Highlights
-
•
Spatiotemporal clusters of COVID-19 in South Korea were analyzed.
-
•
The pattern and duration of clusters changed and reduced over time.
-
•
South Korea's containment strategy was effective in early detection and mitigation.
Keywords: COVID-19, Spatiotemporal analysis, Government response, South Korea
Abstract
Objectives
The aim of this study was to assess how coronavirus disease 2019 (COVID-19) clustered across districts in South Korea and to assess whether the pattern and duration of clusters changed following the country's containment strategy.
Methods
A spatiotemporal analysis of COVID-19 daily confirmed cases by 250 districts in South Korea from January 20 to May 31, 2020, obtained from the Korea Centers for Disease Control and Prevention and each provincial website, was conducted. The global Moran's I statistic was used for spatial autocorrelation analysis, and the retrospective space-time scan statistic was used to analyze spatiotemporal clusters of COVID-19.
Results
The geographical distribution showed strong spatial autocorrelation, with a global Moran's I coefficient of 0.784 (p = 0.0001). Twelve statistically significant spatiotemporal clusters were identified by space–time scan statistic using a discrete Poisson model. The spatial pattern of clusters changed and the duration of clusters became shorter over time.
Conclusions
The results indicate that South Korea's containment strategy for COVID-19 was highly effective in both early detection and mitigation, with recent clusters being small in size and duration. Lessons from South Korea should spark a discussion on epidemic response.
Introduction
In December 2019, an outbreak of viral pneumonia was reported in Wuhan City, Hubei Province, China (World Health Organization, 2020a), which was later found to have been caused by a novel coronavirus–severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)–and was named coronavirus disease 2019 (COVID-19). It quickly spread across China and beyond following human mobility patterns, and the World Health Organization (WHO) declared the outbreak a pandemic on March 11, 2020 (World Health Organization, 2020c). As of May 31, 2020, more than 5.93 million cases of COVID-19 have been reported in over 200 countries and territories worldwide, resulting in approximately 367 166 deaths (World Health Organization, 2020b).
In South Korea, the first case of COVID-19 was identified on January 20, 2020, and 30 cases had been confirmed by February 17. However, patient 31 was a super-spreader’ who had attended massive Shincheonji church services in Daegu on February 9 and 16, and tested positive on February 18. A large-scale outbreak emerged in the city of Daegu, located in the southeast region of the country, which soon became the first COVID-19 epicenter outside China, with up to 741 daily cases (Choi and Ki, 2020).
With the surge of cases at the end of February, measures such as avoiding mass gatherings, wearing face masks, and voluntary physical distancing were implemented immediately. Even though there were recommendations to limit operations of highly crowded and confined spaces, as well as to collect visitor logs, there were no business bans or lockdowns, with the exception of a delay in opening schools (postponed from early March to the end of May).
In addition, South Korea responded swiftly with a strategy called ‘3T-Test, Trace, and Treat’. This involved aggressive and accurate tracking of infected individuals and their potential contacts, and rapid identification of when and where the infection had occurred (epidemiological investigation), followed by rapid mass testing using drive-through or walk-through screening stations for easy access to tests. The 3T strategy was supported by the Infectious Disease Control and Prevention Act (Korea Legislation Research Institute, 2019), which enables the rigorous tracing and testing of potential contacts of confirmed cases utilizing their credit card transaction history, mobile phone GPS data, and CCTV (closed-circuit television) security camera footage when necessary (KCDC division of COVID-19 National Emergency Response Center, 2020). Patients were isolated in hospitals (community treatment centers) until they recovered, their direct contacts were required to be quarantined for 2 weeks (mandatory), and information on the location of those who tested positive was publicly released (facilitating the targeting of physical distancing by the population). The Universal Health Coverage (UHC), provided by the Korea National Health Insurance Service (NHIS), was an important foundation to cope with the epidemic through free testing and low-cost treatment. As a result, South Korea became one of the few countries to dramatically slow the spread of the disease without resorting to lockdowns, a business ban, or suspension of public transportation.
As of May 31, 2020, there have been 11 468 confirmed cases, 270 deaths, and 876 060 people have tested negative (1.3% test positivity rate) in Korea (Korea Centers for Disease Control and Prevention, 2020). The continuation of the 3T strategy was critical in quickly identifying and containing recent outbreaks in the Seoul metropolitan region (Seoul City and neighboring districts) that arose from group infections in night clubs and logistics centers following the relaxation of physical distancing measures in May.
Rapid detection of when and where transmission occurs is crucial to reduce secondary infections, to avoid the surge of small local outbreaks, and ultimately to control the epidemic. This retrospective spatiotemporal analysis of COVID-19 in South Korea was conducted in light of the country's response. An investigation was performed to assess how COVID-19 clustered across districts, and whether the pattern and duration of clusters changed and reduced over time following the country's response.
Methods
Data sources
South Korea has 17 administrative divisions (provinces) that are further divided into 250 districts (called si/gun/gu). Daily confirmed cases of COVID-19 by district from January 20 to May 31, 2020 were obtained from the Korea Centers for Disease Control and Prevention (KCDC) (Korea Centers for Disease Control and Prevention, 2020) and from each provincial website (Seoul Metropolitan Government, 2020). In addition, aggregated data based on all of the publicly available information in Korea are accessible online through Data Science for COVID-19 (DS4C, 2020). Data included the case number, province, district (si/gun/gu), date of diagnosis, date of release from hospital/community treatment center, outcome (released from hospital/isolated for treatment/died), sex, and age. Total population by district in 2020 and shapefiles for mapping were obtained from Statistics Korea (Statistics Korea, 2020).
