In contrast, the corresponding prevalence in another study was 23% and 10% among young Emirati women.10 Both these studies determined increased BMI to be strongly associated with diabetes.
Both obesity and type 2 DM are well-known cardiometabolic risk factors for vascular complications, such as coronary heart disease and peripheral vascular disease. The prevalence of these vascular diseases in the UAE is 10.5% and 11.1%, respectively.1 These and other vascular-related complications have resulted in the UAE having one of the highest reported global death rates for cardiovascular disease—204 per 100 000 for women and 309 per 100 000 for men.11
The rise in the incidence of diabetes and its complications among the UAE population has been in parallel to the economic surge, resulting in growing urbanisation and changing lifestyle habits in the country. Nevertheless, over the last decade, UAE has diverted its attention and endeavoured to curb the burden of overweight and obesity, as well as to decrease the incidence of associated conditions like diabetes. The Weqaya programme, a population-wide CVD screening programme, was initiated in 200812 to enable individuals and healthcare providers to implement CVD preventative measures. For continued assessment of the effectiveness of these local interventions, ad hoc analysis of population data at predefined intervals over a long period is required. However, epidemiological studies on type 2 DM in the UAE have primarily focused on its prevalence in the general population.1 2 13 Despite having information from the Weqaya programme, data regarding the incidence of type 2 DM among obese and overweight UAE nationals remain poorly researched. This lapse is primarily because of the significant resource investment required to conduct observational cohort studies with prolonged follow-up.
Therefore, in this long-term, longitudinal retrospective study, we aimed to calculate the incidence rate of type 2 DM and elucidate the effects of BMI on DM risk in adult UAE nationals who are overweight and obese.
Methods
Study setting
A retrospective electronic medical record review was performed of adult patients who presented to outpatient clinics at Tawam Hospital in Al Ain, UAE, between 1 April 2008 and 31 December 2008. Tawam Hospital is one of the two large government hospitals in the city of Al Ain and serves an estimated 60 000 adult UAE nationals in the city who are overweight and obese.14 15
Subjects and procedures
The study population consisted of UAE nationals who were overweight and obese, aged between 18 and 75 years, who were seen at the outpatient departments at Tawam Hospital. The inclusion criteria were patients without type 2 DM, defined as having glycated haemoglobin (HbA1c) <6.5%; patients not taking antidiabetic medications; and those with BMI ≥25 kg/m2 at baseline. The exclusion criteria were patients with missing HbA1c data, those with a history of chronic medical conditions, such as malignancy, HIV infection, receiving steroids or immunosuppression medications, or stage 3–5 chronic kidney disease (estimated glomerular filtration rate of ≤59 mL/min/1.73 m2).16 Moreover, patients who had undergone weight reduction surgery, defined either as restrictive or malabsorptive bariatric surgery, or pharmacotherapy for weight loss were excluded from the study. The final study group consisted of 362 subjects with a BMI of ≥25 kg/m2 (figure 1).
Figure 1.
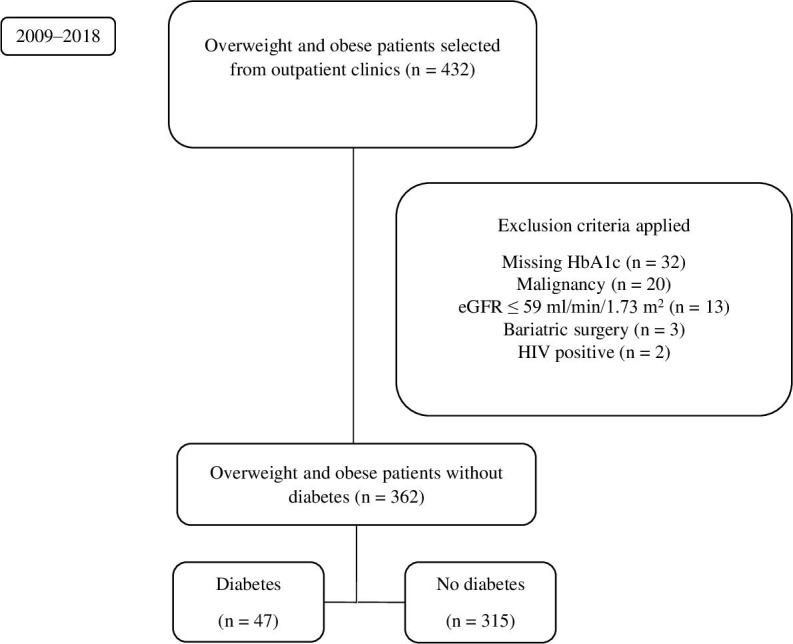
Flow chart for the inclusion and exclusion of patients. eGFR, estimated glomerular filtration rate; HbA1c, glycated haemoglobin.
