Abstract
The network approach to psychopathology posits that mental disorders can be conceptualized and studied as causal systems of mutually reinforcing symptoms. This approach, first posited in 2008, has grown substantially over the past decade and is now a full-fledged area of psychiatric research. In this article, we provide an overview and critical analysis of 363 articles produced in the first decade of this research program, with a focus on key theoretical, methodological, and empirical contributions. In addition, we turn our attention to the next decade of the network approach and propose critical avenues for future research in each of these domains. We argue that this program of research will be best served by working toward two overarching aims: (a) the identification of robust empirical phenomena and (b) the development of formal theories that can explain those phenomena. We recommend specific steps forward within this broad framework and argue that these steps are necessary if the network approach is to develop into a progressive program of research capable of producing a cumulative body of knowledge about how specific mental disorders operate as causal systems.
The network approach to psychopathology began a decade ago with a simple hypothesis: symptoms may cohere as syndromes because of causal relations among the symptoms themselves (Borsboom, 2008, Cramer et al., 2010a). From this perspective, symptoms are not passive indicators of a latent “common cause”; they are agents in a causal system (Borsboom, 2008, Kendler, 2016, Kendler et al., 2011). This hypothesis has proven generative, stimulating a growing body of theoretical, methodological, and empirical work predicated on the idea that mental disorders can be characterized as complex systems in which symptoms play an active causal role (Fried et al., 2017, McNally, 2016). In this paper, we provide an overview of the first decade of this “network approach” to psychopathology and consider directions forward for this research.
Literature Review.
We began by identifying articles within this literature. A description of our literature search and a PRISMA diagram appear in Supplementary Materials. Briefly, we identified articles using keyword searches and citation records in ISI Web of Science, PsycINFO, and PubMed and reference lists from prior reviews. This search produced 1656 unique records, 924 of which were screened out, most commonly because they pertained to another domain of network analysis (e.g., protein interaction networks). The remaining 732 articles were assessed for eligibility. An article was eligible if it addressed a psychiatric phenomenon and incorporated the perspective of the network approach. To facilitate this determination, we first identified articles as being principally theoretical, methodological, or empirical. We deemed 363 articles eligible, including 98 theoretical, 61 methodological, and 204 empirical articles.
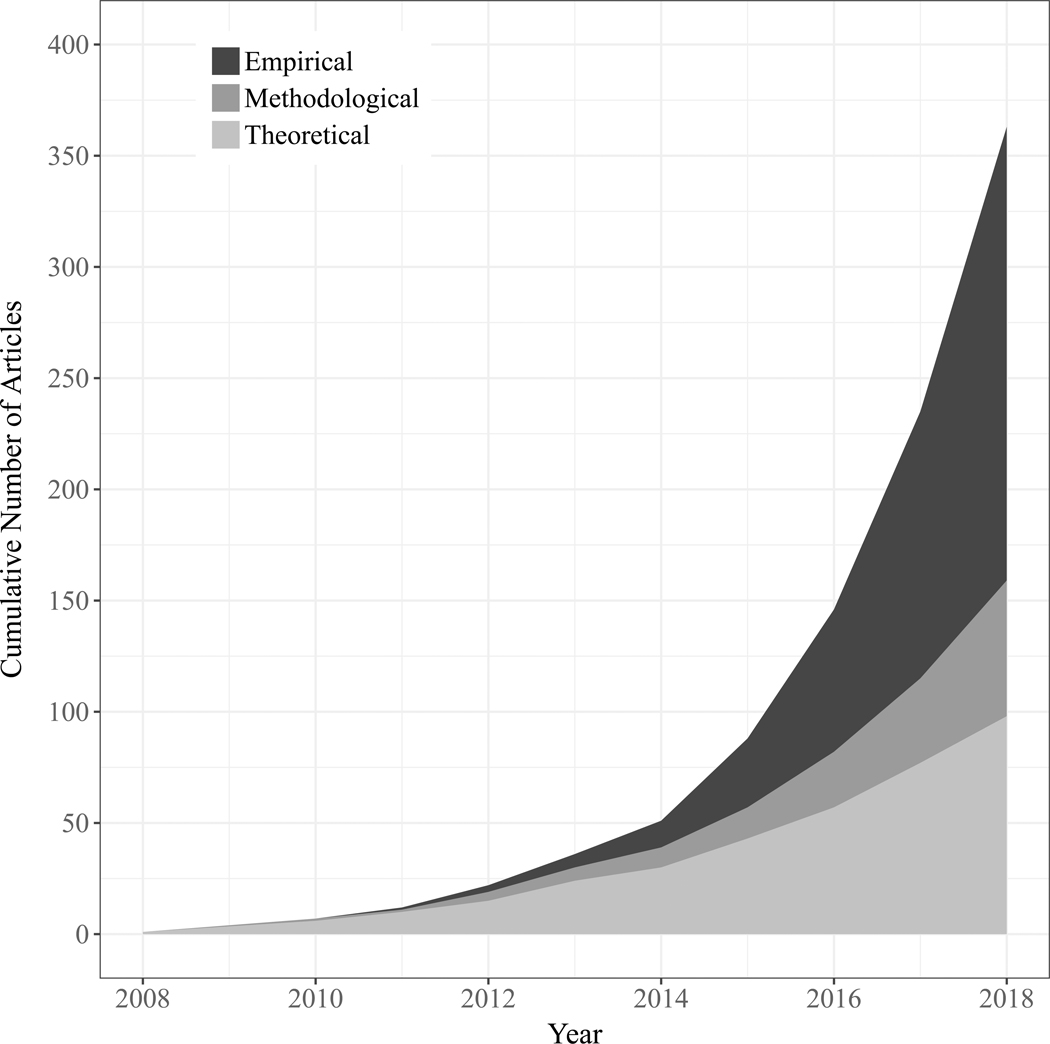
Notably, this literature has grown rapidly in recent years, with 90% of articles published in the last five years and 60% published in the last two years alone (see Figure 1). Much of this growth is driven by empirical articles, especially those using “network psychometrics” (Epskamp et al., 2016): a methodological approach developed within this literature. Indeed, the network approach has become largely synonymous with this type of empirical contribution. However, considerable work has been done beyond these empirical studies. To provide an overview of the full breadth of this work, we independently review theoretical, methodological, and empirical contributions. To our knowledge, this is the first systematic review of the full network approach literature (for a review of the empirical literature, see Contreras et al., 2019).
Figure 1. An overview of the network approach literature.
Examining the cumulative number of empirical, methodological, and theoretical papers published in the network literature from 2008–2018.
Network Theory
Among theory articles (n=97), we identified five areas of work that have substantially contributed to the network conceptualization of psychopathology.
Philosophy of Psychiatry
Parallel to the earliest conceptualization of mental disorders as symptom networks (Borsboom, 2008, Cramer et al., 2010a), another group of theorists independently proposed that mental disorders can be conceptualized as “mechanistic property clusters” (MPCs): kinds unified not by a shared underlying essence, but by causal relations among the features of the disorder (Kendler, 2016, Kendler et al., 2011, Zachar, 2015). Symptom networks can be understood as a particular kind of MPC: one which emphasizes symptoms as features of the disorder. Yet, the origins of these concepts are quite distinct. Whereas symptom networks are rooted in psychometric theory (Borsboom, 2008), MPC theorists draw their ideas from the philosophy of biology (Boyd, 1991, 1999). In doing so, they provide a philosophical foundation for network theory, undergirding it in two ways. First, as argued by Held (2017), it clarifies what kind of things mental disorders are from this perspective: clusters of features sufficiently unified by the causal relations among them that they support induction, explanation, and prediction. Second, it positions network theory within the broader history of psychiatry, contrasting it especially with monocausal and essentialist frameworks that have long dominated psychiatric research. As argued by Radden (2018), the bacterial model of disease has been a powerful and entrenched metaphor in psychiatry, shaping the theories, methods, interpretations, and expectations of the field. A major contribution of network theory, Radden suggests, is that it provides a new metaphor for thinking about mental disorders.
Consistent with this position, much of the network theory literature can be seen as an effort to grapple with what mental disorders are, how they arise, and how they are treated when viewing them through this new lens. Theorists have used this framework to examine psychiatric comorbidity (Cramer et al., 2010a, Eaton, 2015, van Loo and Romeijn, 2015, Yordanova et al., 2010), sudden shifts in the onset or remission of symptoms (Hofmann et al., 2016, van de Leemput et al., 2014), developmental psychopathology (Wass and Karmiloff-Smith, 2010), biological psychiatry (Walter, 2013), psychiatric diagnosis (Maung, 2016, Tsou, 2016, van Os et al., 2013a, b), the “p factor” (a general psychometric factor of psychopathology analogous to the general factor of intelligence; Caspi and Moffitt, 2018, van Bork et al., 2017), and the equifinality and multi-finality of mental disorders (a disorder reached by many causal factors and multiple disorders reached by the same causal factor, respectively; Borsboom, 2017, McGorry et al., 2018). Theorists have also used this lens to examine specific disorders, including depression (de Jonge et al., 2015, Hayes et al., 2015, Wittenborn et al., 2016), post-traumatic stress disorder (Armour et al., 2017, McNally, 2012, 2017), anxiety disorders (Heeren and McNally, 2016), obsessive compulsive disorder (van den Hout, 2014), eating disorders (Smith et al., 2018), autism (Anderson, 2015, Verhoeff, 2013), psychosis (Bentall, 2014, Isvoranu et al., 2016, Looijestijn et al., 2015), psychopathy (Brzović et al., 2017), sleep disorders (Blake et al., 2018, Marques and Azevedo, 2018), and suicidality (de Beurs, 2017).
Network Science
Making use of the network metaphor, early theoretical work drew heavily from network science (Barabasi, 2012), focusing on the network’s structure (i.e., the web of relations among symptoms) and its effect on the network’s state (i.e., the activation of symptoms). Theorists posited that when causal relations among symptoms are strong, the onset of one symptom will lead to the onset of others (“causality hypothesis,” Borsboom, 2008, Cramer et al., 2010a). Strongly inter-connected symptom networks are thus vulnerable to a ‘contagion’ effect of spreading activation through the network (“connectivity hypothesis”). Computational models have supported this notion (Cramer et al., 2016), showing that, in highly connected networks, modest activation of select symptoms initiated by an “external stressor” can trigger a cascade of activation (for a discussion of how external factors relate to the symptom network, see Borsboom, 2017, Fried and Cramer, 2017). Moreover, when symptom activation becomes widespread, it will persist even after the initiating stressor is removed.
