Abstract
Background
The Janani Suraksha Yojana (JSY) is the largest ever conditional cash transfer programme worldwide. It primarily aimed to reduce the maternal and child mortality by increasing the facility based delivery in India. Besides, the JSY has resulted in reduction of out-of-pocket expenditure for delivery care and increased antenatal care. Though studies have examined the direct outcome of JSY, limited studies have attempted to understand the unintended effects (indirect) of the programme. The aim of this study is to examine the effect of JSY on contraceptive use, initiation of breast feeding and postnatal check-up in India.
Data & Methods
Data from the National Family Health Survey 4, 2015–16 was used in the analyses. A total of 148,746 institutional births in five years preceding the survey were analysed and the analyses were carried out for Low Performing States (LPS) and High Performing States (HPS). Descriptive statistics and the propensity score matching were used to understand the unintended effects of JSY.
Results
In India, the use of contraception, early initiation of breastfeeding and postnatal check up was consistently higher among JSY beneficiaries compared to non-JSY beneficiaries. Among JSY beneficiaries, about 45% of the mothers breastfed their child within one hour compared to 42% of the JSY non-beneficiaries. The pattern was almost similar for postnatal check-up. The variations in contraceptive use, breastfeeding practice and postnatal check-up among JSY beneficiaries were higher in LPS states compared to HPS. For instance, in LPS, among JSY beneficiaries, about 58% mothers breastfed their child within one hour of delivery compared to 46% in HPS. Controlling for socio-economic covariates, the JSY beneficiaries in LPS were 12% more likely to use contraception, 8% were more likely to initiate the breast feeding within one hour of child delivery and 6% were more likely to get their postnatal check-up than their counterparts in HPS.
Discussion
The unintended effects of JSY were strong and significant in the low performing states. The coverage of JSY should be further extended and the programme needs to be continued.
Keywords: Janani Suraksha Yojana, Unintended effects, Propensity score matching, India, Low performing states, High performing states, Institutional delivery
Highlights
-
•
This paper attempts to capture the unintended effects of conditional cash transfer programme Janani Suraksha Yojana (JSY) on contraception use, breastfeeding practice and post natal check-up.
-
•
A sample of 148746 births (last birth) from Demographic and Health Survey data for India which named as National Family Health Survey (NFHS) round 4 has been used.
-
•
The use of contraception, early initiation of breastfeeding and post natal check up was consistently higher among JSY beneficiaries compared to non-JSY beneficiaries. The variation in contraceptive use, breastfeed practice and post natal check-up among JSY beneficiaries were higher in LPS states compared to HPS.
-
•
Controlling for socio-economic covariates, the JSY beneficiaries in LPS are 12% more likely to use contraception, 8% more likely to initiate the breastfeeding within one hour and 6% more likely to get their postnatal check-up than mothers from HPS.
1. Introduction
Improving maternal and child health has been accorded priority in global, national and local development agenda. Reduction of maternal and child mortality were placed as two of the eight Millennium Development Goals (MDG, Goal 4 and Goal 5). Goal 3 of the Sustainable Development Goal (SDG) aims to improve health for all by 2030. Despite these, the global progress in reduction of maternal and child mortality has been slow and uneven (Bhutta et al., 2010; Souza et al., 2014; WHO, 2005). An estimated 8.8 million children die before reaching fifth birth day and 0.5 million mothers die during pregnancy and childbirth (Hogan et al., 2010; You et al., 2010). The majority of these deaths are of poor mothers from developing countries.
Improving facility based delivery has been recommended as the most cost effective way to reduce maternal and child mortality and has been included as one of the key monitoring indicators in MDGs and SDGs. Many welfare government, the non-governmental organisation and international organisation in developing countries have implemented the conditional cash transfer programs, also known as the demand-side financing (DSF) to increase the facility based delivery (Ensor et al., 2017; Kuwawenaruwa et al., 2016; Rahman & Pallikadavath, 2018; Skiles et al., 2015; Yang et al., 2016). Studies have found that these programmes have been successful to increase maternal and child health care utilization, (Barber and Gartler, 2008; De Brauw et al., 2011; Morris et al., 2004; Powell-Jackson & Hanson, 2012).
India had the world's highest under five deaths in 2015 and had contributed to one-fifth of the maternal deaths worldwide (Liu et al., 2016; Montgomery et al., 2014). While the level of maternal and child mortality has been declining over time, the relative share remains similar. Poor, less educated and rural mothers are less likely to receive the maternal and child health services in the country (Das Gupta, 1990; Goli et al., 2013; Singh et al., 2012). In 2005, the Govt of India introduced the Janani Suraksha Yojana (JSY), a conditional cash transfer scheme under National Health Mission (NHM) that provides monetary incentives to poor and marginalised mothers to deliver in a health facility. With an estimated budget of 19.8 billion INR in 2009–10, the JSY is one of the largest ever centrally funded conditional cash transfer schemes worldwide. In 2016–17, the JSY covered one crore beneficiaries in the country (MoHFW, 2018). The scheme stratifies the states as Low Performing States (LPS) and High Performing States (HPS) based on rate of institutional delivery and accorded high priority to mothers from LPS. A sum of 1000 INR or $ 22.2 in urban areas and 1400 INR or $ 31.1 in rural areas were paid to mothers delivering at public/accredited private health centers in LPS. The JSY has also made provisional incentives for community-level health workers known as accredited social health activists (ASHAs).
Since the implementation of NHM, the progress in maternal and child health has been significant. The maternal mortality ratio (MMR) has declined from 254 in 2004–06 to 130 by 2014–16, while that of under-five declined from 69 in 2008 to 39 in 2016 (ORGI, 2018). A number of studies in India have focused on the impact assessment and welfares derived from the JSY scheme on maternal and child health care in India at the national, state, district and individual levels (Devadasan et al., 2008; Lim et al., 2010; Sharma et al., 2009; UNFPA, 2009). The JSY has been successful in increasing institutional delivery, reducing maternal and child mortality (Govil et al., 2016; Gupta et al., 2011; Lim et al., 2010), out-of-pocket expenditure and catastrophic health spending (Mohanty et al., 2012). However, regional variations exist in the coverage and effects of the implementation of JSY in India (Thonkong et al., 2017). Though studies have examined the effect of JSY on the coverage of antenatal care, institutional delivery, out-of–pocket expenditure, limited attempts were made to understand the effect of JSY in initiation of breastfeeding, postnatal care and contraceptive use (Carvalho et al., 2014; Gopalan and Durairaj, 2012; Gupta et al., 2011; Kumar et al., 2015; Lim et al., 2010; Lim et al., 2010, 2010; Mukherjee et al., 2018; Mukhopadhyay et al., 2016; Nandi & Laxminarayan, 2016; Ng et al., 2014; Powell-Jackson, 2015; Rahman & Pallikadavath, 2018; Sachdeva & Malik, 2012; Sengupta & Sinha, 2018; Sidney et al., 2016). We have termed these effects as unintended effects and used interchangeably as indirect effects. The objective of the paper is to examine the effects of JSY on contraceptive use, initiation of breastfeeding and postnatal check-up in India.
