Abstract
The global healthcare landscape has changed dramatically and rapidly in 2020. This has had an impact upon paediatricians and in particular respiratory paediatricians. The effects in Europe, with its mature healthcare system, have been far faster and greater than most authorities anticipated. Within six weeks of COVID-19 being declared a public health emergency by the World Health Organisation [WHO] in China, Europe had become the new epicentre of disease. A pandemic was finally declared by the WHO on March 11th 2020. Continued international travel combined with the slow response of some political leaders and a variable focus on economic rather than health consequences resulted in varying containment strategies in response to the threat of the initial wave of the pandemic. It is likely that this variation has contributed to widely differing outcomes across Europe. Common to all countries was the stark lack of preparations and initial poor co-ordination of responses between levels of government to this unforeseen but not unheralded global health crisis. In this article we highlight the impact of the first wave of the COVID-19 pandemic in Italy, Austria, Germany, and the United Kingdom.
Keywords: COVID-19, SARS-CoV-2, Pandemic, Co-ordination, Resource allocation
Introduction
On the 30th January 2020, the World Health Organization (WHO) declared the outbreak of Coronavirus in China a public health emergency. On the 28th February 2020, as more countries reported their first cases, the WHO raised the global risk level for the disease from “high” to “very high”, expressing serious concerns on the infection’s spread. By the 11th March 2020, the WHO declared the worldwide spread of Coronavirus disease and spoke for the first time of “pandemic”. Just two days later, Europe became the new epicentre of the Coronavirus pandemic. Shortly thereafter, Italy, Spain, and United Kingdom would become the European countries with the greatest local transmission.
Italian experience
Italian demographic data
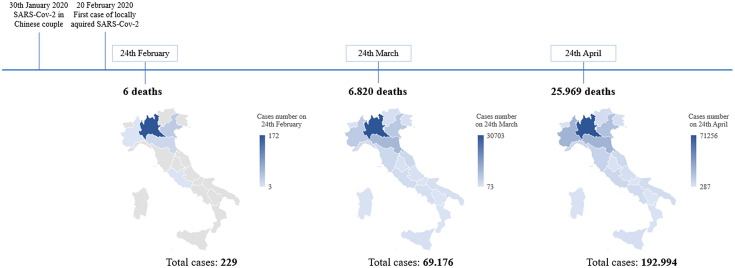
On the 30th January 2020, Italian health officials of the Spallanzani Institute, in Rome, made the first diagnosis of SARS-Coronavirus (SARS-CoV-2) infection in two Chinese tourists with a travel history to Wuhan. On the 20th February 2020, the first case of locally acquired SARS-CoV-2 (COVID-19) infection was diagnosed in Codogno, a Northern Italian village, where a young man with no clear epidemiological link was hospitalized in a critical condition. In the next four days, the number of cases increased rapidly in Northern Italian regions with three major clusters around the cities of Codogno, Bergamo and Cremona in the Lombardia region [1]. By 24th February the number of infected people reached 229 (Lombardia 172, Veneto 33, Emilia-Romagna 18, Piemonte 3, Lazio 3) with six deaths and 1 recovered [2].
Following this, the community spread of infection was rapid, with devastating consequences. Exactly one month later, 69,176 confirmed cases of SARS-CoV-2 were reported nationwide, and 6820 related deaths [3]. By March 24th 2020 all of the Italian regions reported at least one locally acquired case of Covid-19. The incidence variability was related to the local transmission rate that was highest in Northern Italy, with limited but increasing outbreaks in Central-Southern Italy [4].
Despite the containment measures and lockdown ordered by the Italian Government, the numbers of infected people progressively increased, reaching 192,994 cases in late April, two months after the infection’s outbreak in Italy (Fig. 1 ). The spread of infection was accompanied by a growing number of deaths, reaching 31,017 on May 20th 2020 [5].
Fig. 1.
Timeline of spread infection in Italian regions.
