Abstract
The present work describes spreading of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) at the tropical and temperate zones which are explained based on insolation energy, Particulate Matter (PM2.5), latitude, temperature, humidity, Population Density (PD), Human Development Index (HDI) and Global Health Security Index (GHSI) parameters. In order to analyze the spreading of SARS-CoV-2 by statistical data based on the confirmed positive cases which are collected between December 31, 2019 to April 25, 2020. The present analysis reveals that the outbreak of SARS-CoV-2 in the major countries lie on the Equator is 78,509 cases, the countries lie on the Tropic of Cancer is 62,930 cases (excluding China) and the countries lie on the Tropic of Capricorn is 22,842 cases. The tropical countries, which comes between the Tropic of Cancer and Tropic of Capricorn is reported to be 1,77,877 cases. The temperate zone countries, which are above and below the tropical countries are reported to be 25,66,171 cases so, the pandemic analysis describes the correlation between latitude, temperate zones, PM2.5 and local environmental factors. Hence, the temperature plays a pivotal role in the spreading of coronavirus at below 20 °C. The spreading of SARS-CoV-2 cases in Northern and Southern Hemispheres has inverse order against absorption of insolated energy. In temperate zone countries, the concentration of PM2.5 at below 20 μg/m3 has higher spreading rate of SARS-CoV-2 cases. The effect of insolation energy and PM2.5, it is confirmed that the spreading of SARS-CoV-2 is explained by dumb-bell model and solid/liquid interface formation mechanism. The present meta-analysis also focuses on the impact of GHSI, HDI, PD and PM2.5 on spreading of SARS-CoV-2 cases.
Keywords: SARS-CoV-2, Coronavirus, Tropical countries, COVID-19, PM2.5.
Graphical abstract
Highlights
-
•
The temperature zone countries have 14 times higher SARS-CoV-2 cases than tropical countries.
-
•
The HDI and GHSI rank values influence the mortality rate, but not in spreading of SARS-CoV-2 cases.
-
•
The 88% of SARS-CoV-2 cases were observed in very high HDI value (0.935–0.700) countries.
-
•
The dumb-bell cyclic model predicts the spreading of cases based on season, latitude, and PM2.5.
-
•
In the range of PM2.5 < 20, 20 to 35, 35–83 μg/m3 the observed cases are 80%, 12% and 5% respectively.
1. Introduction
The epidemic disease’s spread through stealth mechanism in society and depressing the socio economical status of humans, animals and birds. The SARS-CoV-2 infection rate, recovery and mortality values in particular region or country recommends the proactive approaches, preparedness, usage of advanced technology in social awareness against spreading of coronavirus. At present around 204 countries in the world are affected by the outbreak of a new virus i.e. SARS-CoV-2. The SARS-CoV-2 pandemic spreading from Southern China provinces transmitted globally, with has adverse effect on public health, economy and environment (McKee and Stuckler, 2020; Mahabee-Gittens et al., 2020). The WHO, UNO announced global pandemic on March, 11, 2020. Recently Bukhari and Jameel reported that 90% of SARS-CoV-2 spreading occurred in temperature 3 °C–17 °C and absolute humidity of between 4 and 10 gm/m3. Most of the Asian countries have the absolute humidity >10 gm/m3. The higher rainfall also increases the transmission of SARS-CoV-2 (Bukhari and Jameel, 2020; Marcos et al., 2020).
The global cases are increasing day-by-day, the social distancing is the only way to control the transmission of SARS-CoV-2. The SARS-CoV-2 symptoms are similar to respiratory infections, along with fever, cough and flu. (Vellingiri et al., 2020; Qu et al., 2020; Indranil and Prasenjit, 2020). The severe multi-organ failure leads to greater lethality, in few cases all vaccine medicines are not suitable to the patients with viral infections, due to the various geographical trends at Southern and Northern Poles of the globe (Ou et al., 2020). The respiratory activity mainly depends upon the countries geometric provinces and environmental factors, such as temperature, humidity, rainfall, air quality, PM2.5 and cold oxygen availability. It is a foremost study to establish the adverse effect by SARS-CoV-2 on the tropical and temperate zone countries (Cesar and Fabian, 2019; Zhao et al., 2012; Hongchao et al., 2020; Muhammad et al., 2020). China has reduced new cases by more than 95%, whereas the USA, Italy, Spain, and Iran closely follow exponential trends till April 25, 2020. However, currently this cannot be predicted because of differences between social distancing measures and the capacity to quickly build dedicated facilities, as like some regional provinces in China, South Korea, India. So, the Northern Hemisphere is much affected by corona virus so far (Jingui and Yongjian, 2020; Kampf et al., 2020).
The top-10 most affected countries are China, Italy, Iran, Republic of Korea, France, Spain, Germany, US, Switzerland and Japan are stands between 35° to 45° N latitude. But still there are a few countries like Turkmenistan, Uzbekistan, Tajikistan, Kyrgyzstan and North Korea have not reported many of SARS-CoV-2 cases (Richard et al., 2020; Sasmita et al., 2020). By June 21, 2020 more than 87 lakhs confirmed cases are reported globally, according to the Situation Report of the WHO. Most of these confirmed cases are from USA, Brazil, Russia, India, UK, Spain, Peru, Chile, Italy and Iran. In the fight against SARS-CoV-2, one important strategy is to keep informing the public on progress of SARS-CoV-2 via media, maps and graphics. It is an important fact that a single latitude cannot represent all the most populated countries, even though probability of spreading SARS-CoV-2 may vary with their state of provinces (Andrea and Giuseppe, 2020). Normally bacterias are resistant to temperature when compared to viruses. The coronavirus doesn’t survive very well in hotter and moisturized spots, because coronavirus has protein binders. Such virus persisted even more than 3 day at between 20 and 26 °C with relative humidity of about 45%. The surface is inactivity if more at even at 25 °C than 3 °C. The SARS-CoV-2 cases are linearly increased in Brazil at below 25.8 °C and flat at above 25.8 °C (Aaron and Michael, 2013; Lisa et al., 2010; Chan et al., 2011; David et al., 2020).
