Abstract
The recent outbreak of 2019 coronavirus disease (COVID-19), caused by a novel coronavirus, has now spread quickly worldwide. Like the severe acute respiratory syndrome coronavirus (SARS-CoV), this novel type of coronavirus, SARS-CoV-2, has been demonstrated to utilize angiotensin-converting enzyme 2 (ACE2) as an entry point to the cells. There is a growing body of reports indicating that COVID-19 patients, especially those in severe condition, exhibit neurological symptoms, thus supporting the possibility that SARS-CoV-2 could infect and damage neurons within the central nervous system in humans. Using human pluripotent stem cells-derived neurons, here we show the expression of ACE2 in human neurons via immunocytochemistry. From this perspective, we elaborate on the idea that the neuro-invasive potential of SARS-CoV-2 should be considered as a possible contributory factor, as well as a therapeutic target, for the severe respiratory symptoms in critical COVID-19 cases.
Keywords: COVID-19, SARS-CoV-2, ACE2, Central nervous system, Neurons
In late December of 2019, clustering pneumonia cases caused by unknown etiology were firstly reported in the city of Wuhan, China. As of June 18th, the COVID-19 pandemic has spread in 213 countries and regions, with 8.5 million confirmed cases and 450,000 deaths. After ruling out SARS-CoV (Severe Acute Respiratory Syndrome coronavirus) and MERS-CoV (Middle East Respiratory Syndrome coronavirus), COVID-19 was later identified to be caused by a novel coronavirus, SARS-CoV-2 (Lu et al. 2020). Due to the invasiveness of this virus to the respiratory system, symptoms of COVID-19 include coughing, high temperature, shortness of breath, and notably, loss of smell, which suggests possible infection of neurons (Giacomelli et al. 2020; Yan et al. 2020). Indeed, according to a recent study (Mao et al. 2020), SARS-CoV-2 exhibits neuro-invasive potential in COVID-19 patients, especially those in severe condition. Among the 214 cases of this study, 36.4% of the total patients were reported to have displayed neurological symptoms, meaning that 1 in 3 cases has involvement of the central nervous system (CNS).
Similar to SARS-CoV, which caused the SARS epidemic in 2002–2003, SARS-CoV-2 also binds to angiotensin-converting enzyme 2 (ACE2) in the lung to enter pulmonary cells, via its S1 spike protein (Wan et al. 2020), yet the S protein of SARS-CoV-2 exhibits higher affinity to ACE2 (Wrapp et al. 2020). ACE2 was originally discovered in 2000 in cardiac tissue and now has been established as a major component of the regulatory renin-angiotensin system (RAS) (Donoghue et al. 2000). In mammals, the RNA expression of ACE2 has been reported in multiple organs and variety of cell types. An early work has showed that the ACE2 expression in humans is mainly in the gastrointestinal (GI) system, heart, and the kidney (Harmer et al. 2002). Also, the data reported on “The Human Protein Atlas” (https://www.proteinatlas.org) indicate very little expression of ACE2 RNA in the CNS. However, the enzymatic activity of ACE2 has already been detected in human brain tissues and cerebrospinal fluid (CSF) (Kehoe et al. 2016; Xu et al. 2017), indicating its significant level of protein expression within the human CNS.
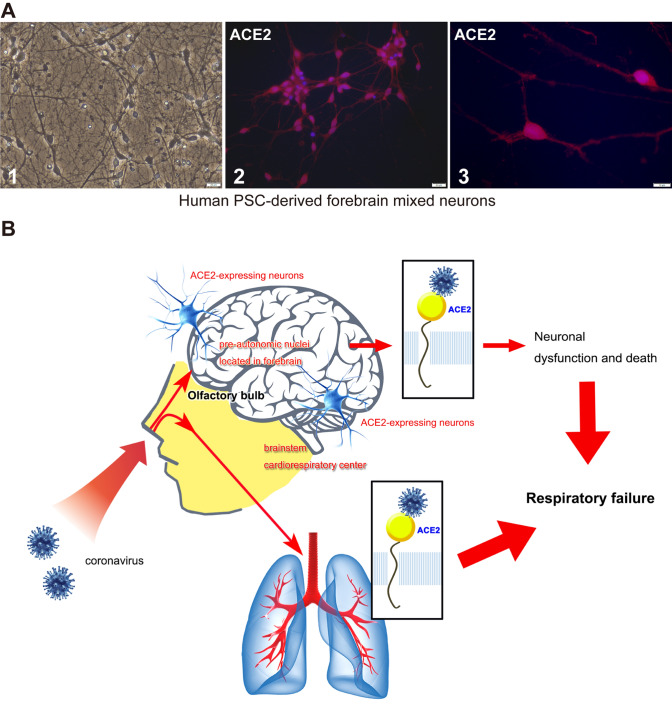
In human pluripotent stem cells (PSC)-derived mixed neurons, we have identified ACE2 expression via immunocytochemistry (Fig. 1a). The human neurons used here were generated from human PSC-derived neuronal precursor cells, and composed of a mixed population of forebrain-type (FOXG1-positive) neurons that are highly pure and functional. Similar to what we previously observed in mice (Doobay et al. 2007), ACE2 is robustly expressed in the cell body of the neurons, with less expression in the axons and dendrites. Although it is not human brain tissue, our data still provide evidence that ACE2 protein is expressed in human