2. Data and methods
2.1. Data
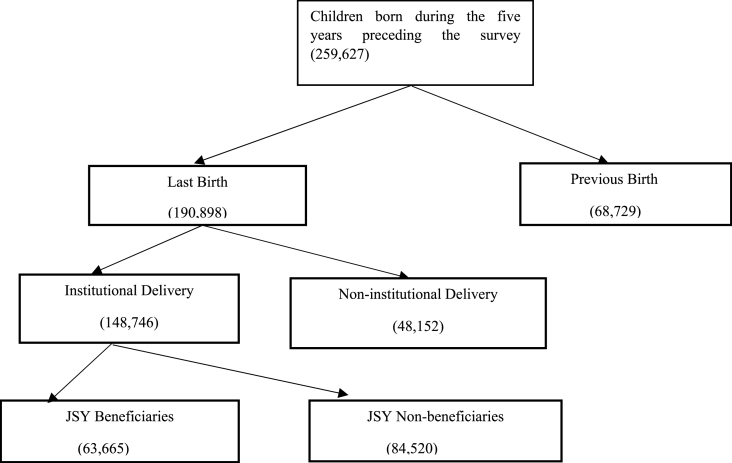
Data from the National Family Health Survey 4 (NFHS 4), 2015-16 has been used in the analyses. The NFHS 4 is the fourth in the series of the repeated cross-sectional Demographic and Health Surveys (DHS), conducted during 2015–16. The primary aim of NFHS 4 was to provide reliable estimates of demographic, maternal and child health (MCH) and nutrition across all states and union territories of India. A total of 601,509 households, 699,686 women aged 15–49 years and 112,112 men aged 15–54 years were successfully interviewed during 2015–16. While maintaining comparability with earlier rounds, the NFHS 4 has included a number of new domains and for the first time provided district level estimates of selected indicators. The detailed sampling design, coverage and findings of the survey are available in the national report (IIPS and ICF, 2017). We have used the unit data from the kids file that covered 190,898 births (last birth) in five year preceding the survey. Of these births, 148,746 births were conducted in health facilities of which JSY assistance was provided to the mothers of 63,665 births (Fig. 1).
Fig. 1.
Schematic presentation of children born in five year preceding the survey by place of delivery and JSY beneficiaries in India, 2015-16.
2.2. Methods
2.2.1. Outcome variables
The current contraceptive use, initiation of breastfeeding within an hour after childbirth and postnatal check-up of baby among the JSY beneficiaries and non-beneficiaries are the outcome variables in the analyses.
2.2.2. Treatment variable
In NFHS 4, mothers were asked about receiving of any financial assistance at the time of delivery. The question was asked only for the last birth. Mothers who received cash assistance (yes/ no) from JSY have been treated as treatment group in this study. There was no overlapping between treatment and control group as they were mutually exclusive in nature.
2.2.3. Matching variables
In this study, a number of matching variables have been included on the basis of available literature. The list of pre-intervention variables includes mothers' and household characteristics. The mother's characteristics include age (15–24, 25–34, 35+ years), educational attainment (no education, primary, secondary and higher), pregnancy complication (no complication, any complications), place of delivery (public health facility, private health facility) religion (Hindu, Muslim and others), caste (scheduled caste, scheduled tribe, other backward classes, others). The household characteristics include wealth quintile (poorest, poorer, middle, richer and richest), place of residence (rural, urban) and sex of the household (male, female). The pregnancy complications include excessive bleeding, prolonged labour or breech position.
2.2.4. Statistical analysis
Descriptive statistics and the propensity score matching were used in the analyses.
2.2.5. Propensity score matching analysis
Propensity score matching (PSM) analysis is a designed statistical tool to evaluate any programme or intervention in the absence of randomized clinical trial (Rosenbaum et al., 1985; Rubin et al., 1996). In this study, we compared the mothers who had received JSY benefit and who did not.
The advantage of matching method is that it compares the outcomes of treated and controlled individuals with similar observed characteristics or in other words, individuals have similar likelihood of being assigned in treated group (Babalola et al., 2005; Dixit et al., 2013; Do et al., 2006; Yanovitzky et al., 2005). A number of research studies have used the PSM for evaluating various programmes (Lechner, 2002:; Pufahl et al., 2009; Diaz et al., 2006; Mensah et al., 2010; Dixit et al., 2013). We have assumed that mothers who had received JSY benefit are random and not correlated with outcome of interest. The average outcome is compared between treated women (who had received JSY benefit) and untreated women (who had not received the benefit). The treated and untreated women are expected to be statistically equivalent in all relevant characteristics.
2.2.5.1. Propensity score
The PSM is the probability that a woman received JSY benefit with a certain pre-specified characteristics and written as
| p (X) = Pr (D = 1|X) | (1) |
where D = 0 if the woman belongs to JSY non-beneficiaries group.
D = 1 if the woman belongs to JSY beneficiaries group.
And X is the vector of pre-intervention characteristics.
2.2.5.2. Defining impact of JSY benefit
In PSM, three parameters are estimated. These are average treatment effect (ATE), average treatment effect on treated (ATT) and average treatment effect on untreated (ATU). The Average Treatment Effect (ATE) measures the mean impact of JSY benefit across all the women in the population. This parameter may be defined as
| ATE = E (δ) = E (Y1– Y0) | (2) |
where E(.) means average and Y1 represents potential outcome for JSY beneficiaries and Y0 represents potential outcome for JSY non-beneficiaries.
With the help of counterfactual model, the Average Treatment Effect on the Treated (ATT) could be measured and can be written as
| ATT = E (Y1|D = 1)- E(Y0|D = 1) | (3) |
Where E (Y1|D = 1) is the average outcome of the women who have received JSY benefit.
E(Y0|D = 1) is the counterfactual, it shows average outcome that the treated individuals would have obtained in absence of JSY benefit, which is unobserved.
Finally, the Average Treatment Effect on the untreated women (ATU) has been measured, which shows the impact of JSY benefit would have had on those who did not receive JSY benefit.
| ATU = E (Y1|D = 0) – E(Y0|D = 0) | (4) |
where E (Y1|D = 0) is the average observed outcome for those women who did not have JSY benefit.
E(Y0|D = 0) the counterfactual and it shows the average outcome for those women who would have received the benefit which they had not received earlier, which is unobserved.
Logistic regression has been used to measure the gaps in odds of socio-economic controls on contraceptive use practice, breastfeeding within one hour and postnatal check-up. The independent variables are age of mother, education level, religion, caste, wealth quintile, sex of the head of the household, place of residence and place of delivery.
3. Results
3.1. Coverage of JSY assistance in India
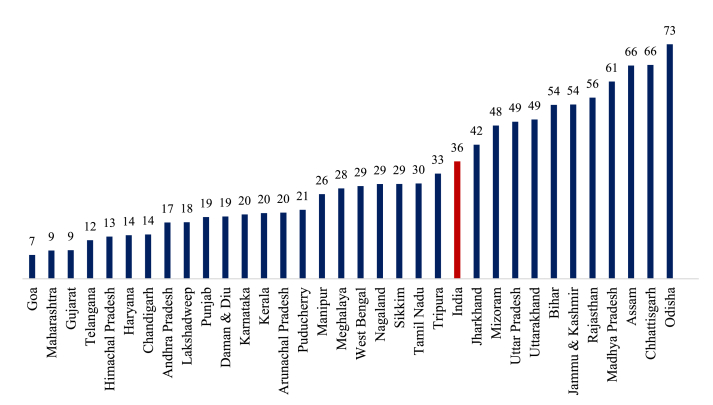
Fig. 2 presents the inter-state variation of JSY coverage in India. Around 36% of the women in India were covered by JSY assistance; lowest in Goa (7%) followed by Maharashtra and Gujarat (9% each). It was highest in Odisha (73%) followed by Chhattisgarh and Assam (66%). More than half of the eligible women in seven states of India had received JSY assistance for facility based delivery.
Fig. 2.
Percentage of mothers received JSY assistance for facility based delivery in India, 2015-16.
Table 1 presents the socio-economic differentials in the coverage of JSY assistance in LPS and HPS. In general, the JSY coverage was higher in the LPS compared to HPS across all the selected socio-economic groups. In the rural areas, the JSY coverage was 60% in LPS compared to 23% in HPS. The JSY coverage was higher among less educated mothers compared to educated mothers in both LPS and HPS. For example, about 62% of women with no education had received JSY in LPS compared to 21% in HPS. The coverage of JSY assistance was 38% among the Hindus and 24% among the others. About 65% of the poorest and 28% of the richest women in the LPS received JSY assistance; and this varied between 30% of the poorest and 9% of the richest women in the HPS of India. In LPS, about 73% of mothers who delivered in public health facility had received JSY assistance compared to 30% in HPS. This percentage was very much lower for the mothers who delivered in private health facility because of very few accredited private hospitals provided JSY assistance. For instance only 5.4% and 4.4% of mothers received JSY in private health facility in LPS and HPS respectively.
Table 1.
