ABSTRACT
Background:
Diabetes control in adolescents is a difficult and tedious process. Diabetic teens need training to control it and prevent its complications. This study aimed to investigate the effect of peer education on self-care behaviors and glycosylated hemoglobin among adolescents with type 1 diabetes
Methods:
This controlled clinical trial was conducted in Iran from July 2018 to June 2019. 84 teenagers with type 1 diabetes were selected using a simple random sampling and randomly divided into control and intervention groups using block randomization. The intervention group received 4 sessions of training by peers on self care behaviors in diabetes. The control group received the routine training. The self-care questionnaire was filled out, and glycosylated hemoglobin was measured before and three months after the intervention. Data were analyzed using SPSS version 23.0. The significance level was set at P<0.0
Results:
Three months after the intervention, the intervention group reported significantly higher levels of score of self-care behaviors (P<0.001) and lower levels of mean glycosylated hemoglobin (P<0.001), as compared with the control. Also, the mean self-care score was not significantly different in the control group before and three months after the intervention (P>0.05). Besides, the mean glycosylated hemoglobin significantly increased three months after the intervention in the controls (P<0.001)
Conclusion:
The implementation of peer education can improve the self-care behaviors and glycosylated hemoglobin in adolescents. Hence, regarding its low cost and high safety, it is suggested that this approach should be established in the control of other chronic diseases in order to strengthen the self-care behaviors in adolescents.
Trial Registration Number: IRCT20180904040944N1.
KEYWORDS: Adolescent, Diabetes, Education, Glycosylated hemoglobin, Peers, Self-care
INTRODUCTION
Diabetes ranks highly on the international health agenda as a global pandemic and as a threat to human health and global economies. 1 , 2 Diabetes causes premature death, severe disability and great economic burden. 3 The annual incidence of type 1 diabetes mellitus is constantly increasing throughout the world. 4 75% of the total cases of diabetes mellitus type 1 have been detected in adolescents under 18, specially in their teen ages. 5 It is estimated that about 80,000 children under 15 years of age develop type 1 diabetes annually worldwide. Over 90% of pediatric and adolescent diabete in most western countries is type 1 diabetes. 6 There were over 3 million type 1 diabetes patients in the United States in 2010. 7 The prevalence of this disorder is estimated about 5-10% in Iran. 8
Adolescence is a period of marked change, including the hormonal and psychosocial changes associated with puberty and emerging young adulthood. While the hormonal changes of adolescence can lead to insulin resistance, there are several other factors (psychosocial, regimen-related, and communication-related) that cause poor glycemic control in adolescents. Understanding and targeting the reasons behind the poor control seen in adolescence are requisite steps to improve glycemic control in this age group. 9
The most important factor in the control of diabetes is the patients’ self-care behaviors that lead to better control of blood sugar. 10 Self-care behaviors increase the quality of life, reduce the expenses and prevent the side-effects of the disease. 11 One of the major causes of disease progression and the emergence of side-effects is lack of self-care behaviors, 12 which might be one of the most basic causes of death in diabetic patients. 13 Research conducted in this area suggests that self-care in diabetic patients is not satisfactory. 14 However, it seems that education can enhance the patients’ self-care. Education is at the core of diabetes prevention and treatment. 15 One of the educational approaches in this regard is peer education method. 16 These instructions play a significant role in improving hygiene and creating a learning environment. 17 Peer education is an appropriate method for providing behavioral change. The influence of peers on the youth is certainly of great importance. Education of peers aims at using positive peer influence on other fellow peers. 18 The purpose of peer education method is to enhance the knowledge, attitude and skill of adolescents, which leads to the responsibility of adolescents for maintaining and promoting their health. 19
There are some studies available in our country that have evaluated the effect of peer education on other diseases. In a study, the researchers showed that the mental health of the hemodialysis patients after peer education was significantly higher than the control group. 20 Moreover, the results of another study revealed that peer education could increase the quality of life in mastectomy patients. 21 In this regard, a study on middle school students showed that peer education changed the adolescents’ behaviors to healthier lifestyles. 22 According to another study, peers are a common source of information and medical knowledge about breast self-examination. The use of peers was more cost-effective and economical, 23 and peer education facilitated learning and led to deep learning and a growing interest in learning. 24 In addition, peer education may have a particular potential in implementing diabetes care without having a large additional burden on the health system. 25 Nurses, as one of the largest health care providers, 26 and diabetes educators are being used to promote diabetes self-management, but such programs are resource intensive; the number of specialist nurses and diabetes educators is not adequate to manage for the increasing demand for diabetes care, especially in low-resource settings. Therefore, it is urgent to find innovative and effective solutions that build on available resources to help the patients successfully manage diabetes. 27
Given the importance of diabetes control in adolescents, the high acceptance level of peer education method among the adolescents, and lack of a clinical trial study about the effect of peer education on adolescents with type 1 diabetes in Iran, this study aimed to assess the effect of peer education on self-care behaviors and glycosylated hemoglobin of type 1 diabetic adolescents.