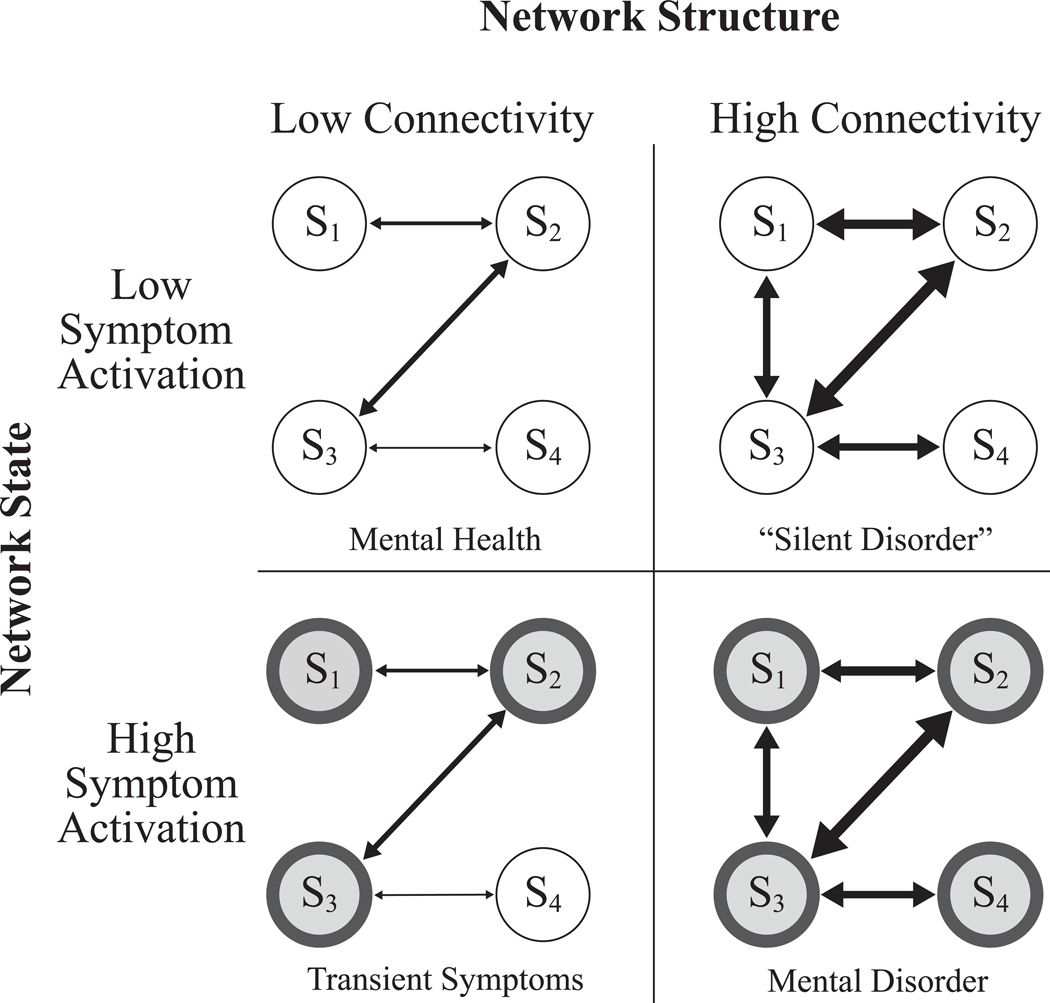
From a network perspective, mental disorder is characterized not only by the state of the network (i.e., elevated symptom activation), but also by the structure of the network: in particular, a strongly connected network in which inter-symptom relationships are sufficient to maintain elevated symptom activation over time (see Figure 2; Borsboom, 2017). In other words, mental disorder is characterized by a state of harmful equilibrium (for thought provoking and sometimes critical discussions of this characterization, see Friston et al., 2017, Guyon et al., 2017, Porter, 2015, Vosgerau and Soom, 2018, Young, 2015). Interestingly, computational modeling studies suggest that the boundary between health and disorder will vary as a function of network structure (Borsboom et al., 2016), yielding a novel perspective on whether disorders are continuous or discrete phenomena (Haslam et al., 2012, Waller and Meehl, 1998). In weakly connected networks, activation varies dimensionally. However, strongly connected networks produce sharper boundaries, as any activation within the system rapidly cascades into a state of psychopathology.
Figure 2. Network structure, network state, and the definition of mental disorder.
Network structure (high vs. low connectivity) and network state (low vs. high symptom activation) can be used to form concrete definitions of mental health and mental disorder (Borsboom, 2017, Cramer et al., 2010b). A weakly connected network with low symptom activation is in a state of mental health (top left panel). If elevated symptom activation arises (for example, due to the effects of time-limited external stressor) the system will no longer be in a state of mental health, but will also not be in a state of mental disorder as symptoms will diminish once the external stressor is removed (bottom left panel). In contrast, a strongly connected network is vulnerable to the persistence of symptom activation even absent the effects of an external stressor. It is this stable state of elevated symptom activation that we refer to as a mental disorder (bottom right panel). Finally, strongly connected networks with minimal symptom activation are perhaps not in a state of mental disorder, but are in a state of vulnerability to the onset or recurrence of a disorder (top right panel). Such a system may thus represent a “silent disorder” where symptoms are not currently manifest, but the risk for such symptoms remains high (Cramer et al., 2010b).
Early work on network structure also contributed to a shifting perspective on individual symptoms (Fried, 2015, Fried et al., 2015). From a network perspective, symptoms are not interchangeable indicators. They are agents in a causal network whose role depends upon their position in that network (Cramer et al., 2010a). Theorists posited that highly ‘central’ symptoms (e.g., those with stronger inter-symptom connections) have greater potential to spread symptom activation throughout the network than do symptoms on the periphery (“centrality hypothesis”; Cramer et al., 2010a). Such symptoms were thus posited to feature in disorder onset and remission (Borsboom and Cramer, 2013, Cramer et al., 2010a, McNally et al., 2015). Further, because some symptoms occur in multiple disorders, symptom activation can spread between syndromes, with symptoms bridging these syndromes playing a critical role in psychiatric comorbidity (“comorbidity hypothesis,” Cramer et al., 2010a).
Affect Dynamics and Momentary Experience
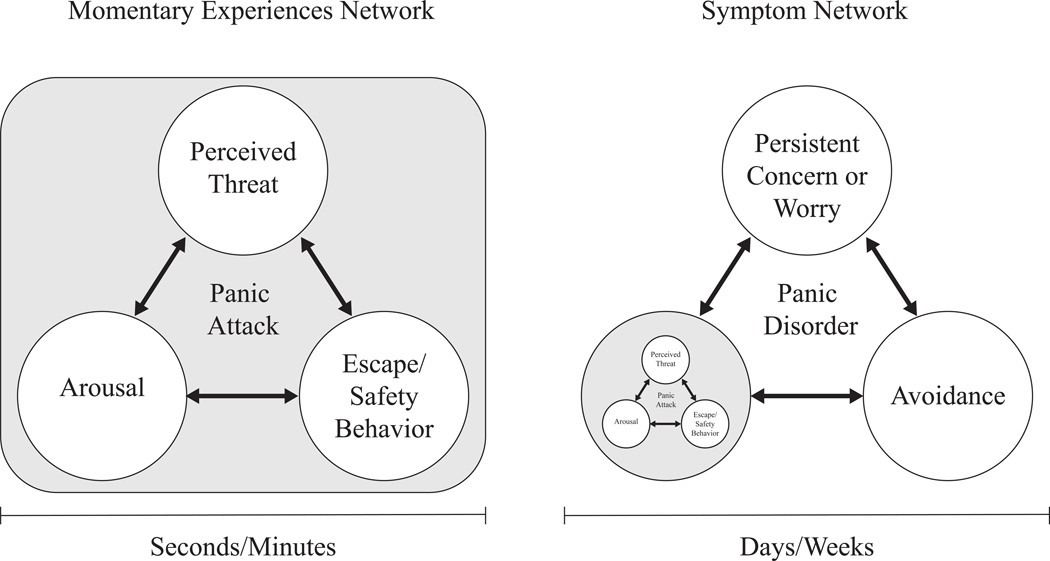
As network theory developed, some researchers argued that we must shift our focus not only from disorders to symptoms, but further to the level of momentary experiences (van Os et al., 2013a, b, Wichers, 2014, Wichers et al., 2015). These researchers note that symptoms are aggregates of moment-to-moment experiences. It is these moment-to-moment “micro-processes,” they argue, that constitute the true building blocks of psychopathology (see Figure 3; cf. Wichers, 2014, p. 1351). This perspective shifts our focus to a more granular level of experience and highlights the importance of understanding the “chronometry” of experiences, symptoms, and disorders (Treadway and Leonard, 2016).
Figure 3. Illustrating symptom networks and momentary experiences with the example of panic disorder.
Panic disorder comprises three core symptoms (recurrent panic attacks, persistent concern or worry about those attacks, and avoidance behavior) that play out on a time scale of days, weeks, or even months (e.g., to meet criteria for panic disorder, these symptoms must persist for at least one month). Panic attacks, in turn, comprise momentary experiences of arousal-related bodily sensations, a sense of impending threat (e.g., fear of having a heart attack), and an urge to escape from or mitigate that threat. These momentary experiences play out over the course of seconds of minutes (e.g., to meet criteria for a panic attack, these experiences must surge to a peak within 10 minutes). Cognitive behavioral theories posit that causal relations at both of these time scales play critical roles in panic attacks (Clark, 1986) and panic disorder (Goldstein and Chambless, 1978). A critical challenge for the network approach literature will be determining precisely how processes at these different time scales interact with one another (cf. Wichers, 2014).
Cognitive Behavioral Theory
From its earliest stages, network theory has drawn on cognitive behavioral models of psychopathology when discussing plausible causal relations among symptoms (e.g., “vicious cycle” theories of Panic Disorder; Cramer et al., 2010a). Indeed, the cognitive behavioral literature offers a long history of theorizing about causal relations among symptoms, empirical research investigating those relationships, and treatment research suggesting that symptom-level interventions are effective treatments (e.g., see van den Hout, 2014). Not surprisingly then, some cognitive behavioral theorists have embraced network theory and proposed integrating it with cognitive behavioral models (Hoffart and Johnson, 2017, Hofmann, 2014, Hofmann et al., 2016, McNally, 2016, van den Hout, 2014).
Systems Science
Most recently, theorists have drawn from areas of systems science beyond network science alone, including dynamical systems theory, catastrophe theory, and cybernetics (Hayes et al., 2015, Nelson et al., 2017, Tretter and Loffler-Stastka, 2018, Yordanova et al., 2010). These fields offer new tools for psychiatric research. For example, the feedback loops emphasized in cognitive behavioral theories of psychopathology have been rigorously investigated in cybernetics and dynamical systems theory (Scheffer, 2009). Illustrating the value of this work, Wittenborn et al. (2016) used the “causal loop diagrams” of dynamical systems theory to generate a conceptual model of depression as a dynamical system, and dynamical systems concepts such as alternative stable states and critical slowing have already begun to be applied to psychopathology (Hayes et al., 2015, Hofmann and Curtiss, 2018, Nelson et al., 2017, Rikkert et al., 2016). Indeed, there is research examining mental disorders as dynamical systems that predates (e.g., Granic, 2005, Hayes and Strauss, 1998, Schiepek, 2003) and, in some cases, has continued to develop independently of (e.g., Pincus and Metten, 2010) the network approach literature. This work anticipated many of the ideas that would later develop within the context of the network approach (e.g., “ideographical system modeling,” Schiepek, 2003) and is thus an invaluable resource for those studying mental disorders as complex systems.
