Highlights
-
•
Assessing overall diet quality rather than individual micro/macro nutrients is needed.
-
•
Students purchasing lunch from a shop/café have the lowest diet quality score among both age groups.
-
•
Packed lunches were the most common type of lunch consumed during a school day.
-
•
For older students, packed lunch consumers had the highest overall diet quality, unlike younger children in primary school.
-
•
The food environment and student preferences have an impact on adolescent food choice.
Keywords: Adolescent, School meals, Diet quality, Fast food, Food, Nutrients
Abstract
Diet quality of children consuming school meals tends to be better than that of children consuming packed lunches (from home) or food bought outside school. This study investigates the association between different types of lunch consumed in a school day and diet quality of UK adolescents. A total of 2118 British adolescents were included from the National Diet and Nutrition Survey (Years 1–8; between 2008 and 2016). All participants attended school and were aged 11–18 years with valid 3 or 4-day diary records and the analyses were stratified by age group (11–14 and 15–18 years). The Diet Quality Index for Adolescents (DQI-A) tool consisting of three components; diet quality, diversity and equilibrium, was used to assess adherence to dietary recommendations. Overall DQI-A scores range from –33 to 100%. Overall mean DQI-A score for all adolescents was low at 21.1%. Fewer (17.4%) adolescents reported buying lunches from cafés and shops, compared to adolescents consuming cooked school meals and packed lunches (28.3% and 36.6%, respectively), and they had the lowest DQI-A% score of 14.8%. Adolescents having cooked school meals (reference group) had a higher overall DQI-A% of 21.8%. Diet quality scores of older adolescents having packed lunches and shop/café-bought lunches were 5.5% higher (CI 2.7 to 8.4%; p < 0.01) and 5.0% lower (CI 8.1 to 2.0%; p < 0.01) than cooked school meals respectively, after adjusting for gender, region, energy under-reporting and equivalised household income. For younger adolescents the results were attenuated particularly among packed lunch consumers. UK adolescents generally consume a poor quality diet and adolescents purchasing lunches from outside the school gates have the lowest quality diets. Unlike with older children there is little difference between school meals and packed lunches for younger children. Regulation policies on food outlets around secondary schools as well as improving food choices within school premises are needed.
1. Introduction
The type and quality of food consumed by children and young people during a school day is a primary concern in many countries. The total number of secondary state school students in England is 3.2 million; and students spend nearly 190 days (approximately half) of the whole year in school (Department for Education, 2019). Legislation exists across the UK to improve the school food environment including cutting down sales of foods that are high in fat, sugars and salt, as well as providing better food choices (Department for Education, 2019). Evidence has consistently shown that the dietary quality of primary school children consuming school meals is better than those consuming packed lunches (food brought from home) (Harrison et al., 2013, Evans et al., 2016) although the research on secondary schools is less consistent (Pearce et al., 2013, Prynne et al., 2013, Ensaff et al., 2013). The four different regions of the UK; England, Wales, Scotland and Northern Ireland, have implemented mandatory school food standards to improve quality of foods provided at school (British Nutrition Foundation, 2020). In England, the revised requirements for School Food Regulations came into force in 2015 and are solely food-based, having dropped nutrient-based standards introduced in 2009 (Department for Education, 2019). These regulations focus on menu planning and provision of school foods and drinks; including types and portion sizes of starchy foods, fruit and vegetables, protein-rich foods and foods high in fats, sugars and salt that can be provided as a part of school lunch (Department for Education, 2019, Ensaff et al., 2016). In England, meals must be available and hot lunches should be provided to all school pupils (Department for Education, 2019). However, the number of children who consume school meals has decreased in England, particularly in secondary schools and there is concern that alternative lunch types are lower in quality. Observational studies have stated that the price of food items (Wills et al., 2019, Sahota et al., 2014) offered at school, the length of the queue to purchase a school meal (Sahota et al., 2014) and appearance and taste of the food (Wills et al., 2019) may affect secondary school students’ food choices. In some cases secondary schools allow older children to leave school premises during the lunchtime break (Public Health England, 2014) which may account for some of the reduction in school meal take-up. Previous work on takeaway food purchased at any time of the day highlighted the negative impact of consuming takeaway meals on adolescents’ overall diet quality scores (Taher et al., 2019). Therefore, one of the factors preventing students from eating a healthy lunch is likely to be the proximity of fast food outlets to secondary schools. Limiting the establishment of new fast food outlets, especially around schools, is a primary goal of health organisations, such as the Chartered Institute for Environmental Health and Department of Health (DOH) (Food Foundation, 2016).
Measuring diet quality is challenging but one validated tool is the Diet Quality Index for Adolescents (DQI-A). It assesses diet quality based on intake of food groups and Food-Based Dietary Guidelines (FBDG) (Huybrechts et al., 2010), without the need for the intensive conversion of foods to nutrients (FAO, 2017, Vyncke et al., 2013). The role of the FBDG are to help individuals to meet their daily dietary requirements by providing guidelines and advice to the public on frequency and portion sizes of specific food groups. These guidelines can also help to provide information for government and other related stakeholders to implement effective interventions toward healthy eating behaviours (FAO, 2016).
Although several UK studies have investigated the effect of having a packed lunch and a school meal on energy intake and individual nutrients of primary (Harrison et al., 2013, Evans et al., 2016) and secondary (Pearce et al., 2013, Prynne et al., 2013) aged students, none has examined the impact of each school lunch type consumed during a school day on British adolescents’ overall diet quality score. The aim of the present study was to evaluate the associations between different types of lunch consumed during a school day and the overall diet quality of UK adolescents using school meals as the reference group. Differences by age were also investigated.
2. Methods
The data were obtained from the National Diet and Nutrition Survey (NDNS) rolling programme years 1–8 (2008–2016). The NDNS is an annual programme that aims to assess the nutritional status of UK people living in private households aged 1·5 years and above. It involves random sampling throughout the year and represents the whole UK population by covering all four regions of the United Kingdom (England, Wales, Scotland and Northern Ireland) (UK Data Service, 2019). All NDNS participants aged 11–18 years and attending secondary school, including Sixth Form colleges, were included. Merging of separate data sets was required to obtain all relevant data.