MATERIALS AND METHODS
This double-blinded controlled clinical trial was conducted in the south of Iran from July 2018 to June 2019. The participants of this study consisted of 84 adolescents with type 1 diabetes, who were examined in the center for diabetic patients in Imam Reza clinic affiliated to Shiraz University of Medical Sciences, Shiraz, Iran.
The Diabetes clinic serves approximately 1000 diabetes patients (all age ranges with both types of diabetes). The services delivered include medical reviews and examinations, such as treatment and disease management plans, diabetes education, and, whenever available, free supply of medical essentials, such as needles and syringes. A certified diabetes educator (nurse, dietitian, social worker,..) facilitates group education visits.
The sample size was calculated using the formula below using α=0.05, β=0.20 and the mean (mean 1=8.7, mean 2=9.6) and variance (σ2=2.105) based on the results of a previous study. 28 At least, a 84-subject sample size (42 subjects in each group) was determined for the study. By considering a 10% attrition rate, the final sample size for both groups was about 96 (48 subjects in each group).
Inclusion criteria for this study were age of 12-18 years, approved type 1 diabetes by a pediatric endocrinologist, glycosylated hemoglobin higher than 7.5%, a history of medical file in the diabetes clinic, at least one-year history of diabetes, and patients’ and their parents’ consent for participation in the study.
The exclusion criteria of the study were psychological disorders that affect learning procedures, history of medications that impair the learning procedure, and consciousness or any history of chronic diseases, absence in more than two training sessions, inability to participate in the training program due to the severity of the disease or hospitalization, and lack of willingness to participate in the study.
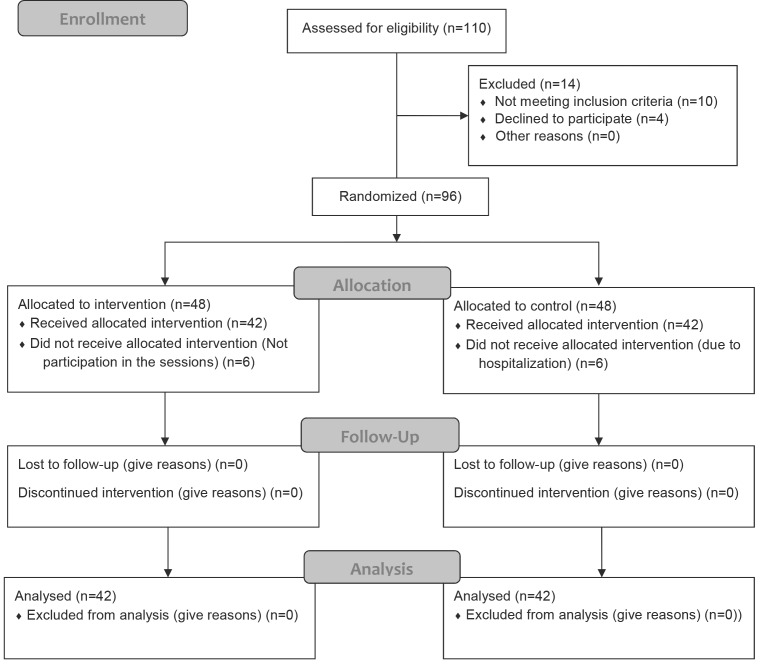
Overall, 110 adolescents were assessed for eligibility. The subjects were selected based on the simple random sampling method (selected from a random number table) among all 350 records of the diabetic patients available at the time of the present study in the diabetes center. The patients interested in participating in the research gave their written informed consent to complete the self-care questionnaire, and their glycosylated hemoglobin was measured. The individuals who obtained glycosylated hemoglobin lower than 7.5% were excluded from the study (10 patients). Moreover, 4 patients were excluded from the study due to their lack of willingness to participate in the study. The remaining patients (96) were randomly divided into control (N=48) and intervention (N=48) groups, using the software Random Allocation and randomized blocking with a random sequence of 24 quadruple blocks. During the study, 6 patients in the control group were excluded due to hospitalization and 6 in the intervention group due to lack of participation in the sessions (Figure 1).