Definitions and measurements
Initial BMI was calculated from baseline height and weight measurements using the formula weight (kg) divided by height squared (m2). Overweight and obesity were defined according to the WHO classification,8 based on a BMI between 25 and 29.99 kg/m2 and ≥30 kg/m2, respectively. Hypertension (HTN) was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg or use of blood pressure medications.17 The definition of dyslipidaemia was a serum total cholesterol (TC) of ≥6.21 mmol/L or if the patient had a documented prescription of lipid-lowering medications.18 Pre-diabetes was defined as having an HbA1c level between 5.7% and 6.4%.19 Current or history of smoking tobacco was considered a positive smoking history. Patients with a documented history of coronary heart disease, cerebrovascular disease or peripheral vascular disease were identified to have a vascular disease.
Outcomes
Our study endpoint was incident type 2 DM, defined as either HbA1c ≥6.5% (based on the definition of DM by the American Diabetes Association) or a diagnosis of type 2 DM established by a physician at any time during the follow-up period.19 The occurrence of incident type 2 DM was based on a review of all the electronic medical records until 30 April 2018. All laboratory analyses were performed at the Medical Laboratory Department of Tawam Hospital. An automated analyser, Integra 400 Plus (Roche Diagnostics, Mannheim, Germany), was used to measure HbA1c levels. The HbA1c results were reported as percentage using the International Federation of Clinical Chemistry-National Glycohemoglobin Standardization Program master equation.20
Statistical analyses
Using a formula from Rosner,21 a sample size of 353 was calculated. This was based on the anticipated incidence of diabetes of 17.3%22 and using 80% power at a two-sided significance level of 0.05. The sample size was further increased by 20% to account for patients lost to follow-up and those with missing data.
Intersex differences were determined using the Mann-Whitney U test or the independent-samples t-test for non-normal and normal data, respectively. For categorical variables, Fisher’s exact test (two-tailed) was used. Person-years at risk for incident type 2 DM was calculated for each patient as the time from the baseline visit to the diagnosis of type 2 DM or the most recent outpatient visit, whichever occurred first. The incidence rate of type 2 DM with a 95% CI was calculated per 1000 person-years by dividing the number of new cases of type 2 DM by the person-years at risk. Sex-specific incidence rates were calculated stratified by age and BMI categories. Kaplan-Meier time-to-event analysis was conducted with a log-rank test to compare age and BMI categories for incident type 2 DM.
Univariable and multivariable Cox proportional hazard models were evaluated to examine predictors of incident type 2 DM in the entire cohort and stratified by sex. The following predictor variables were examined using univariable Cox modelling: age (categorised as <44 years and ≥44 years), sex, vascular disease, HTN, dyslipidaemia, smoking, HbA1c (categorised as <5.7% and ≥5.7%) and BMI (categorised as overweight and obese). All covariables with p<0.1 were included in the final multivariable model. A stepwise method based on likelihood ratios, with entry and removal probabilities set at 0.05 and 0.10, respectively, was used to check the results. The log-log plot was used to evaluate the proportional hazards assumption and was not significant. P<0.05 was considered statistically significant. SPSS V.25 was used to analyse the data.
Patient and public involvement
There was no patient or public involvement in the design and conduct of the study.
Results
Characteristics of study participants
The baseline patient characteristics of the 362 subjects are presented in table 1. The ratio of men to women was almost 1:1. At baseline, the mean age was 44.4±14.5 years and the BMI was 31.7 kg/m2 (IQR 27.6–34.2 kg/m2). When stratified by sex, women were older, had higher BMI and TC values, and had a higher prevalence of dyslipidaemia at baseline. Conversely, men had significantly higher baseline systolic and diastolic blood pressure values, as well as a higher prevalence of smoking history.
Table 1.