2.1. Lunch type and food intake
The interviewers asked all participants the following question “On a school/college day, what do you/does (child’s name) usually have for lunch?” to obtain information about the type of lunch being consumed during a school day. The interviewers made it clear that the lunch did not include snacks such as confectionary, crisps or fruit. Also, the interviewers explained that the main information required from this question was the meal consumed and not the time at which this meal was eaten. The options provided in the questionnaire were as follows (1) “cooked school meal”, (2) “Cold school meal (including sandwiches, salads)”, (3) “Packed lunch (from home)”, (4) “Buy lunch from shop/cafe”, (5) “Go home” and (6) “Do not eat lunch”.
All NDNS participants were asked to complete a four-day food diary, and the analysis included only those who completed at least a 3-day record. Food intake was obtained from the 4-day and 3 day diary records which included school and non-school days (for most participants three school days and one weekend day). The diet quality score was calculated for each day, then the mean value of the three and four days was calculated and used to assess the overall diet quality index of each participant. Adolescents completed the diary themselves and were asked to keep a record of all foods and drinks consumed at home or outside the home including leftovers. Commercial toddler drinks and foods items were excluded from the analysis as this age group do not typically consume these foods.
2.2. Diet quality index for adolescents (DQI-A)
In the UK, the latest version of the Food Based Dietary Guidelines (FBDG) is the Eat-well guide, which was published in 2016 by Public Health England (2017). The Eat-well guide consists of seven main food groups, as follows: (1) potatoes, bread, rice, pasta and other starchy carbohydrates; (2) dairy and alternatives; (3) beans, pulses, fish, eggs, meat and other proteins; (4) fruit and vegetables; (5) oil and spreads; (6) water; and (7) confectionary and high fat and sugar snacks (FAO, 2016, Department of Health, 2017). The Flemish FBDG, which was used to validate the DQI-A, includes almost the same recommended food groups mentioned in the Eat-well guide. The DQI-A relies on three main components, namely the (1) Quality, (2) Diversity and (3) Equilibrium of the diet compared to the governmental dietary guidelines. The Diet quality Component (DQc) assesses diet based on the quality of the obtained food within the nine recommended food groups, namely (1) water; (2) bread and cereal; (3) potatoes and grains; (4) vegetables; (5) fruits; (6) milk products; (7) cheese; (8) meat, fish and substitutes and (9) fat and oils. To calculate the score, the amount of consumed food (m) from each food group is multiplied by a weighting factor based on the quality of the food consumed. The Diet Diversity component (DDc) assesses the degree of variation in an adolescent’s diet, where the scoring range is from 0 to 9 points. Consuming at least one serving from each of the nine recommended food groups adds 1 point to the total score. For example, if a participant has a mean consumption for the vegetables group that is more than 80 g, this individual gains a score of one; otherwise, the score will be zero. The Diet Equilibrium component (DEc) consists of two subcomponents: (1) the adequacy component (diet adequacy, DAx) and (2) the excess component (diet excess, DEx). These two subcomponents express the degree of adherence of an adolescent’s diet to the minimum and maximum intakes of each of the nine recommended food groups. The adequacy component represents the percentage of the minimum recommended intake of each of the nine food groups, whereas the excess component represents the percentage of the intake exceeding the upper limit of the recommendation (11 food groups, 9 recommended and 2 non-recommended).
The percentage ranges for both DDc and DEc are 0–100%, whereas the DQc percentage range is –100 to 100%. Therefore, the mean percentage of the three main components, results in a total DQI-A score ranging from –33 to 100%. A higher DQI-A percentage score reflects a better quality of diet. More details on the calculations for each of the components and sub-components can be found elsewhere (Taher et al., 2019, Vyncke et al., 2013).
2.3. Under-reporting
Under-reporting of energy intake (below the minimum recommended intake) of an adolescent with a given gender, age and weight is believed to contribute to biased reporting on habitual intake and food choices (Albar et al., 2014). The physical activity level was not measured for all adolescents to calculate the total energy expenditure in the NDNS. Therefore, the basal metabolic rate (BMR) (MJ/day) was calculated based on the individual weight and using the standard equations of Schofield for each gender [for male: BMR = 0.074 wt + 2.754; and for female: BMR = 0.056 wt + 2.898]. In addition, based on multiples of BMR, provisional cut-off points (minimum and maximum) were used to identify those adolescents who were under-reporting their energy intake [for male and female aged 6–18 years: 1.39 − 2.24 × BMR, and 1.30 – 2.10 × BMR, respectively] (Albar et al., 2014). However, no participants were excluded based on their level of under-reporting.
2.4. Statistical analysis
All statistical analyses were carried out using Stata statistical software, version 15·0 (College Station, TX: Stata Corp LLC). The data was weighted to adjust for nonresponses and to ensure the data was representative for the UK. The percentage of males and females and ethnicity (white/non-white) were presented. The mean age in years, energy intake in kJ, weight in kg, overall DQI-A% and percentage of students underreporting their energy intake were also calculated for both males and females and for two age groups (11–14 and 15–18 years). A Directed Acyclic Graph (DAG) (Textor et al., 2016) (Supplemental Fig. 1) with type of lunch consumed on a school day as the main exposure and Diet quality index and its components and sub-components (continuous) as the outcome was generated to predict confounding variables. According to minimal sufficient adjustment sets; age (years), region, under-reporting energy intake, equivalised household income, reduced price or subsidised school meal (at lunchtime) and gender (male/female) were needed to estimate the effect of lunch on a school day on DQI-A and its components.
Linear and multiple regression analyses were conducted. The analyses were stratified by age group (11–14 and 15–18 years) taking into account the clustering effect resulting from the 3 and 4-day diary records. The residuals were plotted against fitted values of the predicted variable to check assumptions for regression were met. P-values of <0.05 were considered as statistically significant for all tests, and 95% confidence intervals were presented with results. The number of adolescents consuming each lunch type were analysed by age. Diet quality components and subcomponents were reported for each lunch type. Changes in overall DQI-A% score and percentage of consumption of lunch type were assessed over time; the assessment was smoothed by combing the results of two survey years together (Supplemental Fig. 2).