The electronic search in Medline (PubMed interface), Scopus and Web of Science, using the keywords novel coronavirus up to April 25, 2020 and those reporting data in SARS-CoV-2 patients with or without severe disease (defined as needing admission to intensive care unit or use of mechanical ventilation), are finally included in this analysis. Although the overall number of SARS-CoV-2 publication is drastically increasing, the SARS-CoV-2 become great threat to the community, it is necessary to analyze the SARS-CoV-2 spreading behaviour, with respect to latitude, temperature, PM2.5, wind speed, population density and distance from the sea, which are few major influencing factors for spreading the coronavirus (Sajadi et al., 2020; Lu et al., 2020). The present study focuses the relation between latitude vs cases, effect of insolation energy and population density and transmission mechanism with the dumb-bell model. The dumb-bell model will predict the cases in flu or non-flu season. The effect of concentration of PM2.5 on transmission rate of SARS-CoV-2 cases is also studied.
2. Materials and methods
2.1. Scope of the study area
The present study is forecasting the SARS-CoV-2 spreading behaviour in the tropical and temperate zone countries. The study divides the entire globe into three zones.
Tropical zone countries: The countries stand between 23.5° N latitude to 23.5° S latitude.
Temperate zone countries: The countries stand between 23.5° N latitude to 66.5° N latitude and 23.5° S latitude to 66.5° S latitude.
Frigid zone countries: The countries stand between 66.5° N latitude to 90° N latitude and 66.5° S latitude to 90.0° S latitude.
2.2. Data collection
The day wise reported coronavirus cases are taken from official website of European Centre for Disease Prevention and Control (Nick, 2019). On April 25, 2020 recovered and death cases of SARS-CoV-2 are collected from Johns Hopkins University and Medicine, Corona research Centre and WHO (https://www.who.int/emergencies/diseases/novel-coronavirus-2019). The GHSI of 90 countries is collected from Johons Hopkins Centre for Health Security, the Nuclear Threat Initiative and the Economist Intelligence Unit (Michelle et al., 2019). The Human Development Index of each country is collected from Human Development reports, United Nations Development Programme. The population chart and population density of 2019 are collected from Department of Economic and Social Affairs Population Dynamics, United Nations. The Air Quality Index data is collected from the 2019 World Air Quality Index report, it is one of the largest centralized platform for real-time air quality data (https://www.iqair.com/world-most-polluted-countries).
3. Results and discussion
3.1. Statistical analysis on transmission of SARS-CoV-2
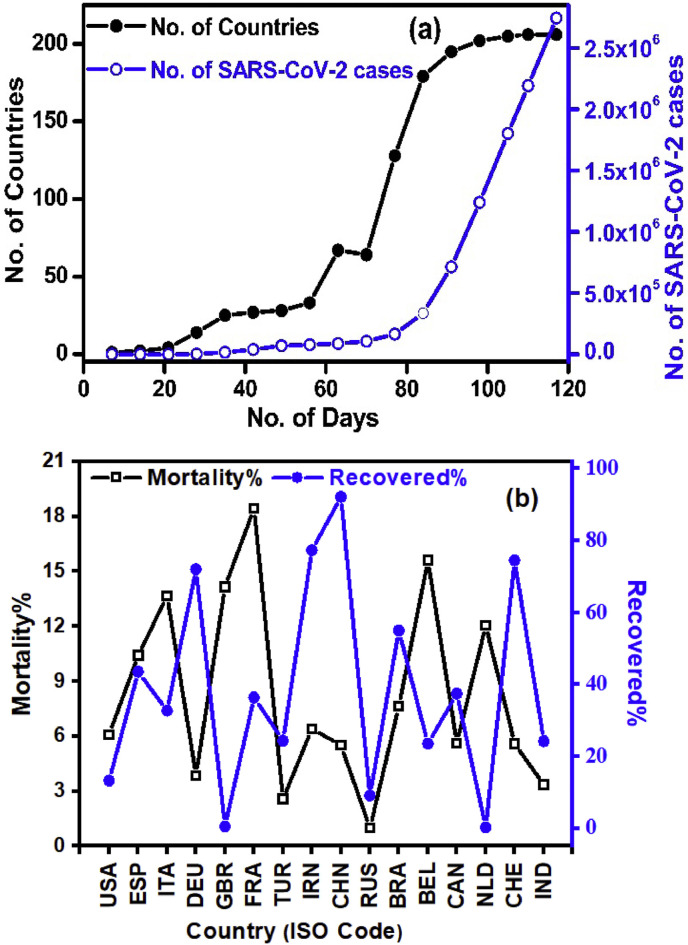
The coronavirus case tracked from December 31, 2019 to April, 25, 2020 throughout the world and depicted in Fig. 1 a. From the figure it reveals that the twenty five fold of SARS-CoV-2 cases across the globe is increased. The European Centre for Disease Prevention and Control report suggests that around 27,44,048 cases are confirmed as on April 25, 2020. The SARS-CoV-2 is spreading at the rate of 16.4 per minute.
Fig. 1.
(a) The number of cases vs number of countries with respect to number of days (This data is taken in between December 31, 2019 to April 25, 2020) (b) Mortality % vs Recovered % in top 15 countries drastically affected by SARS-CoV-2 (This data is taken on April 25, 2020).
The mortality rate and recovered rate of SARS-CoV-2 is shown in Fig. 1b. From this the effect of major outbreak is observed range from 3% to 18% of mortality. The Russia, India, Germany and turkey have lowest mortality (<3%). The effect of temperature and humidity on death rate are studied by Ma et al. group and reported that increase in temperature decreases the number of deaths, hence the SARS-CoV-2 death and growth rate are influenced by meteorological factors (Ma et al., 2020). The China, Iran, Germany and Switzerland countries have high recovered %. Though the 96% of cases are observed in top 50 countries which have high HDI and GHSI. The impact GHSI and HDI is clearly observed in the recovered and death rates.