Figure 1.
CONSORT Flow Diagram of participants
The outcome measures of the study consisted of demographic information, glycosylated hemoglobin and self-care. In addition to the socio-demographic assessment of the age, gender, marital status, education level, accommodation, disease side-effects, job of parents, income of parents, duration of illness, the following variables were measured:
Self-care behavior in diabetic adolescents was measured using the self-care questionnaire. The questionnaire was designed by Schilling in America in 2009. The content validity of the questionnaire was 0.93 and Cronbach’s alphas for the questionnaire ranged from 0.71 to 0.85 and were considered acceptable. Exploratory alpha factor analyses revealed five subscales: Collaboration with Parents, Diabetes Care Activities, Diabetes Problem-Solving, Diabetes Communication, and Goals (α=0.71 to 0.85). 29 , 30
Translation of Schilling et al.’s self-care questionnaire was done by Rezasefat Balasbane in 2012 and the validity and reliability of the questionnaire were determined by the Balasbane and colleagues. In this way, they used a transcript method to determine the content validity, and the questionnaire was given to 10 faculty members of Guilan University of Medical Sciences to express their opinions. To determine the reliability of the questionnaire, they conducted a pilot study on 15 samples, with Cronbach’s alpha of 0.77. Content validity index was also used to estimate the validity of the questionnaire expressions in three areas of simplicity, clarity and importance. After collecting the teachers’ comments, phrases 13 and 15, with a CVI of 0.6 and 0.64 were removed from the questionnaire, and the questionnaire expressions were reduced from 52 to 50. The scale is a 4-point Likert scale ranging from 1 point to 4 points. Ratings of expressions 8, 21, 22, 23, 25, 26 were reversed and consisted of 50 questions with a minimum score of 50 and a maximum of 200 which included areas of cooperation with parents (12 questions), self-care activities (14 questions), problem solving in diabetes (7 questions), communication in diabetes (10 questions), and disbetes objectives (7 questions). 30
For measuring the glycosylated hemoglobin, a venous sample was taken from each participant and sent to laboratory, before and 3 months after the intervention via calorimetry method, using a DIRUI autoanalysis device which was calibrated daily. All participants were tested in Shahid Motahari Clinic of Shiraz University of Medical Sciences.
Patients in the control group received the routine training, including education on exercising, nutrition, and blood glucose control by the clinic personnel. The content of educational program was the same for the two groups.
Apart from the interventional groups, they selected six 12-18 year old teenagers (equal to the number of interventional groups) with type 1 diabetes, whose disease management was approved by an endocrine sub-specialist and their medical records, as peer educators. These teenagers were trained by the investigators for three 90 minute sessions. A peer educator was assigned for each interventional group.
The intervention was designed based on the patients’ needs and the existing literature in this field. The educational intervention consisted of four 90 minute sessions held over four weeks. The patients in the intervention group were divided into 6 sub-groups of 8 members by the researcher to hold the training workshops. A peer educator was assigned for each interventional group. The training sessions were face-to-face question-and-answer meetings using group discussions. Educational sessions were held with the presence and supervision of the second author.
In order to assure peer readiness and their training equality, the researcher used a checklist. If the peer complied, they would be allowed to enter the next stage. Then, the peer group practiced their teaching experiences using role-playing in the presence of the researcher, so that peers could train diabetic adolescents in educational sessions. The researcher modified and supplemented educational content as a booklet, according to scientific textbooks. Ultimately, the booklets were given to peers. Kruskal-wallis test showed no significant difference between the six groups (P>0.05).
The location of the training workshops was the conference hall of the center for diabetes patients. The training was provided by one of the peer educators. The contents of each of the four sessions are summarized in Table 1.
Table 1.