Baseline characteristics of the study participants
| Total (N=362) Mean±SD |
Men (n=170) Mean±SD |
Women (n=192) Mean±SD |
P value† | |
| Women (%) | 53.0 | – | – | – |
| Age (years) | 44.4±14.5 | 40.2±14.7 | 48.1±13.2 | <0.001 |
| Anthropometric values | ||||
| BMI (kg/m2) | 31.7 (27.6–34.2) | 29.6 (27.3–32.8) | 31.2 (27.9–35.8) | 0.001 |
| SBP (mm Hg) | 127.9±17.3 | 129.9±17.9 | 126.2±16.7 | 0.040 |
| DBP (mm Hg) | 76.9±11.0 | 79.0±11.3 | 75.1±10.4 | 0.001 |
| Laboratory values | ||||
| HbA1c (%) | 5.6±0.5 | 5.6±0.5 | 5.6±0.5 | 0.326 |
| eGFR (mL/min/1.73 m2) | 105.9±16.8 (n=359)* | 104.2±18.5 (n=167)* | 107.4±15.1 | 0.073 |
| TC (mmol/L) | 5.1±0.9 | 4.9±1.0 | 5.2±1.0 | 0.002 |
| History of, n (%) | ||||
| HTN | 181 (50.0) | 91 (53.5) | 90 (46.9) | 0.247 |
| Dyslipidaemia | 141 (39.0) | 52 (30.6) | 89 (46.4) | 0.002 |
| Vascular disease | 18 (5.0) | 10 (5.9) | 8 (4.2) | 0.478 |
| Smoking | 56 (15.5) | 54 (31.8) | 2 (1.0) | <0.001 |
*The difference in n is due to missing data.
†Independent-samples t-test was used to calculate p values for continuous variables and Fisher’s exact test (two-tailed) for categorical variables.
BMI, body mass index; DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; HbA1c, glycated haemoglobin; HTN, hypertension; SBP, systolic blood pressure; TC, total cholesterol.
Incidence
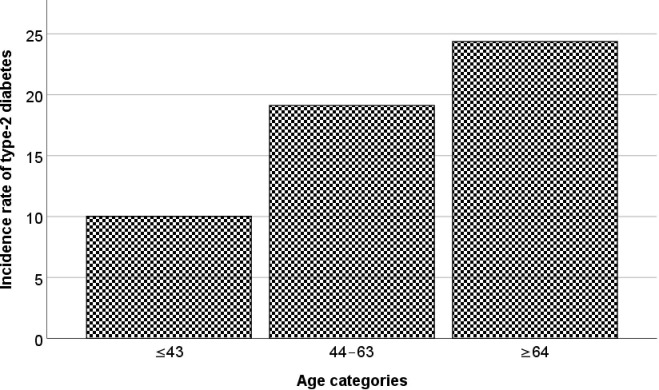
After a median follow-up time of 8.7 years (IQR, 8.2–9.0 years), 47 incident cases of type 2 DM were identified. The overall incidence rate of type 2 DM was 16.3 (95% CI 12.1 to 21.4) cases per 1000 person-years, and the crude incidence over the same period was 13.0% (95% CI 9.8 to 16.8%). The incidence rate of type 2 DM increased with patient age (figure 2). When stratified by sex, the incidence rates were 17.7 (95% CI 11.6 to 25.9) and 15.0 (95% CI 9.8 to 22.2) cases per 1000 person-years in men and women, respectively.
Figure 2.
Overall incidence rate of type 2 diabetes mellitus (cases/1000 person-years) by increasing age.
Sex-specific incidence rates, as stratified by BMI, were higher in obese women (21.1, 95% CI 13.3 to 32.0 cases per 1000 person-years) compared with overweight women (5.1, 95% CI 1.3 to 14.0 cases per 1000 person-years) (p=0.013). Incidence rates for type 2 DM were higher in older women (21.3, 95% CI 13.5 to 31.9 cases per 1000 person-years) compared with younger women (3.7, 95% CI 0.6 to 12.2 cases per 1000 person-years) (p=0.008) (figure 3). However, these differences were not significant among men.
Figure 3.
Sex-specific incidence rate of type 2 diabetes mellitus (cases/1000 person-years) stratified by BMI categories (A) and by age (B). BMI, body mass index.