3. Results
A total of 2118 adolescents were included in the analysis, Table 1. From the initial sample, 469 were excluded due to attending primary not secondary school. Ninety-eight percent of participants had 4-day diary records. The proportion of females was slightly higher than that of males, at 52% (n = 1096) and 48% (n = 1022), respectively; the mean age of both genders was 14.4 years. In terms of ethnicity, out of 1206 adolescents who included information; 91% of them reported being white. The overall mean weight was 57.4 kg, and males had a higher weight than females. The overall mean intake of food energy was 7370 kJ, and males also had a higher energy intake than females. The percentage of under-reporters was high overall at 73.0% and was higher in the older age group for both males (78.6%) and females (76.8%) (Table 1). In addition, the frequency of consumption of reported lunch type differed by under-reporting status. Although the overall DQI-A was not significantly associated with under-reporting, some of the components and subcomponents were significantly impacted in both age groups.
Table 1.
Summary description of age, weight, food energy intake and percentage of under-reporting energy intake among adolescents (11–18 years) from the National Diet and Nutrition Survey (NDNS).
| Total sample n = 2118 |
Age group 11–14 years |
Age group 15–18 years |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males |
Females |
Males |
Females |
||||||||||||
|
n = 521 |
n = 545 |
n = 501 |
n = 551 |
||||||||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | ||||||
| Age (years) | 14.5 | 14.4 | 14.6 | 12.8 | 12.7 | 12.9 | 12.8 | 12.7 | 12.9 | 16.2 | 16.1 | 16.3 | 16.2 | 16.1 | 16.3 |
| Weight (kg) | 57.4 | 56.6 | 58.2 | 53.0 | 51.8 | 54.2 | 53.3 | 52.1 | 54.4 | 69.1 | 67.8 | 70.4 | 62.6 | 61.4 | 63.7 |
| Food energy (kJ) | 7370.3 | 7278.6 | 7461.9 | 7806.4 | 7635.7 | 7977.1 | 6685.2 | 6535.3 | 6835.0 | 8519.1 | 8308.0 | 8730.2 | 6590.9 | 6440.3 | 6741.5 |
| Under-reporter EI* (%) | 73.04 | 71.1 | 74.9 | 70.6 | 66.7 | 74.6 | 66.7 | 62.4 | 70.4 | 78.6 | 75.04 | 82.2 | 76.8 | 73.2 | 80.3 |
| Overall DQI-A% | 21.1 | 20.5 | 21.8 | 20.6 | 19.3 | 21.9 | 20.6 | 19.3 | 21.8 | 20.7 | 19.3 | 22.2 | 22.5 | 21.2 | 23.8 |
CI, Confidence Interval, EI, Energy Intake.
All but 5 participants provided information on type of lunch consumed. Eating lunch at home or skipping lunch were reported by <5% of participants. Purchasing cold school meals and buying lunch from shops or cafes (takeaway meals) was reported by 12.8% and 17.4% of participants, respectively. The remaining participants reported having a cooked school meal (28.3%) or bringing a packed lunch from home (36.6%). Less than 10% of the total (5.5% and 2.9% of cooked and cold school meals consumers respectively) reported they were receiving free school meals or reduced-price meals at lunchtime; therefore, the free school meal variables were excluded from the model.
The overall mean DQI-A score was 21.1% and varied across different lunch types (Table 2). Although few adolescents reported not eating lunch on a school day (n = 37), these participants had the second lowest mean DQI-A% score at 18.9%, whereas shop/café-bought lunch consumers (n = 369) had the lowest DQI-A% score at 14.8%. Participants who consumed cooked (n = 600) and cold (n = 272) school meals and having lunch at home (n = 59) had a relatively higher percentage for the overall DQI-A score with 21.8, 20.5 and 21.5%, respectively. Adolescents who brought packed lunches (n = 776) from home had the highest score at 23.9%. The overall mean DQI-A score varied across the four days recorded according to the type of usual lunch type reported by the students (Table 3). No significant differences were observed in the overall diet quality score between male and female students (Table 3).
Table 2.
Summary description of overall diet quality index and its component and sub-component scores, age and energy intake according to type of meal usually consumed during school lunch among British adolescents aged 11–18 years (n = 2118) from the National Diet and Nutrition Survey (NDNS) rolling programme, Years 1–8 (2008–2016).