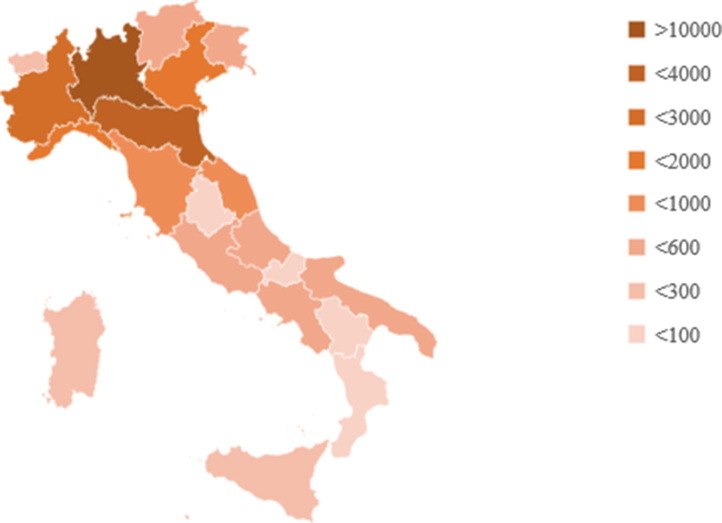
Lombardy and Emilia-Romagna were the most affected regions, followed by Piemonte, Veneto and Liguria (Fig. 2 ).
Fig. 2.
Italian distribution of confirmed SARS-CoV-2 deaths.
Age and sex appear to be the most important prognostic indicators. The most severely affected patients were male (60.9%) at a mean age of 80 years (median 81, range 0–100). Only 312 out of the 27,955 (1.1%) positive SARS-CoV-2 patients under the age of 50 died. Of those who died, 59.9% had 3 or more comorbidities, and cardiovascular diseases were the most common pre-existing conditions [5], [6].
The Italian National Institute of Statistics recorded 25,354 deaths in the period from 20th February to 31th March; an increase of 39% over the numbers reported in the same quarters between 2015 and 2019. Just over half of notified deaths were documented to have SARS-CoV-2 with 6866 of eight thousand Italian Municipalities included in this analysis [7].
Unofficial data in children were more reassuring, as children were less affected by severe disease [8]. Until May 14th, 4922 SARS-CoV-2 infected children, age 0–18 years, were reported, accounting for about 2.2% of total cases. Among 4050 cases where data were available, 13.7% were under 1 year, 17.5% between 2 and 6 years, and 68.8% over 7 years. Just 3.3% of all paediatric cases required hospitalization and, by age group, children aged under 1 year were most frequently hospitalized. Only three children who had serious pre-existing diseases died [9].
Italian authorities’ response to the pandemic
In response to the outbreak of SARS-CoV-2, the Italian government suspended all China flights from 30th January and declared a state of emergency one day later. Public health and social measures to slow or stop the spread of COVID-19 were initially considered in some “red areas” of Northern Italy. Finally, lockdown and social distancing were extended nationwide until May 3 [10].
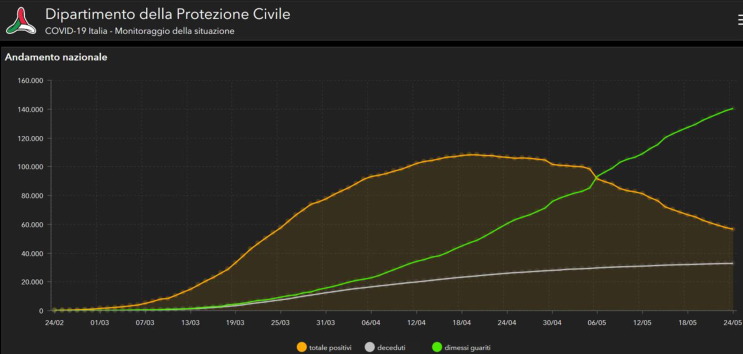
Despite these restrictions, the number of new cases continued to increase (Fig. 3 ) and patients with severe acute respiratory syndrome (SARS) due to COVID-19 presented a severe challenge to the national healthcare system. The Italian Government authorised regions to recruit 20,000 health workers, allocating €660 million for the purpose; the Italian Civil Protection undertook a fast-track public procurement to secure ventilators, additional protective masks, and SARS-CoV-2 tests [11]. To address this emergency, each Italian region had to re-organize activities to increase the number of ICU beds and to address the healthcare workers and the medical equipment shortage. Elective surgeries were postponed to free beds and offer human and material resources. Non-urgent outpatient visits and private practices were suspended, while medical evaluations for pregnant women, cancer patients, and fragile or unstable patients continued as before.