Content of the educational program
| Sessions | Content |
|---|---|
| 1 | Overview of the program and introduction of instructors and members to each other |
| Discussion on the definition and importance of peer education | |
| Explaining the identity and cause of diabetes | |
| Answering patient questions | |
| 2 | Overview of previous sessions |
| Types of diabetes | |
| Symptoms of diabetes | |
| Diabetes risk factors | |
| Complications of diabetes | |
| Answering patient questions | |
| 3 | Overview of previous sessions |
| Expressing the importance of self-care skills | |
| Nutrition in diabetes | |
| Exercise in diabetes | |
| Blood sugar control in diabetes | |
| Answering patient questions | |
| 4 | Overview of previous sessions |
| Treatment of diabetes | |
| Medication in diabetes | |
| Diabetes control | |
| Answering patient questions |
For encouraging the patients to participate in the study, a free glycosylated hemoglobin test was given to all the patients, and some gifts were given to some of the participants at the end of the study.
Three months after the end of the intervention, the self-care questionnaire was filled out again by the two groups and the glycosylated hemoglobin was re-evaluated in the two groups. The control and interventional groups received the educational booklet on self-care skills at the end of the study due to ethical considerations.
This was a double-blind clinical trial, and the researcher’s assistant who was unaware of the types of intervention collected the data, and the statistician who analyzed the data was blind to the study groups.
SPSS version 23.0 was used for the statistical analysis of the collected data. In the beginning, Kolmogorov–Smirnov test was applied to check the distribution for normality. Independent t-test, Analysis of covariance (ANCOVA) and Chi-square test were employed to investigate the differences between the two groups regarding demographic and clinical variables. Paired t-test was used to determine whether improvements in the variable changed before and after the intervention . The significance level was set at P<0.05.
The study was approved by Research Ethics Committee of Shiraz University of Medical Sciences (code: 1397.324). Before the intervention, all the patients and their parents were informed of the objectives of the study, ensured about the confidentiality of their information, and signed the informed consent form. The patients were also informed that they were free to withdraw at any point of the research and the time and place of the intervention were set by their agreement. All parts of the study were reviewed according to the Consolidated Standards for Reporting Trials (CONSORT) statement (Figure 1).
RESULTS
Overall, 84 patients participated in the study. The Kolmogorov-Smirnov test showed a normal distribution of quantitative variables, namely age, duration of illness, self-care, and glycosylated hemoglobin. Analysis of the demographic data revealed that the majority of the participants in both groups were female (n=52, 61.90%). The mean age of the patients in the intervention and control groups was 14.85±1.80 years and 15.02±1.85 years, respectively. Most of the participants in both groups were city dewellers (n=66, 78.60%) and their education was lower than diploma (n=78, 92.20%); they also had no disease side-effects (n=77, 91.70%). The mean of the duration of illness in the intervention and control groups was 5.26±2.78 and 5.24±2.80 years, respectively.
According to the results of independent t-test and Chi-square tests, no significant difference was found between the two groups in terms of demographic characteristics such as age (P=0.67), duration of illness (P=0.96), sex (P=0.82), education (P=0.67), accommodation (P=0.79), disease side-effects (P=0.43), parents’ job (P=0.12), and parents’ income (P=0.38) (Table 2).
Table 2.
Demographic characteristics of the study participants (N=84)
| Variant | Intervention N (%) | Control N (%) | P value* | |
|---|---|---|---|---|
| Gender | Female | 27 (64.30) | 25 (59.50) | 0.82 |
| Male | 15 (35.70) | 17 (40.50) | ||
| Education level | Lower than diploma | 38 (90.50) | 40 (95.20) | 0.67 |
| Diploma | 4 (9.50) | 2 (4.80) | ||
| Accommodation | Urban | 34 (81) | 32 (76.20) | 0.79 |
| Rural | 8 (19) | 10 (23.80) | ||
| Disease side-effects | Yes | 5 (11.90) | 2 (4.80) | 0.43 |
| No | 37 (88.10) | 40 (95.20) | ||
| Job of parents | Employee | 7 (16.70) | 13 (31) | 0.12 |
| Self-employment | 35 (83.30) | 29 (69) | ||
| Income of parents | Less than a million | 25 (59.50) | 21 (50) | 0.38 |
| More than a million | 17 (40.50) | 21 (50) | ||
Chi-square
According to the results of independent t-test for mean glycosylated hemoglobin and self-care score (co-operation with parents, resolving the issue of disease, connections in diabetes, diabetes objective), it was shown that they were not significantly different in these groups before the intervention (co-operation with parents P=0.57, resolving the issue of disease P=0.70, connections in diabetes P=0.92, diabetes objectives P=0.12, and glycosylated hemoglobin P=0.96). Only for self-care activities (P=0.001), the groups were significantly different before the intervention (Table 3). Therefore, ANCOVA was used to compare the groups regarding the mentioned aspect.