3.2. Effect of GHSI and HDI on transmission of SARS-CoV-2
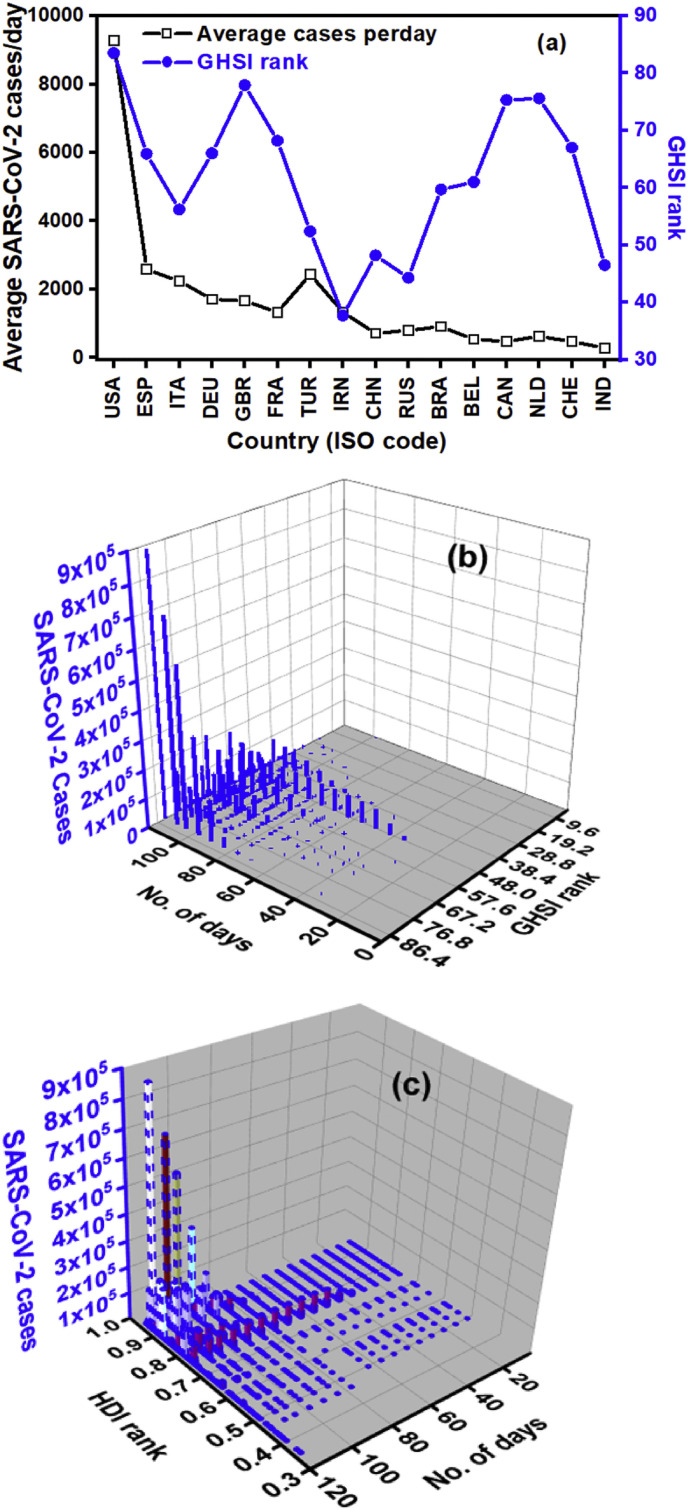
The SARS-CoV-2 becomes a biologic threat to society and world economy. The GHSI considers the prevention, detection, reporting, rapid response, health system, national capacity against epidemic diseases and risk environment factor. The present study considers all the factors in the form of overall GHSI rank. Fig. 2 a reveals that top 15 countries contribute, 85% of cases, it seems the preparedness of each country is not enough to restrict the spreading of SARS-CoV-2. Since the pandemic has no borders, it is essential to discuss the capability of the every country with respect to proactive against epidemic diseases. As per GHSI report 2019, no country is fully prepared for epidemics or pandemics, it is evidenced in Fig. 2b & c. But in the cases of most prepared countries (GHSI rank from 83.5 to 67) like USA, UK, Netherlands, Australia, Canada, Thailand, Sweden, Denmark, South Korea, Finland, France, Slovenia and Switzerland have reported around 48% of cases as on April 25, 2020. In the case of more prepared countries (GHSI rank from 63.8 to 33.7) have reported around 51% of cases as on the same date.
Fig. 2.
Effect of GHSI on (a) SARS-CoV-2 cases (b) Time (c) Effect of HDI on SARS-CoV-2 cases.
The least prepared countries (GHSI rank from 33 to 0.3) have reported around 1% of cases. The effect of the preparedness, rapid testing and sophisticated equipment usage show impact on mortality rate and spreading rate. The HDI value versus cases also reveals that the countries with high HDI (i.e. HDI value from 0.935 to 0.700) values have reported the 88% of cases. The HDI and GHSI ranks do not influence the spreading of SARS-CoV-2 in highly affected countries.
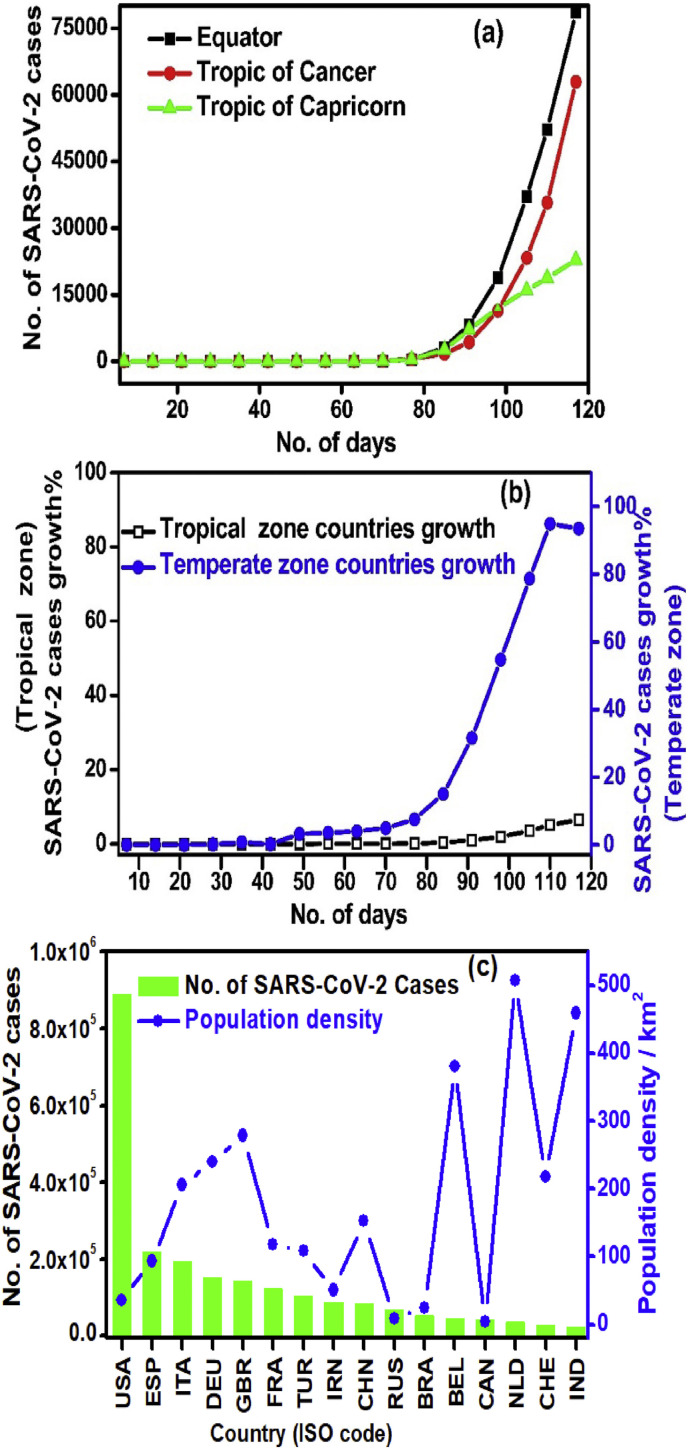
3.3. The effect of latitude and population density on transmission of SARS-CoV-2
The trend of spreading of cases is same in the countries lies on the Tropic of Cancer, Equator and Tropic of Capricorn is shown in Fig. 3 . The cases of tropical zone countries and temperate zone countries are about 6.5% and 93.5%. The cases reported in tropical zone countries are 14-times less, when compared to temperate zone countries, due to the temperature, heat of insolation, humidity, wind speed and local winds as a factor. As per previous studies, the Brazil affected by the Influenza-2009 pandemic mortality was very less in equitorial states and tropical regions of Southern Hemisphere (Cynthia et al., 2012). The role of humidity and temperature on transmission efficiency of influenza in pigs are analyzed systematically and results show that at temperature above 30 °C and absolute humidity between (6–11 gm/m3) transmission efficiency is very less (Anice and John, 2014).
