Abstract
We present magnetic resonance imaging findings of an 11-year-old girl with a mammary analogue secretory carcinoma (MASC) of the parotid gland. MASC is a recently described tumor of the salivary glands that is genetically and histologically similar to secretory breast carcinoma. To date, a few cases have been reported in the pediatric population, with limited information of its imaging characteristics. We suggest that decreased T2 signal of the solid component of the MASC representing cellular components with associated complex cystic parts may be a helpful imaging finding and can make a substantial contribution in differentiating this new entity from other rare pediatric parotid masses. Although there are no characteristic imaging findings at this time, MASC should be considered in the differential of salivary gland tumors in the pediatric population as well.
Keywords: Mammary analogue secretory carcinoma, Parotid gland, Salivary gland, Mass, Magnetic resonance imaging, Pediatric
Introduction
Mammary analogue secretory carcinoma (MASC) is a rare salivary gland tumor that is named for its histologic and genetic similarity to secretory breast carcinoma. MASC was first described in a 2010 case series by Skalova et al. [1] as having the characteristic translocation t(12;15) ETV6-NTRK3 which produces a chimeric, constitutively active tyrosine kinase receptor. This translocation has been reported in secretory breast carcinoma and MASC, as well as several other malignancies including congenital mesoblastic nephroma and congenital fibrosarcoma [2]. Before it was characterized as a distinct pathologic entity, MASC was misdiagnosed as a different salivary tumor, usually acinic cell carcinoma or cystadenocarcinoma [3,4].
MASC is an extremely rare diagnosis in the pediatric population with 13 previously reported cases in the literature [5,6]. Information regarding the clinical course and optimal treatment of MASC is therefore limited. Presentation is usually as a slow-growing, painless mass, incidentally discovered by the patient with palpation. Metastases have not been reported in the pediatric population, and all reported pediatric cases have been treated with surgical resection. Adult patients with MASC are rarely reported to present with metastases, 20% have received postoperative radiation therapy, and 2% have received chemotherapy. Mean disease-free survival in adult patients has been reported to be 92 months [3]. Imaging findings of MASC have been underreported, particularly in pediatric patients.
We report a rare case of MASC in a pediatric patient, with MRI findings and histopathologic confirmation.
Case report
An 11-year-old female presented to her pediatrician for evaluation of a right cheek mass that slowly grew over the course of 2 months, first noticed after she had braces placed. She had no other symptoms. Physical exam showed a 2 × 2 cm, mobile, nontender right cheek mass. She was referred to pediatric otolaryngology, and fine needle aspiration was performed at an outside institution. The fine needle aspiration showed epithelial cells with vacuolated cytoplasm and small, round nuclei. Staining was positive for mammoglobin and S100, and negative for DOG1. Fluorescence in situ hybridization (FISH) was positive for ETV6 gene rearrangement on chromosome 12. A diagnosis of mammary analogue secretory carcinoma was established.
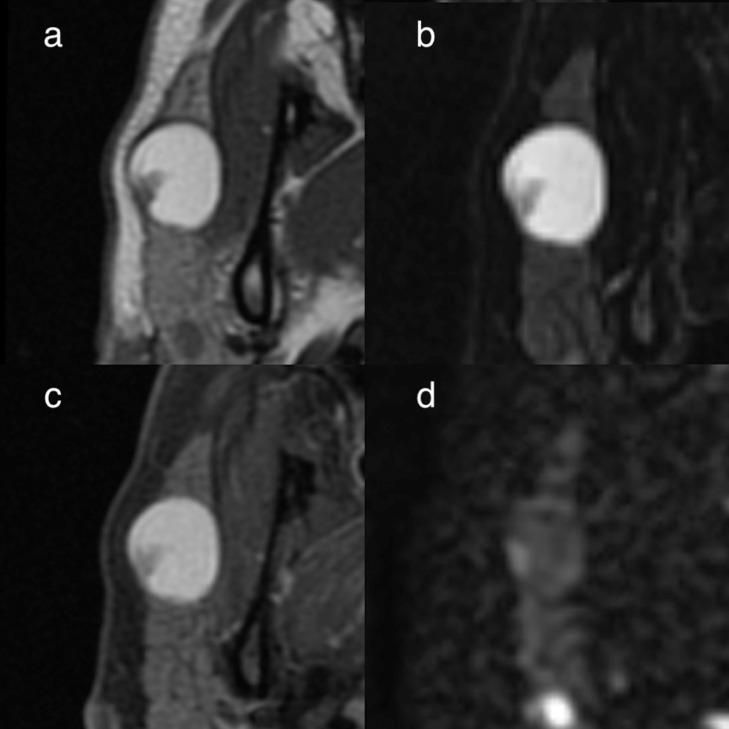
Preoperative MRI with and without contrast (Fig. 1) showed a well-circumscribed, mixed solid, and cystic mass of the superficial right parotid gland. The smaller solid component showed decreased signal on T1- and T2-weighted imaging and was associated with mild enhancement. The larger cystic component of the mass demonstrated nodular septations and increased signal on T1- and T2-weighted imaging. There was no evidence of metastases or invasion into adjacent structures.