Analyses of risk factors
We used multivariable Cox regression analyses to examine the association of age, sex, vascular disease, dyslipidaemia, smoking, HTN, BMI and HbA1c levels with the risk of developing type 2 DM in the entire study cohort, as well as between men and women. When adjusted for all other variables, we observed that in men an HbA1c level ≥5.7% (HR=3.02, 95% CI 1.20 to 7.62) and in women age ≥44 years (HR=4.84, 95% CI 1.13 to 20.73) and obesity (HR=3.42, 95% CI 1.01 to 11.57) were significant risk factors for the development of type 2 DM (table 2).
Table 2.
Predictors of incident type 2 diabetes mellitus in the study population
| Predictor variables | Total (N=362) | Men (n=170) | Women (n=192) | |||
| HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | |
| Age | ||||||
| <44 years | Reference | Reference | Reference | |||
| ≥44 years | 1.20 (0.59 to 2.44) | 0.619 | 0.46 (0.17 to 1.13) | 0.135 | 4.84 (1.13 to 20.73) | 0.034 |
| Sex | ||||||
| Female | Reference | |||||
| Male | 1.60 (0.83 to 3.05) | 0.160 | ||||
| History of HTN | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 1.78 (0.94 to 3.37) | 0.075 | 1.89 (0.74 to 4.81) | 0.183 | 1.61 (0.67 to 3.88) | 0.292 |
| History of dyslipidaemia | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 1.32 (0.70 to 2.51) | 0.393 | 2.01 (0.80 to 5.04) | 0.135 | 0.80 (0.34 to 1.90) | 0.608 |
| History of smoking | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 0.58 (0.23 to 1.49) | 0.259 | 0.36 (0.12 to 1.04) | 0.060 | 4.88 (0.44 to 54.08) | 0.196 |
| History of vascular disease | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 1.57 (0.54 to 4.54) | 0.408 | 2.46 (0.65 to 9.27) | 0.183 | 0.60 (0.06 to 5.50) | 0.647 |
| HbA1c | ||||||
| <5.7% | Reference | Reference | Reference | |||
| ≥5.7% | 2.29 (1.16 to 4.52) | 0.016 | 3.02 (1.20 to 7.62) | 0.019 | 2.30 (0.83 to 6.39) | 0.109 |
| BMI | ||||||
| Overweight | Reference | Reference | Reference | |||
| Obese | 1.86 (0.99 to 3.50) | 0.053 | 1.17 (0.51 to 2.68) | 0.713 | 3.42 (1.01 to 11.57) | 0.048 |
BMI, body mass index; HbA1c, glycated haemoglobin; HTN, hypertension.
Discussion
The results of this study revealed that the crude incidence of type 2 DM among UAE nationals who are overweight and obese was 1.49% per year during the 9-year study period. The overall incidence rate was 16.3 per 1000 person-years. The independent predictors for the development of type 2 DM were age (≥44 years) and obesity in women and pre-diabetes in men.
Incidence rates
The incidence rates of type 2 DM in high-risk populations differ worldwide. This difference is probably due to variations in insulin sensitivity related to the interaction between genetic and environmental factors among different ethnic and population groups globally.23 In a US study of predominantly overweight and obese African–American women, the reported incidence rate of type 2 DM was 15.2 per 1000 person-years24 and is comparable with our study. There has been only one other study that has assessed the incidence rate of type 2 DM in the UAE.13 The study was conducted over 12 months in Ajman, one of the emirates in the UAE, and revealed that the incidence rate for type 2 DM was 4.8 per 1000 person-years. However, this study cannot be directly compared with our study because it was conducted on the general population, and our study cohort comprised only overweight and obese UAE nationals.
Risk factors
This study revealed some interesting findings regarding the risk factors for developing type 2 DM in the high-risk UAE population. Sex-specific incidence rates of type 2 DM exhibited a female preponderance, particularly older women. Nevertheless, these results were not unique and were also observed among the general population of the UAE.13 The higher incidence of type 2 DM among older women may be attributable to the high prevalence of overweight and obesity, sedentary lifestyle, nutritional habits and early menopause witnessed in our population.25–28
Furthermore, individuals with high-normal HbA1c levels have a greater risk of developing type 2 DM.29 However, when we stratified our cohort by sex, the independent predictive property of the HbA1c level was only observed in men. An explanation for this finding could be the high prevalence of smoking history in men, as smoking has been shown to increase HbA1c levels in individuals without diabetes.30 Moreover, obesity in women was noted to be an independent risk predictor for type 2 DM. Studies have demonstrated that the risk of developing type 2 DM is significantly higher in individuals with BMI ≥30 kg/m2 compared with those with normal BMI.9 Therefore, interventions that promote weight loss and reduce BMI can reduce the risk of developing type 2 DM. Notably, an 8-week exercise intervention programme in a UAE student population demonstrated a significant reduction in BMI.31 In addition, other controlled intervention studies in high-risk populations32 33 demonstrated a significant decrease in the risk of type 2 DM consequent to BMI reduction.