| Dietary quality* | Total sample |
Cooked school meal |
Cold school meal |
Packed lunch (from home) |
Buy lunch from shop/cafe |
Go home |
Do not eat lunch |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
n = 2118 |
n = 600 |
n = 272 |
n = 776 |
n = 369 |
n = 59 |
n = 37 |
|||||||||||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | ||||||||
| DQI-A Overall | 21.1 | 20.5 | 21.8 | 21.8 | 20.6 | 23.0 | 20.5 | 18.8 | 22.2 | 23.9 | 22.8 | 24.9 | 14.8 | 13.2 | 16.3 | 21.5 | 17.0 | 26.0 | 18.9 | 12.9 | 25.0 |
| (DQc) | −4.3 | −5.7 | −3.0 | −2.4 | −4.9 | 0.1 | −5.3 | −9.1 | −1.6 | −0.1 | −2.3 | 2.1 | −15.9 | −19.2 | −12.6 | −3.1 | −13.0 | 6.9 | −4.2 | 17.1 | 8.6 |
| (DDc) | 44.5 | 44.0 | 45.0 | 44.7 | 43.7 | 45.7 | 43.9 | 42.6 | 45.3 | 46.5 | 45.6 | 47.5 | 40.6 | 39.3 | 41.8 | 45.7 | 42.3 | 49.1 | 39.2 | 34.8 | 43.7 |
| (DEc) | 23.2 | 22.8 | 23.5 | 23.2 | 22.5 | 23.8 | 22.8 | 21.9 | 23.6 | 25.2 | 24.6 | 25.7 | 19.6 | 18.8 | 20.4 | 21.9 | 19.7 | 24.0 | 21.8 | 19.0 | 24.6 |
| (DAx) | 53.5 | 53.0 | 53.9 | 53.7 | 52.8 | 54.5 | 53.0 | 51.8 | 54.2 | 55.6 | 54.8 | 56.3 | 49.8 | 48.8 | 50.9 | 52.3 | 49.5 | 55.1 | 48.5 | 45.4 | 51.7 |
| (DEx) | 20.6 | 20.3 | 20.9 | 20.8 | 20.2 | 21.3 | 20.6 | 19.7 | 21.5 | 20.3 | 19.8 | 20.8 | 21.1 | 20.4 | 21.9 | 21.0 | 19.1 | 22.8 | 17.9 | 15.8 | 20.1 |
| Age (years) | 14.5 | 14.4 | 14.6 | 13.8 | 13.7 | 14.0 | 14.3 | 14.1 | 14.5 | 14.3 | 14.2 | 14.5 | 15.7 | 15.5 | 15.9 | 15.9 | 15.5 | 16.4 | 15.4 | 14.9 | 15.9 |
| Energy (KJ) | 7370.3 | 7278.6 | 7461.9 | 7493.0 | 7321.1 | 7665.0 | 7348.8 | 7080.8 | 7616.8 | 7303.7 | 7161.0 | 7446.4 | 7396.8 | 7153.4 | 7640.2 | 7368.9 | 6795.9 | 7941.9 | 6783.4 | 6223.9 | 7342.9 |
CI, Confidence Interval; DQI-A, Diet Quality Index for Adolescents; DQc, Diet quality component; DDc, Diet diversity component; DEc, Diet equilibrium component; DAx, Diet adequacy sub-component; DEx, Diet excess sub-component.
*Scores presented as %.
Table 3.
The diet quality score across all days for each participant according to the type of usual lunch type reported and differences in the overall diet quality score by gender.
| What do you usually have for lunch? | Mean overall DQI-A% |
Overall diet quality score (mean of all days recorded) |
Gender differences in the overall diet quality score (meal of all days recorded) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Day Number | |||||||||
| Day 1 |
Day 2 |
Day 3 |
Day 4 |
||||||
| n = 2118 | n = 2118 | n = 2118 | n = 2084 | n = 2118 |
n = 2118 |
||||
| Male as reference group | |||||||||
| Cooked school meal | 22.3 | 22.4 | 21.3 | 21.3 | 21.8 | B | CI | P-value | |
| −0.4 | −2.8 | 1.9 | 0.7 | ||||||
| Cold school meal | 20.6 | 20.8 | 20.4 | 20.0 | 20.5 | B | CI | P-value | |
| −0.3 | −3.7 | 3.2 | 0.9 | ||||||
| Packed lunch (from home) | 25.3 | 23.9 | 23.2 | 23.1 | 23.8 | B | CI | P-value | |
| 0.9 | −1.3 | 3.0 | 0.4 | ||||||
| Buy lunch from shop/café | 16.3 | 14.6 | 14.6 | 13.7 | 14.8 | B | CI | P-value | |
| 1.8 | −1.3 | 4.9 | 0.2 | ||||||
| Go home | 22.4 | 23.3 | 21.4 | 19.2 | 21.6 | B | CI | P-value | |
| −1.6 | −10.7 | 7.5 | 0.7 | ||||||
| Do not eat lunch | 16.7 | 19.4 | 22.2 | 18.1 | 19.1 | B | CI | P-value | |
| 0.5 | −11.8 | 12.8 | 0.9 | ||||||
The results from the regression analysis indicated an association between school lunch type and overall diet quality over the 4 days which included school and non-school days. In the older age group of 15–18 year old participants, after adjusting for confounders, significant differences were observed between consumption of cooked school meals (reference group) and packed lunches and shop/café-bought lunches in DQI-A scores (Table 5). The results for the younger age group of 11–14 year old participants were attenuated and significant differences were only observed between consumption of cooked school meals and shop/café lunches and not for packed lunches compared to school meals (Table 4). For older adolescents, consuming a packed lunch had a 5.5% (95% CI 2.7, 8.4%; P < 0.01) higher overall DQI-A score than consuming a cooked school meal. Conversely, consuming a shop/café-bought lunch had a 5.0% (95% CI −8.1, −2.0%, p < 0.01) lower overall DQI-A% than consuming a cooked school meal. For younger students the diet quality score was 6.6% (95% CI −10.2, −3.1%; p < 0.01) lower for shop/café lunches. No significant differences were observed between adolescents who reported to have a cooked school meal and those who had a cold school meal, lunch at home or did not have lunch in both age groups (Table 4, Table 5).
Table 5.
Regression (clustered) analysis between Diet quality index and its components and subcomponents and type of lunch consumed on a school day for older adolescents aged 15–18 years from the NDNS rolling programme (Years 1–8).