Table 3.
The inter-group comparison of self-care scores and glycosylated hemoglobin in the intervention and control groups
| Group | Intervention | Mean±SDControl | Mean±SDP-value | ||||
|---|---|---|---|---|---|---|---|
| Time Variant | Before Intervention | After Intervention | Before Intervention | After Intervention | Before Intervention | After Intervention | |
| Self-care | Co-operation with parents | 24.70±3.80 | 36.70±4.30 | 25.10±3.90 | 24.10±3.20 | 0.57 | <0.001* |
| Self-care activity | 27.30±2.80 | 40.40±2.80 | 29.50±3.10 | 28.50±2.40 | 0.001 | <0.001* | |
| Resolving the diabetes issue | 15±2.30 | 19.90±1.90 | 14.80±2.20 | 14.60±2.05 | 0.70 | <0.001* | |
| Diabetes connections | 20.70±2.30 | 28.90±2.30 | 20.60±1.90 | 20.2±2.30 | 0.92 | <0.001* | |
| Diabetes objectives | 14.09±2.70 | 20.90±2.60 | 14.90±2.20 | 14.20±2.10 | 0.12 | <0.001* | |
| Glycosylated hemoglobin | 12.20±2.90 | 11.28±2.80 | 12.21±2.90 | 15.20±2.80 | 0.96 | <0.001* | |
Independent t-test
Analysis of covariance(ANCOVA)
The result of independent t-test showed a significant difference in the mean glycosylated hemoglobin and self-care score (co-operation with parents, resolving the issue of disease, connections in diabetes, diabetes objective), between the two groups (P<0.001) three months after the intervention; also, the result of ANCOVA showed a significant difference in self-care score (self-care activities) between the two groups (P<0.001) three months after the intervention; the average self-care score (co-operation with parents, resolving the issue of disease, connections in diabetes, diabetes objective and self-care activities) was significantly higher and the mean glycosylated hemoglobin was significantly lower in the intervention group three months after the intervention, compared with the control group (Table 3).
Paired t-test showed increased self-care score and reduced glycosylated hemoglobin in the intervention group three months after the intervention (P<0.001) (Table 4), while the mean self-care score was not significantly different in the control group before and three months after the intervention (co-operation with parents P=0.17, self-care activities P=0.07, resolving the issue of disease P=0.75, connections in diabetes P=0.33, and diabetes objectives P=0.07). Besides, the mean glycosylated hemoglobin significantly increased three months after the intervention in the control group (P<0.001) (Table 4).
Table 4.
The intra-group comparison of self-care scores and glycosylated hemoglobin for the intervention and control groups before and three months after the intervention
| Group | Intervention | Control | |||||
|---|---|---|---|---|---|---|---|
| (Mean±SD) | P value* | (Mean±SD) | P value* | ||||
| Time | Before Intervention | After Intervention | Before Intervention | After Intervention | |||
| Self-care | Co-operation with parents | 24.70±3.80 | 36.70±4.30 | <0.001 | 25.10±3.90 | 24.10±3.20 | 0.17 |
| Self-care activities | 27.30±2.80 | 40.40±2.80 | <0.001 | 29.50±1.30 | 28.50±2.40 | 0.07 | |
| Resolving the diabetes issue | 15±2.30 | 19.90±1.90 | <0.001 | 14.80±2.20 | 14.60±2.05 | 0.75 | |
| Connections of diabetes | 20.70±2.30 | 28.90±2.30 | <0.001 | 20.60±1.90 | 20.20±2.30 | 0.33 | |
| Diabetes objectives | 14.09±2.70 | 20.90±2.60 | <0.001 | 14.90±2.20 | 14.20±2.10 | 0.07 | |
| Glycosylated hemoglobin | 12.20±2.90 | 11.28±2.80 | <0.001 | 12.21±2.90 | 15.20±2.80 | <0.001 | |
Paired t-test
DISCUSSION
The effect of peer education on self-care behaviors and the mean of glycosylated hemoglobin in type 1 diabetic adolescents were evaluated in this study. The results of the study revealed that peer education increased and improved the self-care behaviors and decreased the mean of glycosylated hemoglobin in type 1 diabetic adolescents. Findings of this study highlight the importance of peer education in order to control diabetese in diabetic adolescents.This result indicated that peer education in the intervention group was effective.