Percentage of mothers receiving JSY assistance by socio-economic characteristics in India, 2015–16.
| Background characteristics | India |
Low Performing States |
High Performing States |
|||
|---|---|---|---|---|---|---|
| % | N | % | N | % | N | |
| Age of Mother | ||||||
| 15–24 | 36.57 | 19,560 | 54.21 | 16,377 | 21.07 | 4850 |
| 24–35 | 35.9 | 29,785 | 56.37 | 26,803 | 17.42 | 6137 |
| 35 and above | 38.75 | 4548 | 57.34 | 4670 | 13.64 | 550 |
| Place of Residence | ||||||
| Rural | 43.77 | 43,408 | 60.19 | 40,504 | 22.72 | 7979 |
| Urban | 21.39 | 10,484 | 39.49 | 7346 | 13.1 | 3558 |
| Level of Education | ||||||
| No education | 51.38 | 16,450 | 62.39 | 17,554 | 21.97 | 1548 |
| Primary | 44.41 | 8218 | 61.72 | 7579 | 23.3 | 1571 |
| Secondary | 32.92 | 25,163 | 54.55 | 19,700 | 19.02 | 7155 |
| Higher | 19.13 | 4060 | 32.2 | 3017 | 11.6 | 1263 |
| Religion | ||||||
| Hindu | 37.92 | 45,276 | 56.93 | 41,008 | 18.94 | 9152 |
| Muslim | 32.08 | 6786 | 49.19 | 6188 | 15.48 | 1344 |
| Others | 24.01 | 1830 | 50.63 | 654 | 19.67 | 1042 |
| Sex of Head oftheHousehold | ||||||
| Male | 36.11 | 47,182 | 55.71 | 41,807 | 18.34 | 10,157 |
| Female | 38.29 | 6710 | 55.67 | 6042 | 19.99 | 1380 |
| Wealth Quintile | ||||||
| Poorest | 58.83 | 15,337 | 65.45 | 16,707 | 30.48 | 1215 |
| Poorer | 48.28 | 14,335 | 63.44 | 13,418 | 26.48 | 2607 |
| Middle | 36.28 | 11,419 | 56.7 | 8809 | 22.17 | 3334 |
| Richer | 26.36 | 8393 | 46.18 | 5755 | 16.86 | 2932 |
| Richest | 15.14 | 4409 | 28.15 | 3160 | 9.04 | 1449 |
| Pregnancy Complication | ||||||
| No complication | 39.84 | 24,632 | 55.88 | 24,630 | 16.74 | 3426 |
| Any complications | 33.88 | 29,260 | 55.52 | 23,220 | 19.4 | 8111 |
| Place of Delivery | ||||||
| Public | 53.5 | 61,219 | 73.1 | 48,324 | 29.5 | 12,895 |
| Private | 4.7 | 2446 | 5.4 | 1181 | 4.41 | 1265 |
3.2. Variation in contraceptive use, breastfeeding practice and postnatal check-up
Table 2 presents the inter-state variations in contraceptive use, breastfeeding initiation and postnatal check-up of baby among JSY beneficiaries and non-beneficiaries in India in 2015–16. In LPS, the contraceptive use was 41% among JSY beneficiaries compared to 35% among JSY non-beneficiaries. The state pattern was almost similar; higher contraceptive use among JSY beneficiaries compared to JSY non-beneficiary with exception of Uttar Pradesh (38% among JSY vs. 42% among JSY non-beneficiaries). The variation in contraceptive use among JSY beneficiaries and JSY non-beneficiaries was lower in HPS. In the LPS, breastfeeding initiation within one hour was almost double among women receiving JSY assistance compared to JSY non-beneficiaries (58% among JSY beneficiaries and 29.9% among JSY non-beneficiaries). The pattern holds true across states of India. Among the LPS, breastfeeding initiation was highest in Odisha (70.6% among JSY beneficiaries and 62.8% among JSY non-beneficiaries) and lowest in Rajasthan (31.2% among JSY beneficiaries and 24.3% among JSY non-beneficiaries). More than 10% difference in breastfeeding initiation was observed in Chhattisgarh, Jharkhand and Madhya Pradesh among these states among those covered and not covered by JSY assistance.
Table 2.
Percentage of mothers used contraceptive, initiate breastfeeding and had postnatal check-up of baby by JSY coverage in India, 2015–16.
| State | JSY beneficiaries |
JSY non-beneficiaries |
||||||
|---|---|---|---|---|---|---|---|---|
| Using any contraceptive method | Breast feeding within 1 h | Baby's postnatal check-up | N | Using any contraceptive method | Breast feeding within 1 h | Baby's postnatal check-up | N | |
| India | 43.6 | 45.2 | 40.9 | 63,665 | 44.1 | 41.9 | 37.7 | 84,520 |
| Low performing states | 40.5 | 58 | 63 | 49,505 | 35.3 | 29.9 | 33.9 | 36,393 |
| Assam | 61.3 | 63.6 | 44.7 | 4305 | 55 | 56 | 37.4 | 1904 |
| Bihar | 19.5 | 38.4 | 23.9 | 6532 | 14.1 | 32.5 | 20.7 | 4945 |
| Chhattisgarh | 41.1 | 52.5 | 57 | 3278 | 40.7 | 38.3 | 54.1 | 1650 |
| Jammu and Kashmir | 60.6 | 47 | 31.8 | 2967 | 47.8 | 42.4 | 28.4 | 2317 |
| Jharkhand | 31.9 | 41.3 | 38.7 | 2468 | 27 | 29 | 37.9 | 3283 |
| Madhya Pradesh | 41.9 | 39 | 29.1 | 8678 | 33 | 28.5 | 23.8 | 5461 |
| Odisha | 58.2 | 70.6 | 61.6 | 5742 | 48.1 | 62.8 | 46.5 | 1993 |
| Rajasthan | 48.9 | 31.2 | 30.7 | 5852 | 43.7 | 24.3 | 30.8 | 4393 |
| Uttar Pradesh | 38.4 | 32.4 | 38.1 | 9683 | 41.5 | 21.9 | 41.6 | 10,447 |
| Uttarakhand | 45.4 | 33.2 | 33.7 | 1595 | 41.7 | 21.5 | 32 | 1439 |
| High performing states | 52 | 45.7 | 48 | 14,160 | 48.5 | 47.9 | 39.5 | 48,127 |
| Andhra Pradesh | 54.7 | 42.1 | 47.8 | 365 | 50.7 | 39.2 | 37.1 | 1731 |
| Gujarat | 36.2 | 41.1 | 39.1 | 601 | 33.3 | 50.5 | 27.4 | 4499 |
| Haryana | 60.1 | 62 | 54 | 643 | 55.1 | 41.6 | 39.7 | 4144 |
| Karnataka | 33.5 | 61 | 36.4 | 1302 | 35.9 | 53.8 | 26.9 | 4223 |
| Kerala | 46.1 | 62.4 | 56.4 | 440 | 39.2 | 62.8 | 53.7 | 1685 |
| Maharashtra | 53.9 | 66.5 | 56.2 | 600 | 50.6 | 57.5 | 37.9 | 5842 |
| Punjab | 74 | 34.5 | 69.2 | 815 | 71.8 | 28.3 | 56.5 | 3020 |
| Tamil Nadu | 43.8 | 59.5 | 63.6 | 1871 | 41 | 53.7 | 53.3 | 4259 |
| Telangana | 42.5 | 49.1 | 27.4 | 219 | 43.3 | 36 | 32.7 | 1405 |
| West Bengal | 70.7 | 53.3 | 56.8 | 1046 | 72.1 | 41.2 | 48.9 | 2425 |
**Manipur, Mizoram, Meghalaya, Tripura, Himachal Pradesh, Delhi are excluded due to smaller sample size.
In the LPS, postnatal check-up was 63% among JSY beneficiaries compared to 34% among JSY non-beneficiaries. The pattern holds true across all the states with the exception of Uttar Pradesh and Telangana. Among the LPS, it was highest in Odisha (62% among JSY beneficiaries vs. 47% among non-beneficiaries). Bihar had the lowest prevalence of baby's postnatal check-up (23.9% for the JSY beneficiaries and 20.7% among the JSY non-beneficiaries).