Fig. 3.
(a) The countries lie on Equator, Tropic of Cancer and Tropic of Capricorn vs number of cases growth (b) The SARS-CoV-2 growth percentage in tropical and temperate zone countries (c) The effect of population density on cases.
The effect of population density on number of SARS-CoV-2 cases which are taken for highly affected countries. However there is inverse relationship between the number of cases and population density of affected countries. From Fig. 3c, the 15 affected countries have 84% cases with a population of 268.4 Crore.
The Dhaka is one of the highest population denisity (47,400/km2) and highly polluted city in South East Asian Region in the world. The Dhaka division remains the Bangladesh epicenter with 81% cases in total reported cases as on May 18, 2020. The world’s biggest slum with a population density of 2.7 lakh/km2 is called Dharavi in Mumbai reported around 1000 cases and 40 fatalities. There are 60,000 families with daily wage earners, working in small-scale leather and packaging industries and auto-rickshaw drivers spread over in 2.4 sq. km. The index patient was detected on April 1, 2020. Social distancing was difficult in dense packets in Dharavi, high risk contacts were shifted to schools, sports complexes, hostels and community halls (https://indianexpress.com/article/cities/mumbai, May 14, 2020). This suggest that the average population density of a country does not influence the spreading of cases. But the average population density of the metropolitan cities has a considerable influence on the spreading of SARS-CoV-2.
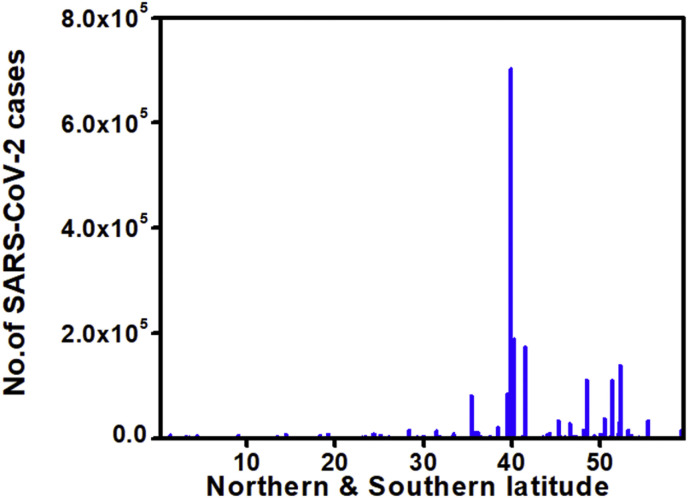
The effect of latitude on SARS-CoV-2 cases is shown in Fig. 4 . The temperate zone countries stands between 35° N to 50° N latitude are having 70% cases as on April 25, 2020. Fig. 4 reveals that the increase in latitude from 0° to 23.5° N slight increases in SARS-CoV-2 cases. The tropical countries like Brazil, Peru, Ecuador, Indonesia, Mexico, Singapore, Malaysia, Panama and Columbia have the 83% of cases. The spreading of SARS-CoV-2 in Frigid Zone (i.e. Polar Regions) could be high, because of the climatic conditions and limited facilities. Fortunately, in Antarctic region, there is no confirmed cases were observed by the end of May 2020. The total number of observed cases in Northern Frigid Zone are around 3000. These cases are reported from countries like Iceland, Alaska and Faroe Islands. Initially 13 cases were observed and at present there are no active cases in Green lands. Though the cases are less in Frigid Zone, the social distancing is mandatory to control the spread of SARS-CoV-2.
Fig. 4.
The effect of latitude on spreading of SARS-CoV-2.