Critical Analysis & Future Directions
With these diverse scientific and philosophical contributions, considerable progress has been made in developing a general network theory of mental disorders (Borsboom, 2017). However, formal theories that specify precisely how any specific disorder operates as a causal system are still scarce. We regard the development of such theories to be a critical next step for network theory. Computational models will play a critical role if the field is to achieve this aim (Huys et al., 2016, Robinaugh et al., 2019, Tryon, 2018).
One key advantage of such models is that they render all aspects of the theory explicit and available for evaluation (Epstein, 2008). Computational models of symptom networks thus provide insight into the assumptions made in network theory, as they are the most explicit representation in the literature of how symptom networks are posited to operate. Unfortunately, currently operational models (Borsboom et al., 2016, Cramer et al., 2016) reveal a restrictive set of assumptions: they typically assume binary symptoms that operate on the same time scale and interact with instantaneous and positive effects (i.e., symptoms exacerbate, rather than inhibit one another). Further, interactions between symptoms are pairwise and symmetric (i.e., X causes Y to the same extent that Y causes X).
Models adhering to these assumptions (Binary Instantaneous Positive Pairwise and Symmetric [BIPPS] models) are unrealistic for most mental disorders. Many symptoms are dimensional. Some inter-symptom effects occur over minutes (fear→avoidance) whereas others occur over days (insomnia→fatigue), weeks (appetite loss→weight loss), or years (childhood sexual abuse→adulthood social disconnection). Negative inter-symptom effects are plausible, as are higher order interactions (e.g., sleep moderating the effect of trauma memories on emotional reactivity), and many inter-symptom relations are asymmetric (e.g., fear elicits avoidance, but avoidance dampens fear). Violations of these assumptions will almost certainly impact core network theory hypotheses. For example, whether “central symptoms” are indeed especially important almost certainly depends on the specifics of the network structure and inter-symptom interactions, making it unclear when this hypothesis should be expected to hold (cf. Bringmann et al., 2019, Dablander and Hinne, 2018, Hallquist et al., 2019). Theorists may rightly object that their own theory of symptom networks does not require adherence to these assumptions. However, to the extent that such theories remain verbal in character, their assumptions remain unclear and unavailable for careful evaluation.
It will thus be important to develop computational models in which the assumptions embodied in the model better align with how specific disorders are thought to operate (e.g., see Hosseinichimeh et al., 2018). This work can (indeed, must) be directly informed by each of the areas of work that have already contributed to network theory. For example, cognitive behavioral models of psychopathology bring a wealth of theory and empirical research about inter-symptom causal relations (cf. van den Hout, 2014); the literature on affective dynamics can inform our understanding of the timescales on which processes operate and how moment-to-moment experiences become symptoms and, in turn, disorders (cf. Wichers, 2014); and the dynamical systems literature can provide a host of tools for modeling and evaluating complex systems (cf. Wittenborn et al., 2016, Yang et al., 2018).
Methodology
When the network approach was first proposed, there was no established method for assessing symptom network structure. The methodology developed to meet this need in the 61 methodological articles we reviewed has two primary components: (a) estimating network structure and (b) assessing network characteristics.
Network Structure
Early efforts defined network structure using symptom cooccurrence or correlation (Cramer et al., 2012, Cramer et al., 2010a). Aiming to better identify the direct inter-symptom relations posited in network theory, subsequent efforts have focused on conditional dependence relationships with a penalty on regression parameters to obtain a sparse network of dependence relationships known as a Pairwise Markov Random Field (PMRF; see Figure 4). This approach was first implemented by van Borkulo et al. (2014) and subsequently extended to multivariate normal data (Epskamp et al., 2018a), mixed data (Haslbeck and Lourens, 2016) and latent variables (Epskamp et al., 2017b). Researchers have made these methods freely available (Epskamp et al., 2012, van Borkulo et al., 2014), provided tutorials on their use (Borsboom and Cramer, 2013, Costantini et al., 2015, Epskamp and Fried, 2018, Epskamp et al., 2017a, Jones et al., 2018), and extensively discussed their properties (Kruis and Maris, 2016, Marsman et al., 2018).
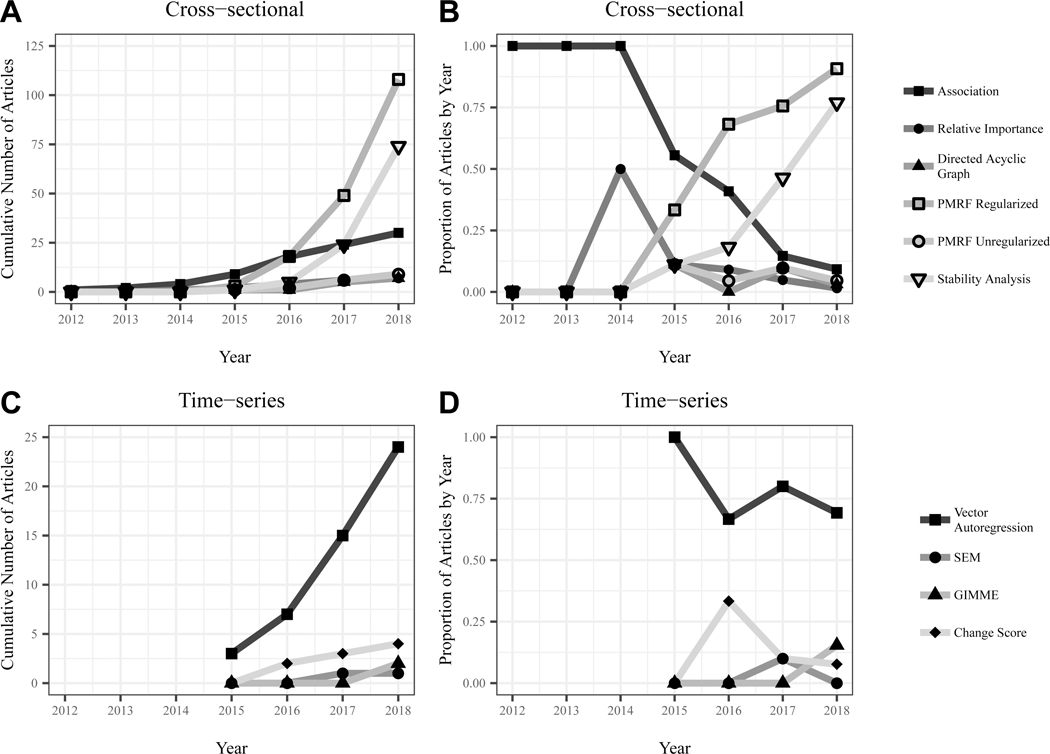
Figure 4. Network estimation methods commonly utilized in empirical network studies.
This figure depicts methods commonly used in estimating network structure from cross-sectional (panels A & B) and time-series data (panels C & D). Panels A & C depict the cumulative number of articles applying a given estimation method for cross-sectional and time-series data, respectively. Panels B & D depict the proportion of articles in a given year that utilized these estimation methods. For the purposes of this summary, we considered any network based on multiple time points to be based on “time-series” data, thus incorporating change score networks into this category. Note that the earliest cross-sectional (Cramer et al., 2010a) and time-series (Bringmann et al., 2013) networks were regarded as theoretical and methodological contributions, respectively, given their substantial contributions in these domains, and thus are not included in this report. PMRF = Pairwise Markov Random Field; SEM = Structural Equation Modeling; GIMME = Group Iterative Multiple Model Estimation
Conditional dependence networks can be constructed from either cross-sectional or intra-individual time series data. Cross-sectional networks have been criticized on two fronts. First, researchers have expressed concerns about their replicability (Fried and Cramer, 2017, Fried et al., 2016), with some arguing that these methods are inherently unstable (for an extended discussion, see Borsboom et al., 2017, Borsboom et al., 2018, Forbes et al., 2017a, b). Some have further argued that instability is exacerbated by the use of single-item assessments and small samples (DeYoung and Krueger, 2018). To promote robustness, methods have been developed for evaluating the precision and stability of estimated network parameters (Epskamp et al., 2018a). These methods have been rapidly adopted in the empirical network literature (see Figure 4). Nonetheless, replicability remains an important subject of ongoing debate (e.g., Forbes et al., 2019, Jones et al., 2019).
Researchers have also argued that cross-sectional findings cannot demonstrate causality and cannot be assumed to generalize to the level of most interest in network theory: the level of the individual (e.g., Bos and Wanders, 2016, Bringmann and Eronen, 2018, Forbes et al., 2017a, Tzur-Bitan et al., 2010). These researchers suggest that conditional dependence structure should instead be based on within-person variation, assessing network relations “where (i.e., within-person) and when (i.e., in real time)” they are posited to operate (Hamaker and Wichers, 2017). Researchers have thus developed (Beltz and Gates, 2017, Bringmann et al., 2018, Bringmann et al., 2013, Bulteel et al., 2018, Epskamp et al., 2018c) and evaluated (Bulteel et al., 2016b, de Haan-Rietdijk et al., 2017, Kuiper and Ryan, 2018, Schuurman et al., 2016, Schuurman et al., 2015) methods for estimating within-subject network structure. These methods, especially vector autoregressive models, are growing in popularity and promise to substantially inform our understanding of the relationships among symptoms (see Figure 4).
Alternative Methods.
Although most studies estimate network structure using statistical associations, additional methods have been used (e.g., Borsboom et al., 2011, Tio et al., 2016). In one method of note, researchers query patients or clinicians about the relations among symptoms (Frewen et al., 2013, Ruzzano et al., 2015). Despite their promise, these perceived causal relation networks remain underutilized.
Network Characteristics
Researchers have adopted or developed methods for examining local and global characteristics of symptom networks, including assessments of node centrality (Epskamp et al., 2012), node predictability (Haslbeck and Waldorp, 2018), node clustering (Costantini and Perugini, 2014), community structure (Blanken et al., 2018, Golino and Epskamp, 2017, Zhao et al., 2017), and similarity of intra-individual network structure (Bulteel et al., 2016a). These characteristics are often a primary focus of network analysis studies.
Critical Analysis & Future Directions
The network psychometric toolbox is rapidly evolving. Researchers are developing new methods for comparing (van Borkulo et al., 2017, Williams et al., 2019) and estimating network structure, including methods that integrate latent variable and network models (Chen et al., 2018, Christensen et al., 2018, Epskamp, 2019, Williams and Rast, 2018). Researchers have also called for increased adoption of tools from other domains of systems science (Nelson et al., 2017), such as the use of autocorrelations to signal shifts into a state of psychopathology (van de Leemput et al., 2014). Here, we highlight three additional areas in need of development.