neurons, which is, consequently, a highly possible target for SARS-CoV-2 infection. So far, most of the known coronaviruses are neurotropic. For example, human coronavirus OC43 can propagate from neuron to neuron through axonal transportation (Dube et al. 2018). In mice, we have shown expression of ACE2 in neurons located in various pre-autonomic regions, such as the subfornical organ (SFO), paraventricular nucleus of hypothalamus (PVN), solitary tract (NTS), dorsal motor nucleus of the vagus nerve (DMNX), and the rostral ventrolateral medulla (RVLM) (Xia and Lazartigues 2010). Therefore, if the same pattern of ACE2 expression applies to humans, the SARS-CoV-2 infection in such neurons could contribute to the respiratory failure observed in the severe cases of COVID-19 (Fig. 1b): some patients were not gasping for air, despite their dangerously low blood oxygen levels. Indeed, SARS-CoV has been reported to infect the brain from both patients and experimental animals (Gu et al. 2005; Netland et al. 2008). In human ACE2 knock-in mice, SARS-CoV infection was significantly detected in the areas that involves cardiorespiratory regulation, including both hypothalamus and brainstem (Netland et al. 2008). Moreover, autopsy studies from the SARS patients revealed that SARS-CoV resides nearly exclusively in the neurons (Xu et al. 2005), rather than in other cell types, matching what we know about the expression profile of ACE2 within the CNS.
Fig. 1.
ACE2 expresses in human neurons, therefore COVID-19 virus could invade the CNS, causing neurological symptoms and respiratory failure. (a) ACE2 expresses in cultured human pluripotent stem cell (PSC)-derived mixed neurons. A1: A bright field image of cultured human PSC-derived neurons (STEMCELL, 70905, Canada). The scale bar represents 20 μm. A2–3: Immunofluorescent labeling for visualization of ACE2 (red) in cultured human PSC-derived neurons (blue: DAPI). The scale bars represent 20 μm in (A2) and 10 μm in (A3), respectively. The specimens were incubated with rabbit anti-mouse ACE2 antibody (1:100 dilution; Aviva System Biology, OASG00144, CA, USA) overnight at 4 ºC. (b) A schematic of how neuronal ACE2 could contribute to coronavirus-related respiratory diseases
ACE2 is a cell surface-bound enzyme and can be secreted via ectodomain shedding. Whether the secreted ACE2 (i.e., shed) can be bound by the S1 protein is still unknown, there is a possibility that it may compete with the membrane-bound ACE2 for potential virus binding. In a correspondence by Batlle et al., the application of recombinant soluble ACE2 was discussed as a possible therapeutic approach for treating COVID-19 to avoid severe infection (Batlle et al. 2020). We previously reported markedly higher level of secreted ACE2 in the CSF of patients with uncontrolled hypertension (Xu et al. 2017), however, whether this increased ACE2 ectodomain shedding will affect the infection and mortality rates of hypertensive patients in the COVID-19 epidemic is still beyond investigation. Membrane-bound ACE2 also undergoes internalization. In ACE2-transfected Neuro-2A cells exposed to angiotensin-II, activation of the octapeptide receptor (AT1) was found to induce the internalization of ACE2 and its degradation into lysosomes (Deshotels et al. 2014). Since coronaviruses utilize ACE2 as a means to enter the cell, ACE2 internalization could also be related to the process of coronavirus infection. From this perspective, hypertensive patients, who have an overactive systemic or central RAS, might be more susceptible to SARS-CoV-2 infection and under higher risk of transforming into severe cases. However, the usage of ACE inhibitors and AT1 receptor blockers is currently controversial, for their potentials in raising ACE2 levels, and the consequential possibility that the patients, who are treated with those anti-hypertensive drugs, might be more susceptible to SARS-CoV-2 infection (Table 1).
Table 1.