Fig. 3.
Italian national trend of new positives, healed patients and deaths in the last three months (data updated to 24 May 2020). http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1. Yellow line: total positives; green line: discharged and healed patients; gray line: deaths.
Healthcare workers not directly involved in the emergency were redeployed. They joined COVID-19 Internal Medicine, Respiratory and Infectious Disease Departments, as well as Emergency Departments, often with gruelling 12-h shifts. General practitioners modified their practice of delivering care, mostly through telephone calls or telehealth [12].
As people avoided hospitals during the Coronavirus crisis, Emergency Department visits across Italian hospitals were down, but the number of late-presenting, serious cases increased. Control visits for patients with chronic medical complexity, both adults and children, were postponed, increasing the unease of their families. To face this situation, healthcare workers added telehealth monitoring visits to their already extraordinary activity.
Lessons to be learned from the Italian experience
The worldwide scientific community and healthcare systems were caught unprepared by the sudden SARS-CoV-2 pandemic. Italy was the first European country that had to deal with this. Under the Italian constitution, the Italian Ministry of Health controls the distribution of public financing and secures for free the “essential levels of care” (Livelli Essenziali di Assistenza, or LEA) to all residents in every region. However, recent changes in Italian health policy had decreased the number of beds and healthcare workers; undermining the stability of the health system. In addition, the recent greater autonomy of individual regions accentuated inequalities in the quality of services available.
Accordingly, the first challenge was a thorough re-organization of the healthcare infrastructure, where many units were re-purposed to provide services solely dedicated to the COVID-19 emergency, while others continued to provide primary care. As well, the territorial health care systems were unprepared; with an insufficient supply of personal protective equipment (PPE), inadequate discussion and coordination with health departments and institutions, lack of diagnostic tests, and insufficient training. To meet these needs, private financing and the Italian government allocated €3.5 billion to support the Italian healthcare system in order to increase the number of beds in intensive care units, infectious diseases, and respiratory units, to augment medical and nursing staff through new staff hiring and to purchase medical material and equipment.
Collaboration between regions made it possible to decant overcrowded hospital ICUs and to perform nasopharyngeal swab testing in regions where the tests were not easily available. Despite these efforts, the number of affected people exceeded the capabilities of the workforce deployed. Italian healthcare workers paid a very high price with more than 26,746 confirmed cases [13], 163 clinicians and 40 nurses succumbing to COVID-19, and many more suffering with burnout.
The Austria/Germany perspectives
The pandemic cases
The early establishment of contact restrictions led to a moderate increase of SARS-CoV-2 infected cases in Austria (1854 tested positive per million inhabitants) and Germany (2159 tested positive per million inhabitants, data as of May 22nd) with decreasing numbers of new cases per day since late March (Austria) and early April (Germany), respectively. Capacities of healthcare institutions including ICUs were never threatened in both countries. In contrast to other countries, where big cities such as Paris, London, Madrid, and New York were the most affected areas, more rural areas were affected early and more intensely in Austria (skiing areas in the Tyrol and Salzburg) and Germany (in Bavaria and Baden-Württemberg).
Reported paediatric cases (patients <15 years of age) represent 3.3% (5814 of 177,212) and 2.9% (467 of 16,360) of all registered cases in Germany (population of 83 millions) and Austria (population of 8.8 millions), respectively. Hospitalised paediatric cases are registered by paediatric societies in both countries. Only a minority of paediatric patients were hospitalised (Germany, n = 196; Austria, n = 16, 3.4% of paediatric cases, each), very few required intensive care treatment (Germany, n = 19; Austria, n = 2, both with SARS-CoV-2 associated hyperinflammatory conditions), and one child died (Germany) (data as of May 22nd).