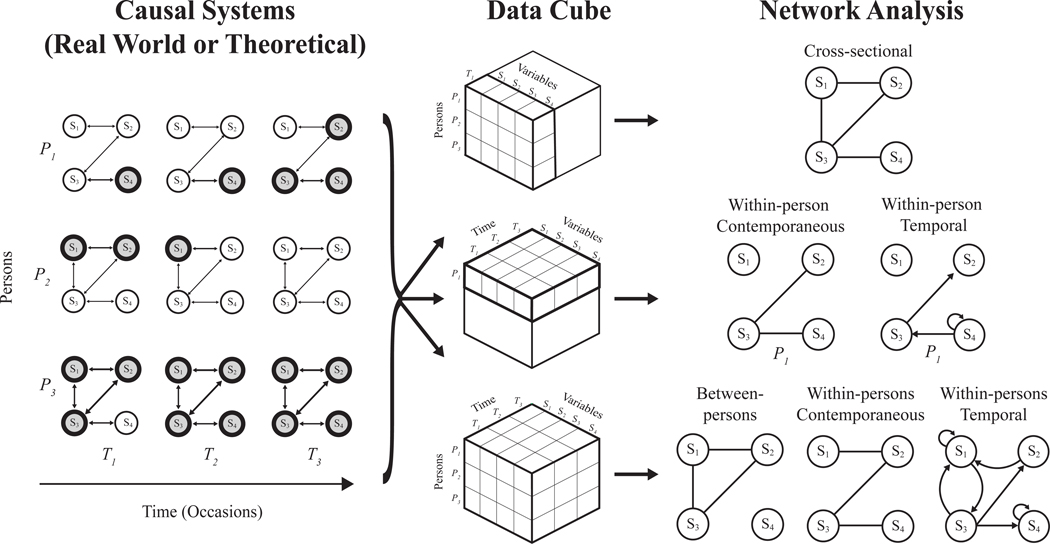
Most importantly, the relationship between data generating causal systems and empirical networks estimated from data requires further evaluation (see Figure 5). Network psychometrics recover the “true” causal system when that system is itself a PMRF (Epskamp et al., 2018b), as would be the case for a causal system meeting the BIPPS assumptions. We also know what empirical PMRF we should expect for one specific type of causal system (i.e., directed acyclic graphs; Pearl, 2009). However, neither of these systems are theoretically plausible for most mental disorders, and we have minimal insight into the relationship between causal systems and network structures estimated using network psychometrics in more realistic frameworks. This is true of both cross-sectional networks and within-subject networks. Clarifying this relationship is fundamental to our ability to draw inferences from these analyses and, therefore, a critical direction for future research.
Figure 5. An overview of network methodology, with a focus on the relationship between causal systems, data, and the empirical networks most commonly used in the network approach literature (Pairwise Markov Random Fields).
In many areas of network science, both the elements of the network and the connections among them can be directly observed (e.g., train stations and the tracks that connect them). In psychiatry, symptoms can be assessed, but the relationships among them must be inferred. Network psychometrics aims to infer those relationships using statistical associations. The method by which this is done depends on the data collected (for a discussion of Cattell’s data cube and its relation to specific analyses, see Wardenaar and de Jonge, 2013). For cross-sectional data, a single network is estimated based on the covariation of symptoms between-persons at that point in time. For n=1 time-series data, networks are estimated based on the covariation of symptoms over time within one individual, and can be used to inform contemporaneous and temporal (lagged) associations among symptoms. In time series data in larger samples, networks can be estimated using both within- and between-person information. Importantly, the network structure derived from between-person analyses and within-person analyses are unlikely to be equivalent and, for many plausible causal systems, it remains unclear how the structured derived from either analysis corresponds to the “true structure” of the causal system. The relationships among between-person networks, within-person networks, and the “true structure” of different types of causal systems are critical directions for future research.
Second, methodologies for aggregating findings across this growing literature are needed, including methods for combining networks derived from similar analyses and methods for integrating findings across different analyses. Because no single methodology has been shown to directly recover the network structure of mental disorders, both cross-sectional networks and within-subjects networks provide valuable but incomplete information about the relationships among symptoms. Accordingly, a genuine understanding of causal systems will almost certainly require an aggregation of evidence across multiple studies and methodological approaches.
Finally, the field must develop a methodology for network data collection. The majority of empirical network studies have used data that were not collected for the purpose of network analysis (Guloksuz et al., 2017). The selection and measurement of network components is fundamentally important to the estimation (Hallquist et al., 2019) and interpretation (Forbes et al., 2017a) of network structure. Even seemingly minor measurement decisions can impact the results of these analyses (Hoffman et al., 2018). Accordingly, psychometric strategies focused on the optimal assessment of components of psychopathology networks are needed.
Empirical Studies
Among 204 empirical articles in the reviewed literature, 174 used some form of network analysis. Among these, 170 used network psychometrics to estimate network structure, including 141 articles that examined cross-sectional data in 176 samples (mean N = 2,169; median N = 508) and 32 articles that examined time-series data in 44 samples (mean N = 185; median N = 76). This approach has been applied to a wide range of disorders, but especially to depression (incorporated in 69 articles) and PTSD (31 articles). This empirical work provides rich and nuanced information about inter-symptom relationships for these disorders. A complete review of these disorder-specific findings is beyond the scope of this review. In our Supplementary Materials, we list empirical publications organized by disorder and we encourage readers to use this resource to read further. Here, we adopt a broader focus and consider findings across disorders for the two most commonly examined network characteristics: network connectivity and node centrality (see Figure 6).
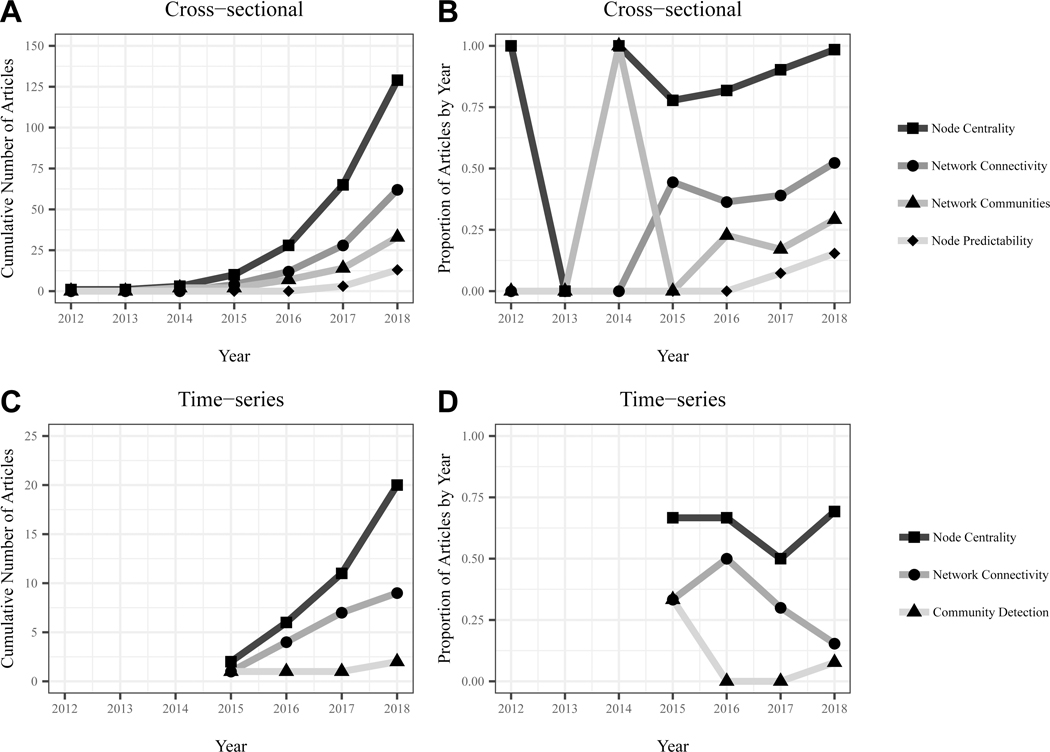
Figure 6. Network characteristics commonly examined in empirical network studies.
This figure depicts characteristics commonly examined in empirical network studies utilizing cross-sectional (panels A & B) and time-series data (panels C & D). Panels A & C depict the cumulative number of articles reporting a given characteristic for cross-sectional and time-series data, respectively. Panels B & D depict the proportion of articles in a given year that examined those characteristics. In both cross-sectional and time-series networks, node centrality and network connectivity were the most examined network characteristics.
Network Connectivity.
Most fundamentally, empirical network studies have found that symptoms are highly interconnected. There is not only a positive manifold (i.e., all variables are positively correlated), but a conditional positive manifold for most disorders. That is, with some exceptions, even after controlling for shared variance among symptoms, these symptoms tend to be positively interconnected. This high connectivity is not surprising, but bears noting as it suggests meaningful clustering of symptoms in the syndromes we identify as mental disorders. Connectivity tends to be consistent across time (e.g., Curtiss et al., 2018, Rouquette et al., 2018, von Stockert et al., 2018) and demographic groups, especially gender and age (e.g., Belvederi Murri et al., 2018, Fonseca-Pedrero et al., 2018, Russell et al., 2017); though differences have been observed between countries (Fonseca-Pedrero et al., 2018, Wusten et al., 2018).
Researchers have investigated the hypothesis that greater connectivity (aka network density or global strength) confers risk for psychopathology using cross-sectional analyses in several ways. First, researchers have compared connectivity between groups based on clinical severity. These studies typically found greater connectivity in those with greater severity (e.g., Heeren and McNally, 2018, Santos et al., 2017, van Rooijen et al., 2018), though one reported no difference (Levinson et al., 2018a) and another found the opposite pattern (Southward and Cheavens, 2018). However, these findings should be interpreted with caution as grouping subjects on severity affects the estimation of the network (De Ron et al., 2019). Second, researchers have retrospectively examined baseline network connectivity in those whose disorder subsequently remitted vs. persisted, reasoning that greater connectivity should lead to disorder persistence. van Borkulo et al. (2015) indeed found greater baseline connectivity among depression symptoms in those with persistent vs. remitted depression. In two subsequent studies, one similarly reported greater baseline connectivity in those with persistent depression, but could not reject the null hypothesis that networks were equal at the population level (Schweren et al., 2018) and another reported greater connectivity in treatment non-responders vs. responders for psychotic disorder symptoms, but no statistical tests were performed (Esfahlani et al., 2017). Accordingly, there is at best modest support for the notion that connectivity is associated with disorder persistence. Third, researchers have examined whether those at risk for psychopathology (e.g., genetic risk; van Loo et al., 2018) exhibit elevated network connectivity. No such elevations have been observed. Fourth, researchers have examined whether connectivity reduces over the course of treatment, hypothesizing that treatments may have their effect by reducing connectivity. Most such studies reported no change in connectivity (e.g., Levine and Leucht, 2016, Lydon-Staley et al., 2018, Schuler et al., 2018) and two reported an increase in connectivity over time (Beard et al., 2016, Bos et al., 2018). Notably, the only study to find significant connectivity change naturally over time similarly found increased connectivity among PTSD symptoms from 24-hours to 12-months post-trauma, a timeframe in which there is significant reduction in symptom severity (Bryant et al., 2017).
Importantly, these cross-sectional studies are predicated on the assumption that greater connectivity at the group level indicates greater connectivity in the individuals who compose the group (Bos and Wanders, 2016, van Borkulo et al., 2016). To our knowledge, there is no evidence to support or disconfirm this assumption, making it unclear whether these findings are an adequate test of the connectivity hypothesis. Several studies have avoided this limitation using intra-individual network analyses. These studies have found greater connectivity among negative mood states in those with depression (Pe et al., 2015), elevated neuroticism (Bringmann et al., 2016), and genetic liability for psychopathology (Hasmi et al., 2017). However, de Vos et al. (2017) found that whether mood state network connectivity was indeed stronger among depressed patients varied considerably depending on methodological choices. In addition, in a network encompassing a broader range of components (e.g., cognitions, emotions, psychotic experiences), Klippel et al (2018) observed differences in the number but not strength of connections among psychotic patients, first-degree relatives, and healthy controls. Together, these studies utilizing time-series data provide qualified support for the notion that connectivity of negative mood state networks is associated with psychopathology, but minimal evidence that broader networks of momentary experiences exhibit such associations.