Table 3 presents the percentage variation of contraceptive use, breastfeeding initiation and postnatal check-up by JSY coverage and selected social and demographic correlates. The contraceptive use among the JSY beneficiaries and non-beneficiaries did not show much difference across the age groups, place of residence, religion, sex of the head of household, children ever born and pregnancy complications at the last birth. On the other hand, JSY beneficiaries had higher prevalence of initiation of breastfeeding within one hour and postnatal check-up across all socio-demographic strata. However, the contraceptive use has shown positive relation with wealth quintile for both JSY beneficiaries and non-beneficiaries. But in case of breastfeeding and postnatal check-up, no strong relation has been found.
Table 3.
Percentage of mothers using contraception, initiate breastfeeding and having postnatal check-up of baby by JSY and non-JSY beneficiaries in India, 2015–16.
| Variable | JSY beneficiaries |
Non-JSY beneficiaries |
|||||
|---|---|---|---|---|---|---|---|
| Using any contraceptive method | Breast feeding within 1 h | Baby's postnatal check-up | Using any contraceptive method | Breast feeding within 1 h | Baby's postnatal check-up | ||
| Age of Mother | |||||||
| 15–24 | 35.1 | 45.8 | 41.8 | 34.6 | 41.8 | 37.6 | |
| 24–35 | 48.3 | 45.3 | 40.5 | 49.2 | 42.2 | 37.7 | |
| 35 and above | 49.4 | 42.3 | 39.5 | 51.3 | 40.5 | 37.4 | |
| Place of Residence | |||||||
| Rural | 41.9 | 44.8 | 40.8 | 41.1 | 41.3 | 38.7 | |
| Urban | 50.8 | 47 | 41.1 | 48.4 | 42.8 | 36 | |
| Level of Education | |||||||
| No education | 38.6 | 40.5 | 34.9 | 37.1 | 36.3 | 32.4 | |
| Primary | 44.7 | 44.2 | 40.7 | 44.6 | 39.8 | 36.4 | |
| Secondary | 46.2 | 48.7 | 44.5 | 45.6 | 44.5 | 38.9 | |
| Higher | 45.6 | 45.3 | 42.8 | 45.7 | 40.6 | 39.4 | |
| Religion | |||||||
| Hindu | 43.4 | 45.3 | 40.9 | 44.2 | 41.7 | 37.5 | |
| Muslim | 42.2 | 43.4 | 37 | 41 | 41.7 | 36.2 | |
| Others | 53.4 | 50.9 | 54.3 | 50.8 | 45.7 | 42.8 | |
| Caste | |||||||
| SC/ST | 43.7 | 47 | 43.9 | 43.3 | 42.9 | 38.7 | |
| Non SC/ST | 43.6 | 44.2 | 39.1 | 44.4 | 41.6 | 37.2 | |
| Sexof Head of the Household | |||||||
| Male | 45.2 | 45.4 | 41.3 | 45.2 | 41.9 | 37.7 | |
| Female | 32.6 | 44 | 37.9 | 35.9 | 42 | 37.2 | |
| Children ever Born | |||||||
| 1 | 30.6 | 45.5 | 43.6 | 29.6 | 40.3 | 38.2 | |
| 2–3 | 50.9 | 47 | 40.8 | 55.1 | 43.6 | 37.7 | |
| 4 and more | 47 | 39.2 | 35.5 | 47.1 | 39.6 | 34.5 | |
| Wealth Quintile | |||||||
| Poorest | 34.7 | 43.3 | 35.9 | 30.7 | 38.4 | 31.3 | |
| Poorer | 43.6 | 45.1 | 40.1 | 39.4 | 41.7 | 37.1 | |
| Middle | 47.5 | 46.9 | 44.8 | 43.9 | 43.7 | 38.7 | |
| Richer | 48.9 | 46.9 | 44 | 46.1 | 44.2 | 39.2 | |
| Richest | 54.6 | 44.7 | 44.6 | 51.1 | 40 | 38.2 | |
| Pregnancy Complication | |||||||
| No complication | 37.9 | 40.6 | 31.1 | 38.7 | 38.5 | 30.5 | |
| Any complications | 48.4 | 49.1 | 49.1 | 47.6 | 44.2 | 42.3 | |
| Place of delivery | |||||||
| Public | 43.7 | 45.3 | 40.6 | 43.8 | 46.4 | 37.9 | |
| Private | 42.0 | 43.5 | 48.5 | 44.3 | 37.8 | 37.5 | |
3.3. Impact assessment of JSY on contraceptive use, breastfeeding initiation and postnatal check-up of baby in India
Table 4 illustrates the results of propensity matching score to understand the impact of JSY assistance on contraceptive use, breastfeeding initiation and postnatal check-up. It eliminates most of the bias attributable to observable covariates. The differences in the mean outcomes in the matched samples are used to get an estimate of the average treatment effect on the treated cases. Moreover, the raw estimates, i.e. without matching results are measured using unmatched sample estimates. ATT, ATU and ATE present the estimates after matching.
Table 4.
Matching estimates of JSY on contraceptive use, breastfeeding initiation and postnatal check-up of baby among JSY beneficiaries and non-beneficiaries in India, 2015–16.
| Dependent Variables | Sample | India |
LPS |
HPS |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treated | Controls | Difference | S.E. | t-statistic | Treated | Controls | Difference | S.E. | T-stat | Treated | Controls | Difference | S.E. | T-stat | ||
| Contraceptive use | Unmatched | 0.4425 | 0.4093 | 0.0333 | 0.003 | 12.83 | 0.4399 | 0.3785 | 0.0614 | 0.003 | 18.1 | 0.4512 | 0.4324 | 0.0188 | 0.005 | 3.96 |
| ATT | 0.4425 | 0.3856 | 0.0568 | 0.033 | 1.73 | 0.4399 | 0.2795 | 0.1604 | 0.036 | 4.48 | 0.4512 | 0.4964 | 0.0452 | 0.030 | −1.49 | |
| ATU | 0.4093 | 0.4705 | 0.0612 | . | . | 0.3785 | 0.4576 | 0.0791 | . | . | 0.4324 | 0.4402 | 0.0078 | . | . | |
| ATE | 0.0308 | . | . | 0.1260 | . | . | 0.0427 | . | . | |||||||
| Breast feeding initiation within 1 h | Unmatched | 0.4683 | 0.4082 | 0.0600 | 0.003 | 23.13 | 0.4446 | 0.3121 | 0.1325 | 0.003 | 39.72 | 0.5513 | 0.4810 | 0.0703 | 0.005 | 14.74 |
| ATT | 0.4683 | 0.4089 | 0.0594 | 0.034 | 1.75 | 0.4446 | 0.3732 | 0.0713 | 0.036 | 1.99 | 0.5513 | 0.4559 | 0.0954 | 0.031 | 3.09 | |
| ATU | 0.4082 | 0.4925 | 0.0842 | 0.3121 | 0.4091 | 0.0970 | . | . | 0.4810 | 0.4981 | 0.0171 | . | . | |||
| ATE | 0.0735 | 0.0822 | . | . | 0.0349 | . | . | |||||||||
| Baby postnatal check-up | Unmatched | 0.4001 | 0.3596 | 0.0412 | 0.003 | 16.19 | 0.3865 | 0.3496 | 0.0369 | 0.003 | 11.07 | 0.4505 | 0.3671 | 0.0834 | 0.005 | 17.94 |
| ATT | 0.4007 | 0.3404 | 0.0604 | 0.033 | 1.86 | 0.3865 | 0.3266 | 0.0599 | 0.035 | 1.69 | 0.4505 | 0.3746 | 0.0759 | 0.029 | 2.6 | |
| ATU | 0.3596 | 0.3893 | 0.0298 | 0.3496 | 0.4038 | 0.0542 | . | . | 0.3671 | 0.4595 | 0.0924 | . | . | |||
| ATE | 0.0429 | 0.0575 | . | . | 0.0487 | . | . | |||||||||
The unmatched sample estimates revealed that before matching the JSY beneficiaries in India had 3% higher chance of using contraception than the JSY non-beneficiaries. The ATT value of treated and control groups were 0.443 and 0.385 respectively which suggests that mothers who received JSY assistance if they would not have received it, then only 38% mothers used contraception. This pattern was similar for LPS, but for HPS the difference in ATT was very low than LPS. ATU value shows that mothers who did not receive JSY assistance would have received the benefit; their chances of using contraception would have increased up to 6%. This increment is higher in LPS than HPS (7% in LPS vs. 0.7% in HPS). The ATE for contraceptive use was 3%. This indicates that the average treatment effect of JSY on contraceptive use. ATE was much higher in LPS (12%) compared to HPS (4%). Similarly, in case of breastfeeding practice, the difference of ATT between treated and control was 5%. It was higher in HPS (9%) compared to LPS (7%). ATU follows reverse pattern of higher difference in LPS compare to HPS (9% in LPS vs. 1% in HPS). For breastfeeding, ATE was 8% in LPS and 3% in HPS. ATE for postnatal check-up was 4% which shows positive impact of JSY on postnatal check-up.