Clinical and public health implications
In the UAE, much of the increase in type 2 DM has occurred due to social and economic changes—from traditional, seminomadic lifestyle to sedentary, urban and high-income lifestyle. Consequently, the progression towards type 2 DM and cardiovascular disease starts early in the UAE due to the high prevalence of childhood obesity.1 34 A 2015 study of Emirati children and adolescents with a BMI ≥25 kg/m2 determined the prevalence of pre-diabetes and type 2 DM to be 5.4% and 0.87%, respectively.35 Therefore, reducing the burden of type 2 DM in the UAE will require intensive population-wide interventions to promote regular physical activity and a healthy diet,33 36 particularly among the Emirati youth.
Furthermore, the results of this study highlight the need to focus on Emirati women as a specific target group for obesity prevention programmes. These programmes should begin in childhood because 21% are obese by the time they are 30 years of age.26 In addition, it is imperative to have a multidisciplinary approach to address the high incidence of type 2 DM, where paediatricians, primary care providers, dietitians and specialists work collaboratively towards promoting weight reduction and maintaining a healthy BMI in our population.
Strengths and limitations
The strengths of this study include the long duration of follow-up for our representative sample of overweight and obese individuals in the second largest city in the Abu Dhabi Emirate of UAE. We used the anthropometric and laboratory data documented in patient charts instead of self-reported information and diagnostic codes for the classification of risk factors and identification of incident cases. In addition, HbA1c levels or physician diagnosis formed the basis to identify incident cases of type 2 DM instead of fasting plasma glucose, which has more variability.37 38
Nonetheless, this study had some limitations. Baseline data regarding family history of type 2 DM, history of gestational diabetes, physical activity and abdominal obesity were unavailable—all of which are well-researched risk factors for the development of DM. Nevertheless, a prospective study can provide more robust results. Furthermore, data on additional confounders, such as family history, changes in weight and physical activity, were unavailable for review. Finally, the subjects for this study were recruited from a single largest tertiary care hospital’s ambulatory clinics; thus, our findings may not apply to the general UAE population.
Conclusions
The overall incidence rate of type 2 DM in UAE nationals who are overweight and obese was 16.3 per 1000 person-years. Notably, pre-diabetes in men and obesity in women, particularly older women, were determined to be independent predictors for the development of incident type 2 DM. Hence, it is imperative to emphasise BMI reduction through lifestyle modifications in these high-risk groups.
Supplementary Material
Acknowledgments
The authors would like to thank Shehab Majud for his help on the language in this manuscript.
Footnotes
Contributors: DR conceived the study and its design, performed the literature search and drafted the initial manuscript. SA-S was involved in data management, statistical analysis, interpretation of data and critical review of the manuscript. RDG assisted in statistical analysis, contributed to the discussion, and reviewed and edited the manuscript. JA-K performed a critical review of the manuscript, was involved in data interpretation and also guided the research methodology. All authors read and approved the final manuscript.
Funding: This work was supported by the College of Medicine and Health Sciences, United Arab Emirates University (no 31M325). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The Research and Ethics Board of Tawam Hospital and the United Arab Emirates University granted ethical approval to this study (CRD239/13). Informed consent was waived because patient records and information were anonymised and deidentified before analysis.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: The data that support the findings of this study are available from the corresponding author, SA-S, upon reasonable request.