Node Centrality.
Empirical research has focused heavily on examining individual symptoms using node centrality. Among centrality indices, the most popular and robust is node strength (i.e., summed absolute strength of a node’s direct links). At least two broad conclusions can be drawn from this work. First, there is no evidence that the symptoms identified in the DSM play a privileged role in these networks. Fried et al. (2016) and Kendler et al. (2018) found that there was, on average, no difference between DSM and non-DSM symptoms of depression. Indeed, non-DSM symptoms often exhibit elevated centrality (e.g., feeling disliked in deperession and fear of weight gain in bulimia nervosa; Levinson et al., 2018b, Santos et al., 2017) and some DSM nodes are weakly connected to the network (e.g., traumatic amnesia in PTSD networks; Fried et al., 2018). Relatedly, there is mixed evidence as to whether those symptoms the DSM identifies as being especially important (e.g., depressed mood and anhedonia) are more central than other DSM symptoms. For example, the cardinal symptoms of depression are indeed often highly central, but perhaps the most consistently central depression symptom is low energy/fatigue (cf. Contreras et al., 2019). Accordingly, while connectivity analyses suggest that the DSM accurately identifies symptoms that cohere as syndromes, centrality analyses suggest it has not captured all symptoms or even uniquely important symptoms within these syndromes.
Second, there is modest evidence to support the notion that centrality indices identify important symptoms. Central symptoms have been found to be more predictive of subsequent diagnosis than are peripheral symptoms in both depression and PTSD (Boschloo et al., 2016, Haag et al., 2017), and a symptom’s centrality is positively correlated with the strength of association between change in the symptom and change in the remainder of the network (Robinaugh et al., 2016, Rodebaugh et al., 2018). However, while these findings are consistent with the centrality hypothesis, they are also consistent with a common cause framework where symptoms arise from a single underlying dimension. In that case, symptoms with higher strength centrality would be identified as more reliable indicator variables and the same pattern of findings would be expected, as more reliable indicators are more predictive (Lord and Novick, 1968, Muchinsky, 1996). Accordingly, these findings are consistent with, but not especially strong evidence for, the centrality hypothesis.
Critical Analysis & Future Directions
We have three broad critiques of the empirical literature. First, these studies have relied heavily on data collected for purposes other than network analysis. This raises concern about whether individual items used in these analyses indeed represent discrete components of the syndrome (Fried and Cramer, 2017, Hallquist et al., 2019, Levinson et al., 2018a). It has also contributed to substantial differences between studies in the components included in the network. For example, among 18 studies estimating the depression symptom network in isolation, researchers used 12 different pre-existing scales, with the number of symptoms ranging from 9 to 28 (see Supplementary Materials). This problem is not unique to the network approach (Fried, 2017), but is especially problematic in this context given the emphasis on individual symptoms. It will thus be important to design studies expressly for the purpose of investigating mental disorders as complex systems. Second, to our knowledge no studies within this literature have experimentally manipulated individual symptoms in order to evaluate their impact on other symptoms. Even in the absence of network analysis, such studies are fundamentally important to our understanding of how symptoms relate to one another (Blanken et al., 2019, Marsman et al., 2018). Finally, we believe that researchers (including authors of this article), must be more cautious when deriving hypotheses from network theory to be tested in empirical research. The behavior of complex systems is notoriously difficult to predict and the process of deriving hypotheses about the data models these systems should produce is likely prone to error. For instance, it is uncertain whether stronger inter-symptom causal relations will indeed produce greater connectivity in conditional dependence networks, as intuition would suggest. As detailed in the next section, we believe computational models are needed to more accurately derive the predictions made by network theory.
An Agenda for Future Research
The central task for the next decade of the network approach is to build on the theoretical, methodological, and empirical foundations we have described here and advance our understanding of how specific mental disorders operate as causal systems. We believe that the path to this aim is clarified by viewing the network approach as an abductive program of research: one rooted in the twin aims of identifying robust empirical phenomena and developing formal theories that explain those phenomena (Haig, 2005, 2008).
Most empirical network studies can be understood as carrying out the initial stages of phenomena detection: using exploratory network analyses to uncover data patterns (e.g., a conditional positive manifold, community structure, or centrality ordering). Indeed, the most widely used methodological tools developed within this literature are especially valuable for this exploratory work, as they allow researchers to visualize and quantify complex dependencies in the data. Over the next decade, it will be necessary for empirical researchers to evaluate which among these exploratory findings are replicable and generalizable phenomena. Carrying out our recommendations for methodological development will support this effort, providing tools for aggregating findings across studies and for conducting confirmatory network analyses. It will be important for empirical researchers to use such methods in studies designed specifically for assessing symptom networks, ideally with large samples and time-series data that can support both between-subject and within-subject analyses (cf. Wichers et al., 2017). These efforts will allow researchers to evaluate whether observed data patterns are sufficiently robust that they can inform and constrain the development of formal theories.
The development of network theory over the past decade has provided a theoretical framework that accounts for a fundamental psychiatric phenomenon: the tendency for symptoms to cohere as syndromes. Over the next decade, we must use this framework to develop computational models that posit precisely how specific mental disorders are thought to operate. Such models will explicate theory assumptions and provide a tool for evaluating what theories can and cannot explain, thus guiding their ongoing development. Moreover, these models will facilitate the recommendations for methodological and empirical work we have made in this review. For methodologists, computational models will provide theoretically plausible causal systems from which to generate data, equipping them to investigate the relation between network psychometric models and the causal systems we expect to see in psychiatric research. For empirical researchers, computational models can guide study design, clarifying the components to be investigated and the timeframe in which they should be assessed. Moreover, model simulations can more precisely derive theory predictions, thereby strengthening empirical tests of network theory hypotheses. In turn, the phenomena detected through empirical research can inform the advancement of network theories, clarifying the features of psychopathology for which they must account. Through this ongoing exchange between theoretical development and empirical research, formal theories can be evaluated and advanced, permitting genuine advances in our understanding of how mental disorders operate as causal systems.
Conclusion
The first decade of the network approach has been a period of considerable growth. An inter-disciplinary group of researchers developed the hypothesis that there are important causal relationships among symptoms into a theory regarding the nature of psychopathology, a nascent methodology for investigating symptom networks, and a growing body of empirical research. To build upon this work, we believe that theorists, methodologists, and empirical researchers must collaboratively work toward two overarching aims: (a) establishing robust empirical phenomena and (b) developing formal theories that can explain those phenomena. Progress toward these aims will be critical if the network approach is to be a cumulative program of research over the next decade: one that does not merely produce a growing number of empirical analyses, but also represents the accumulation of knowledge about psychopathology.
Supplementary Material
Acknowledgements
This manuscript was supported by a National Institute of Mental Health Career Development Award (1K23MH113805-01A1) awarded to D. Robinaugh, ERC Consolidator Grant no. 647209 awarded to D. Borsboom, and NWO Research Talent Grant no. 406-18-532 awarded to R. Hoekstra. We would like to thank Alex Millner and Eiko Fried for their thoughtful feedback on an earlier draft of this manuscript.
References
- Anderson GM (2015). Autism biomarkers: challenges, pitfalls and possibilities. Journal of Autism and Developmental Disorders 45, 1103–13. [DOI] [PubMed] [Google Scholar]
- Armour C, Fried EI & Olff M (2017). PTSD symptomics: network analyses in the field of psychotraumatology. European Journal of Psychotraumatology 8, 1398003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barabasi AL (2012). The network takeover. Nature Physics 8, 14–16. [Google Scholar]
- Beard C, Millner AJ, Forgeard MJ, Fried EI, Hsu KJ, Treadway MT, Leonard CV, Kertz SJ & Bjorgvinsson T (2016). Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychological Medicine 46, 3359–3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltz AM & Gates KM (2017). Network mapping with GIMME. Multivariate Behavioral Research 52, 789–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belvederi Murri M, Amore M, Respino M & Alexopoulos GS (2018). The symptom network structure of depressive symptoms in late-life: Results from a European population study. Molecular Psychiatry, 44, 1–10. [DOI] [PubMed] [Google Scholar]
- Bentall RP (2014). The search for elusive structure: a promiscuous realist case for researching specific psychotic experiences such as hallucinations. Schizophrenia Bulletin 40 Supplement 4, S198–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake MJ, Trinder JA & Allen NB (2018). Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: Implications for behavioral sleep interventions. Clinical Psychology Review 63, 25–40. [DOI] [PubMed] [Google Scholar]
- Blanken TF, Deserno MK, Dalege J, Borsboom D, Blanken P, Kerkhof GA & Cramer AOJ (2018). The role of stabilizing and communicating symptoms given overlapping communities in psychopathology networks. Scientific Reports 8, 5854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanken TF, Van Der Zweerde T, Van Straten A, Van Someren EJW, Borsboom D & Lancee J (2019). Introducing network intervention analysis to investigate sequential, symptom-specific treatment effects: A demonstration in co-occurring insomnia and depression. Psychotherapy and Psychosomatics 88, 52–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D (2008). Psychometric perspectives on diagnostic systems. Journal of Clinical Psychology 64, 1089–108. [DOI] [PubMed] [Google Scholar]