3.3.1. Verification of the estimates of PSM analysis
Table 5 shows the mean value of each matching variables before and after matching for both treated and control groups. Also, the table represents percentage bias reduction after matching and t-test for the differences between matched pairs. The percentage bias reduction was varied from 70.8% for sex of the head of the households to 100% for education level of mother, wealth quintile and place of delivery. It was found that mean difference became insignificant after matching for almost all covariates, i.e. covariates were sufficiently balanced.
Table 5.
Covariate balance check and absolute bias reduction, India, 2015–16.
| Variable | Mean |
t-test |
|||||
|---|---|---|---|---|---|---|---|
| Sample | Treated | Control | % bias | % reduction bias | t | p > t | |
| Age of Mother | U | 1.7503 | 1.7559 | −0.9 | −1.73 | 0.083 | |
| M | 1.7503 | 1.7493 | 0.2 | 81.4 | 0.30 | 0.763 | |
| Level of Education | U | 1.3304 | 1.7073 | −39.0 | −74.49 | 0.000 | |
| M | 1.3304 | 1.3304 | 0.0 | 100.0 | 0.00 | 0.998 | |
| Pregnancy Complication | U | 0.5557 | 0.5853 | −6.0 | −11.41 | 0.000 | |
| M | 0.5557 | 0.5559 | 0.0 | 99.3 | −0.08 | 0.937 | |
| Religion | U | 1.2928 | 1.3922 | −15.3 | −28.79 | 0.000 | |
| M | 1.2928 | 1.2924 | 0.1 | 99.6 | 0.12 | 0.904 | |
| Caste | U | 0.6017 | 0.6859 | −17.7 | −33.77 | 0.000 | |
| M | 0.6017 | 0.6026 | −0.2 | 99.0 | −0.32 | 0.748 | |
| Wealth Quintile | U | 2.5171 | 3.3341 | −62.3 | −118.26 | 0.000 | |
| M | 2.5171 | 2.5174 | 0.0 | 100.0 | −0.04 | 0.968 | |
| Place of Residence | U | 1.8087 | 1.6447 | 37.4 | 70.39 | 0.000 | |
| M | 1.8087 | 1.8092 | −0.1 | 99.7 | −0.24 | 0.814 | |
| Sex of Head ofHousehold | U | 1.1176 | 1.121 | −1.0 | −1.99 | 0.047 | |
| M | 1.1176 | 1.1167 | 0.3 | 70.8 | 0.55 | 0.583 | |
| Place ofDelivery | U | 1.0384 | 1.4747 | −115.3 | −209.1 | 0.000 | |
| M | 1.0834 | 1.0384 | 0.0 | 100.0 | 0.0 | 1.000 | |
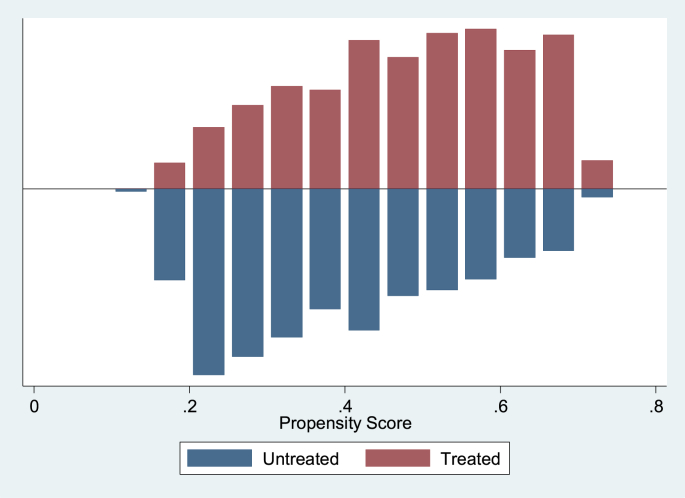
Fig. 3 represents the quality of the matching by the distribution of the propensity scores for women who had received JSY benefits. Treated women with propensity score were above the line and controlled women were below the line. From the figure, it can be said that the distributions are almost identical for treated and control groups after propensity score matching. The common support assumption has been confirmed by the existence of a substantial overlap between the characteristics of treated and controlled women.
Fig. 3.
Predicted probability of JSY assistance: matched sample, India, 2015–16.
Result from logistic regression in Table 6 also supports the fact that odds of using contraception, breastfeeding within 1 h of delivery and postnatal check-up were higher for the mothers who had received JSY assistance. Although, both PSM and regression analysis serves the purpose of removing confounders and adjusting for imbalances between the groups, here, regression model captures the gaps in odds of unintended effects with JSY beneficiaries and other socio-economic correlates. Moreover, it serves as robustness check of the PSM model.
Table 6.
Odds ratio (OR) and 95% Confidence Interval (CI) of Contraceptive use, Breastfeeding Practice and Postnatal Check-up with JSY assistance and other socio-economic correlates in India, 2015–16.
| Using any contraceptive method |
Breastfeeding within 1 h |
Postnatal check-up |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| JSY received | ||||||
| No | ||||||
| Yes | 1.30*** | 1.26, 1.33 | 1.12*** | 1.10,1.15 | 1.28*** | 1.25,1.31 |
| Age of mother | ||||||
| 15–24 | ||||||
| 24–35 | 1.86*** | 1.81,1.90 | 1.08*** | 1.06,1.11 | 1.01 | 0.98,1.03 |
| 35 and above | 2.08*** | 2.00,2.16 | 1.12*** | 1.07,1.16 | 0.99 | 0.95,1.03 |
| Level of Education | ||||||
| No education | ||||||
| Primary | 1.16*** | 1.12,1.21 | 1.14*** | 1.10,1.18 | 1.15*** | 1.11,1.19 |
| Secondary | 1.08*** | 1.04,1.11 | 1.40*** | 1.36,1.44 | 1.15*** | 1.11,1.18 |
| Higher | 0.87*** | 0.83,0.91 | 1.29*** | 1.24,1.35 | 1.13*** | 1.08,1.18 |
| Religion | ||||||
| Hindu | ||||||
| Muslim | 0.87*** | 0.85,0.90 | 0.99 | 0.96,1.02 | 0.90*** | 0.87,0.93 |
| Others | 0.73*** | 0.70,0.76 | 1.36*** | 1.31,1.41 | 0.77*** | 0.74,0.80 |
| Caste | ||||||
| SC/ST | ||||||
| Non SC/ST | 1.05*** | 1.02,1.08 | 0.91*** | 0.89,0.93 | 0.91*** | 0.89,0.93 |
| Wealth quintile | ||||||
| Poorest | ||||||
| Poorer | 1.34*** | 1.30,1.39 | 1.03* | 0.99,1.06 | 1.05** | 1.01,1.08 |
| Middle | 1.54*** | 1.49,1.60 | 1.01 | 0.97,1.05 | 1.12*** | 1.08,1.16 |
| Richer | 1.67*** | 1.60,1.74 | 0.96* | 0.92,1.01 | 1.14*** | 1.10,1.19 |
| Richest | 2.22*** | 2.12,2.32 | 0.81*** | 0.77,0.84 | 1.26*** | 1.20,1.32 |
| Place of residence | ||||||
| Urban | ||||||
| Rural | 0.97** | 0.94,0.99 | 0.94*** | 0.91,0.96 | 1.22*** | 1.19,1.26 |
| Sex of the head of the household | ||||||
| Male | ||||||
| Female | 0.64*** | 0.62,0.66 | 1.01 | 0.98,1.04 | 0.98 | 0.94,1.01 |
| Place of delivery | ||||||
| Public | ||||||
| Private | 0.96** | 0.93,0.98 | 0.70*** | 0.69,0.72 | 1.10*** | 1.07,1.13 |
| Constant | 0.24*** | 0.23,0.26 | 0.58*** | 0.55,0.60 | 0.28*** | 0.26,0.29 |
*p = <.1, **p < .05, ***p < .01.