The most important factor in the control of diabetes is patients’ self-care behaviors. Self-care behaviors have been found to be positively correlated with good glycemic control. Despite this fact, adherence to self-care behaviors has been found to be low. Social support factors can be considered as positive contributors in facilitating self-care behaviors in diabetic patients. 31 Social support enables the adolescents with diabete type 1 to cope with difficulties associated with the management and treatment. Social support for children is provided by parents and family, while it is provided by peer groups for adolescents. 32 Despite the potential benefits of peer education that could improve the self-care behaviors and decrease glycosylated hemoglobin in type 1 diabetic adolescents, there are few studies on the positive effect of peer education in this population. Our findings were in line with those of other studies. In a study, it was concluded that peer education improved the self-care behaviors, quality of life, and psychological status of type 2 diabetic patients. 33 Another study also showed that peer education could improve self-care behaviors in patients with type 2 diabetes. 34 The results of another study also confirmed that peer-led structured education can improve the glycaemic control in patients with type 2 diabetes. 35
In the above-mentioned studies, the researchers examined the effects of peer education in type 2 diabetic patients. However, in the present study the samples consisted of adolescents with type 1 diabetes. The results of some studies were inconsistent with our findings. One study showed that the glycosylated hemoglobin and self-care behaviors in type 1 diabetic adolescents did not significantly change after participation in the camp. 36 The finding of the mentioned study was inconsistent with the results of the current study. The difference in duration of the follow up (12 months after intervention) and sample size (27 patients) might be the probable causes of this difference in results. In the above-mentioned study, the sample size was 27 patients and duration of the follow up was 12 months after the intervention. However, in the present study the sample size was 84 patients and duration of the follow up was 3 months after the intervention. Another study indicated that the peer support caused an insignificant reduction in the level of glycosylated hemoglobin and patients’ wellbeing. 37 This result was also in contrast with our findings. The difference in the samples and number of sessions might be the causes of this difference in results. In the above-mentioned study, the researchers examined the effects of peer education in type 2 diabetic patients in 9 sessions. However, in the present study the samples were the adolescents with type 1 diabetes and number of sessions were 4 sessions.
The significant findings of the present research showed that peer education led to increased self-care behaviors and decreased glycosylated hemoglobin in type 1 diabetic adolescents. Findings of this study suggest the importance of including routine use of peer education in the management of type 1 diabetic adolescents. The results of the study showed a significant increase in the self-care scores and decreased glycosylated hemoglobin of the intervention group in the post-test, which were reflected in large effect sizes.
Overall, in peer education, patients learn to use similar life experiences between the peer educator and the peers and cope with difficulties associated with the management and treatment. It might enhance their self-care. In addition, the high acceptance level of peer education method among adolescents might improve the control of diabetes in type 1 diabetic adolescents. This illustrates that the peer education in the present study can be especially effective in increasing self-care behaviors and decreasing the glycosylated hemoglobin in type 1 diabetic adolescents. Thus, the findings of the study can expand our horizons about the concept of peer education.
Overall, considering the findings of the present research and those of the previous studies, we can claim that peer education can enhance the self-care behaviors and decrease glycosylated hemoglobin in type 1 diabetic adolescents.
Limited training sessions, performance of the study in a single center, and lack of follow up were some of the limitations of the current study. Thus, it is suggested that similar studies should be conducted in larger centers, with scheduled follow up periods and increased training sessions.
CONCLUSION
The implementation of peer education with participation of peers and patients can improve the self-care behaviors and glycosylated hemoglobin in diabetic patients and increase the control over this disease in adolescents. Hence, regarding its low cost, high safety and effectiveness, it is suggested that this approach should be established in the control of other chronic diseases and in different care aspects, in order to instruct and strengthen the self-care behaviors in patients, specially adolescents.
ACKNOWLEDGEMENT
This study was extracted from the second authors’ master’s thesis. It was approved with the code number of 97-01-08016816. The authors would like to thank the adolescents and their parents, the personnel of Imam Reza diabetes clinic for participating in the study and Shiraz University of Medical Sciences for financial support. The authors would like to thank Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Conflict of Interest: None declared.