- Borsboom D (2017). A network theory of mental disorders. World Psychiatry 16, 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D & Cramer AO (2013). Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO, Schmittmann VD, Epskamp S & Waldorp LJ (2011). The small world of psychopathology. PLoS One 6, e27407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Fried EI, Epskamp S, Waldorp LJ, van Borkulo CD, van der Maas HLJ & Cramer AOJ (2017). False alarm? A comprehensive reanalysis of “Evidence that psychopathology symptom networks have limited replicability” by Forbes, Wright, Markon, and Krueger (2017). Journal of Abnormal Psychology 126, 989–999. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Rhemtulla M, Cramer AOJ, van der Maas HLJ, Scheffer M & Dolan CV (2016). Kinds versus continua: a review of psychometric approaches to uncover the structure of psychiatric constructs. Psychological Medicine 46, 1567–1579. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Robinaugh DJ, The Psychosystems Group, Rhemtulla M & Cramer AOJ (2018). Robustness and replicability of psychopathology networks. World Psychiatry 17, 143–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos EH & Wanders RB (2016). Group-level symptom networks in depression. JAMA Psychiatry 73, 411. [DOI] [PubMed] [Google Scholar]
- Bos FM, Fried EI, Hollon SD, Bringmann LF, Dimidjian S, DeRubeis RJ & Bockting CLH (2018). Cross-sectional networks of depressive symptoms before and after antidepressant medication treatment. Soc Psychiatry Psychiatr Epidemiol 53, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boschloo L, van Borkulo CD, Borsboom D & Schoevers RA (2016). A prospective study on how symptoms in a network predict the onset of depression. Psychotherapy and Psychosomatics 85, 183–4. [DOI] [PubMed] [Google Scholar]
- Boyd R (1991). Realism, antifoundationalism and the enthusiasm for natural kinds. Philosophical Studies 61, 127–148. [Google Scholar]
- Boyd R (1999). Homeostasis, species, and higher taxa. A Bradford Book/MIT Press: Cambridge, MA. [Google Scholar]
- Bringmann LF, Elmber T, Epskamp S, Kraus RW, Schoch D, Wichers M, Wigman JT & Snippe E (2019). What do centrality measures measure in psychological networks. Journal of Abnormal Psychology, 128, 892–903. [DOI] [PubMed] [Google Scholar]
- Bringmann LF & Eronen MI (2018). Don’t blame the model: Reconsidering the network approach to psychopathology. Psychological Review 125, 606–615. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Ferrer E, Hamaker EL, Borsboom D & Tuerlinckx F (2018). Modeling Nonstationary Emotion Dynamics in Dyads using a Time-Varying Vector-Autoregressive Model. Multivariate Behavioral Research 53, 293–314. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Pe ML, Vissers N, Ceulemans E, Borsboom D, Vanpaemel W, Tuerlinckx F & Kuppens P (2016). Assessing Temporal Emotion Dynamics Using Networks. Assessment 23, 425–435. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Vissers N, Wichers M, Geschwind N, Kuppens P, Peeters F, Borsboom D & Tuerlinckx F (2013). A network approach to psychopathology: new insights into clinical longitudinal data. PLoS One 8, e60188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA, Creamer M, O’Donnell M, Forbes D, McFarlane AC, Silove D & Hadzi-Pavlovic D (2017). Acute and Chronic Posttraumatic Stress Symptoms in the Emergence of Posttraumatic Stress Disorder: A Network Analysis. JAMA Psychiatry 74, 135–142. [DOI] [PubMed] [Google Scholar]
- Brzović Z, Jurjako M & Šustar P (2017). The kindness of psychopaths. International Studies in the Philosophy of Science 31, 189–211. [Google Scholar]
- Bulteel K, Tuerlinckx F, Brose A & Ceulemans E (2016a). Clustering vector autoregressive models: Capturing qualitative differences in within-person dynamics. Frontiers in Psychology 7, 1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulteel K, Tuerlinckx F, Brose A & Ceulemans E (2016b). Using raw VAR regression coefficients to build networks can be misleading. Multivariate Behavioral Research 51, 330–44. [DOI] [PubMed] [Google Scholar]
- Bulteel K, Tuerlinckx F, Brose A & Ceulemans E (2018). Improved Insight into and Prediction of Network Dynamics by Combining VAR and Dimension Reduction. Multivariate Behavioral Research 53, 853–875. [DOI] [PubMed] [Google Scholar]
- Caspi A & Moffitt TEM (2018). All for one and one for all: Mental disorders in all for one and one for all: Mental disorders in one dimension. The American Journal of Psychiatry 175, 831–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Li X, Liu J & Ying Z (2018). Robust Measurement via A Fused Latent and Graphical Item Response Theory Model. Psychometrika 83, 538–562. [DOI] [PubMed] [Google Scholar]
- Christensen AP, Kenett YN, Aste T, Silvia PJ & Kwapil TR (2018). Network structure of the Wisconsin Schizotypy Scales-Short Forms: Examining psychometric network filtering approaches. Behavior Research Methods 50, 2531–2550. [DOI] [PubMed] [Google Scholar]
- Clark DM (1986). A cognitive approach to panic. Behaviour Research and Therapy 24, 461–70. [DOI] [PubMed] [Google Scholar]
- Contreras A, Nieto I, Valiente C, Espinosa R & Vazquez C (2019). The Study of Psychopathology from the Network Analysis Perspective: A Systematic Review. Psychotherapy and Psychosomatics 88, 71–83. [DOI] [PubMed] [Google Scholar]
- Costantini G, Epskamp S, Borsboom D, Perugini M, Mottus R, Waldorp LJ & Cramer AOJ (2015). State of the aRt personality research: A tutorial on network analysis of personality data in R. Journal of Research in Personality 54, 13–29. [Google Scholar]
- Costantini G & Perugini M (2014). Generalization of clustering coefficients to signed correlation networks. PLoS One 9, e88669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer AO, Borsboom D, Aggen SH & Kendler KS (2012). The pathoplasticity of dysphoric episodes: differential impact of stressful life events on the pattern of depressive symptom inter-correlations. Psychological Medicine 42, 957–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer AO, van Borkulo CD, Giltay EJ, van der Maas HL, Kendler KS, Scheffer M & Borsboom D (2016). Major depression as a complex dynamic system. PLoS One 11, e0167490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer AO, Waldorp LJ, van der Maas HL & Borsboom D (2010a). Comorbidity: a network perspective. Behavioral and Brain Sciences 33, 137–50; discussion 150–93. [DOI] [PubMed] [Google Scholar]
- Cramer AO, Waldorp LJ, van der Maas HL & Borsboom D (2010b). Complex realities require complex theories: Refining and extending the network approach to mental disorders. Behavioral and Brain Sciences 33, 178–193. [Google Scholar]
- Curtiss J, Ito M, Takebayashi Y & Hofmann SG (2018). Longitudinal Network Stability of the Functional Impairment of Anxiety and Depression. Clinical Psychological Science 6, 325–334. [Google Scholar]
- Dablander F & Hinne M (2018). Node centrality measures are a poor substitute for causal inference. Scientific Reports 9, 6846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Beurs D (2017). Network analysis: A novel approach to understand suicidal behaviour. International Journal of Environmental Research and Public Health 14, 219. [Google Scholar]
- de Haan-Rietdijk S, Voelkle MC, Keijsers L & Hamaker EL (2017). Discrete- vs. Continuous-Time Modeling of Unequally Spaced Experience Sampling Method Data. Frontiers in Psychology 8, 1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jonge P, Wardenaar KJ & Wichers M (2015). What kind of thing is depression? Epidemiology and Psychiatric Sciences 24, 312–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Ron J, Fried EI & Epskamp S (2019). Psychological Networks in Clinical Populations: A tutorial on the consequences of Berkson’s Bias. https://psyarxiv.com/5t8zw/ [DOI] [PubMed]
- de Vos S, Wardenaar KJ, Bos EH, Wit EC, Bouwmans MEJ & de Jonge P (2017). An investigation of emotion dynamics in major depressive disorder patients and healthy persons using sparse longitudinal networks. PLoS One 12, e0178586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeYoung CG & Krueger RF (2018). Understanding Psychopathology: Cybernetics and Psychology on the Boundary between Order and Chaos. Psychologial Inquiry 29, 165–174. [Google Scholar]
- Eaton NR (2015). Latent variable and network models of comorbidity: toward an empirically derived nosology. Social Psychiatry and Psychiatric Epidemiology 50, 845–9. [DOI] [PubMed] [Google Scholar]
- Epskamp S (2019). Psychometric network models from time-series and panel data. https://psyarxiv.com/8ha93/ [DOI] [PMC free article] [PubMed]
- Epskamp S, Borsboom D & Fried EI (2018a). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods 50, 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD & Borsboom D (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software 48, 1–18. [Google Scholar]
- Epskamp S & Fried EI (2018). A tutorial on regularized partial correlation networks. Psychological Methods 23, 617–634. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Fried EI, van Borkulo CD, Robinaugh DJ, Marsman M, Dalege J, Rhemtulla M & Cramer AOJ (2018b). Investigating the utility of fixed-margin sampling in network psychometrics. Multivariate Behavioral Research, 1–15. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Kruis J & Marsman M (2017a). Estimating psychopathological networks: Be careful what you wish for. PLoS One 12, e0179891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Maris GKJ, Waldorp LJ & Borsboom D (2016). Network psychometrics. In Handbook of Psychometrics (ed. Irwing P, Hughes D and Booth T). Wiley: New York. [Google Scholar]
- Epskamp S, Rhemtulla M & Borsboom D (2017b). Generalized network psychometrics: Combining network and latent variable models. Psychometrika 82, 904–927. [DOI] [PubMed] [Google Scholar]
- Epskamp S, van Borkulo CD, van der Veen DC, Servaas MN, Isvoranu AM, Riese H & Cramer AOJ (2018c). Personalized network modeling in psychopathology: The importance of contemporaneous and temporal connections. Clinical Psychological Science 6, 416–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein JM (2008). Why model? Journal of Artificial Societies and Social Simulation 11, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- sfahlani FZ, Sayama H, Visser K, Strauss GP(2017). Sensitivity of the positive and negative syndrome (PANSS) in detecting treatment effects via network analysis. Innovations in clinical neuroscience, 14, 59–67. [PMC free article] [PubMed] [Google Scholar]
- Fonseca-Pedrero E, Ortuno J, Debbane M, Chan RCK, Cicero D, Zhang LC, Brenner C, Barkus E, Linscott RJ, Kwapil T, Barrantes-Vidal N, Cohen A, Raine A, Compton MT, Tone EB, Suhr J, Inchausti F, Bobes J, Fumero A, Giakoumaki S, Tsaousis I, Preti A, Chmielewski M, Laloyaux J, Mechri A, Aymen Lahmar M, Wuthrich V, Laroi F, Badcock JC, Jablensky A, Isvoranu AM, Epskamp S & Fried EI (2018). The network structure of schizotypal personality traits. Schizophrenia Bulletin 44, S468–S479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes MK, Wright AG, Markon KE & Krueger RF (2019). Quantifying the reliability and replicability of psychopathology network characteristics. Multivariate Behavioral Research,1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes MK, Wright AGC, Markon KE & Krueger RF (2017a). Evidence that psychopathology symptom networks have limited replicability. Journal of Abnormal Psychology 126, 969–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes MK, Wright AGC, Markon KE & Krueger RF (2017b). Further evidence that psychopathology networks have limited replicability and utility: Response to Borsboom et al. (2017) and Steinley et al. (2017). Journal of Abnormal Psychology 126, 1011–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Schmittmann VD, Bringmann LF & Borsboom D (2013). Perceived causal relations between anxiety, posttraumatic stress and depression: extension to moderation, mediation, and network analysis. European Journal of Psychotraumatology 4, 20656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E (2015). Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Frontiers in Psychology 6, 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI (2017). The 52 symptoms of major depression: Lack of content overlap among seven common depression scales. Journal of Affective Disorders 208, 191–197. [DOI] [PubMed] [Google Scholar]
- Fried EI, Boschloo L, van Borkulo CD, Schoevers RA, Romeijn J, Wichers M, de Jonge P, Nesse RM, Tuerlinckx F & Borsboom D (2015). Commentary: “Consistent superiority of selective serotonin reuptake inhibitors over placebo in reducing depressed mood in patients with major depression”. Frontiers in Psychiatry 6, 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI & Cramer AOJ (2017). Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science 12, 999–1020. [DOI] [PubMed] [Google Scholar]