4. Discussion
The primary objective of JSY in India was to increase the facility based delivery through financial incentives. It was initially launched in low performing states and was extended to all states and union territories of India over time. Besides its direct outcome, it also provides an opportunity to examine the unintended consequences of the financial incentives on closely inter-wined yet non-incentivised behaviours of women. Beyond the primary objective of increasing facility based delivery, this paper is essentially examined the positive externalities of JSY induced facility based delivery, namely, contraception use, breastfeeding practice and postnatal check-up in India. All these variables are important component of reproductive health and helpful in improving the health of mothers and children. The salient findings of this study are as follows:
First, the inter-state variation in receiving JSY assistance was prominent. It was higher in the low performing states compared to high performing states of India. Over half of the women in the states of Bihar, Jammu & Kashmir, Rajasthan, Madhya Pradesh, Assam, Chhattisgarh, Odisha received JSY assistance while it was less than 10% in Gujarat, Maharashtra, Goa. The socio-economic distribution of JSY coverage also suggested that it was higher in rural, among uneducated mothers, mothers with higher parity and mothers belonging to poor households at the national level as well as in the low performing states. Second, the state variations in outcome variables such as contraceptive use, breastfeeding initiation and postnatal check-up varied widely across the LPS and HPS. The states such as Odisha, Chhattisgarh and Assam with the highest prevalence of JSY coverage performed better not only than the other LPS but better than many HPS. For example, the JSY beneficiaries in the LPS had higher contraceptive prevalence than Gujarat, Maharashtra and Telangana where around less than 15 percent of the women were covered under the JSY scheme. The breastfeeding initiation after delivery in Odisha (68.1%) was one of the highest in India after Goa (70.3%) and Mizoram (70%). Besides some of the LPS having low postnatal coverage, quite a few states with lower JSY coverage also had low prevalence of postnatal coverage. Third, all three outcome variables were higher among JSY beneficiaries compared to non-beneficiaries in LPS. However, states such as Bihar and Uttar Pradesh among the LPS had lower prevalence of contraceptive use, breastfeeding initiation and postnatal check-up. Fourth, results from propensity score matching suggested that the JSY has significantly contributed to the increase use of contraceptive, initiation of breastfeeding within 1 h and have postnatal check-up done that their other counterpart controlling for socio-economic characteristics. Though both the LPS and HPS had benefitted from the JSY assistance, the unintended effects were more prominent in the LPS. We found that women who were covered under the JSY scheme in LPS had 12% higher chance to adopt contraception compared to those not covered. The pattern was similar but of lower magnitude in HPS. Similarly, in case of breastfeeding, the JSY recipients in the LPS had 8% higher chances of initiating breastfeeding within 1 h compared to 3% in HPS. When the impact of JSY assistance on postnatal care was examined, we found that JSY beneficiaries were 6% and 5% more likely to opt for postnatal check-up in LPS and HPS respectively. Fifth, logistic results support the findings that after controlling the selected socio-economic factors, the odds of the outcome variables are higher for the mothers who had received JSY assistance.
Here, we provide some plausible explanations for the above findings. The financial incentive received through JSY probably motivated the mothers to avail the facility based delivery and that in turn has positive externalities on outcome variables. In the absence of JSY, the institutional delivery would have been lower than what we observed and would have also lowered these three outcome variables. The higher unintended effects in the LPS could be explained by the fact that the advanced states have already achieved better health facilities and better maternal and child indicators compared to the LPS. Thus, receiving JSY provides an impetus to them to avail reproductive health care utilization. Earlier studies have demonstrated that fertility is amenable to change in the face of conditional cash transfer (Morris et al., 2004; Stecklov et al., 2006). Our findings suggest that receiving JSY is having a modest and stronger effect in the uptake of contraception in the LPS than the HPS could be validated by the fact that fertility is much lower in the HPS. It has been documented in the literature that during pregnancy, women are most amenable to being convinced to use services that are favourable to them and their children (Agha & Carton, 2011). The increased interaction of the JSY beneficiaries with the health system, specifically ASHA workers, might elevate the likelihood of up-taking better health decisions, particularly in the early postpartum period (Carvalho et al., 2014). This is reflected in the early initiation of breastfeeding among women. Seeking medical assistance following delivery could impart knowledge to women for the benefits of receiving child immunization (Anichukwu & Asamoah, 2019). Moreover, certain studies have revealed that the roles played by the ASHAs have a large impact on receiving JSY and thereby adhering to the better health decisions. The availability of contraception should be universal along with the method choices. The promotion of modern spacing methods among first time mothers is recommended along with the early implementation of JSY was understandably prioritized in the LPS.
Following the success of JSY, the next step could be strengthening it beyond the states and focus on the low performing districts. The unintended effects shown in this paper may be larger than those observed when JSY finally reaches to all the districts of India. Furthermore, demand side financial incentive further needs supply side in place and, therefore, efforts may be taken to enhance and strengthen the prevailing infrastructure to intensify the quality of obstetric care available to women in the health facilities. This should include improvements in staff behaviour, improved interpersonal communications, availability of skilled staffs and supply of essential drugs and equipment (Ahmed and Khan, 2011). Earlier studies have suggested that the implementation of JSY has led to increased workload and thereby degrading quality of obstetric care especially in the low performing states have been observed (Devadasan et al., 2008; Lahariya, 2009). Expanding the cash incentives for receiving institutional delivery in the private health facilities through public-private partnerships could reduce the loads from the public health centers alone.
5. Conclusion
Receipt of cash assistance for institutional delivery through cash transfer programme resulted in an increased subsequent use of contraceptives, initiation of breastfeeding and postnatal check-ups. Besides improving the existing health infrastructure with special emphasis being laid on the low performing states, the continuation of conditional cash transfer programme for maternal care is highly recommended.
Ethical approval
Ethical approval is not required; the study used secondary data from cross-sectional survey.
Data sharing
The data used in this study is available at: https://dhsprogram.com/data/available-datasets.cfm, which can be downloaded after request from DHS website.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial or non-for-profit sectors.
CRediT authorship contribution statement
Soumendu Sen: Conceptualization, Formal analysis, Writing - original draft, Writing - review & editing. Sayantani Chatterjee: Formal analysis, Writing - original draft, Writing - review & editing. Pijush Kanti Khan: Formal analysis, Writing - review & editing. Sanjay K. Mohanty: Conceptualization, Writing - review & editing, Supervision.
Declaration of competing interest
The authors declare that they have no competing interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100619.
Contributor Information
Soumendu Sen, Email: sen.soumendu16@gmail.com.
Sayantani Chatterjee, Email: 612sayantani@gmail.com.
Pijush Kanti Khan, Email: pijush.pkk@gmail.com.
Sanjay K. Mohanty, Email: sanjayiips@yahoo.co.in.
Appendix.