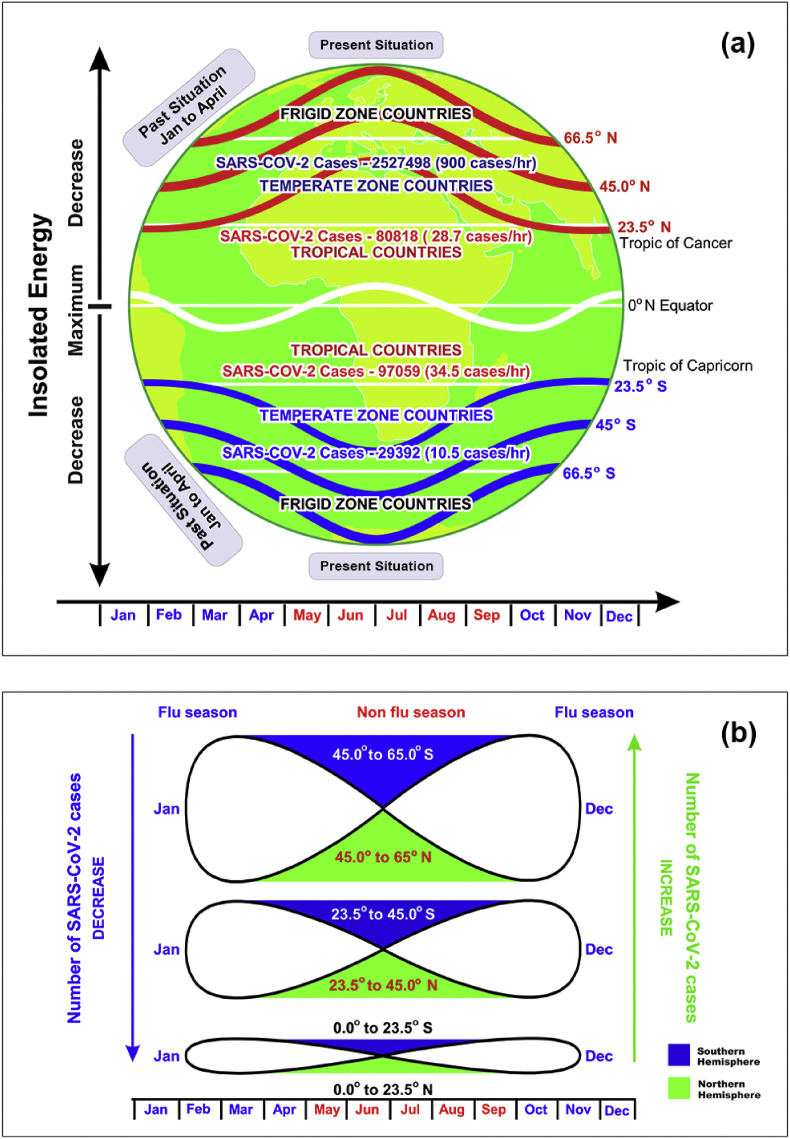
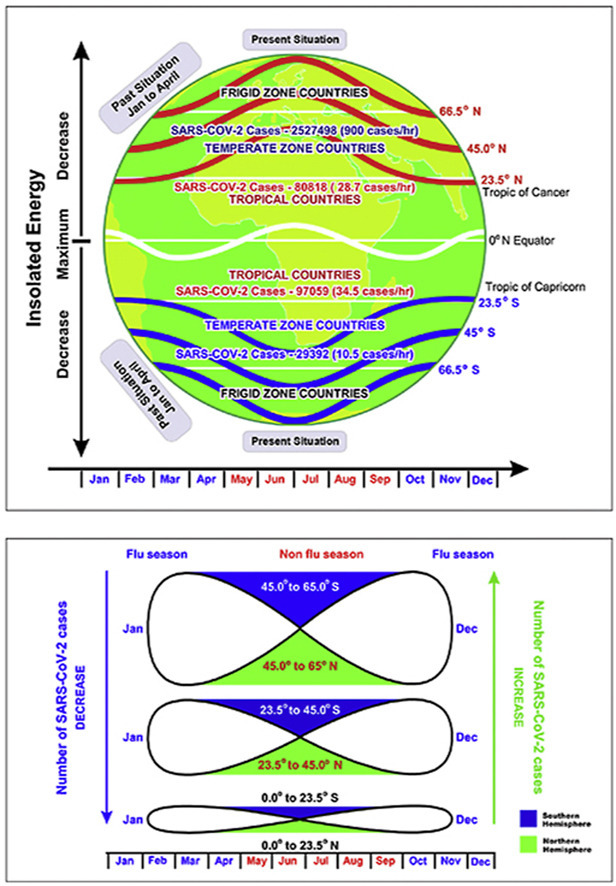
3.4. Effect of insolation energy and PM2.5
As per Robert Simmon’s illustration from NASA observatory, the insolation energy of the Northern Hemisphere is minimum in October to April month (Robert, 2009). The low amount of insolated energy results 97.5% of cases were observed in Northern Hemisphere. The high amount of insolated energy results only 2.5% cases in Southern Hemisphere. If the SARS-CoV-2 pandemic continues in future i.e. May to September, due to low energy insolation the SARS-CoV-2 pandemic cases will increase in Southern Hemisphere. But in May and June 2020 the SARS-CoV-2 cases should decrease in Northern Hemisphere (Fig. 5 ). This confirms the relation between latitude vs cases with season and helps in future for prediction of SARS-CoV-2 spread in tropical, temperate zone countries.
Fig. 5.
(a) The effect of latitude and insolation energy on growth of SARS-CoV-2 and (b) The dumb-bell model predicts the growth rate of SARS-CoV-2 (which explains the inverse relationship between Northern and Southern Hemispheres on growth of SARS-CoV-2 cases).