| Adjusted* analysis | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cooked school meals as reference group | Cold school meal |
Packed lunch (from home) |
Buy lunch from shop/cafe |
Lunch at home |
Do not eat lunch |
|||||||||||||||
| B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | ||||||
| DQI-A % | −0.8 | −4.5 | 2.9 | 0.7 | 5.5 | 2.7 | 8.4 | <0.01 | −5.0 | −8.1 | −2.0 | <0.01 | 3.9 | −1.6 | 9.3 | 0.2 | −0.9 | −8.6 | 6.8 | 0.8 |
| DQc % | −1.6 | −9.4 | 6.3 | 0.7 | 8.9 | 3.1 | 14.7 | <0.01 | −10.0 | −16.2 | −3.7 | <0.01 | 8.0 | −5.1 | 21.1 | 0.2 | 4.2 | −12.8 | 21.3 | 0.63 |
| DDc % | −0.6 | −3.5 | 2.4 | 0.7 | 4.2 | 1.8 | 6.5 | <0.01 | −3.2 | −5.7 | −0.6 | <0.01 | 3.0 | −0.8 | 6.7 | 0.1 | −6.4 | −12.0 | −0.8 | 0.02 |
| DEc % | −0.2 | −2.2 | 1.7 | 0.8 | 3.6 | 2.1 | 5.0 | <0.01 | −2.0 | −3.6 | −0.4 | <0.01 | 0.6 | −2.0 | 3.2 | 0.6 | −0.5 | −3.8 | 2.8 | 0.8 |
| DAx % | −0.7 | −2.9 | 1.5 | 0.5 | 3.3 | 1.6 | 5.1 | <0.01 | −2.8 | −4.7 | −0.8 | <0.01 | 0.6 | −2.5 | 3.6 | 0.7 | −5.7 | −9.4 | −2.1 | <0.01 |
| DEx % | −0.3 | −1.8 | 1.1 | 0.7 | −0.8 | −2.0 | 0.3 | 0.2 | −0.2 | −1.5 | 1.0 | 0.7 | −0.1 | −2.3 | 2.0 | 0.9 | −4.2 | −7.2 | −1.2 | 0.01 |
CI, Confidence Interval; DQI-A, Diet Quality Index for Adolescents; DQc, Diet quality component; DDc, Diet diversity component; DEc, Diet equilibrium component; DAx, Diet adequacy sub-component; DEx, Diet excess sub-component,
*Adjusted for gender, Region, energy under-reporting and equivalised household income.
Table 4.
Regression (clustered) analysis between Diet quality index and its components and subcomponents and type of lunch consumed on a school day for younger adolescents aged 11–14 years from the NDNS rolling programme (Years 1–8).
| Adjusted* analysis | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cooked school meals as reference group | Cold school meal |
Packed lunch (from home) |
Buy lunch from shop/cafe |
Lunch at home |
Do not eat lunch |
|||||||||||||||
| B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | ||||||
| DQI-A % | −1.7 | −4.4 | 1.1 | 0.2 | −0.8 | −2.9 | 1.3 | 0.46 | −6.6 | −10.2 | −3.1 | <0.01 | −5.1 | −16.9 | 6.7 | 0.4 | −0.5 | −12.0 | 11.0 | 0.9 |
| DQc % | −4.9 | −10.7 | 0.9 | 0.1 | −4.3 | −8.8 | 0.1 | 0.1 | −13.0 | −20.6 | −5.4 | <0.01 | −12.2 | −33.9 | 9.5 | 0.3 | −1.8 | −23.4 | 19.8 | 0.87 |
| DDc % | −0.1 | −2.4 | 2.2 | 0.9 | 0.9 | −0.8 | 2.6 | 0.30 | −4.2 | −7.2 | −1.2 | <0.01 | −2.5 | −11.7 | 6.7 | 0.6 | −0.1 | −9.5 | 9.4 | 0.99 |
| DEc % | 0.1 | −1.4 | 1.6 | 0.9 | 1.0 | −0.1 | 2.1 | 0.1 | −2.8 | −4.8 | −0.8 | 0.01 | −0.8 | −7.4 | 5.8 | 0.8 | 0.4 | −5.9 | 6.6 | 0.9 |
| DAx % | 0.8 | −1.1 | 2.7 | 0.4 | 2.2 | 0.8 | 3.6 | <0.01 | −2.5 | −4.9 | −0.1 | <0.01 | −0.6 | −8.2 | 7.0 | 0.9 | 0.6 | −6.4 | 7.6 | 0.87 |
| DEx % | 0.6 | −0.6 | 1.8 | 0.4 | 0.8 | −0.1 | 1.6 | 0.1 | 0.8 | −0.8 | 2.3 | 0.3 | 0.3 | −4.0 | 4.6 | 0.9 | 0.1 | −2.7 | 2.9 | 0.94 |
CI, Confidence Interval; DQI-A, Diet Quality Index for Adolescents; DQc, Diet quality component; DDc, Diet diversity component; DEc, Diet equilibrium component; DAx, Diet adequacy sub-component; DEx, Diet excess sub-component
*Adjusted for gender, region, energy under-reporting and equivalised household income.
In addition, for older adolescents significant differences were observed between cooked school meal consumers and packed lunches and shop/café-bought lunch consumers for most of the DQI-A components and subcomponents. For example, packed lunch consumers had a higher DQc%, DDc%, DEc% and DAx% than cooked school meal consumers among the older age group while the results for the younger age group were attenuated and not statistically significant for all subcomponents (Table 4, Table 5). Furthermore, shop/café-bought lunch consumers had a significantly lower DQc%, DDc%, DEc% and DAx% than cooked school meal consumers among both age groups (Table 4, Table 5). No statistically significant differences were observed between cooked school meal consumers and cold school meal or lunch at home consumers for any of the diet quality components and sub-components in either age group. Unadjusted analyses produced similar results to the adjusted analyses with attenuated results for some of the subcomponents among both age groups (Supplemental Table 1 and 2).
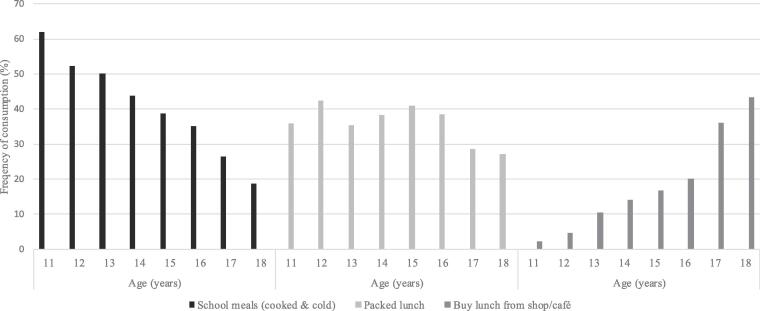
The percentage of students consuming the most common types of lunch during a school day varied by age (Fig. 1). The number of students consuming school meals (cooked and cold) decreased as age increased. Conversely, the number of students consuming shop/café-bought lunch increased with age. The percentage of packed lunch consumers fluctuated between the age of 11 and 16 years and dropped at age 17 and 18 years.
