Abstract
Purpose
Immunoglobulin G4-related disease is a systemic fibroinflammatory disease of unknown etiology. Immunoglobulin G4-related ophthalmic disease (IgG4-ROD) can manifest in multiple ways, but lacrimal sac involvement is rare. We present the first case in Chinese population of lacrimal sac IgG4-ROD.
Observations
Lacrimal sac IgG4-ROD is rare, and only 9 cases were reported in literature. Despite reported cases in Asian population, mainly in Japan, there was none from the Chinese population or South Asia. Our index case is a 67-year-old Chinese male, who presented with a left insidious nasolacrimal duct swelling mimicking dacryocystocele. Lacrimal sac IgG4-ROD was diagnosed with radiological, serological, pathological and immunohistochemical evidence. The under-reporting of this disease entity may suggest a benign course of such.
Conclusions and importance
This is the first reported case of biopsy proven lacrimal sac definite IgG4-ROD in Chinese patient on English literature. With the limited cases reported in literature, the pathology of Immunoglobulin G4 immune process in lacrimal sac demands further investigation.
Keywords: Immunoglobulin-G4 related disease, Lacrimal sac tumor, Dacryocystocele, Chinese
1. Introduction
Immunoglobulin G4-related disease (IgG4-RD) is a systemic fibro-inflammatory disease of unknown etiology that involves single or multiple organs, characterized by lymphoproliferation with infiltration of IgG4-positive plasma cells. It can mimic malignant, infectious, and inflammatory disorders.1,2 Multiple diagnostic criteria concerning different organs involvement are available in literature, but the most commonly adapted for general use is the comprehensive diagnostic criteria of IgG4-RD introduced in 2011.3 Eye related cases can manifest in multiple ways,4 with the increase in knowledge, further diagnostic criteria for ophthalmic use was developed in 2014.5 Histopathology is always the key to diagnosis.6 Lacrimal gland involvement is common, but lacrimal sac involvement of IgG4-RD is rare, with only 9 cases reported in literature.7 We present the first case in Chinese population of lacrimal sac definite Immunoglobulin G4-related ophthalmic disease (IgG4-ROD), which is also first reported in the South Asia area.5
1.1. Case report
A 67-year old Chinese male with a history of primary open angle glaucoma presented to our clinic with a 3-month history of swelling over the left lacrimal sac region. It was symptomatic with epiphoria and sticky discharge. The swelling was non tender, and patient declined any history of trauma or injury. Examination revealed a firm swelling over the lacrimal sac to nasolacrimal duct area, with regurgitation over the left punctum upon massage of the nasolacrimal sac. There were no signs of dacryocystitis or cellulitis, and other ocular examinations were unremarkable except bilateral glaucomatous discs. Syringing was non-patent over the left side, but patent over the right side. Imaging was arranged to further evaluate the condition. Contrast Computed Tomography revealed an ~1cm hyperdense shadow over the left nasolacrimal sac to duct area, with no evidence of calcification or surrounding bony destruction (Fig. 1). Left external dacryocystorhinostomy with both diagnostic and therapeutic intent was performed. A lumpy lacrimal sac wall was found intraoperatively, and biopsy was taken for histopathological evaluation. Microscopic evaluation showed dense mixed inflammatory cell infiltrate rich in plasma cells (Fig. 2, Fig. 3). On immunostaining, the IgG4/IgG ratio was greater than 40%, with IgG4+ plasma cell count of 80–100/High Power Field (HPF) (Fig. 4, Fig. 5). There was no evidence of light chain restriction or other lymphoma features. Serum IgG4 level was 2.456 g/L (reference range: 0.168–1.000). Concluding all these investigation results with the diagnostic criteria, this patient was diagnosed of definite IgG4-ROD. Systemic screening by general physical examinations over the salivary glands, cervical and axillary lymph nodes, respiratory and abdominal systems; with the help of chest radiography, liver and renal function blood tests, did not reveal any extra-orbital involvement, and patient declined whole body imaging to look for other organs’ involvement. Patient was offered conservative treatment, without starting any steroid therapy. Post-operatively, patient symptoms improved, and there was no recurrence of the disease, nor other orbital or lacrimal gland involvement on 6th month follow-up.