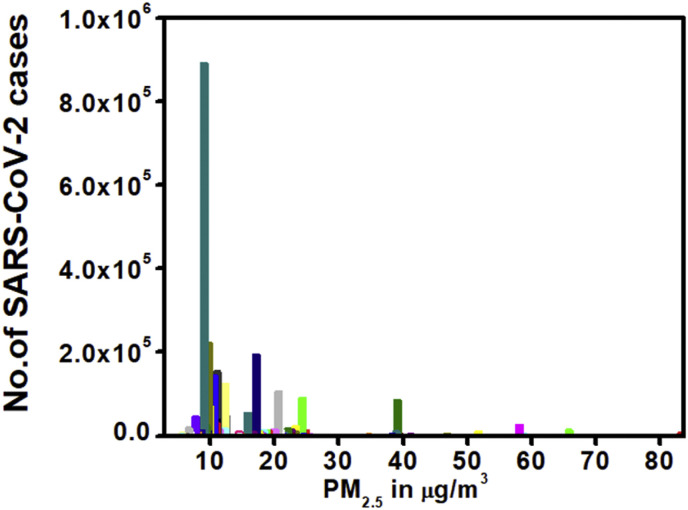
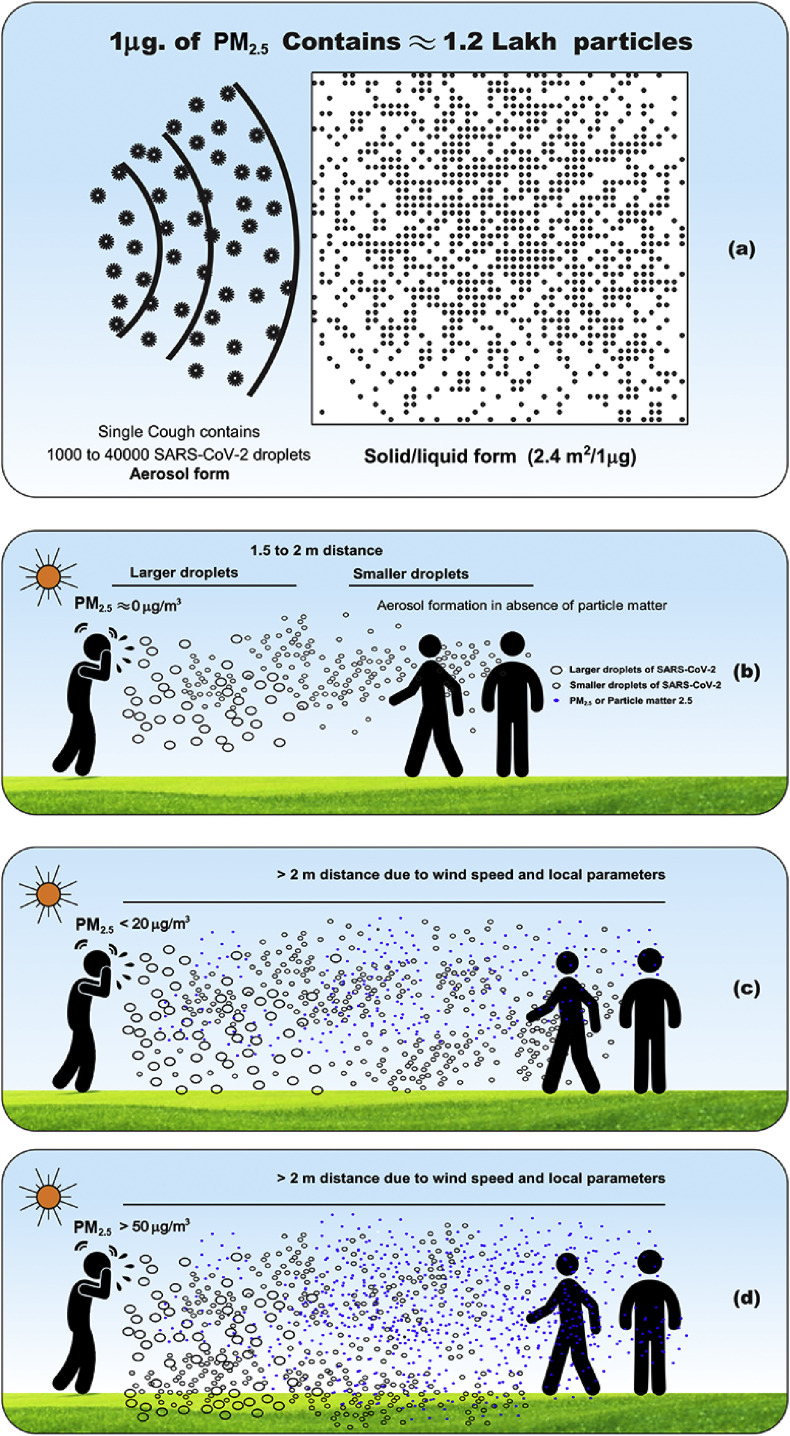
In the present proposed study a dumb-bell model, which matches with the growth of cases on different latitudes. In general flu season (October to April) the relation between influenza-like illness risk with different age groups versus of PM2.5 is reported (Feng et al., 2016). Generally the temperature and relative humidity may auxilarate the PM2.5 generation rush to spread the virus. But there is no significant relation between Influenza-like illness risk versus of PM2.5 in non-flu season (May to September). The effect of PM2.5 concentration on transmission of SARS-CoV-2 was shown in Fig. 6 . It reveals that higher number of cases were observed, when PM2.5 concentration is below 20 μg/m3. The 90% of people from the globe inhale the toxic air quality. According to World Health Organization, PM2.5 concentration should be less than 10 μg/m3. But United State Air Quality Index classifies the levels into six types. The four types are mentioned in Table .1 . The level of Good and Moderate regions, the reported cases are about 92%. At present 40% of the population is under vulnerable condition, though the PM2.5 is below 35 μg/m3. This is one of the essential points, which needs to be addresed in further research. These PM2.5 particles may contain toxic metals ions and organic matter. If virus droplet interacts with PM2.5, depends on the size of PM, shape, density and air flow or wind flow. Single cough or sneezing releases approximately from 710 to 40,000 SARS-CoV-2 droplets (Aaron and Michael, 2013). It is a huge number; definitely these virus droplets can make great interaction with PM2.5. These aerosolized droplets can remain in the air and travel long distances, >1 metre. The number of cases reported in the present study are contradictionary to the Feng et al., (2016) group results. This might be due to nature of PM2.5, temperature, humidity, wind speed and local winds favours the transmission of SARS-CoV-2 from human to human. The PM2.5/SARS-CoV-2 have high surface to volume ratio, it attaches to the respiratory epithelial cells and deposit deep in the lungs (Su et al., 2019). Moreover these particles enter the blood stream via respiratory system and travel through the body and can cause asthma, lung diseases and heart diseases. This needs to be addressed and it is challeging task. The present study results also support the airborne transmission of SARS-CoV-2. Recently Morawska and Junji also reported that the possibility of airborne transmission SARS-CoV-2 and aerosols can travel up to 10 metre (Morawska and Junji, 2020). The proposed mechanism for SARS-CoV-2 droplet with different concentrations of PM2.5, settling velocity and travel distance is shown in Fig. 7 . At ideal conditions (PM2.5 = 0 μg/m3) SARS-CoV-2 transmission could be explained within 2 metre distance through aerosol formation. But in the presence of PM2.5, SARS-CoV-2 droplets adsorb on PM2.5 and forms solid/liquid (PM2.5/SARS-CoV-2) interface. The local wind speed, temperature, humidity influences the movement of PM2.5/SARS-CoV-2 particle. At lower concentration (i.e. PM2.5 <20 μg/m3) SARS-CoV-2 droplets can travel up to 10 m which is shown in Fig. 7c. The present study results also support the airborne transmission mechanism. At higher concentration (PM2.5 >50 μg/m3), the coughing may not sufficient to displace the PM2.5 particles for longer distances, hence those PM2.5/SARS-CoV-2 droplets settle at shorter distances. Generally a single cough produces 40,000 droplets, but 1 μg of PM2.5 contains 1,20,000 particles, which have a surface area of 2.4 m2/μg (Hext et al., 1999). At higher concentrations of PM2.5 (i.e. PM2.5 >50 μg/m3) surface area and number of particles will be > 120 m2 and 60 lakh particles respectively. The SARS-CoV-2 droplets does not have the possibility to displace such a huge number of PM2.5 particles and travel for longer distances. The SARS-CoV-2/PM2.5 droplet will be influenced by wind speed and alters the settling velocity of the particle and travel distance. The South East Asian Region cities (which are having higher concentration of PM2.5) like Mumbai, Delhi, Chennai, Dhaka, Ahmadabad and Jakarta reported cases are 66,488, 62,655, 41,172, 19,492, 18,837 and 10,994 respectively (Supplementary data: Table 5). These six cities contribute 40% cases in total number of 5,80,533 cases in South East Region countries as on June 21, 2020. This reveals the effect of PM2.5 on transmission of SARS-CoV-2 cases in South East Asian Region. The India contributes 70% of cases and 65% of deaths in total South East Asian Region cases.