A. State differentials in contraceptive use, breastfeeding practice and postnatal check-up of baby in India, 2015–2016.
| Using any method of contraceptives | Breastfeeding within 1 h | Postnatal check-up of new-born | N | |
|---|---|---|---|---|
| India | 42.6 | 41.4 | 37 | 148,746 |
| Low performing states | 36.5 | 34.9 | 32.8 | 72,559 |
| Assam | 57.3 | 61.3 | 38.8 | 6223 |
| Bihar | 16.3 | 34.1 | 20.1 | 11,525 |
| Chhattisgarh | 40.8 | 46.5 | 53.7 | 4936 |
| Jammu and Kashmir | 53 | 45.6 | 28.6 | 5310 |
| Jharkhand | 27.2 | 32.2 | 33.6 | 5783 |
| Madhya Pradesh | 37.8 | 33.9 | 26.2 | 14,186 |
| Odisha | 55.2 | 68.1 | 57.6 | 7777 |
| Rajasthan | 46.5 | 28.1 | 28.6 | 10,273 |
| Uttar Pradesh | 39 | 24.9 | 36.2 | 3051 |
| Uttarakhand | 42.6 | 27.3 | 30.4 | 3495 |
| High performing states | 49.3 | 48.6 | 41.7 | 59,447 |
| Andaman and Nicobar Islands | 37.3 | NA | NA | 503 |
| Andhra Pradesh | 51.3 | 39.9 | 40.1 | 2100 |
| Arunachal Pradesh | 28 | 55.6 | 32.9 | 2085 |
| Chandigarh | 73.8 | 31.5 | 54.2 | 138 |
| Dadra and Nagar Haveli | 24.3 | NA | NA | 218 |
| Daman and Diu | 17.5 | NA | NA | 301 |
| Delhi | 52.4 | 26.9 | 28.2 | 1126 |
| Goa | 23.1 | 70.3 | 53.2 | 342 |
| Gujarat | 33.3 | 49.1 | 29.4 | 5122 |
| Haryana | 52.7 | 42.3 | 39 | 4792 |
| Himachal Pradesh | 44.5 | 40.9 | 44.3 | 1775 |
| Karnataka | 36.1 | 55 | 28.6 | 5555 |
| Kerala | 40.5 | 62.7 | 54.3 | 2126 |
| Lakshadweep | 35.5 | NA | NA | 260 |
| Maharashtra | 51 | 57.9 | 39.7 | 6451 |
| Manipur | 25.9 | 64.1 | 17.2 | 3034 |
| Meghalaya | 19.7 | 61.4 | 36.4 | 1774 |
| Mizoram | 30.3 | 70 | 26.6 | 2887 |
| Nagaland | 20.2 | 52.6 | 4.1 | 1081 |
| Puducherry | 46.9 | 64.5 | 57.9 | 876 |
| Punjab | 72.1 | 30.1 | 58.3 | 3835 |
| Sikkim | 36.6 | NA | NA | 856 |
| Tamil Nadu | 41.8 | 55.2 | 56.2 | 6136 |
| Telangana | 43.6 | 36.8 | 32.5 | 1637 |
| Tripura | 65.1 | 43.3 | 14.7 | 942 |
| West Bengal | 70.3 | 45.4 | 50.8 | 3495 |
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Agha S., Carton T.W. Determinants of institutional delivery in rural Jhang, Pakistan. International Journal for Equity in Health. 2011;10(1):31. doi: 10.1186/1475-9276-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S., Khan M.M. Is demand-side financing equity enhancing? Lessons from a maternal health voucher scheme in Bangladesh. Social Science & Medicine. 2011;72(10):1704–1710. doi: 10.1016/j.socscimed.2011.03.031. [DOI] [PubMed] [Google Scholar]
- Anichukwu O.I., Asamoah B.O. The impact of maternal health care utilisation on routine immunisation coverage of children in Nigeria: A cross-sectional study. BMJ open. 2019;9(6) doi: 10.1136/bmjopen-2018-026324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babalola S., Vonrasek C. Communication, ideation and contraceptive use in Burkina Faso: An application of the propensity score matching method. BMJ Sexual & Reproductive Health. 2005;31(3):207–212. doi: 10.1783/1471189054484022. [DOI] [PubMed] [Google Scholar]
- Barber S.L., Gertler P.J. Empowering women to obtain high quality care: Evidence from an evaluation of Mexico's conditional cash transfer programme. Health Policy and Planning. 2008;24(1):18–25. doi: 10.1093/heapol/czn039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta Z.A., Chopra M., Axelson H., Berman P., Boerma T., Bryce J., de Francisco A. Countdown to 2015 decade report (2000–10): Taking stock of maternal, newborn, and child survival. Lancet. 2010;375(9730):2032–2044. doi: 10.1016/S0140-6736(10)60678-2. [DOI] [PubMed] [Google Scholar]
- Carvalho N., Thacker N., Gupta S.S., Salomon J.A. More evidence on the impact of India's conditional cash transfer program, Janani Suraksha Yojana: Quasi-experimental evaluation of the effects on childhood immunization and other reproductive and child health outcomes. PloS One. 2014;9(10) doi: 10.1371/journal.pone.0109311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das Gupta M. Death clustering, mothers' education and the determinants of child mortality in rural Punjab, India. Population Studies. 1990;44(3):489–505. [Google Scholar]
- De Brauw A., Hoddinott J. Must conditional cash transfer programs be conditioned to be effective? The impact of conditioning transfers on school enrollment in Mexico. Journal of Development Economics. 2011;96(2):359–370. [Google Scholar]
- Devadasan N., Elias M.A., John D., Grahacharya S., Ralte L. 2008. A conditional cash assistance programme for promoting institutional deliveries among the poor in India: Process evaluation results. Reducing financial barriers to obstetric care in low-income countries. [Google Scholar]
- Diaz J.J., Handa S. An assessment of propensity score matching as a nonexperimental impact estimator evidence from Mexico's PROGRESA program. Journal of Human Resources. 2006;41(2):319–345. [Google Scholar]
- Dixit P., Dwivedi L.K., Ram F. Strategies to improve child immunization via antenatal care visits in India: A propensity score matching analysis. PloS One. 2013;8(6) doi: 10.1371/journal.pone.0066175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do M.P., Kincaid D.L. Impact of an entertainment-education television drama on health knowledge and behavior in Bangladesh: An application of propensity score matching. Journal of Health Communication. 2006;11(3):301–325. doi: 10.1080/10810730600614045. [DOI] [PubMed] [Google Scholar]
- Ensor T., Chhun C., Kimsun T., McPake B., Edoka I. Impact of health financing policies in Cambodia: A 20 year experience. Social Science & Medicine. 2017;177:118–126. doi: 10.1016/j.socscimed.2017.01.034. [DOI] [PubMed] [Google Scholar]
- Gopalan S.S., Varatharajan D. Addressing maternal healthcare through demand side financial incentives: Experience of Janani Suraksha Yojana program in India. BMC Health Services Research. 2012;12(1):319. doi: 10.1186/1472-6963-12-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S.K., Pal D.K., Tiwari R., Garg R., Sarawagi R. Assessment of Janani Suraksha Yojana (JSY)–in jabalpur, Madhya Pradesh: Knowledge, attitude and utilization pattern of beneficiaries: A descriptive study. International Journal of Current Biological and Medical Science. 2011;1(2):6–11. [Google Scholar]
- Goli S., Doshi R., Perianayagam A. Pathways of economic inequalities in maternal and child health in urban India: A decomposition analysis. PloS One. 2013;8(3) doi: 10.1371/journal.pone.0058573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govil D., Purohit N., Gupta S.D., Mohanty S.K. Out-of-pocket expenditure on prenatal and natal care post Janani Suraksha Yojana: A case from Rajasthan, India. Journal of Health, Population and Nutrition. 2016;35(1):15. doi: 10.1186/s41043-016-0051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan M.C., Foreman K.J., Naghavi M., Ahn S.Y., Wang M., Makela S.M., Murray C.J. Maternal mortality for 181 countries, 1980–2008: A systematic analysis of progress towards Millennium development goal 5. Lancet. 2010;375(9726):1609–1623. doi: 10.1016/S0140-6736(10)60518-1. [DOI] [PubMed] [Google Scholar]
- International Institute for Population Sciences (Iips) and Icf . IIPS; Mumbai: 2017. National family health survey (NFHS-4), 2015-16: India. [Google Scholar]
- Kumar V., Misra S.K., Kaushal S.K., Gupta S.C., Maroof K.A. Janani Suraksha Yojana: Its utilization and perception among mothers and health care providers in a rural area of North India. International Journal of Medicine and Public Health. 2015;5(2) [Google Scholar]
- Kuwawenaruwa A., Mtei G., Baraka J., Tani K. Implementing demand side targeting mechanisms for maternal and child health-experiences from national health insurance fund program in Rungwe District, Tanzania. Globalization and Health. 2016;12(1):41. doi: 10.1186/s12992-016-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lechner M. Program heterogeneity and propensity score matching: An application to the evaluation of active labor market policies. The Review of Economics and Statistics. 2002;84(2):205–220. [Google Scholar]