Fig. 1.
Axial T1-weighted (a), T2-weighted with fat saturation (b), postgadolinium T1-weighted with fat saturation (c), and DWI (d) MRI sequences of a right parotid gland mammary analogue secretory carcinoma in an 11-year-old girl.
The subtotal parotidectomy was performed after a multidisciplinary tumor board decision, with no additional treatment of radiation or chemotherapy. During surgical resection, multiple branches of the facial nerve were found to be intertwined with the mass. Photographs of the gross specimen were taken after resection (Fig. 2). Surgical pathology showed a 2.5 × 1.8 cm cystic mass with an appearance consistent with a low-grade epithelial tumor (Fig. 3). An ETV6-involved translocation (12p13.2 (ETV6 sep) was documented by FISH. Postoperatively the patient had right facial weakness, which had essentially completely resolved 6 months after the surgery. She has no evidence of recurrence.
Fig. 2.
Gross specimen of the surgically resected mammary analogue secretory carcinoma.
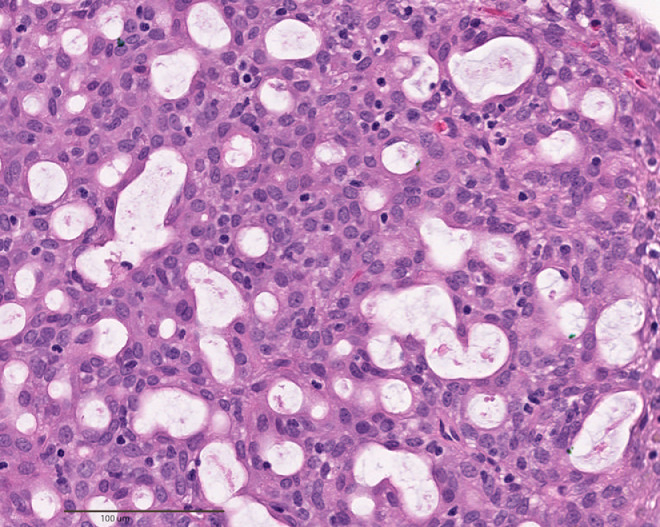
Fig. 3.
Microscopic appearance of the resected right parotid mammary analogue secretory carcinoma. A formalin fixed, paraffin embedded, hematoxylin and eosin stained section shows the solid portion of the tumor to be predominantly microcystic with some abortive tubules. Cells have indistinct borders and eosinophilic, finely vacuolated cytoplasm. Nuclei are mildly enlarged, tend to be centrally located, and contain coarse but evenly distributed chromatin. No mitotic figures are present. Histology alone does not diagnose MASC because other low grade salivary tumors, such as acinic cell carcinoma, can have the same appearance. Genetic testing is necessary.
Discussion
MASC is a recently described entity that is extremely rare in pediatric patients. Our case report focuses on MR imaging findings of MASC that can help differentiate this newly recognized neoplasm from other rare parotid masses in children.
The disease can present initially as an incidentally detected painless unilateral swelling of the cheek as in our case. The imaging plays a crucial role to further characterization of parotid lesions. Although cases of metastatic and fatal disease have been reported in adults [3], no pediatric cases with metastases or treatment with radiation or chemotherapy have been reported.
In our case, preoperative MRI showed a complex mass with cystic and small solid components in the left superficial parotid gland. The solid component was hypointense on T2-weighted imaging and showed mild enhancement after gadolinium administration, corresponding to the cellular, microcystic region seen on the histology. The cystic component was hyperintense on T1- and T2-weighted imaging, corresponding to the proteinaceous cystic fluid seen on histology. On diffusion-weighted images, nonenhancing large portion of the mass has increased ADC signal (mean ADC value: 2.4 × 10−3 mm2/s) and small peripheral enhancing component (mean ADC value: 1.1 × 10−3 mm2/s) of the mass with relatively lower signal.
There are a few reports of MASC in pediatric cases with varying imaging findings such as a "well-circumscribed lesion with internal T2 hyperintensity and intermediate T1 signal with a dependent fluid level"; a "mildly enhancing preauricular subcutaneous soft tissue mass"; and a "heterogeneously enhancing tumor." CT findings described as a "cystic, peripherally enhancing mass"; a "fluid collection with rim enhancement"; “a well-defined, lobulated, heterogeneously enhancing soft tissue density mass”; and a "mass" [5], [6], [7].