Fig. 1.
Computed Tomography scan of orbit. Serial cut showing left dacryocystocele without calcification or surrounding bone erosion.
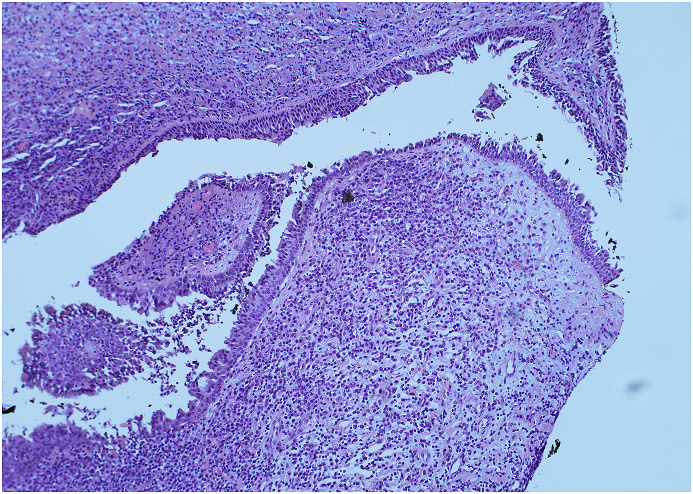
Fig. 2.
Hematoxylin-eosin staining of the left lacrimal sac wall demonstrated lymphoplasmacytic infiltration of the epithelium. (Magnification X 10).
Fig. 3.
Hematoxylin-eosin staining of the left lacrimal sac wall showing dense lymphoplasmacytic infiltration. (Magnification X40).
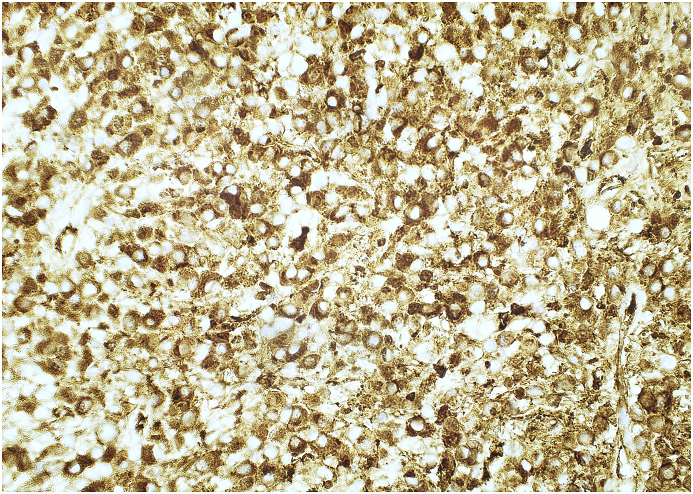
Fig. 4.
Immunostaining of the left lacrimal sac wall. Brown color outlines the immunoglobulin G. (Magnification X40). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
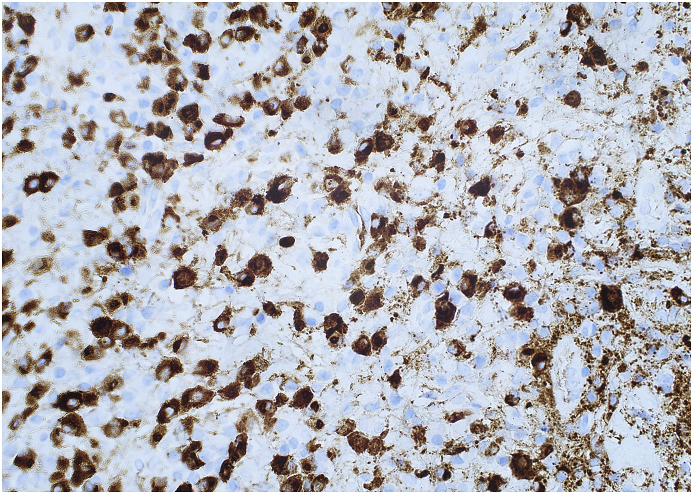
Fig. 5.