- Lim S.S., Dandona L., Hoisington J.A., James S.L., Hogan M.C., Gakidou E. India's Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: An impact evaluation. The Lancet. 2010;375(9730):2009–2023. doi: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- Liu L., Oza S., Hogan D., Chu Y., Perin J., Zhu J., Black R.E. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the sustainable development Goals. The Lancet. 2016;388(10063):3027–3035. doi: 10.1016/S0140-6736(16)31593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensah J., Oppong J.R., Schmidt C.M. Ghana's National Health Insurance Scheme in the context of the health MDGs: An empirical evaluation using propensity score matching. Health Economics. 2010;19(S1):95–106. doi: 10.1002/hec.1633. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Family Welfare (MoHFW) Government of India; New Delhi: 2018. Annual report of department of health and family welfare 2017-18. [Google Scholar]
- Mohanty S.K., Srivastava A. Out-of-pocket expenditure on institutional delivery in India. Health Policy and Planning. 2012;28(3):247–262. doi: 10.1093/heapol/czs057. [DOI] [PubMed] [Google Scholar]
- Montgomery A.L., Ram U., Kumar R., Jha P., Million Death Study Collaborators Maternal mortality in India: Causes and healthcare service use based on a nationally representative survey. PloS One. 2014;9(1) doi: 10.1371/journal.pone.0083331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris S.S., Flores R., Olinto P., Medina J.M. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: Cluster randomised trial. The Lancet. 2004;364(9450):2030–2037. doi: 10.1016/S0140-6736(04)17515-6. [DOI] [PubMed] [Google Scholar]
- Mukherjee S., Singh A. Has the Janani Suraksha Yojana (a conditional maternity benefit transferscheme) succeeded in reducing the economic burden of maternity in rural India? Evidence from theVaranasi district of Uttar Pradesh. Journal of Public Health Research. 2018;7(1) doi: 10.4081/jphr.2018.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukhopadhyay D.K., Mukhopadhyay S., Mallik S., Nayak S., Biswas A.K., Biswas A.B. Astudy on utilization of Janani Suraksha Yojana and its association with institutional delivery in the stateof West Bengal, India. Indian Journal of Public Health. 2016;60(2):118. doi: 10.4103/0019-557X.184543. [DOI] [PubMed] [Google Scholar]
- Nandi A., Laxminarayan R. The unintended effects of cash transfers on fertility: Evidence from the safe motherhood scheme in India. Journal of Population Economics. 2016;29(2):457–491. [Google Scholar]
- Ng M., Misra A., Diwan V., Agnani M., Levin-Rector A., De Costa A. An assessment of the impact of the JSY cash transfer program on maternal mortality reduction in Madhya Pradesh, India. Global Health Action. 2014;7(1):24939. doi: 10.3402/gha.v7.24939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Registrar General of India (Orgi) Vol. 2018. Statistical Report; New Delhi: 2018. (Sample registration system). [Google Scholar]
- Powell-Jackson T., Hanson K. Financial incentives for maternal health: Impact of a national programme in Nepal. Journal of Health Economics. 2012;31(1):271–284. doi: 10.1016/j.jhealeco.2011.10.010. [DOI] [PubMed] [Google Scholar]
- Powell-Jackson T., Mazumdar S., Mills A. Financial incentives in health: New evidence from India's Janani Suraksha Yojana. Journal of Health Economics. 2015;43:154–169. doi: 10.1016/j.jhealeco.2015.07.001. [DOI] [PubMed] [Google Scholar]
- Pufahl A., Weiss C.R. Evaluating the effects of farm programmes: Results from propensity score matching. European Review of Agricultural Economics. 2009;36(1):79–101. [Google Scholar]
- Rahman M.M., Pallikadavath S. How much do conditional cash transfers increase the utilization of maternal and child health care services? New evidence from Janani Suraksha Yojana in India. Economics and Human Biology. 2018;31:164–183. doi: 10.1016/j.ehb.2018.08.007. [DOI] [PubMed] [Google Scholar]
- Rosenbaum P.R., Rubin D.B. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. The American Statistician. 1985;39(1):33–38. [Google Scholar]
- Rubin D.B., Thomas N. Matching using estimated propensity scores: Relating theory to practice. Biometrics. 1996:249–264. [PubMed] [Google Scholar]
- Sachdeva S., Malik J.S. Assessment of maternal and child health (MCH) practices with a focus on Janani Suraksh Yojana (JSY) Global Journal of Medicine and Public Health. 2012;1(6) [Google Scholar]
- Sengupta N., Sinha A. Is India's safe motherhood scheme leading to better child health care practices? Global Social Welfare. 2018;5(1):49–58. [Google Scholar]
- Sharma M.P., Soni S.C., Bhattacharya M., Datta U., Gupta S., Nandan D. An assessment of institutional deliveries under JSY at different levels of health care in Jaipur District, Rajasthan. Indian Journal of Public Health. 2009;53(3):177–182. [PubMed] [Google Scholar]
- Sidney K., Tolhurst R., Jehan K., Diwan V., Costa A. “The money is important but all womenanyway go to hospital for childbirth nowadays”-a qualitative exploration of why women participate in aconditional cash transfer program to promote institutional deliveries in Madhya Pradesh, India. BMC Pregnancy and Childbirth. 2016;16(1):47. doi: 10.1186/s12884-016-0834-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A., Padmadas S.S., Mishra U.S., Pallikadavath S., Johnson F.A., Matthews Z. Socio-economic inequalities in the use of postnatal care in India. PloS One. 2012;7(5) doi: 10.1371/journal.pone.0037037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skiles M.P., Curtis S.L., Basinga P., Angeles G., Thirumurthy H. The effect of performance-based financing on illness, care-seeking and treatment among children: An impact evaluation in Rwanda. BMC Health Services Research. 2015;15(1):375. doi: 10.1186/s12913-015-1033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza J.P., Tunçalp Ö., Vogel J.P., Bohren M., Widmer M., Oladapo O.T.…Temmerman M. Obstetric transition: The pathway towards ending preventable maternal deaths. BJOG: An International Journal of Obstetrics and Gynaecology. 2014;121:1–4. doi: 10.1111/1471-0528.12735. [DOI] [PubMed] [Google Scholar]
- Stecklov G., Winters P., Todd J., Regalia F. American University: Washington DC Department of Economics Working Paper Series; 2006. Demographic externalities from poverty programs in developing countries: Experimental evidence from Latin America. 2006-1. [Google Scholar]
- Thongkong N., Van de Poel E., Roy S.S., Rath S., Houweling T.A.J. How equitable is the uptake of conditional cash transfers for maternity care in India? Evidence from the Janani Suraksha Yojana scheme in Odisha and Jharkhand. International Journal for Equity in Health. 2017;16(1):48. doi: 10.1186/s12939-017-0539-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unfpa N.D. 2009. Concurrent assessment of Janani Suraksha yojna (JSY) in selected states of India. 2008. [Google Scholar]
- World Health Organization . 2005. The world health report: 2005: Make every mother and child count. [Google Scholar]
- Yang L., Sun L., Wen L., Zhang H., Li C., Hanson K., Fang H. Financing strategies to improve essential public health equalization and its effects in China. International Journal for Equity in Health. 2016;15(1):194. doi: 10.1186/s12939-016-0482-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanovitzky I., Zanutto E., Hornik R. Estimating causal effects of public health education campaigns using propensity score methodology. Evaluation and Program Planning. 2005;28(2):209–220. [Google Scholar]
- You D., Wardlaw T., Salama P., Jones G. Levels and trends in under-5 mortality, 1990–2008. The Lancet. 2010;375(9709):100–103. doi: 10.1016/S0140-6736(09)61601-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.