References
- 1.Saadi H, Carruthers SG, Nagelkerke N, et al. . Prevalence of diabetes mellitus and its complications in a population-based sample in Al Ain, United Arab Emirates. Diabetes Res Clin Pract 2007;78:369–77. 10.1016/j.diabres.2007.04.008 [DOI] [PubMed] [Google Scholar]
- 2.Alzaabi A, Al-Kaabi J, Al-Maskari F, et al. . Prevalence of diabetes and cardio-metabolic risk factors in young men in the United Arab Emirates: a cross-sectional national survey. Endocrinol Diabetes Metab 2019;2:e00081. 10.1002/edm2.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eschwege E, Basdevant A, Crine A, et al. . Type 2 diabetes mellitus in France in 2012: results from the ObEpi survey. Diabetes Metab 2015;41:55–61. 10.1016/j.diabet.2014.11.007 [DOI] [PubMed] [Google Scholar]
- 4.Caspard H, Jabbour S, Hammar N, et al. . Recent trends in the prevalence of type 2 diabetes and the association with abdominal obesity lead to growing health disparities in the USA: an analysis of the NHANES surveys from 1999 to 2014. Diabetes Obes Metab 2018;20:667–71. 10.1111/dom.13143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tamayo T, Brinks R, Hoyer A, et al. . The prevalence and incidence of diabetes in Germany. Dtsch Arztebl Int 2016;113:177–82. 10.3238/arztebl.2016.0177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greiver M, Williamson T, Barber D, et al. . Prevalence and epidemiology of diabetes in Canadian primary care practices: a report from the Canadian primary care sentinel surveillance network. Can J Diabetes 2014;38:179–85. 10.1016/j.jcjd.2014.02.030 [DOI] [PubMed] [Google Scholar]
- 7.Center ICLD UAE diabetes trends and numbers [Internet]. Available: http://www.icldc.ae/about-us/p/UAE-Diabetes-Trends [Accessed 19 Apr 2018].
- 8.World Health Organization (WHO) BMI classification [Internet], 2006. Available: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [Accessed 18 Apr 2018].
- 9.Ganz ML, Wintfeld N, Li Q, et al. . The association of body mass index with the risk of type 2 diabetes: a case-control study nested in an electronic health records system in the United States. Diabetol Metab Syndr 2014;6:50. 10.1186/1758-5996-6-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al Dhaheri AS, Mohamad MN, Jarrar AH, et al. . A cross-sectional study of the prevalence of metabolic syndrome among young female Emirati adults. PLoS One 2016;11:e0159378. 10.1371/journal.pone.0159378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loney T, Aw T-C, Handysides DG, et al. . An analysis of the health status of the United Arab Emirates: the 'Big 4' public health issues. Glob Health Action 2013;6:20100. 10.3402/gha.v6i0.20100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hajat C, Harrison O, Al Siksek Z. Weqaya: a population-wide cardiovascular screening program in Abu Dhabi, United Arab Emirates. Am J Public Health 2012;102:909–14. 10.2105/AJPH.2011.300290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sreedharan J, Muttappallymyalil J, Al Sharbatti S, et al. . Incidence of type 2 diabetes mellitus among Emirati residents in Ajman, United Arab Emirates. Korean J Fam Med 2015;36:253–7. 10.4082/kjfm.2015.36.5.253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dhabi SCA. Statistics center. In: SCAD [Internet], 2017. Available: https://www.scad.gov.abudhabi/Release%20Documents/Statistical%20Yearbook%20-%20Population%20-%20EN.pdf [Accessed 19 Apr 2018].
- 15.Razzak H, El-Metwally A, Harbi A, et al. . The prevalence and risk factors of obesity in the United Arab Emirates. Saudi Journal of Obesity 2017;5:57 10.4103/sjo.sjo_9_17 [DOI] [Google Scholar]
- 16.Levin A, Stevens PE, Bilous RW, et al. . Kidney disease: improving global outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013;3:1–150. [Google Scholar]
- 17.National High Blood Pressure Education Program The seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Bethesda (MD: National heart, lung, and blood Institute (US), 2004. http://www.ncbi.nlm.nih.gov/books/NBK9630/ [PubMed] [Google Scholar]
- 18.Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. executive summary of the third report of the National cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001;285:2486–97. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33 Suppl 1:S62–9. 10.2337/dc10-S062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The American Diabetes Association, European Association for the Study of Diabetes, International Federation of Clinical Chemistry and Laboratory Medicine, International Diabetes Federation . Consensus statement on the worldwide standardization of the hemoglobin A1c measurement. Diabetes Care 2007;30:2399–400. 10.2337/dc07-9925 [DOI] [PubMed] [Google Scholar]