Reported expression of ACE2 protein in human tissues and the corresponding COVID-19 symptoms
| Tissue name | ACE2 protein expression | ACE2 protein expression levels | Related COVID-19 symptoms |
|---|---|---|---|
| Duodenum | ✓ | High | GI disturbance |
| Gallbladder | ✓ | High | NA |
| Heart | ✓ | High | Heart injury |
| Kidney | ✓ | High | Kidney injury |
| Small intestines | ✓ | High | Diarrhea and other GI disturbance |
| Testis | ✓ | High | NA |
| Adrenal gland | ✓ | Medium | NA |
| Colon | ✓ | Medium | Diarrhea |
| Rectum | ✓ | Medium | NA |
| Brain | ✓ (validated via enzymatic activity assays) | Low | Loss of taste or smell, respiratory failure, and other neurological symptoms |
| Liver | ✓ | Low | Increased levels of liver enzymes (ALT, AST) |
| Lung | ✓ | Low | Pneumonia and respiratory symptoms |
| Oral mucosa | ✓ | Low | NA |
| Seminal vesicle | Only in glandular cells | Low | NA |
| Skin | ✓ | Low | A rash on skin, or discoloration of fingers or toes |
| Spleen | Only in vascular and red pulp sinus endothelium | Low | NA |
| Eye | NA | NA | Conjunctivitis |
| Adipose tissue | × | ||
| Common blood cells | × | Abnormal blood clotting | |
| Endometrium | × | ||
| Esophagus | × | ||
| Nasopharynx | × | ||
| Stomach | × |
The data of ACE2 protein expression were obtained via published reports (Hamming et al. 2004; Kehoe et al. 2016; Xu et al. 2017; Hikmet et al. 2020) and version 19 of the Human Protein Atlas (https://www.proteinatlas.org). The data of related COVID-19 symptoms were obtained via the website of Centers for Disease Control and Prevention (CDC)
“✓”: yes; “×”: no; NA: data are currently not available
So far, there have been several theories regarding how SARS-CoV-2 invades the CNS. It was recently reported in Italy that about 34% of COVID-19 patients exhibited olfactory and/or taste disorders (Giacomelli et al. 2020). According to a study posted on medRxiv, both SARS-CoV-2 and ACE2 RNAs were detected in the nasal epithelial cells in COVID-19 patients (Wu et al. 2020), confirming that SARS-CoV-2 did infect olfactory epithelium. Considering that intranasal drug delivery is able to bypass the blood–brain barrier (BBB) (Duchi et al. 2013), it is possible that SARS-CoV-2 could infect the brain through olfactory nerves located in the nasal cavity, like other neurotropic coronaviruses (Perlman et al. 1989). Additionally, in severe cases of COVID-19, hyperactivity of the immune system may trigger a "cytokine storm" (Savarin and Bergmann 2018), characterized by over-activation of immune cells and cytokine release, therefore contributing to a breakdown of the BBB and neuronal damage. Besides the nasal cavity and the BBB, there is another speculation, raised from previous studies on SARS-CoV, that the coronavirus could spread to the brainstem directly through mechanoreceptors and chemoreceptors located in the lung and the lower respiratory tract (Hadziefendic and Haxhiu 1999). Although there has been a growing body of studies revealing the pathological characteristics of SARS-CoV-2 (Natoli et al. 2020), the hypothesis proposed above still need to be validated in COVID-19 cases or animal models.
The expression of ACE2 in human neurons brings up the neuro-invasive potential of SARS-CoV-2 and the possibility that infected neurons could affect the patient’s ability to breathe and deteriorate respiratory function. This suggests that respiratory failure in severe COVID-19 cases might be treated from the perspective of the CNS.
Funding
This project was supported in part by Xi’an Jiaotong University (TX6J007 to JX), the department of Veterans Affairs (BX004294 to EL) and the Research Enhancement Program at LSUHSC-NO (to EL).
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jiaxi Xu, Email: xujiaxi@xjtu.edu.cn.
Eric Lazartigues, Email: elazar@lsuhsc.edu.