Fig. 1.
Frequency of consumption of the most common types of school lunch on a school day by adolescent’s age from the NDNS rolling programme (Years 1–8).
4. Discussion
This is the first study to evaluate the associations between type of school lunch and overall diet quality in adolescents using representative national UK data. The results suggest that the type of school lunch consumed is associated with overall diet quality and adolescents consuming lunches from cafes or shops have the worst diet quality. For older children, packed lunch consumers had the highest overall diet quality score, closely followed by school meals but this was not the case for younger children where no differences were observed between cooked schools meals and packed lunches. In addition, the consumption of shop/café-bought lunches increases with age, whereas the consumption of school meals decreases.
4.1. Comparison between school meals and packed lunches
The impact of school lunch type on diet quality appears to vary by age. Previous research in younger children indicates that children between 5 and 11 years having a school meal have a better diet quality and nutrient intake than packed lunch consumers (food brought from home) both in the UK (Evans et al., 2016) and in the US (Vernarelli and O'Brien, 2017). Previous evidence from secondary schools in England reported that school meals are better quality than packed lunches although they only looked at lunchtime intakes and not intakes over the whole day (Pearce et al., 2013). Although school meals improved after the introduction of standards in 2008–9 both in younger (Wickramasinghe et al., 2017) and older age groups (Prynne et al., 2013), studies show that both packed and school lunches of secondary school students fail to provide the recommended levels of energy and nutrients (Stevens et al., 2013) and therefore both types of meals are typically poor quality. Nevertheless, diet quality has continued to increase (2008–2015; Supplemental Fig. 2) since the revised version of the school food standards were introduced in January 2015 in the vast majority of schools (Pearce et al., 2013, Stevens et al., 2013, Browne et al., 2017) when food-based standards were maintained but nutrient-based standards were dropped.
Previous studies (Pearce et al., 2013, Stevens et al., 2013) comparing the quality of school lunches and packed lunches among secondary school students did not take into consideration the effect of age. Interestingly, the results from this study show that diet quality in younger students differs little by lunch type, while for older adolescents those consuming packed lunches have a higher overall diet quality score compared with school meal consumers. This corresponds well with previous research indicating that in secondary school, packed lunches from home contain more fruits, wholemeal bread, cheese and red meat than school lunches whereas high calorie beverages, chips and meat products are consumed more frequently as part of a school meal (Browne et al., 2017). Students who receive a free school meal may be more likely to choose dishes with more nutritional value during that day at school (Ensaff et al., 2013). In this study, <10% of the students reported having a free school meal and therefore this was not explored in detail.
The lack of a difference between school meals and packed lunches in secondary school students compared with primary schools could be due to the differences in the style of operation between these schools in the UK (Prynne et al., 2013, Stevens et al., 2013). Menus in secondary schools have a much wider selection of foods available for children to choose from, compared to primary schools allowing secondary students to choose food from a wider range of items for their lunch with different prices and nutritional content for each of the selected food item. A study of two secondary schools that held “National Healthy Schools Status”, showed that the main food items being selected by the adolescent's students during lunch at school were Pizza, Pasta, sandwiches, desserts and beverages while <10% of the students selected the healthier options (Ensaff et al., 2013). Furthermore, a higher proportion of secondary school students prefer to bring their own packed lunch to school (Addis and Murphy, 2019) compared to younger age groups. It is known that in many countries including the UK and US, parents and carers have a large role in preparing packed lunches for younger children to consume at school (Nathan et al., 2019). Conversely, older adolescents prefer to make their own food choices which reflects the smaller role of carers on preparation of packed lunches for 15–18 year old (Addis and Murphy, 2019). Educating students to choose healthier options from the food available at school is needed and may have an impact on improving the overall diet quality (Pearce et al., 2013).
4.2. Comparisons between lunch purchased inside and outside school
The number of older adolescents who consume school meals decreases with age with the number leaving the premises during lunchtime increasing with age (Public Health England, 2014). This is mainly due to students preferring to have control of their food choice (Prynne et al., 2013, Addis and Murphy, 2019, Macdiarmid et al., 2015). This may confirm the fact that the food environment and student’s preferences have a large impact on food and beverage (Ensaff et al., 2016) choices, particularly among adolescent students despite the restrictions introduced by the UK school food standards (Browne et al., 2017). Indeed, in this study, about 17% of students bought lunches from a café or a shop and both age groups had the lowest overall diet quality and the lowest score among all diet quality components and sub-components, except Diet excess sub-component (DEx). Similar results were reported from studies in Northern England (McInnes and Blackwell,), the Republic of Ireland (Browne et al., 2017) and Canada (Tugault-Lafleur et al., 2018).
In the UK, secondary schools have independent policies on whether they allow students to leave the school site during the lunch break (UK Government and Parliament, 2016) hence regulating accessibility of outlets. Students have a limited period of time to purchase and consume lunch and the number of food outlets located within a 10 min walk varies from one school to another (Crawford et al., 2017). The majority of purchases made from convenience foods and local shops such as fish and chip shops, cafes, pizzerias, kebab shops and supermarkets during the lunch break are unhealthy foods high in fats, sugars and salt [2633]. The lower diet quality score of adolescents purchasing food from shops and cafes indicates that this lunch choice on school days has a sufficient negative impact on an adolescent’s diet to impact overall diet quality. One study (Sinclair and Winkler, 2008) reported that around 23% of the recommended energy intake of secondary school students was obtained from foods purchased from fringe shops. This study also found that the nutritional quality of the purchased food items was found to comprise 38% saturated fat, 22% sugar and 15% non-milk extrinsic sugar (Sinclair and Winkler, 2008). A reduction in diet quality of 6.6% for younger students and 5.0% for older students seen in this study is substantial. The DQI-A score typically reduces by about 3% for each reduction of a portion of vegetables or other healthy food component (Taher et al., 2019). For example, students reported to consume meals from takeaway shops and cafes may consume less fruit, vegetables and milk and more of non-recommended food groups such as soft drinks, french fries, crisps, fried chicken and confectionary products and therefore will have a lower DQc and higher DEx.