- 21.Rosner B. Fundamentals of biostatistics. 7th edn Boston: Cengage Learning, Inc, 2010. [Google Scholar]
- 22.International Diabetes Federation IDF diabetes atlas. 8th edn Brussels, Belgium: International Diabetes Federation, 2017. [Google Scholar]
- 23.Dagenais GR, Gerstein HC, Zhang X, et al. . Variations in diabetes prevalence in low-, middle-, and high-income countries: results from the prospective urban and rural epidemiological study. Diabetes Care 2016;39:780–7. 10.2337/dc15-2338 [DOI] [PubMed] [Google Scholar]
- 24.Krishnan S, Rosenberg L, Djoussé L, et al. . Overall and central obesity and risk of type 2 diabetes in U.S. black women. Obesity 2007;15:1860–6. 10.1038/oby.2007.220 [DOI] [PubMed] [Google Scholar]
- 25.Sheikh-Ismail LI, Henry CJK, Lightowler HJ, et al. . Prevalence of overweight and obesity among adult females in the United Arab Emirates. Int J Food Sci Nutr 2009;60:26–33. 10.1080/09637480802331179 [DOI] [PubMed] [Google Scholar]
- 26.Carter AO, Saadi HF, Reed RL, et al. . Assessment of obesity, lifestyle, and reproductive health needs of female citizens of al Ain, United Arab Emirates. J Health Popul Nutr 2004;22:75–83. [PubMed] [Google Scholar]
- 27.Trainer S. Negotiating weight and body image in the UAE: strategies among young Emirati women. Am J Hum Biol 2012;24:314–24. 10.1002/ajhb.22251 [DOI] [PubMed] [Google Scholar]
- 28.Rizk DE, Bener A, Ezimokhai M, et al. . The age and symptomatology of natural menopause among United Arab Emirates women. Maturitas 1998;29:197–202. 10.1016/S0378-5122(98)00010-3 [DOI] [PubMed] [Google Scholar]
- 29.Bonora E, Kiechl S, Mayr A, et al. . High-normal HbA1c is a strong predictor of type 2 diabetes in the general population. Diabetes Care 2011;34:1038–40. 10.2337/dc10-1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clair C, Bitton A, Meigs JB, et al. . Relationships of cotinine and self-reported cigarette smoking with hemoglobin A1c in the U.S.: results from the National health and nutrition examination survey, 1999-2008. Diabetes Care 2011;34:2250–5. 10.2337/dc11-0710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dalibalta S, Mirshafiei F, Davison G. Exercise intervention on cardiovascular disease risk factors in a university population in the United Arab Emirates. Int J Adolesc Med Health 2017;30:ijamh-2016-0132. 10.1515/ijamh-2016-0132 [DOI] [PubMed] [Google Scholar]
- 32.Lindström J, Eriksson JG, Valle TT, et al. . Prevention of diabetes mellitus in subjects with impaired glucose tolerance in the Finnish diabetes prevention study: results from a randomized clinical trial. J Am Soc Nephrol 2003;14:108S–13. 10.1097/01.ASN.0000070157.96264.13 [DOI] [PubMed] [Google Scholar]
- 33.Penn L, White M, Lindström J, et al. . Importance of weight loss maintenance and risk prediction in the prevention of type 2 diabetes: analysis of European diabetes prevention study RCT. PLoS One 2013;8:e57143. 10.1371/journal.pone.0057143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al Junaibi A, Abdulle A, Sabri S, et al. . The prevalence and potential determinants of obesity among school children and adolescents in abu dhabi, United Arab Emirates. Int J Obes 2013;37:68–74. 10.1038/ijo.2012.131 [DOI] [PubMed] [Google Scholar]
- 35.Al Amiri E, Abdullatif M, Abdulle A, et al. . The prevalence, risk factors, and screening measure for prediabetes and diabetes among Emirati overweight/obese children and adolescents. BMC Public Health 2015;15:1298. 10.1186/s12889-015-2649-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Souto SB, Souto EB, Braga DC, et al. . Prevention and current onset delay approaches of type 2 diabetes mellitus (T2DM). Eur J Clin Pharmacol 2011;67:653–61. 10.1007/s00228-011-1038-z [DOI] [PubMed] [Google Scholar]
- 37.Sacks DB. A1C versus glucose testing: a comparison. Diabetes Care 2011;34:518–23. 10.2337/dc10-1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Selvin E, Crainiceanu CM, Brancati FL, et al. . Short-term variability in measures of glycemia and implications for the classification of diabetes. Arch Intern Med 2007;167:1545–51. 10.1001/archinte.167.14.1545 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.