The precautions in response to the pandemic
In Austria and Germany, restrictions for public life were imposed early on. In Austria, by March 10th indoor events with >100 and outdoor events with >500 attenders were banned, and universities closed. This was followed by a partial lockdown on March 16th comprising closure of all shops except those providing basic supplies such as groceries and pharmacies, and closure of restaurants, day care centres and schools. Lockdown measures included strict and monitored regulations with regard to leaving home. This was only allowed for going to work (if necessary), running errands, helping other people, and going for a walk alone or with members of the same household. Outside the home individuals were expected to keep at least 1 metre distance between themselves and other people during all activities.
In Germany, almost identical regulations were implemented in the same periods of time. The early implementation of these restrictions was followed by a delayed and initially moderate increase of infections. In this phase, the healthcare systems prepared for the emergence of numerous SARS-CoV-2 infected patients.
As both Austria and Germany are federal republics, instructions for testing, taking precautions in the healthcare system and managing SARS-CoV-2 infected patients differed from federal state to federal state, and sometimes even from region to region, despite (new) federal laws regarding an epidemic, and advice from authorized and highly acknowledged entities such as the Robert Koch Institute.
The response in hospitals
All hospitals and other healthcare institutions were obliged to identify patients with proven or suspected SARS-CoV-2 infections by triage systems. Specific hospitals, and specific departments (including paediatric departments), wards and intensive care units (including PICUs), were designated and prepared for caring for COVID-19 cases.
In Germany and Austria whilst some ‘non-acute’ medical departments such as dermatology and ophthalmology were designated for the management of COVID-19 cases, no paediatric departments were repurposed nor were paediatricians redeployed for attending adult patients. Non-emergency appointments and elective surgical procedures were universally cancelled to increase capacity for the pandemic.
In common with many other countries, emergency visits and paediatric admissions decreased significantly for at least two reasons: (1) In contrast to the pre-pandemic era, parents sought hospital contact only when their children had more severe medical problems, and (2) social distancing not only resulted in a limited spread of SARS-CoV-2, but also of other pathogens causing acute diseases or exacerbations of chronic respiratory diseases. Staff presence in the hospitals was reduced, and whenever possible teams were divided into two groups to avoid virus transmissions.
In addition, visiting bans were established and strictly controlled in many hospitals and nursing homes. Exceptions were only made for children, palliative care and dying patients, again with regional differences. For children, often only one reference person (resulting in usually fathers not being allowed to see their children for prolonged periods of time) or one visiting person per day and patient was allowed. In many hospitals, fathers were also not allowed to enter delivery rooms. All these precautions were already taken before the peak of infections was reached.
Particularly during the early phase, a shortage of personal protective equipment (PPE) occurred. Therefore, FFP2 and FFP3 masks were sterilised and reused. In some institutions and even more among paediatric practitioners, self-made masks were used. Furthermore, test capacities were also limited in the early phase. As a consequence, restrictive and non-homogenous guidelines for when and in whom tests should be performed were established and occasionally modified. Comprehensive testing for health care personal was not routinely and universally performed.
Opportunities and threats associated with the pandemic
The pandemic has resulted in a more intense collaboration between paediatric institutions, paediatric and adult services, specialists in infectious diseases, pneumologists, and intensivists; and also within professional societies in both countries [14]. Similar to other countries, telemedicine has been more widely applied during the pandemic, and will probably become standard practice in some areas. On the other hand, coming along with significantly decreased paediatric emergency visits, outpatients in general, and hospital admissions the significance and relative importance of paediatrics in general and paediatric respiratory medicine in particular might be questioned by hospital administrations.
The United Kingdom: Is it the sick man of Europe?
By the 5th May 2020, the UK had overtaken Italy, as the worst affected country in Europe, with almost 30,000 deaths attributed to COVID-19 (and one month later over 40,000 deaths). In common with other countries, children appear to have been mildly affected in most instances. The precise clinical picture is still emerging but despite a well-established and admired universal healthcare system (the National Health Service) the mortality has been higher than its neighbours.