REFRENCES
- 1.Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. The lancet Diabetes & Endocrinology. 2014;2:56–64. doi: 10.1016/S2213-8587(13)70112-8. [DOI] [PubMed] [Google Scholar]
- 2.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Research and Clinical Practice. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Sabban ENC, Puchulu FM, Cusi K. Dermatology and Diabetes. Switzerland: Springer; 2018. [Google Scholar]
- 4.Marcdante K, Kliegman RM. Nelson Essentials of Pediatrics E-Book. 7 th ed. Philadelphia: Elsevier; 2014 . [Google Scholar]
- 5.American Diabetes Association. Children and adolescents: standards of medical care in diabetes. Diabetes Care. 2018;41:S126–36. doi: 10.2337/dc18-S012. [DOI] [PubMed] [Google Scholar]
- 6.Craig ME, Jefferies C, Dabelea D, et al. Definition, epidemiology, and classification of diabetes in children and adolescents. Pediatric Diabetes. 2014;15:4–17. doi: 10.1111/pedi.12186. [DOI] [PubMed] [Google Scholar]
- 7.Khawandanah J. Double or hybrid diabetes: A systematic review on disease prevalence, characteristics and risk factors. Nutrition & Diabetes. 2019;9:33. doi: 10.1038/s41387-019-0101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.kermansaravi F, Navidian A, Ansari moghadam A. Quality of Life in Type 1 Diabetic Adolescents in Zahedan (2011) . Iranian Journal of Endocrinology and Metabolism. 2011;13:651–7. [In Persian] [Google Scholar]
- 9.Datye KA, Moore DJ, Russell WE, Jaser SS. A review of adolescent adherence in type 1 diabetes and the untapped potential of diabetes providers to improve outcomes. Current Diabetes Reports. 2015;15:51. doi: 10.1007/s11892-015-0621-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahmoodi A, Alavi M, Mosavi N. The relationship between self-care behaviors and HbA1c in diabetic patients. Scientific Journal of Hamadan Nursing & Midwifery Faculty. 2013;20:20–5. [In Persian] [Google Scholar]
- 11.Jalilian F, Zinat Motlagh F, Solhi M. Effectiveness of Education Program on Increasing Self Management Among Patients with Type II Diabetes. Journal of Ilam University Of Medical Sciences. 2012;20:26–34. [In Persian] [Google Scholar]
- 12.Jackson IL, Adibe MO, Okonta MJ, Ukwe CV. Knowledge of self-care among type 2 diabetes patients in two states of Nigeria. Pharmacy Practice. 2014;12:404. doi: 10.4321/s1886-36552014000300001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baji Z, Zamani alavijeh F, Nouhjah S, Haghighizadeh MH. Self-care behaviors and related factors in women with type 2 diabetes. Iranian Journal of Endocrinology and Metabolism. 2015;16:393–401. [In Persian] [Google Scholar]
- 14.Firooz M, Hosseini SJ, Mazlom SR, et al. Self-care of Patient with Diabetes Type II. Sabzevar University of Medical Sciences. 2016;22:1018–24. [In Persian] [Google Scholar]
- 15.Torabizadeh C, Asadabadi poor Z, Shaygan M. The Effects of Resilience Training on the Self-Efficacy of Patients with Type 2 Diabetes: A Randomized Controlled Clinical Trial. International Journal of Community Based Nursing & Midwifery. 2019;7:211–21. doi: 10.30476/IJCBNM.2019.44996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morowatisharifabad M, Alizadeh Mradkandi A, Mozaffari Khosravi H, et al. Comparison of the effect nutrition education by peers and health personnel on knowledge, attitude and nutritional indices of 18-35 years old women of Orumieh health care centers. The Journal of Tolooebehdasht. 2012;11:54–64. [In Persian] [Google Scholar]
- 17.Webel AR, Okonsky J, Trompeta J, Holzemer WL. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. American Journal Of Public Health. 2010;100:247–53. doi: 10.2105/AJPH.2008.149419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bilgiç N, Günay T. Evaluation of effectiveness of peer education on smoking behavior among high school students. Saudi Medical Journal. 2018;39:74–80. doi: 10.15537/smj.2018.1.21774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bulduk S, Erdogan S. The effects of peer education on reduction of the HIV/sexually transmitted infection risk behaviors among Turkish university students. Journal of the Association of Nurses in AIDS Care. 2012;23:233–43. doi: 10.1016/j.jana.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Malek khahi A, Jadid Milani M, Amiri P. The Effects of Peer Support Groups on Mental Health of Hemodialysis Patients. Iran Journal of Nursing. 2015;28:40–9. [In Persian] [Google Scholar]