4.3. Limitations
This study has limitations mainly due to the cross-sectional and observational nature of the data as well as the difficulties of measuring diet quality. In addition, the source of the food consumed outside of the home was not mentioned for all types of food consumed (Taher et al., 2019), and in this study school meals (of all types) may be considered as one source of the out of home meals. The percentages of adolescents reporting buying lunch from a café and shop were 23.5% and 17.4% for those that completed 3-day and 4-day diaries respectively. Similarly, the percentages of adolescents reporting consuming cooked school meals were 47.1% and 28.1% for those that completed 3-day and 4-day diaries respectively. Factors that could have affected the validity of the results include using reported information on lunch type. Adolescents may have had a mixture of lunches in one week but because data was collected for less than a whole week it was not possible to solely rely on the information collected during the four days to assess intakes of each type of lunch during a school day. If the adolescents who only collected data for 3 days were excluded, the results may have been different from participants providing complete data, introducing further bias. In addition, when the participants reported the place where the food was actually eaten, the majority (59.6%) reported consuming food at home while 17.7% and 11.4% reported eating the food at school and takeaway outlets, respectively. The school lunch only contributes about a third of the overall diet on a school day (Harrison et al., 2013), where the food can also be consumed for example on the way to and from school. However, improving lunches consumed during the school day may also improve the overall diet quality of those students (Harrison et al., 2013). Also, in year 1, more weekend days were included in the study compared with other years of the survey, which may be considered to have an impact on estimates but are likely to under-estimate the impact of lunch type on diet quality.
4.4. Recommendations
Policies already exist in the UK to improve the quality of food sold within schools although many students choose not to purchase healthy foods offered such as fruits and vegetables. Packed lunches are rarely regulated although they are similar in quality to school food for this age group. Less attention has focussed on improving the food environment outside schools compared to inside. Some cities are however introducing policies to restrict easy access to high-density foods (Public Health England, 2014). Some authorities have plans in place to control the over-clustering of hot food takeaways near schools (Public Health England, 2014) although due to the lack of evidence demonstrating the effects of opening a takeaway shop close to schools, others such as Bristol, have recommended allowing the establishment of Hot Food Takeaways within a 400 m radius from premises where young people are gathering (Bristol-City-Council, 2017). The findings of this study point to strategies to prevent the over-clustering of takeaway outlets around schools, given that they may encourage students to eat unhealthy foods, reducing diet quality and potentially increasing risk of obesity (Food Foundation, 2016).
5. Conclusions
UK adolescents consume a poor quality diet and the type of lunch they choose on school days is important. Purchasing foods from shops and cafes outside school, for their lunch, has a negative impact on their diet quality score compared with choosing a school meal or packed lunch among both age groups. The results also highlight the importance of focusing on older adolescents as their packed lunches had a higher overall diet quality score compared with school meals, unlike younger adolescents. These results suggest that for secondary school children, unlike younger school children, regulation policies focussing on food outlets including shops near secondary schools are needed in addition to improvements in school meals.
6. Funding source
The research was funded by the University of Leeds, UK
7. Ethics committee approval
No separate ethics approval was needed for this secondary analysis
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101133.
Contributor Information
Ayyoub K. Taher, Email: fy06akt@leeds.ac.uk, aktaher@kisr.edu.kw.
Hannah Ensaff, Email: H.Ensaff@leeds.ac.uk.
Charlotte E.L. Evans, Email: C.E.L.Evans@leeds.ac.uk.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Addis S., Murphy S. 'There is such a thing as too healthy!' The impact of minimum nutritional guidelines on school food practices in secondary schools. J. Hum. Nutr. Diet. 2019;32(1):31–40. doi: 10.1111/jhn.12598. PubMed PMID: 30253441. [DOI] [PubMed] [Google Scholar]
- Albar S.A., Alwan N.A., Evans C.E.L. Is there an association between food portion size and BMI among British adolescents? Br. J. Nutr. 2014;112(5):841–851. doi: 10.1017/S0007114514001548. [DOI] [PubMed] [Google Scholar]
- Bristol City Council, 2017. Neighbourhoods Scrutiny 2017 [cited 2017 7 December]. Available from: https://democracy.bristol.gov.uk/documents/s13120/10hotfoodtakeawayscompletereport.pdf.
- British Nutrition Foundation. Food provision 2020 [cited 2020 27 January]. Available from: https://www.nutrition.org.uk/foodinschools/foodprovision/food-provision.html.
- Browne S., Staines A., Barron C. School lunches in the Republic of Ireland: a comparison of the nutritional quality of adolescents’ lunches sourced from home or purchased at school or ‘out’ at local food outlets. Public Health Nutr. 2017;20(3):504–514. doi: 10.1017/S1368980016001944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford F., Mackison D., Mooney J.D. Observation and assessment of the nutritional quality of 'out of school' foods popular with secondary school pupils at lunchtime. BMC Public Health. 2017;17(1):887. doi: 10.1186/s12889-017-4900-9. PubMed PMID: 29149874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department for Education, 2019. Schools, pupils and their characteristics: January 2019 Department of Health2019 [cited 2019 25 June]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/812539/Schools_Pupils_and_their_Characteristics_2019_Main_Text.pdf.
- Department for Education. School food in England: Departmental advice for governing boards 2019 [cited 2019 1 February]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/551813/School_food_in_England.pdf.
- Department of Health, 2017. Guidance: The Eatwell Guide 2017 [cited 2017 19 January]. Available from: https://www.gov.uk/government/publications/the-eatwell-guide.
- Ensaff H., Russell J., Barker M.E. Meeting school food standards – students’ food choice and free school meals. Public Health Nutr. 2013;16(12):2162–2168. doi: 10.1017/S1368980012005575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ensaff H., Russell J., Barker M.E. Adolescents’ beverage choice at school and the impact on sugar intake. Eur. J. Clin. Nutr. 2016;70(2):243–249. doi: 10.1038/ejcn.2015.158. [DOI] [PubMed] [Google Scholar]
- Evans C.E.L, Mandl V., Christian M.S. Impact of school lunch type on nutritional quality of English children’s diets. Public Health Nutr. 2016;19(1):36–45. doi: 10.1017/S1368980015000853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO, 2016. Food-based dietary guidelines 2016 [cited 2016 14 December]. Available from: http://www.fao.org/nutrition/nutrition-education/food-dietary-guidelines/en/.