It became apparent early in the course of the pandemic that children would be likely to be less severely affected and this resulted in a very significant reorganisation of care across the National Health Service (NHS). However, a small number of children have presented far later than expected and a new condition, Paediatric Inflammatory Multisystem Syndrome – Temporally associated with SARS-CoV-2 pandemic (PIMS-TS) has emerged [15]. Some children have had associated circulatory shock requiring PICU, a serious issue considering the reduced PICU capacity since some have been converted into AICUs for adult patients with COVID-19.
Response to the pandemic: reorganisation of care in the UK
For paediatricians this reorganisation resulted in the centralisation of paediatric services with the complete closure of some paediatric departments in major (e.g. London and Birmingham). In many centres, paediatricians were redeployed to adult services and adult intensive care units.
Fortunately, this redeployment was associated with a very significant fall in paediatric admissions over the same period. This initial relief was quickly followed by a realisation that children and families were, in many instances, too frightened to attend hospital or their general practitioner. This led to the launch of a position statement from the Royal College of Paediatrics and Child Health (RCPCH) on the 3rd April 2020 regarding delayed access to care for children during COVID-19 [16].
The RCPCH also provided guidance for planning paediatric staffing and rotas. This specifically recommended reducing the number of staff per shift but having more senior availability in the hospital to support decision making. Coupled with a marked reduction in referrals from primary care and the difficulty in providing safe, face-to-face outpatient reviews led to a significant change in patterns of working for paediatricians. The most generally reported experience is that the hours for most paediatricians have been much longer but work intensity and patient numbers have reduced significantly.
Infection issues
One of the biggest challenges which arose in the early phases of the pandemic in the UK was a shortage of personal protective equipment (PPE). The situation was complicated by the lack of a single voice on what was required, and by whom. Individual organisations and professional groups issued their own, often contradictory advice to those issued by Public Health England (PHE) [17]. In general, these tended to suggest that higher levels of PPE were required by their own members and this inevitably led to confusion and distress amongst healthcare professionals.
Much time, effort and intellectual energy was consumed on defining what was (and what was not) an aerosol generating procedure. This led to concern from families about the safety of nebulisation of drugs and non-invasive ventilation in the home, including safety of professional carers. Shortages of PPE, coupled with the deaths of healthcare workers, led to national headlines. Hopefully, greater consensus will be achieved about the relative risks of different procedures and patient groups in the coming months, which will allow us to adequately plan the purchase, provision and distribution of PPE to meet the needs of healthcare professionals.
In the classic British style of ‘make do and mend’ originating with the clothing shortages in the Second World War, many hospitals have made their own PPE. For example, at the Royal Brompton Hospital, the engineering department produced plastic face shields whilst fashion students sat in the local Town Hall and made PPE gowns.
Shielding advice
On 22nd March 2020 the UK government announced a recommendation that those who may be at increased risk of severe illness from COVID-19, due to significant underlying conditions, should be shielded. This guidance is updated regularly [18]. Shielding, known in some countries as cocooning, meant the person was to stay indoors at home for 12 weeks with further restrictions within the home. As is often the case, this seemed quite orientated to adult patients. As regards respiratory conditions, initial definitions of ‘clinically extremely vulnerable’ were brief, and there was particular difficulty with defining which asthmatic patients needed to shield. There was inconsistency between information sources for the public (for example NICE and Asthma UK), and definitions kept changing. There were also many omissions from the government recommendations, for example children with interstitial lung disease, bronchiectasis etc. The British Paediatric Respiratory Society [BPRS] produced a consensus list (Table 1 ).
Table 1.
Initial BPRS guidance on which patients should shield.
|
|
|
|
|
|
|
|
|
|
|
|
Fragmented communication and blurred lines of responsibility
At the start, the government stated that 1.5 million people would receive a letter telling them if they needed to shield, within 7 days, starting in 2 days’ time. How they came up with that figure is uncertain, but data was being taken from primary care systems. Contact was haphazard missing out some patients who should be shielding and sending unnecessary advice to others who clearly should not. Lists of who had received the shielding letter were eventually sent to tertiary units and they were able to identify patients from clinic lists and databases and advise accordingly. Whilst shielding has been helpful for some families, for example, allowing priority for supermarket home delivery, it has caused problems and financial hardship when parents/carers need to go out to work. In May, the BPRS made new recommendations to RCPCH and thus on to Public Health England, which were defining those needing mandatory shielding versus those with diseases in which decisions could be made on a case by case basis. It was recommended that the changes be made at the end of the initial shielding period that was due to finish at the end of June. Then suddenly the politicians announced on a Saturday evening (May 30th) with no prior warning, nor seemingly any consultation with the specialist groups, that shielding could stop now, in that all vulnerable people could now go outside once a day, and if they lived alone could meet someone from a different household. Inevitably this resulted in confusion and anxiety amongst patients and families.