- 21.Sharif F, Abshorshori N, Tahmasebi S, et al. The effect of peer-led education on the life quality of mastectomy patients referred to breast cancer-clinics in Shiraz, Iran 2009. Health and Quality of Life Outcomes. 2010;8:74. doi: 10.1186/1477-7525-8-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmadizade fini E, Madani A, Alizade A, et al. Effect of Peer Education on Health Promoting Behaviors of Junior High School Students. Iranian Journal of Health Education and Health Promotion. 2015;3:105–15. [In Persian] [Google Scholar]
- 23.Akbarzadeh M, Zangiabadi M, Moattari M, Tabatabaei H. Comparing the effect of teaching breast self-examination by peers and health care personnel on students knowledge and attitude. Iranian Journal of Medical Education. 2009;8:195–203. [In Persian] [Google Scholar]
- 24.Zarifnejad G, Mazloom SR, Mirhaghi A, et al. Learning experience through peer education: a qualitative study. Iranian Journal of Medical Education. 2015;15:27–40. [In Persian] [Google Scholar]
- 25.Seuring T, Marthoenis, Rhode S, et al. Using peer education to improve diabetes management and outcomes in a low-income setting: a randomized controlled trial. Trials. 2019;20:548. doi: 10.1186/s13063-019-3656-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soltanian M, Molazem Z, Mohammadi E, et al. Professional responsibility: an ethical concept extracted from practices of Iranian nurses during drug administration. International Journal of Pharmaceutical Research. 2018;10:346–53. [Google Scholar]
- 27.Qi L, Liu Q, Qi X, et al. Effectiveness of peer support for improving glycaemic control in patients with type 2 diabetes: a meta-analysis of randomized controlled trials. BMC Public Health. 2015;15:471. doi: 10.1186/s12889-015-1798-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Najmi B, ahadi H, Deldavar A, Hashemipoor M. The effectiveness of multidimentional psychological treatment in enhancing the adherence to medical treatment in adolescents with type 1 diabetes. Journal of research behavioural science. 2007; 5(2):127–136. [Google Scholar]
- 29.Schilling LS, Dixon JK, Knafl KA, et al. A New Self-Report Measure of Self-Management of Type 1 Diabetes for Adolescents. Nursing Research. 2009;58:228–36. doi: 10.1097/NNR.0b013e3181ac142a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rezasefat Balesbaneh A, Mirhaghjou N, Jafsri Asl M, et al. Correlation between self-care and self-efficacy in adolescents with type 1 diabetes. Journal of Holistic Nursing And Midwifery. 2014;24:18–24. [In Persian] [Google Scholar]
- 31.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. Journal of Diabetes & Metabolic Disorders. 2013;12:14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Altundag S, Bayat M. Peer interaction and group education for adaptation to disease in adolescents with Type 1 diabetes mellitus. Pakistan Journal of Medical Sciences. 2016;32:1010–4. doi: 10.12669/pjms.324.9809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Y, Han Y, Shi J, et al. Effect of peer education on self-management and psychological status in type 2 diabetes patients with emotional disorders. Journal of Diabetes Investigation. 2015;6:479–86. doi: 10.1111/jdi.12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ahmadi Z, Sadeghi T, Loripoor M. The effect of peer education on self-care behaviors among diabetic patients. Iranian Journal of Diabetes and Metabolism. 2016;15:382–91. [In Persian] [Google Scholar]
- 35.Debussche X, Besançon S, Balcou Debussche M, et al. Structured peer-led diabetes self-management and support in a low-income country: The ST2EP randomised controlled trial in Mali. PLoS One. 2018;13:e0191262. doi: 10.1371/journal.pone.0191262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Santiprabhob J, Kiattisakthavee P, Likitmaskul S, et al. Glycemic control, quality of life and self-care behavior among adolescents with type 1 diabetes who attended a diabetes camp. Southeast Asian Journal of Tropical Medicineand Public Health. 2012;43:172–84. [PubMed] [Google Scholar]
- 37.Smith SM, Paul G, Kelly A, et al. Peer support for patients with type 2 diabetes: cluster randomised controlled trial. BMJ. 2011;342:d715. doi: 10.1136/bmj.d715. [DOI] [PMC free article] [PubMed] [Google Scholar]