Immunostaining of the left lacrimal sac wall. Brown color highlights immunoglobulin G4 showing intensely stained Immunoglobulin G4-positive plasma cells (Magnification X40). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
2. Discussion
IgG4-RD is less commonly reported in Chinese population, to the best of our knowledge, this is the first case of biopsy proven lacrimal sac involvement of IgG4-ROD in the Chinese population reported in the English literature. Detailed search was done by searching on Pubmed, EMBASE and Medline via Ovid SP with the following terms: [“lacrimal sac” OR “dacryocystocele” OR “dacryocystitis”] AND “Immunoglobulin G4”. Results were reviewed, and articles were gone through for potential reported cases. Searching done on Jan 1, 2019 revealed no reported case of Chinese origin patient with IgG4 related lacrimal sac tumor or dacryocystocele or dacryocystitis. IgG4-RD studies focused on Chinese population were particularly searched. Few prospective large studies of IgG4-RD conducted in China published in the English literature showed some cases of typical orbital and lacrimal gland involvement, but none at the lacrimal sac.8, 9, 10, 11 Literature in Chinese with English abstract were also included. One study which presented 17 cases did not get any subject with lacrimal sac involvement.12 Another large series with of 346 patients, which reported rare features of IgG4-RD, was also lack of cases with lacrimal sac involvement.13 Back to our reported case's local data in Hong Kong, the cohort up to the end of 2016 on IgG4-RD was also reviewed, and there were no cases of lacrimal sac involvement.14
Approaching from the lesion site, lacrimal sac tumor was searched in the literature hoping to find related IgG4-ROD case reports on lacrimal sac IgG4. Although lacrimal sac tumor is rare and only <1000 cases reported in literature,15 the majority were epithelial in origin, with squamous cell carcinoma being the commonest.15, 16, 17, 18, 19 Lymphoid origin is even less, and none reported as a case of IgG4-RD.15, 16, 17, 18, 19 Particular publications on lacrimal sac tumor focused among Chinese population were also searched.20,21 The largest reported single case series in literature on 90 cases of lacrimal sac tumor, was on Chinese population, and there were no reported case of lacrimal sac IgG4-ROD.21
In this case report, we presented the details of an IgG4-ROD case with biopsy proven lacrimal sac involvement, both clinicopathologically and radiologically. The definitive diagnosis of IgG4-related ophthalmic disease was based on the findings of lacrimal sac swelling on imaging, IgG4-positive lymphoplasmacytes with 80–100 IgG4 plasma cells/HPF, and elevated serum IgG4 levels. There was no further case report found in literature after Takahashi's publication,7 and our report act as the next one. Cases reported by Takahashi,7 Sogabe,22 Marunaka,23 Kase,24 Suzuki,25 were recruited in Japan. Ginat's cases were retrieved from imaging database in United States of America,26 whereas Batra's case was in United Kingdom.27 Our case enhanced the lacrimal sac IgG4-ROD series with the first Chinese patient on literature, as well as first case reported from South Asia.
Previously reported cases mainly focused on the site of involvement, with some inadequate clinical and laboratory details for diagnosis. Eosinophilic angiocentric fibrosis or lymphoma secondary to IgG4-RD were found among them.7 When compared our case with those reported, Batra's case was the most similar.27 Both patients had history of glaucoma, presented unilaterally, with atypical dacryocystitis picture not responsive to topical antibiotics, and no systemic treatment given for the disease, nor any steroid. In our patient, only the lacrimal sac was involved without other organs involvement clinically, which is not common in IgG4-RD. However, IgG4-ROD without systemic or other organ involvement was also reported in other case series.28 Whether lacrimal sac IgG4-ROD is pathophysiologically a milder form of IgG4-RD, that usually does not have systemic involvement, making it under-diagnosed by physicians and under-reported in literature, should be observed in the future. Future studies with more cases is needed to let us understand more about this disease entity.
3. Conclusion
This is the first reported case of biopsy proven lacrimal sac definite IgG4-ROD in Chinese patient on English literature. The pathology of IgG4 immune process in lacrimal sac wall is still under investigation, and is too early to draw any conclusion with the limited number of reported case.