Fig. 6.
Effect of PM2.5 on transmission of SARS-CoV-2.
Table 1.
Effect of PM2.5 concentration on SARS-CoV-2 cases.
| S.No. | No. of countries | Range of PM2.5 μg/m3 | US AQI level | No. of SARS-CoV-2 cases | People exposed |
|---|---|---|---|---|---|
| 1 | 26 | 0 to 12 | Good | 17,040,25 | 96.3 Cr |
| 2 | 59 | 12.1 to 35.4 | Moderate | 8,19,560 | 207.8 Cr |
| 3 | 8 | 35.5 to 55.4 | Sensitive groups | 1,10,116 | 182.0 Cr |
| 4 | 5 | 55.5 to 150.5 | Unhealthy group | 42,522 | 178.7 Cr |
Fig. 7.
(a) Comparison between SARS-CoV-2 droplets and PM2.5 particles (b) Transmission of SARS-CoV-2 by Aerosol mechanism (PM2.5 = 0 μg/m3) (c) Solid/liquid interface (PM2.5 concentration < 20 μg/m3) formation d) Solid/liquid interface (PM2.5 >50 μg/m3) formation.
The spreading of SARS-CoV-2 was evidenced by PM2.5 and population density in Mumbai, Dhaka, Ahmadabad, Chennai and Jakarta cities. The best incident to explain the PM2.5 on spreading of SARS-CoV-2 cases in Asia’s largest Koyambedu Market in end of April 2020. Generally the Koyambedu Market yard is the source for vegetables, fruits and flowers. The daily labour, loading men, vendors, visitors, buyers, who spends their day time in market yard and cramped places have been exposed to the aerosolized PM2.5/SARS-CoV-2 droplets generated by infected people through coughing or sneezing or talking. This might be the major reason behind spreading of 1863 cases on May 09, 2020 (https://stopcorona.tn.gov.in/daily-bulletin). Particle size of the PM2.5 decreases, settling velocity of the particles decreases, travel distance increases and the SARS-CoV-2 spreading rate increases. This supports clearly the transmission of SARS-CoV-2 that is very high in temperate zone countries particularly at 40° N latitude.
3.5. Effect of the temperature and local winds
The top ten countries affected by SARS-CoV-2 and stands between 40° N to 50° N latitude contributes 80% of cases. Since the 40° N to 50° N latitudes have westerly winds (i.e. roaring forties and furious fifties). Particularly in Spain, France, Italy, Germany, UK and Irland the local winds like Mistral, which has speed of 66 km/h to 185 km/h. The trend of growing cases in tropical and temperate zones are well matched with Fig. S1. The growth rate of SARS-CoV-2 cases at tropical countries is around 5%, which is well matching with red colour (which indicates the temperature range between 20 °C to 45 °C) tropical zone countries shown in Fig. S1 (Supplementary data). The growth rate of cases in temperate zone countries is around 95%, which is shown with green colour (which indicates the temperature range between 3 °C to 13 °C) shown in Fig. S1. The insolated energy of tropical countries to temperate countries will varies from 0 to 50 MJ/m2 per day. In tropical countries from January to April 2020 the spreading of SARS-CoV-2 is very slow, when compared to temperate zone countries, because the insolated energy is maximum for the tropical countries. From Fig. 5 and Fig. S1, it can be confirmed that in non-flu season, possibly Southern Hemisphere cases may increase in future. In May to September 2020 the spreading of SARS-CoV-2 will be reduced and the amount of insolated energy is very high in temperate zone countries.
4. Conclusions
The present analysis reveals that the major outbreak of SARS-CoV-2 in the countries lie on the Equator, Tropic of Cancer and Tropic of Capricorn are reported to be 2.8%, 2.2% and 0.8% of SARS-CoV-2 cases. The tropical countries, which stands between the Tropic of Cancer and Tropic of Capricorn is reported to be 6.5% cases. The temperate zone countries are reported to be 93.5% cases. The effect of population density does not have a significant effect on spreading of SARS-CoV-2. The effect of the temperature and latitude is studied and proposed a dumb-bell shape model for SARS-CoV-2 spreading. The dumb-bell shape model predicts the growth of cases is cyclic process depends on season. The reported cases in Southern Hemisphere is less, Northern Hemisphere cases are more or vice versa. The effect of PM2.5 on transmission of SARS-CoV-2 and probable aerosol and solid/liquid formation mechanism is proposed. The mechanism explains the effect of particle size of PM2.5 and concentration of PM2.5 on spreading of cases. The concentration of PM2.5 < 20 μg/m3, PM2.5 ≈ 20–35 μg/m3 and PM2.5 ≈ 35–83 μg/m3 the observed cases are 80%, 12% and 5% respectively. The above results confirms that the parameters, latitude (35° – 45° N), temperature (<13 °C), lower concentration (PM2.5 < 20 μg/m3) & particle size < PM2.5 are favourable conditions for spreading of SARS-CoV-2.
CRediT authorship contribution statement
K. Chennakesavulu: Conceptualization, Investigation, Methodology, Writing - original draft. G. Ramanjaneya Reddy: Visualization, Data curation, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to express sincere thanks to Dr. Mariazeena Johnson, Chancellor, Dr. Marie Johnson, President and Dr. T. Sasipraba, Vice Chancellor of Sathyabama Institute of Science and Technology (Deemed to be University), Chennai, Tamil Nadu for their constant encouragement.
Footnotes
This paper has been recommended for acceptance by Pavlos Kassomenos.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envpol.2020.115176.