References
- Batlle D, Wysocki J, Satchell K. Soluble angiotensin-converting enzyme 2: a potential approach for coronavirus infection therapy? Clin Sci. 2020;134(5):543–545. doi: 10.1042/CS20200163. [DOI] [PubMed] [Google Scholar]
- Deshotels MR, Xia H, Sriramula S, Lazartigues E, Filipeanu CM. Angiotensin II mediates angiotensin converting enzyme type 2 internalization and degradation through an angiotensin II type I receptor-dependent mechanism. Hypertension. 2014;64(6):1368–1375. doi: 10.1161/HYPERTENSIONAHA.114.03743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, Donovan M, Woolf B, Robison K, Jeyaseelan R, Breitbart RE, Acton S. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9. Circ Res. 2000;87(5):E1–9. doi: 10.1161/01.res.87.5.e1. [DOI] [PubMed] [Google Scholar]
- Doobay MF, Talman LS, Obr TD, Tian X, Davisson RL, Lazartigues E. Differential expression of neuronal ACE2 in transgenic mice with overexpression of the brain renin-angiotensin system. Am J Physiol Regul Integr Comp Physiol. 2007;292(1):R373–381. doi: 10.1152/ajpregu.00292.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube M, Le Coupanec A, Wong AHM, Rini JM, Desforges M, Talbot PJ. Axonal transport enables neuron-to-neuron propagation of human coronavirus OC43. J Virol. 2018 doi: 10.1128/JVI.00404-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duchi S, Ovadia H, Touitou E. Nasal administration of drugs as a new non-invasive strategy for efficient treatment of multiple sclerosis. J Neuroimmunol. 2013;258(1–2):32–40. doi: 10.1016/j.jneuroim.2013.02.013. [DOI] [PubMed] [Google Scholar]
- Giacomelli A, Pezzati L, Conti F, Bernacchia D, Siano M, Oreni L, Rusconi S, Gervasoni C, Ridolfo AL, Rizzardini G, Antinori S, Galli M. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu J, Gong E, Zhang B, Zheng J, Gao Z, Zhong Y, Zou W, Zhan J, Wang S, Xie Z, Zhuang H, Wu B, Zhong H, Shao H, Fang W, Gao D, Pei F, Li X, He Z, Xu D, Shi X, Anderson VM, Leong AS. Multiple organ infection and the pathogenesis of SARS. J Exp Med. 2005;202(3):415–424. doi: 10.1084/jem.20050828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadziefendic S, Haxhiu MA. CNS innervation of vagal preganglionic neurons controlling peripheral airways: a transneuronal labeling study using pseudorabies virus. J Auton Nerv Syst. 1999;76(2–3):135–145. doi: 10.1016/s0165-1838(99)00020-x. [DOI] [PubMed] [Google Scholar]
- Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmer D, Gilbert M, Borman R, Clark KL. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532(1–2):107–110. doi: 10.1016/s0014-5793(02)03640-2. [DOI] [PubMed] [Google Scholar]
- Hikmet F, Méar L, Uhlén M, Lindskog C. The protein expression profile of ACE2 in human tissues. bioRxiv. 2020 doi: 10.1101/2020.03.31.016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehoe PG, Wong S, Al Mulhim N, Palmer LE, Miners JS. Angiotensin-converting enzyme 2 is reduced in Alzheimer's disease in association with increasing amyloid-beta and tau pathology. Alzheimer Res Ther. 2016;8(1):50. doi: 10.1186/s13195-016-0217-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natoli S, Oliveira V, Calabresi P, Maia LF, Pisani A. Does SARS-Cov-2 invade the brain. Translational lessons from animal models. Eur J Neurol. 2020 doi: 10.1111/ene.14277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82(15):7264–7275. doi: 10.1128/JVI.00737-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman S, Jacobsen G, Afifi A. Spread of a neurotropic murine coronavirus into the CNS via the trigeminal and olfactory nerves. Virology. 1989;170(2):556–560. doi: 10.1016/0042-6822(89)90446-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savarin C, Bergmann CC. Fine tuning the cytokine storm by IFN and IL-10 following neurotropic coronavirus encephalomyelitis. Front Immunol. 2018;9:3022. doi: 10.3389/fimmu.2018.03022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020 doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS, McLellan JS. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C, Zheng S, Chen Y, Zheng M. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov, in the nasal tissue. MedRxiv. 2020 doi: 10.1101/2020.02.11.20022228. [DOI] [Google Scholar]
- Xia H, Lazartigues E. Angiotensin-converting enzyme 2: central regulator for cardiovascular function. Curr Hypertens Rep. 2010;12(3):170–175. doi: 10.1007/s11906-010-0105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J, Zhong S, Liu J, Li L, Li Y, Wu X, Li Z, Deng P, Zhang J, Zhong N, Ding Y, Jiang Y. Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clin Infect Dis. 2005;41(8):1089–1096. doi: 10.1086/444461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J, Sriramula S, Xia H, Moreno-Walton L, Culicchia F, Domenig O, Poglitsch M, Lazartigues E. Clinical relevance and role of neuronal AT1 receptors in ADAM17-mediated ACE2 shedding in neurogenic hypertension. Circ Res. 2017;121(1):43–55. doi: 10.1161/CIRCRESAHA.116.310509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS. Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol. 2020 doi: 10.1002/alr.22579. [DOI] [PMC free article] [PubMed] [Google Scholar]