Parotid gland masses are rare in the pediatric population with variable clinical presentations and imaging findings. Differential diagnosis for a parotid gland mass in children commonly include infectious or inflammatory etiologies such as sialadenitis, abscess, or reactive lymphadenopathy; congenital lesions such as first branchial cleft cyst; and benign neoplasms such as hemangioma, lymphangioma, or pleomorphic adenoma. The malignant neoplasms such as acinic cell carcinoma, adenoid cystic carcinoma, or mucoepidermoid carcinoma are very rare in the pediatric age group.
The imaging features of parotid tumors particularly in adults are well known and widely discussed in the literature.
MRI features of MASC particularly the solid components are very similar to adenoid cystic carcinoma reflecting the tumors’ similar histology. It has been noted shortly after the initial description of MASC that many previously diagnosed adenoid cystic carcinomas in fact were MASCs after testing for the ETV6-NTRK3 fusion gene [4,7]. As Christe et al. reported on their study, low T2 signal intensity and ill-defined margins of the parotid mass after contrast administration have been shown to predict malignancy, and likely the most helpful MRI finding as predictive of adenoid cystic carcinoma [8].
MASC is characterized by the t(12;15) translocation which creates the ETV6-NTRK3 fusion gene. The resultant chimeric tyrosine kinase receptor is a potential target for therapy. Ongoing studies show the promise of targeted therapy for MASC which differs from adenoid cystic carcinoma treatment [9].
MASC may mimic other parotid tumors such as adenoid cystic carcinoma which requires a different clinical and treatment management. As radiologists, we should consider MASC in our differential diagnosis as a potential rare pediatric parotid tumor. We suggest that decreased T2 signal of solid component of the MASC representing cellular components with associated complex cystic parts may be a helpful imaging finding and can make a significant contribution in differentiating this new entity from other rare pediatric parotid masses. Future prospective studies are needed to evaluate the clinical significance of these imaging features as a noninvasive diagnostic tool.
Footnotes
Competing Interest: None.
References
- 1.Skalova A., Vanecek T, Sima R, Laco J, Weinreb I, Perez-Ordonez B. Mammary analogue secretory carcinoma of salivary glands, containing the ETV6-NTRK3 fusion gene: a hitherto undescribed salivary gland tumor entity. Am J Surg Pathol. 2010;34(5):599–608. doi: 10.1097/PAS.0b013e3181d9efcc. [DOI] [PubMed] [Google Scholar]
- 2.Knezevich S.R., McFadden DE, Tao W, Lim JF, Sorensen PH. A novel ETV6-NTRK3 gene fusion in congenital fibrosarcoma. Nat Genet. 1998;18(2):184–187. doi: 10.1038/ng0298-184. [DOI] [PubMed] [Google Scholar]
- 3.Chiosea S.I., Griffith C, Assaad A, Seethala RR. Clinicopathological characterization of mammary analogue secretory carcinoma of salivary glands. Histopathology. 2012;61(3):387–394. doi: 10.1111/j.1365-2559.2012.04232.x. [DOI] [PubMed] [Google Scholar]
- 4.Bishop J.A., Yonescu R, Batista DAS, Westra WH, Syed ZA. Cytopathologic features of mammary analogue secretory carcinoma. Cancer Cytopathol. 2013;121(5):228–233. doi: 10.1002/cncy.21245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ngouajio A.L., Drejet SM, Philipps DR, Summerlin D-J, Dohl JP. A systematic review including an additional pediatric case report: Pediatric cases of mammary analogue secretory carcinoma. Int J Pediatr Otorhinolaryngol. 2017;100:187–193. doi: 10.1016/j.ijporl.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Mahmood H., Fatima H., Faheem M. Mammary analogue secretory carcinoma of parotid gland in a teenage boy. J Coll Physicians Surg Pak. 2017;27(9):579–581. [PubMed] [Google Scholar]
- 7.Quattlebaum S.C., Roby B, Dishop MK, Said MS, Chan K. A pediatric case of mammary analogue secretory carcinoma within the parotid. Am J Otolaryngol. 2015;36(6):741–743. doi: 10.1016/j.amjoto.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Christe A., Waldherr C, Hallett R, Zbaeren P, Thoeny H. MR imaging of parotid tumors: typical lesion characteristics in MR imaging improve discrimination between benign and malignant disease. AJNR Am J Neuroradiol. 2011;32(7):1202–1207. doi: 10.3174/ajnr.A2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drilon A., Li G, Dogan S, Gounder M, Shen R, Arcila M. What hides behind the MASC: clinical response and acquired resistance to entrectinib after ETV6-NTRK3 identification in a mammary analogue secretory carcinoma (MASC) Ann Oncol. 2016;27(5):920–926. doi: 10.1093/annonc/mdw042. [DOI] [PMC free article] [PubMed] [Google Scholar]