Contributions
Sunny, Chi Lik Au: Concept and design of study, acquisition of data and images, drafting the article, Kai Ching Peter Leung: drafting the article, Edwin Chan: revising article critically for important intellectual content, Simon, Tak Chuen Ko: revising article critically for important intellectual content
Declaration of competing interest
Nil.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2020.100789.
Contributor Information
Sunny Chi Lik Au, Email: kilihcua@gmail.com.
Kai Ching Peter Leung, Email: heyays@gmail.com.
Edwin Chan, Email: chane1@ha.org.hk.
Simon Tak Chuen Ko, Email: simonkokoko@yahoo.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kamisawa T., Zen Y., Pillai S., Stone J.H. IgG4-related disease. Lancet. 2015;385:1460–1471. doi: 10.1016/S0140-6736(14)60720-0. [DOI] [PubMed] [Google Scholar]
- 2.Stone J.H., Zen Y., Deshpande V. IgG4-related disease. N Engl J Med. 2012;366:539–551. doi: 10.1056/NEJMra1104650. [DOI] [PubMed] [Google Scholar]
- 3.Umehara H., Okazaki K., Masaki Y. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012;22:21–30. doi: 10.1007/s10165-011-0571-z. [DOI] [PubMed] [Google Scholar]
- 4.Wallace Z.S., Deshpande V., Stone J.H. Ophthalmic manifestations of IgG4-related disease: single-center experience and literature review. Semin Arthritis Rheum. 2013;43:806–817. doi: 10.1016/j.semarthrit.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Goto H., Takahira M., Azumi A. Japanese study group for IgG-related ophthalmic disease. Erratum to: diagnostic criteria for IgG4-related ophthalmic disease. Jpn J Ophthalmol. 2015;59:201. doi: 10.1007/s10384-015-0376-2. [DOI] [PubMed] [Google Scholar]
- 6.Weindorf S.C., Frederiksen J.K. IgG4-Related disease: a reminder for practicing pathologists. Arch Pathol Lab Med. 2017;141:1476–1483. doi: 10.5858/arpa.2017-0257-RA. [DOI] [PubMed] [Google Scholar]
- 7.Takahashi Y., Takahashi E., Nishimura K., Kakizaki H. Immunoglobulin G4-related dacryocystitis. Can J Ophthalmol. 2017;52:e188–e190. doi: 10.1016/j.jcjo.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Chen H., Lin W., Wang Q. IgG4-related disease in Chinese cohort: prospective study. Scand J Rheumatol. 2014;43:70–74. doi: 10.3109/03009742.2013.822094. [DOI] [PubMed] [Google Scholar]
- 9.Lin W., Lu S., Chen H. Clinical characteristics of immunoglobulin G4–related disease: a prospective study of 118 Chinese patients. Rheumatology (Oxford) 2015;54:1982–1990. doi: 10.1093/rheumatology/kev203. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y., Zhao J.Z., Feng R.E. Types of organ involvement in patients with immunoglobulin G4-related disease. Chin Med J. 2016;129(13):1525–1532. doi: 10.4103/0366-6999.184459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang L., Zhang P., Zhang X. Sex disparities in clinical characteristics and prognosis of immunoglobulin G4–related disease: a prospective study of 403 patients. Rheumatology (Oxford) 2018:key397. doi: 10.1093/rheumatology/key397. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 12.He X., Xing L., Liu H. Clinicopathologic characteristics of IgG4-related disease in orbital and periorbital tissue. Zhonghua Bing Li Xue Za Zhi. 2014 Dec;43(12):799–804. [PubMed] [Google Scholar]