Production of guidelines
Since the pandemic, there has been a deluge of guidelines. The UK based National Institute for Health and Care Excellence (NICE) usually takes 18–24 months to produce a guideline and 11–13 months for short clinical guidelines. During the Pandemic their COVID-19 rapid guidelines have been produced in 1–2 weeks. Royal Colleges, Specialist Societies and Charities/Family Support groups have also put guidance on their websites. Most relevant to respiratory paediatrics are the NICE guidelines on severe asthma [19] and cystic fibrosis (CF) [20]. Inevitably, much of these NICE guidelines is generic and not too detailed, but at a time when staff were being redeployed from paediatric to adult COVID work, and paediatric wards were being closed down, it was important to state that specialist CF units should retain in-patient services and that sufficient clinical expertise (i.e., the multidisciplinary team) remain within the CF teams.
What have we gained from the pandemic in the UK?
There have been some aspects of the enforced changes in the delivery of health care as a result of the pandemic that have been beneficial to patients and the National Health Service (NHS). Telemedicine has taken a remarkable leap forward. It has been used in some units, for example in adult CF care, over the last few years, both via telephone and video conferencing. With the shutdown of face to face clinics, telephone and video clinics have become standard practice, and seem to work well. In CF care, this has been carried out in conjunction with respiratory samples sent in from home, home spirometry and weighing, and medication sent in the post to patients.
CF families have been intent on avoiding cross infection for many years, and it is likely that telemedicine and home monitoring will be increasingly used post-pandemic. Another bonus is summed up by a recent teenager with CF who said he was doing his physiotherapy now as “there is nothing else to do”.
An unexpected consequence of the pandemic has been an increased focus on the self-management of chronic respiratory conditions. Some of the complacency seen in management of common conditions like asthma, was replaced with real concern amongst adults and children. Remarkably, inhaled beclomethasone for asthma became temporarily unavailable in the UK, partly as a supply problem with patient stockpiling, but perhaps also patients were actually taking it!
There has been incredible team bonding within many departments as everyone pulls together in a crisis; and also, between paediatric and adult services, as paediatricians have supported adult intensive care. Even more so, there has been overwhelming respect and gratitude from the British public towards NHS staff, with gifts and discounts offered by many, and the weekly ‘Clap for Carers’ event. Perhaps there will be less complaints going forward when a patient waits half an hour to be seen in clinic!
Common ground across Europe
Much has been endured during the first wave of the COVID-19 pandemic. Similar challenges have been met with heartening resolve by so many in the healthcare sector and for this we should be thankful and have the wisdom to be better prepared for future health crises (Table 2 ). Whilst many low-middle income countries are currently facing the onslaught of COVID-19, those from first world countries in Europe and the United Kingdom can offer financial support, advice from similar lessons learnt and a sense of co-operative responsibility as we await the promise of a vaccine.
Table 2.
For future pandemics we must:
|
|
|
|
|
|
|
Educational aims
The reader will come to appreciate that:
-
•
Under-preparedness for a pandemic was evident in all European countries.
-
•
Diverging disease trajectories occurred with children comprising <4% of reported cases.
-
•
Poor co-ordination between federal, state and regional jurisdictions was common.
-
•
In the worst affected countries paediatric resources were redeployed to support adult patients.
Directions for future research
-
•
Establish and assess the effectiveness of better protocols for centralised distribution of national resources, such as personal protective equipment, in response to future pandemics.
-
•
Determine the relative effectiveness of strategies of hand hygiene, wearing of masks, physical distancing and school closures on the disease trajectory in pandemics.