Abbreviations
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus-2
- WHO
World Health Organization
- PM2.5
Particulate Matter 2.5
- GHSI
Global Health Security Index
- HDI
Human Development Index
- AQI
Air Quality Index
- US AQI
United States Air Quality Index
- PD
Population Density
- ECDC
European Centre for Disease Prevention and Control
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Aaron F., Michael G. Aerobiology and its role in the transmission of infectious diseases. J. Pathogens. 2013:1–13. doi: 10.1155/2013/493960. Article ID: 493960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrea R., Giuseppe R. COVID-19 and Italy: what next? 2020. The Lancet Health Policy. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [Google Scholar]
- Anice C.L., John S. Roles of humidity and temperature in shaping influenza seasonality. J. Virol. 2014;88:7692–7695. doi: 10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukhari Q., Jameel Y. Elsevier; 2020. Will Coronavirus Pandemic Diminish by Summer? SSRN. [DOI] [Google Scholar]
- Cesar C., Fabian J. Organ dysfunction in sepsis: an ominous trajectory from infection to death. Yale J. Biol. Med. 2019;92:629–640. Corpus ID: 209432908. [PMC free article] [PubMed] [Google Scholar]
- Chan K.H., Peiris J.S., Lam S.Y., Poon L.L., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS corona virus. Adv. Virol. 2011:1–7. doi: 10.1155/2011/734690. 2011. Article ID: 734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cynthia S.P., Cecile V., Lone S., Mark A.M., Fernanda E.A.M., Roberto M.F., Marcia L.C., Wladimir J.A. Were equatorial regions less affected by the 2009 influenza pandemic? The Brazilian experience. PloS One. 2012;7(8) doi: 10.1371/journal.pone.0041918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David N.P., Waldecy R., Paulo H.B. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020;729:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng C., Jian L., Wenjie S., Yi Z., Quanyi W. Impact of ambient fine particulate matter (PM2.5) exposure on the risk of influenza like-illness: a time-series analysis in Beijing, China. Environ. Health. 2016;15:1–12. doi: 10.1186/s12940-016-0115-2. 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hext P.M., Rogers K.O., Paddle G.M. CONCAWE; Brussels: November 1999. The Health Effects of PM2.5 (Including Ultrafine Particles) Concawe. Report No: 99/60. [Google Scholar]
- Hongchao Q., Shuang X., Runye S., Michael P.W., Yue C., Wei T., Qing S., Wenge W., Xinyi W., Zhijie Z. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indranil C., Prasenjit M. COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci. Total Environ. 2020;728:13888. doi: 10.1016/j.scitotenv.2020.138882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jingui X., Yongjian Z. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisa M.C., Soyoung J., William A.R., David J.W., Mark D.S. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76:2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu J., Gu J., Li K., Xu C., Su W., Lai Z., Zhou D., Yu C., Xu B., Yang Z. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg. Infect. Dis. 2020;26(7):1628–1631. doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Zhou J., Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahabee-Gittens E.M., Merianos A.L., Matt G.E. Letter to the editor regarding: “an imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19)” secondhand and thirdhand smoke as potential sources of COVID-19. Environ. Sci. Technol. 2020;54(9):5309–5310. doi: 10.1021/acs.est.0c02041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcos F.F.S., Gisleia D., Ana I.G.P.S., Marcelo L.M.M., Andrede S.M. Association between climate variables and global transmission of SARS-CoV-2. Sci. Total Environ. 2020;729:138997. doi: 10.1016/j.scitotenv.2020.138997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee M., Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat. Med. 2020;26:640–642. doi: 10.1038/s41591-020-0863-y. [DOI] [PubMed] [Google Scholar]
- Michelle N., John O., Avery L., Sanjana R., Diane M., Michael S., Lucia M., Lane W. Global health security index-building collective action and accountability. 2019. https://www.ghsindex.org/wp-content/uploads/2020/04/2019-Global-Health-Security-Index.pdf
- Morawska L., Junji C. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhammad F.B., Benjiang M., Bilal, Busra K., Muhammad A.B., Duojiao T., Madiha B. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728:138835. doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nick R. Infection trajectory: see which countries are flattening their COVID-19 curve. 2019. https://www.visualcapitalist.com/infection-trajectory-flattening-the-covid19-curve/
- Ou X., Liu Y., Lei X., Li P., Mi D., Ren L., Guo L., Guo R., Chen T., Hu J., Xiang Z., Mu Z., Chen X., Chen J., Hu K., Jin Q., Wang J., Qian Z. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat. Commun. 2020;11:1620. doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu G., Li X., Hu L., Jiang G. An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19) Environ. Sci. Technol. 2020;54:3730–3732. doi: 10.1021/acs.est.0c01102. [DOI] [PubMed] [Google Scholar]
- Richard A.N., Robert D., Valentin D., Emma B.H., Jan A. Potential impact of seasonal forcing on a SARS-CoV-2 pandemic. Swiss Med. Wkly. 2020;150 doi: 10.4414/smw.2020.20224. [DOI] [PubMed] [Google Scholar]
- Robert S. 2009. https://earthobservatory.nasa.gov/features/EnergyBalance
- Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles W.F., Amoroso A. SSRN. Elsevier; 2020. Temperature, Humidity and Latitude Analysis to Predict Potential Spread and Seasonality for COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasmita P.A., Sha M., Yu J.W., Yu-Ping M., Rui-Xue Y., Qing-Zhi W., Chang S., Sean S., Scott R., Hein R., Huan Z. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect. Dis. Pov. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su W., Xiuguo W., Xingyi G., Xiaodong Z., Qiang L., Ti L. The short-term effects of air pollutants on influenza-like illness in Jinan, China. BMC Publ. Health. 2019;19:1–12. doi: 10.1186/s12889-019-7607-2. 1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellingiri B., Jayaramayya K., Iyer M., Narayanasamy A., Govindasamy V., Giridharan B., Ganesan S., Venugopal A., Venkatesan D., Ganesan H., Rajagopalan K., Rahman P.K.S.M., Cho S.G., Kumar N.S., Subramaniam M.D. COVID-19: a promising cure for the global panic. Sci. Total Environ. 2020;725:138277. doi: 10.1016/j.scitotenv.2020.138277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Aarnink A.J., Dijkman R., Fabri T., de Jong M.C., Groot K.P.W. Effects of temperature, relative humidity, absolute humidity, and evaporation potential on survival of airborne gumboro vaccine virus. Appl. Environ. Microbiol. 2012:1048–1054. doi: 10.1128/AEM.06477-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.