- FAO, 2017. Measuring Diet Quality: Where we are and where we might want to go: Terri Ballard; 2017 [cited 2017 23 January]. Available from: http://www.fao.org/search/en/?cx=018170620143701104933%3Aqq82jsfba7w&q=DQI&cof=FORID%3A9.
- Food Foundation, 2016. Food Environment Policy Index: Policy Briefing 2016 [cited 2017 13 February]. Available from: http://foodfoundation.org.uk/publications.
- Harrison F., Jennings A., Jones A. Food and drink consumption at school lunchtime: the impact of lunch type and contribution to overall intake in British 9–10-year-old children. Public Health Nutr. 2013;16(6):1132–1139. doi: 10.1017/S1368980011002321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huybrechts I., Vereecken C., De Bacquer D. Reproducibility and validity of a diet quality index for children assessed using a FFQ. Br. J. Nutr. 2010;104(1):135–144. doi: 10.1017/S0007114510000231. [DOI] [PubMed] [Google Scholar]
- Macdiarmid J.I., Wills W.J., Masson L.F. Food and drink purchasing habits out of school at lunchtime: a national survey of secondary school pupils in Scotland. Int. J. Behav. Nutr. Phys. Act. 2015;12(1) doi: 10.1186/s12966-015-0259-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McInnes, A, Blackwell, D., 2017. Self-reported perceptions of weight and eating behavior of school children in Sunderland, England. Front Public Health 14;5. PubMed PMID: WOS:000408412900001. English. [DOI] [PMC free article] [PubMed]
- Nathan N., Janssen L., Sutherland R. The effectiveness of lunchbox interventions on improving the foods and beverages packed and consumed by children at centre-based care or school: a systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2019;16(1) doi: 10.1186/s12966-019-0798-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce J., Wood L., Nelson M. Lunchtime food and nutrient intakes of secondary-school pupils; a comparison of school lunches and packed lunches following the introduction of mandatory food-based standards for school lunch. Public Health Nutr. 2013;16(6):1126–1131. doi: 10.1017/S1368980012003928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prynne C.J., Handford C., Dunn V. The quality of midday meals eaten at school by adolescents; school lunches compared with packed lunches and their contribution to total energy and nutrient intakes. Public Health Nutr. 2013;16(6):1118–1125. doi: 10.1017/S1368980011002205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health England . HM Government; UK: 2014. Healthy people, healthy places briefing Obesity and the environment: regulating the growth of fast food outlets. [Google Scholar]
- Sahota P., Woodward J., Molinari R. Factors influencing take-up of free school meals in primary- and secondary-school children in England. Public Health Nutr. 2014;17(6):1271–1279. doi: 10.1017/S136898001300092X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair S., Winkler J.T. London Metropolitan University, Nutrition Policy Unit; London: 2008. The School Fringe: What Pupils Buy and Eat from Shops Surrounding Secondary Schools. [Google Scholar]
- Stevens L., Nicholas J., Wood L. School lunches v. packed lunches: a comparison of secondary schools in England following the introduction of compulsory school food standards. Public Health Nutr. 2013;16(6):1037–1042. doi: 10.1017/S1368980013000852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taher A.K, Evans N., Evans C.E. The cross-sectional relationships between consumption of takeaway food, eating meals outside the home and diet quality in British adolescents. Public Health Nutr. 2019;22(1):63–73. doi: 10.1017/S1368980018002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Textor, J., van der Zander, B., Gilthorpe, M.S., et al., 2016. Robust causal inference using directed acyclic graphs: the R package 'dagitty', Int. J. Epidemiol. 45(6), 1887–1894. PubMed PMID: WOS:000398261100024. English. [DOI] [PubMed]
- Tugault-Lafleur C.N., Black J.L., Barr S.I. Lunch-time food source is associated with school hour and school day diet quality among Canadian children. J. Hum. Nutr. Diet. 2018;31(1):96–107. doi: 10.1111/jhn.2018.31.issue-1. [DOI] [PubMed] [Google Scholar]
- UK Data Service, 2019. National Diet and Nutrition Survey Years 1-9, 2008/09-2016/17 2019 [cited 2018 21 December]. Available from: https://beta.ukdataservice.ac.uk/datacatalogue/studies/study?id=6533.
- UK Government and Parliament, 2016. Allow Secondary School Students to leave school for lunch 2016 [cited 2016 1 December]. Available from: https://petition.parliament.uk/petitions/130923.
- Vernarelli, J.A., O'Brien, B., 2017. A vote for school lunches: school lunches provide superior nutrient quality than lunches obtained from other sources in a nationally representative sample of US children. Nutrients 9(9). PubMed PMID: WOS:000411973200007. English. [DOI] [PMC free article] [PubMed]
- K. Vyncke, E.C. Fernandez, M. Fajo-Pascual, et al. Validation of the Diet Quality Index for Adolescents by comparison with biomarkers, nutrient and food intakes: the HELENA study. Brit. J. Nutr. 2013 Jun 14;109(11):2067–2078. PubMed PMID: WOS:000319126700018. English. [DOI] [PubMed]
- Wickramasinghe K., Rayner M., Goldacre M. Environmental and nutrition impact of achieving new School Food Plan recommendations in the primary school meals sector in England. BMJ Open. 2017;7(4):e013840. doi: 10.1136/bmjopen-2016-013840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- W. Wills, G. Danesi, A.B. Kapetanaki, et al. Socio-economic factors, the food environment and lunchtime food purchasing by young people at secondary school. Int. J. Env. Res. Pub. He. 2019 May 1;16(9). PubMed PMID: WOS:000469517300130. English. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.