-
•
Using economic modelling, assess the cost benefits to all countries of improved funding to international organisations such as the World Health Organisation to monitor, intervene and co-ordinate the response to pandemics.
References
- 1.Cereda D, Tirani M, Rovida F, Demicheli V, Ajelli M, Poletti P, et al. The early phase of the COVID-19 outbreak in Lombardy, Italy. ArXiv200309320 Q-Bio [Internet]. 20 Mar 2020; Available at: http://arxiv.org/abs/2003.09320.
- 2.http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4098 (Accessed 9th June 2020).
- 3.http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4310 (Accessed 9th June 2020).
- 4.http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4596 (Accessed 9th June 2020).
- 5.https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_20-maggio-2020.pdf (Accessed 9th June 2020).
- 6.Riccardo F, Ajelli M, Andrianou XD, Bella A, Del Manso M, Fabiani M, et al. Epidemiological characteristics of COVID-19 cases in Italy and estimates of the reproductive numbers one month into the epidemic. Available at: https://www.medrxiv.org/content/10.1101/2020.04.08.20056861v1.full.pdf (Accessed 9th June 2020).
- 7.https://www.istat.it/it/files//2020/05/Rapporto_Istat_ISS.pdf (Accessed 9th June 2020).
- 8.Garazzino S., Montagnani C., Donà D., et al. Multicentre Italian study of SARS-CoV-2 infection in children and adolescents, preliminary data as at 10 April 2020. Euro Surveill. 2020;25(18):2000600. doi: 10.2807/1560-7917.ES.2020.25.18.2000600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_14-maggio-2020.pdf (Accessed 9th June 2020).
- 10.http://www.governo.it/it/coronavirus-misure-del-governo (Accessed 9th June 2020).
- 11.Consip. Emergenza COVID-19: precisazioni sulla qualità e le modalità di distribuzione dei dispositivi di protezione individuale. March 15, 2020. https://www.consip.it/media/news-e-comunicati/emergenza-COVID-19-precisazioni-sulla-qualit-e-le-modalit-didistribuzione-dei-dispositivi-di-protezioneindividuale (Accessed 9th June 2020).
- 12.https://healthmanagement.org/c/hospital/news/covid-19-experience-of-italian-gps (Accessed 9th June 2020).
- 13.https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_20-maggio-2020.pdf (Accessed 9th June 2020).
- 14.Flick H, Arns BM, Bolitschek J, et al. Management of patients with SARS-CoV-2 infections and of patients with chronic lung diseases during the COVID-19 pandemic (as of 9 May 2020): Statement of the Austrian Society of Pneumology (ASP). Wien Klin Wochenschr. 2020 Jun 12:1–22. doi: 10.1007/s00508-020-01691-0. Online ahead of print. [DOI] [PMC free article] [PubMed]
- 15.RCPCH. Guidance: paediatric multisystem inflammatory syndrome temporally associated with COVID-19. (1.5.20) https://www.rcpch.ac.uk/sites/default/files/2020-05/COVID-19-Paediatric-multisystem-%20inflammatory%20syndrome-20200501.pdf (Accessed 9th June 2020).
- 16.RCPCH. Delayed access to care for children during COVID-19: our role as paediatricians – position statement. (3.4.20). https://www.rcpch.ac.uk/resources/delayed-presentation-during-covid-19-position. (Accessed 9th June 2020).
- 17.Public Health England. Guidance: COVD-19 personal protective equipment (PPE). (Updated 3.5.20) https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe. (Accessed 9th June 2020).
- 18.Public Health England. Guidance on shielding and protecting people who are clinically extremely vulnerable from COVID-19. Updated 17.4.20. https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19. (Accessed 9th June 2020).
- 19.NICE. COVID-19 rapid guideline: severe asthma (3.4.20). https://www.nice.org.uk/guidance/ng166. (Accessed 9th June 2020). [PubMed]
- 20.NICE. COVID-19 rapid guideline: cystic fibrosis (9.4.20). https://www.nice.org.uk/guidance/ng170. (Accessed 9th June 2020). [PubMed]