- Fried EI, Eidhof MB, Palic S, Costantini G, Huisman-van Dijk HM, Bockting CL & Karstoft KI (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science 6, 335–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, Epskamp S, Nesse RM, Tuerlinckx F & Borsboom D (2016). What are ‘good’ depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. Journal of Affective Disorders 189, 314–20. [DOI] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Cramer AO, Boschloo L, Schoevers RA & Borsboom D (2017). Mental disorders as networks of problems: a review of recent insights. Social Psychiatry and Psychiatric Epidemiology 52, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friston KJ, Redish AD & Gordon JA (2017). Computational Nosology and Precision Psychiatry. Computational Psychiatry 1, 2–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein AJ & Chambless DL (1978). A reanalysis of agoraphobia. Behavior Therapy 9, 47–59. [Google Scholar]
- Golino HF & Epskamp S (2017). Exploratory graph analysis: A new approach for estimating the number of dimensions in psychological research. PLoS One 12, e0174035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granic I (2005). Timing is everything: Developmental psychopathology from a dynamic systems perspective. Developmental Review 25, 386–407. [Google Scholar]
- Guloksuz S, Pries LK & van Os J (2017). Application of network methods for understanding mental disorders: pitfalls and promise. Psychological Medicine 47, 2743–2752. [DOI] [PubMed] [Google Scholar]
- Guyon H, Falissard B & Kop JL (2017). Modeling psychological attributes in psychology - An epistemological discussion: Network analysis vs. latent variables. Frontiers in Psychology 8, 798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haag C, Robinaugh DJ, Ehlers A & Kleim B (2017). Understanding the emergence of chronic posttraumatic stress disorder through acute stress symptom networks. JAMA Psychiatry 74, 649–650. [DOI] [PubMed] [Google Scholar]
- Haig BD (2005). An abductive theory of scientific method. Psychological Methods 10, 371–88. [DOI] [PubMed] [Google Scholar]
- Haig BD (2008). Precis of ‘an abductive theory of scientific method’. Journal of Clinical Psychology 64, 1019–22. [DOI] [PubMed] [Google Scholar]
- Hallquist M, Wright AG & Molenaar PC (2019). Problems with centrality measures in psychopathology symptom networks: Why network psychometrics cannot escape psychometric theory. Multivariate Behavioral Research. 1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker EL & Wichers M (2017). No Time Like the Present: Discovering the Hidden Dynamics in Intensive Longitudinal Data. Current Directions in Psychological Science 26, 10–15. [Google Scholar]
- Haslam N, Holland E & Kuppens P (2012). Categories versus dimensions in personality and psychopathology: a quantitative review of taxometric research. Psychological Medicine 42, 903–20. [DOI] [PubMed] [Google Scholar]
- Haslbeck JMB & Lourens LJ (2016). mgm: structure estimation for time-varying mixed graphical models in high-dimensional data. https://arxiv.org/abs/1510.06871
- Haslbeck JMB & Waldorp LJ (2018). How well do network models predict observations? On the importance of predictability in network models. Behavior Research Methods 50, 853–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasmi L, Drukker M, Guloksuz S, Menne-Lothmann C, Decoster J, van Winkel R, Collip D, Delespaul P, De Hert M, Derom C, Thiery E, Jacobs N, Rutten BPF, Wichers M & van Os J (2017). Network Approach to Understanding Emotion Dynamics in Relation to Childhood Trauma and Genetic Liability to Psychopathology: Replication of a Prospective Experience Sampling Analysis. Frontiers in Psychology 8, 1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AM & Strauss JL (1998). Dynamic systems theory as a paradigm for the study of change in psychotherapy: an application to cognitive therapy for depression. Journal of Consulting and Clinical Psychology 66, 939–47. [DOI] [PubMed] [Google Scholar]
- Hayes AM, Yasinski C, Ben Barnes J & Bockting CL (2015). Network destabilization and transition in depression: New methods for studying the dynamics of therapeutic change. Clinical Psychology Review 41, 27–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeren A & McNally RJ (2016). A call for complexity in the study of social anxiety disorder. Commentary: The aetiology and maintenance of social anxiety disorder: A synthesis of complementary theoretical models and formulation of a new integrated model. Frontiers in Psychology 7, 1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeren A & McNally RJ (2018). Social Anxiety Disorder as a Densely Interconnected Network of Fear and Avoidance for Social Situations. Cognitive Therapy and Research 42, 103–113. [Google Scholar]
- Held BS (2017). The distinction between psychological kinds and natural kinds revisited: Can updated natural-kind theory help clinical psychological science and beyond meet psychology’s philosophical challenges? Review of General Psychology 21, 82–94. [Google Scholar]
- Hoffart A & Johnson SU (2017). Psychodynamic and cognitive-behavioral therapies are more different than you think: Conceptualizations of mental problems and consequences for studying mechanisms of change. Clinical Psychological Science 5, 1070–1086. [Google Scholar]
- Hoffman M, Steinley D, Trull TJ & Sher KJ (2018). Criteria definitions and network relations: The importance of criterion thresholds. Clinical Psychological Science 6, 506–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG (2014). Toward a cognitive-behavioral classification system for mental disorders. Behavior Therapy 45, 576–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG & Curtiss J (2018). A complex network approach to clinical science. European Journal of Clinical Investigation 48, e12986. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss J & McNally RJ (2016). A complex network perspective on clinical science. Perspectives on Psychological Science 11, 597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosseinichimeh N, Wittenborn AK, Rick J, Jalali MS & Rahmandad H (2018). Modeling and estimating the feedback mechanisms among depression, rumination, and stressors in adolescents. PLoS One 13, e0204389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huys QJ, Maia TV & Frank MJ (2016). Computational psychiatry as a bridge from neuroscience to clinical applications. Nature Neuroscience 19, 404–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isvoranu AM, Borsboom D, van Os J & Guloksuz S (2016). A network approach to environmental impact in psychotic disorder: brief theoretical framework. Schizophrenia Bulletin 42, 870–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones P, Williams D & McNally RJ (2019). Sampling Variability is not Nonreplication: A Bayesian Reanalysis of Forbes, Wright, Markon, & Krueger. https://psyarxiv.com/egwfj/ [DOI] [PubMed]
- Jones PJ, Mair P & McNally R (2018). Visualizing psychological networks: a tutorial in R. Frontiers in Psychology 9, 1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS (2016). The nature of psychiatric disorders. World Psychiatry 15, 5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Flint J, Borsboom D & Fried EI (2018). The centrality of DSM and non-DSM depressive symptoms in Han Chinese women with major depression. Journal of Affective Disorders 227, 739–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Zachar P & Craver C (2011). What kinds of things are psychiatric disorders? Psychological Medicine 41, 1143–50. [DOI] [PubMed] [Google Scholar]
- Klippel A, Viechtbauer W, Reininghaus U, Wigman J, van Borkulo C, MERGE Inez Myin-Germeys, & Wichers M (2018). The cascade of stress: a network approach to explore differential dynamics in populations varying in risk for psychosis. Schizophrenia Bulletin, 44, 328–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruis J & Maris G (2016). Three representations of the Ising model. Scientific Reports 6, 34175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuiper RM & Ryan O (2018). Drawing Conclusions from Cross-Lagged Relationships: Re-Considering the Role of the Time-Interval. Structural Equation Modeling: A Multidisciplinary Journal 25, 809–823. [Google Scholar]
- Levine SZ & Leucht S (2016). Identifying a system of predominant negative symptoms: Network analysis of three randomized clinical trials. Schizophrenia Research 178, 17–22. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Brosof LC, Vanzhula I, Christian C, Jones P, Rodebaugh TL, Langer JK, White EK, Warren C, Weeks JW, Menatti A, Lim MH & Fernandez KC (2018a). Social anxiety and eating disorder comorbidity and underlying vulnerabilities: Using network analysis to conceptualize comorbidity. International Journal of Eating Disorders 51, 693–709. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Vanzhula IA, Brosof LC & Forbush K (2018b). Network Analysis as an Alternative Approach to Conceptualizing Eating Disordrs: Implications for Research and Treatment. Eating Disorders 20, 67. [DOI] [PubMed] [Google Scholar]
- Looijestijn J, Blom JD, Aleman A, Hoek HW & Goekoop R (2015). An integrated network model of psychotic symptoms. Neuroscience & Biobehavioral Reviews 59, 238–50. [DOI] [PubMed] [Google Scholar]
- Lord FM & Novick MR (1968). Statistical theories of mental test scores. Addison-Wesley: Reading. [Google Scholar]
- Lydon-Staley DM, Schnoll RA, Hitsman B & Bassett DS (2018). The network structure of tobacco withdrawal in a community sample of smokers treated with nicotine patch and behavioral counseling. Nicotine & Tobacco Research, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques DR & Azevedo MHP (2018). Potentialities of network analysis for sleep medicine. Journal of Psychosomatic Research 111, 89–90. [DOI] [PubMed] [Google Scholar]
- Marsman M, Borsboom D, Kruis J, Epskamp S, van Bork R, Waldorp LJ, Maas H & Maris G (2018). An introduction to network psychometrics: Relating Ising network models to item response theory models. Multivariate Behavioral Research 53, 15–35. [DOI] [PubMed] [Google Scholar]
- Maung HH (2016). Diagnosis and causal explanation in psychiatry. Studies in History and Philosophy of Biological and Biomedical Sciences 60, 15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGorry PD, Hartmann JA, Spooner R & Nelson B (2018). Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry 17, 133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ (2012). The ontology of posttraumatic stress disorder: Natural kind, social construction, or causal system? Clinical Psychology: Science and Practice 19, 220–228. [Google Scholar]
- McNally RJ (2016). Can network analysis transform psychopathology? Behaviour Research and Therapy 86, 95–104. [DOI] [PubMed] [Google Scholar]
- McNally RJ (2017). Networks and nosology in posttraumatic stress disorder. JAMA Psychiatry 74, 124–125. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK & Borsboom D (2015). Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science 3, 836–849. [Google Scholar]
- Muchinsky PM (1996). The correction for attenuation. Educational and Psychological Measurement 56, 63–75. [Google Scholar]
- Nelson B, McGorry PD, Wichers M, Wigman JTW & Hartmann JA (2017). Moving from static to dynamic models of the onset of mental disorder: A review. JAMA Psychiatry 74, 528–534. [DOI] [PubMed] [Google Scholar]
- Pe ML, Kircanski K, Thompson RJ, Bringmann LF, Tuerlinckx F, Mestdagh M, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, Kuppens P & Gotlib IH (2015). Emotion-network density in major depressive disorder. Clinical Psychological Science 3, 292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl J (2009). Causality: Models, reasoning, and inference. Cambridge University Press: Cambridge. [Google Scholar]
- Pincus D & Metten A (2010). Nonlinear dynamics in biopsychosocial resilience. Nonlinear Dynamics, Psychology, and Life Sciences 14, 353–80. [PubMed] [Google Scholar]