- 13.Zhang P.P., Zhao J.Z., Wang M. The clinical characteristics of 346 patients with IgG4-related disease. Zhonghua Nei Ke Za Zhi. 2017;56:644–649. doi: 10.3760/cma.j.issn.0578-1426.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Li P.H., Ko K.L., Ho C.T.K. Immunoglobulin G4–related disease in Hong Kong: clinical features, treatment practices, and its association with multisystem disease. Hong Kong Med J. 2017 Oct;23(5):446–453. doi: 10.12809/hkmj176229. [DOI] [PubMed] [Google Scholar]
- 15.Krishna Y., Coupland S.E. Lacrimal sac tumors--a review. J Asia Pac Ophthalmol. 2017;6:173–178. doi: 10.22608/APO.201713. [DOI] [PubMed] [Google Scholar]
- 16.Tanweer F., Mahkamova K., Harkness P. Nasolacrimal duct tumours in the era of endoscopic dacryocystorhinostomy: literature review. J Laryngol Otol. 2013;127:670–675. doi: 10.1017/S0022215113001163. [DOI] [PubMed] [Google Scholar]
- 17.Heindl L.M., Junemann A.G., Kruse F.E., Holbach L.M. Tumors of the lacrimal drainage system. Orbit. 2010;29:298–306. doi: 10.3109/01676830.2010.492887. [DOI] [PubMed] [Google Scholar]
- 18.Montalban A., Lietin B., Louvrier C. Malignant lacrimal sac tumors. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127:165–172. doi: 10.1016/j.anorl.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Anderson N.G., Wojno T.H., Grossniklaus H.E. Clinicopathologic findings from lacrimal sac biopsy specimens obtained during dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg. 2003;19:173–176. doi: 10.1097/01.iop.0000066646.59045.5a. [DOI] [PubMed] [Google Scholar]
- 20.Zhu L.J., Zhu Y., Hao S.C. Clinical experience on diagnosis and treatment for malignancy originating from the dacryocyst. Eye(Lond) 2018;32:1519–1522. doi: 10.1038/s41433-018-0132-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song X., Wang J., Wang S., Wang W., Wang S., Zhu W. Clinical analysis of 90 cases of malignant lacrimal sac tumor. Graefes Arch Clin Exp Ophthalmol. 2018;256:1333. doi: 10.1007/s00417-018-3962-4. [DOI] [PubMed] [Google Scholar]
- 22.Sogabe Y., Ohshima K., Azumi A. Location and frequency of lesions in patients with IgG4-related ophthalmic diseases. Graefes Arch Clin Exp Ophthalmol. 2014;252:531–538. doi: 10.1007/s00417-013-2548-4. [DOI] [PubMed] [Google Scholar]
- 23.Marunaka H., Orita Y., Tachibana T. Diffuse large B-cell lymphoma of the lacrimal sac arising from a patient with IgG4-related disease. Mod Rheumatol. 2016;16:1–5. doi: 10.3109/14397595.2015.1131353. [DOI] [PubMed] [Google Scholar]
- 24.Kase S., Suzuki Y., Shinohara T., Kase M. IgG4-related lacrimal sac diverticulitis. Orbit. 2014;33:217–219. doi: 10.3109/01676830.2014.884147. [DOI] [PubMed] [Google Scholar]
- 25.Suzuki M., Mizumachi T., Morita S., Kubota K., Iizuka K. A case of immunoglobulin 4-related disease with bilateral mass-forming lesions in the nasolacrimal ducts. J Clin Rheumatol. 2011;17 doi: 10.1097/RHU.0b013e31821c71a3. 2077–10. [DOI] [PubMed] [Google Scholar]
- 26.Ginat D.T., Freitag S.K., Kieff D. Radiographic patterns of orbital involvement in IgG4-related disease. Ophthalmic Plast Reconstr Surg. 2013;29:261–266. doi: 10.1097/IOP.0b013e31829165ad. [DOI] [PubMed] [Google Scholar]
- 27.Batra R., Mudhar H.S., Sandramouli S. A unique case of IgG4 sclerosing dacryocystitis. Ophthalmic Plast Reconstr Surg. 2012;28:e70–e72. doi: 10.1097/IOP.0b013e31822d7f9b. [DOI] [PubMed] [Google Scholar]
- 28.Matsuo T., Ichimura K., Sato Y. Immunoglobulin G4 (IgG4)-positive or -negative ocular adnexal benign lymphoid lesions in relation to systemic involvement. J Clin Exp Hematop. 2010;50:129–142. doi: 10.3960/jslrt.50.129. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.