- Porter D (2015). Colonization by/in psychiatry: From over-medicalization to democratization. Journal of Ethics in Mental Health Open Volume, 1. [Google Scholar]
- Radden J (2018). Rethinking disease in psychiatry: Disease models and the medical imaginary. Journal of Evaluation in Clinical Practice 24, 1087–1092. [DOI] [PubMed] [Google Scholar]
- Rikkert O, Marcel GM, Dakos V, Buchman TG, Boer RD, Glass L, Cramer AOJ, Simon L, van Nes E, Sugihara G, Ferrari MD, Tolner EA, van de Leemput I, Lagro J, Melis R & Scheffer M (2016). Slowing down of recovery as generic risk marker for acute severity transitions in chronic diseases. Critical Care Medicine 44, 601–606. [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, Haslbeck J, Waldorp L, Kossakowski JJ, Fried EI, Millner AJ, McNally RJ, Kendler KS, van Ness E, Scheffer M & Borsboom D (2019). Advancing the network theory of mental disorders: A computational model of panic disorder. doi: 10.31234/osf.io/km37w [DOI] [Google Scholar]
- Robinaugh DJ, Millner AJ & McNally RJ (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology 125, 747–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodebaugh TL, Tonge NA, Piccirillo ML, Fried E, Horenstein A, Morrison AS, Goldin P, Gross JJ, Lim MH, Fernandez KC, Blanco C, Schneier FR, Bogdan R, Thompson RJ & Heimberg RG (2018). Does centrality in a cross-sectional network suggest intervention targets for social anxiety disorder? Journal of Consulting and Clinical Psychology 86, 831–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouquette A, Pingault JB, Fried EI, Orri M, Falissard B, Kossakowski JJ, Vitaro F, Tremblay R, Cote SM & Borsboom D (2018). Emotional and behavioral symptom network structure in elementary school girls and association with anxiety disorders and depression in adolescence and early adulthood: a network analysis. JAMA Psychiatry 75, 1173–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell JD, Neill EL, Carrion VG & Weems CF (2017). The network structure of posttraumatic stress symptoms in children and adolescents exposed to disasters. Journal of the American Academy of Child and Adolescent Psychiatry 56, 669–677 e5. [DOI] [PubMed] [Google Scholar]
- Ruzzano L, Borsboom D & Geurts HM (2015). Repetitive behaviors in autism and obsessive-compulsive disorder: new perspectives from a network analysis. Journal of Autism and Developmental Disorders 45, 192–202. [DOI] [PubMed] [Google Scholar]
- Santos H Jr., Fried EI, Asafu-Adjei J & Ruiz RJ (2017). Network structure of perinatal depressive symptoms in Latinas: Relationship to stress and reproductive biomarkers. Research in Nursing & Health 40, 218–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheffer M (2009). Critical transitions in nature and society. Princeton University Press, Princeton, NJ. [Google Scholar]
- Schiepek G (2003). A dynamic systems approach to clinical case formulation. European Journal of Psychological Assessment 19, 175–184. [Google Scholar]
- Schuler M, Wittmann M, Faller H & Schultz K (2018). The interrelations among aspects of dyspnea and symptoms of depression in COPD patients – a network analysis. Journal of Affective Disorders 240, 33–40. [DOI] [PubMed] [Google Scholar]
- Schuurman NK, Ferrer E, de Boer-Sonnenschein M & Hamaker EL (2016). How to compare cross-lagged associations in a multilevel autoregressive model. Psychological Methods 21, 206–221. [DOI] [PubMed] [Google Scholar]
- Schuurman NK, Houtveen JH & Hamaker EL (2015). Incorporating measurement error in n = 1 psychological autoregressive modeling. Frontiers in Psychology 6, 1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweren L, van Borkulo CD, Fried E & Goodyer IM (2018). Assessment of symptom network density as a prognostic marker of treatment response in adolescent depression. JAMA Psychiatry 75, 98–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KE, Crosby RD, Wonderlich SA, Forbush KT, Mason TB & Moessner M (2018). Network analysis: An innovative framework for understanding eating disorder psychopathology. International Journal of Eating Disorders 51, 214–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southward MW & Cheavens JS (2018). Identifying core deficits in a dimensional model of Borderline Personality Disorder features: A network analysis. Clinical Psychological Science 6, 685–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tio P, Epskamp S, Noordhof A & Borsboom D (2016). Mapping the manuals of madness: Comparing the ICD-10 and DSM-IV-TR using a network approach. International Journal of Methods in Psychiatric Research 25, 267–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treadway MT & Leonard CV (2016). Isolating biomarkers for symptomatic states: considering symptom-substrate chronometry. Molecular Psychiatry 21, 1180–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tretter F & Loffler-Stastka H (2018). Steps toward an integrative clinical systems psychology. Frontiers in Psychology 9, 1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tryon WW (2018). Mediators and Mechanisms. Clinical Psychological Science 6, 619–628. [Google Scholar]
- Tsou JY (2016). Natural kinds, psychiatric classification and the history of the DSM. History of Psychiatry 27, 406–424. [DOI] [PubMed] [Google Scholar]
- Tzur-Bitan D, Meiran N & Shahar G (2010). The importance of modeling comorbidity using an intra-individual, time-series approach. Behavioral and Brain Sciences 33, 172–3. [DOI] [PubMed] [Google Scholar]
- van Bork R, Epskamp S, Rhemtulla M, Borsboom D & van der Maas HL (2017). What is the p-factor of psychopathology? Some risks of general factor modeling. Theory & Psychology 27, 759–773. [Google Scholar]
- van Borkulo CD, Borsboom D, Epskamp S, Blanken TF, Boschloo L, Schoevers RA & Waldorp LJ (2014). A new method for constructing networks from binary data. Scientific Reports 4, 5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo CD, Borsboom D & Schoevers RA (2016). Group-level symptom networks in depression-Reply. JAMA Psychiatry 73, 411–2. [DOI] [PubMed] [Google Scholar]
- van Borkulo CD, Boschloo L, Borsboom D, Penninx BW, Waldorp LJ & Schoevers RA (2015). Association of symptom network structure with the course of depression. JAMA Psychiatry 72, 1219–26. [DOI] [PubMed] [Google Scholar]
- van Borkulo CD, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, Borsboom D & Waldorp L (2017). Comparing network structures on three aspects: A permutation test. https://www.researchgate.net/publication314750838_Comparing_network_structures_on_three_aspects_A_permutation_test [DOI] [PubMed]
- van de Leemput IA, Wichers M, Cramer AOJ, Borsboom D, Tuerlinckx F, Kuppens P, van Nes EH, Viechtbauer W, Giltay EJ, Aggen SH, Derom C, Jacobs N, Kendler KS, van der Maas HLJ, Neale MC, Peeters F, Thiery E, Zachar P & Scheffer M (2014). Critical slowing down as early warning for the onset and termination of depression. Proceedings of the National Academy of Sciences of the United States of America 111, 87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Hout M (2014). Psychiatric symptoms as pathogens. Journal of Treatment Evaluation 11, 153–159. [Google Scholar]
- van Loo HM & Romeijn JW (2015). Psychiatric comorbidity: fact or artifact? Theor Med Bioeth 36, 41–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Loo HM, Van Borkulo CD, Peterson RE, Fried EI, Aggen SH, Borsboom D & Kendler KS (2018). Robust symptom networks in recurrent major depression across different levels of genetic and environmental risk. J Affect Disord 227, 313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J, Delespaul P, Wigman J, Myin-Germeys I & Wichers M (2013a). Beyond DSM and ICD: introducing “precision diagnosis” for psychiatry using momentary assessment technology. World Psychiatry 12, 113–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J, Delespaul P, Wigman J, Myin-Germeys I & Wichers M (2013b). Psychiatry beyond labels: introducing contextual precision diagnosis across stages of psychopathology. Psychological Medicine 43, 1563–7. [DOI] [PubMed] [Google Scholar]
- van Rooijen G, Isvoranu AM, Kruijt OH, van Borkulo CD, Meijer CJ, Wigman JTW, Ruhe HG, de Haan L & investigators G (2018). A state-independent network of depressive, negative and positive symptoms in male patients with schizophrenia spectrum disorders. Schizophr Res 193, 232–239. [DOI] [PubMed] [Google Scholar]
- Verhoeff B (2013). The autism puzzle: challenging a mechanistic model on conceptual and historical grounds. Philos Ethics Humanit Med 8, 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Stockert SHH, Fried EI, Armour C & Pietrzak RH (2018). Evaluating the stability of DSM-5 PTSD symptom network structure in a national sample of U.S. military veterans. Journal of Affective Disorders 229, 63–68. [DOI] [PubMed] [Google Scholar]
- Vosgerau G & Soom P (2018). Reduction without elimination: Mental disorders as causally efficacious properties. Minds & Machines 28, 311–330. [Google Scholar]
- Waller NG & Meehl PE (1998). Multivariate taxometric procedures: Distinguishing types from continua. Sage: Thousand Oaks. [Google Scholar]
- Walter H (2013). The third wave of biological psychiatry. Front Psychol 4, 582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardenaar KJ & de Jonge P (2013). Diagnostic heterogeneity in psychiatry: towards an empirical solution. BMC Medicine 11, 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wass S & Karmiloff-Smith A (2010). The missing developmental dimension in the network perspective. Behav Brain Sci 33, 175–6. [DOI] [PubMed] [Google Scholar]
- Wichers M (2014). The dynamic nature of depression: a new micro-level perspective of mental disorder that meets current challenges. Psychological Medicine 44, 1349–60. [DOI] [PubMed] [Google Scholar]
- Wichers M, Wigman JTW, Bringmann LF & De Jonge P (2017). Mental disorders as networks: Some cautionary reflections on a promising approach. Social Psychiatry and Psychiatric Epidemiology 52, 143–145. [DOI] [PubMed] [Google Scholar]
- Wichers M, Wigman JTW & Myin-Germeys I (2015). Micro-level affect dynamics in psychopathology viewed from complex dynamical system theory. Emotion Review 7, 362–367. [Google Scholar]
- Williams D & Rast P (2018). Back to the basics: rethinking partial correlation network methodology. https://osf.io/fndru [DOI] [PMC free article] [PubMed]
- Williams D, Rast P & Mulder J (2019). Comparing gaussian graphical models with the posterior predictive distribution and bayesian model selection. https://psyarxiv.com/yt386/ [DOI] [PMC free article] [PubMed]
- Wittenborn AK, Rahmandad H, Rick J & Hosseinichimeh N (2016). Depression as a systemic syndrome: mapping the feedback loops of major depressive disorder. Psychological Medicine 46, 551–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wusten C, Schlier B, Jaya ES, Genetic R, Outcome of Psychosis I, Fonseca-Pedrero E, Peters E, Verdoux H, Woodward TS, Ziermans TB & Lincoln TM (2018). Psychotic experiences and related distress: A cross-national comparison and network analysis based on 7141 participants from 13 countries. Schizophrenia Bulletin 44, 1185–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X, Ram N, Gest SD, Lydon-Staley DM, Conroy DE, Pincus AL & Molenaar PCM (2018). Socioemotional dynamics of emotion regulation and depressive symptoms: A person-specific network approach. Complexity, 2018, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yordanova J, Kolev V, Kirov R & Rothenberger A (2010). Comorbidity in the context of neural network properties. Behav Brain Sci 33, 176–7. [DOI] [PubMed] [Google Scholar]
- Young G (2015). Causality in Psychiatry: A Hybrid Symptom Network Construct Model. Frontiers in Psychiatry 6, 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachar P (2015). Psychiatric disorders: natural kinds made by the world or practical kinds made by us? World Psychiatry 14, 288–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X, Yang B, Liu X & Chen H (2017). Statistical inference for community detection in signed networks. Physical Review E 95, 042313. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.