Statistical analysis
The global Moran's I statistic was used to assess whether the cumulative incidence of COVID-19 per 100 000 population in each district was spatially correlated. Moran's I follows a normal distribution and significance is tested based on a random permutation procedure of Monte Carlo simulation consisting of 9999 random replications of the dataset (Besag and Diggle, 1977). The values of I range from −1 (clustering of dissimilar values) to +1 (clustering of similar values), and a value of zero indicates no spatial autocorrelation. The greater the absolute value of I, the stronger the spatial autocorrelation. Given the physical characteristics of the Korean peninsula (with many islands), we defined the neighborhood structure as the k nearest neighbors (k = 4) based on the centroid distance (1/d ij, where d ij represents the Euclidean distances between the ith and jth points). Open GeoDa v 1.14 (Anselin et al., 2006) was used for the spatial autocorrelation analysis.
A retrospective space-time scan statistic method (Kulldorff et al., 1998) was used to include a time dimension into the analysis and identify where and when (and for how long) clusters occurred. A discrete Poisson model was used to analyze spatiotemporal clusters of COVID-19 cases in SaTScan v 9.6 (Kulldorff and Information Management Services Inc., 2018). As COVID-19 spreads from person to person and a higher number of cases are expected in more densely populated areas, a Poisson model was chosen to account for the population in each district.
The scanning window for space-time scan statistics is a cylindrical window with a circular geographic base and with height corresponding to time (Kulldorff et al., 1998). The base is centered around one of the possible centroids positioned throughout the districts, with the radius varying in size continuously from zero to a specified maximum value (Kulldorff et al., 1998). The height reflects any possible time interval including not only the total study period but also the interval of less than or equal to half of the study period (Kulldorff et al., 1998). In this study, a day was selected as a time interval, since the number of daily cases increased rapidly due to the infectiousness of the disease. The maximum spatial cluster size was set to 5% of the population at risk and the maximum temporal cluster size was set to 4 weeks, 25% of the total duration, in order to avoid extremely large (and thus meaningless) clusters. In addition, the minimum number of cases in a cluster of high rates was set to 30.
A likelihood ratio test was used to identify the spatiotemporal clusters of COVID-19 cases. The likelihood was calculated for each cylinder to determine whether the observed number of cases exceeded the expected number of cases, based on the number of cases and population size observed in the geographical district over a particular time period (Kulldorff, 1997, Linton et al., 2014). The ratio of observed to expected cases represents the risk within the window, and the relative risk represents the risk within the window compared to the risk outside the window (Linton et al., 2014). The statistical significance was evaluated using Monte Carlo simulation consisting of 999 random replications of the dataset (Dwass, 1957, Kulldorff and Nagarwalla, 1995). All mappings were done in ArcMap v 10.6.1 (ESRI Inc., 2018).
Results
As of May 31, 2020, the cumulative number of confirmed COVID-19 cases in South Korea was 11 468 (including 1259 imported cases), with 270 deaths. The region with the largest number of cases was the city of Daegu (n = 6883), followed by Gyeongbuk Province (n = 1379), while the provinces of Jeonbuk and Jeonnam had only 21 and 19 cases, respectively, during the entire study period. Overall, the regional distribution of confirmed cases varied significantly.
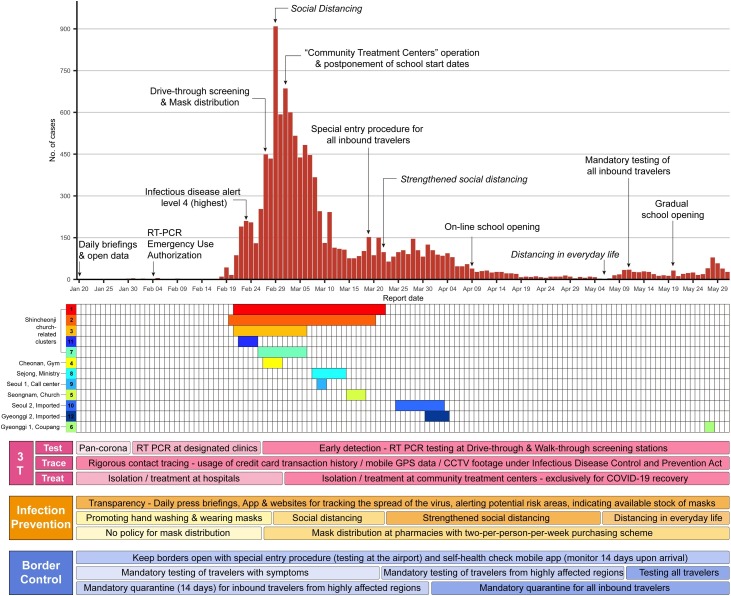
The time series of the daily confirmed cases showed a surge at the end of February (a maximum of 909 cases reported in one single day – February 29), with the epidemic contained as of April 30 (Figure 1 ). Recently, after the consecutive holidays from April 30 to May 5 and the relaxation of social distancing measures on May 6, the daily number of new infections increased to double digits due to group infections around a few nightclubs in a district (Itaewon) in Seoul and logistics centers in Gyeonggi Province. The government has been guarding against the possibility of another surge of infections.
Figure 1.
Epidemiological curve, timeline for each cluster (categorized by clustering events), and public health interventions.
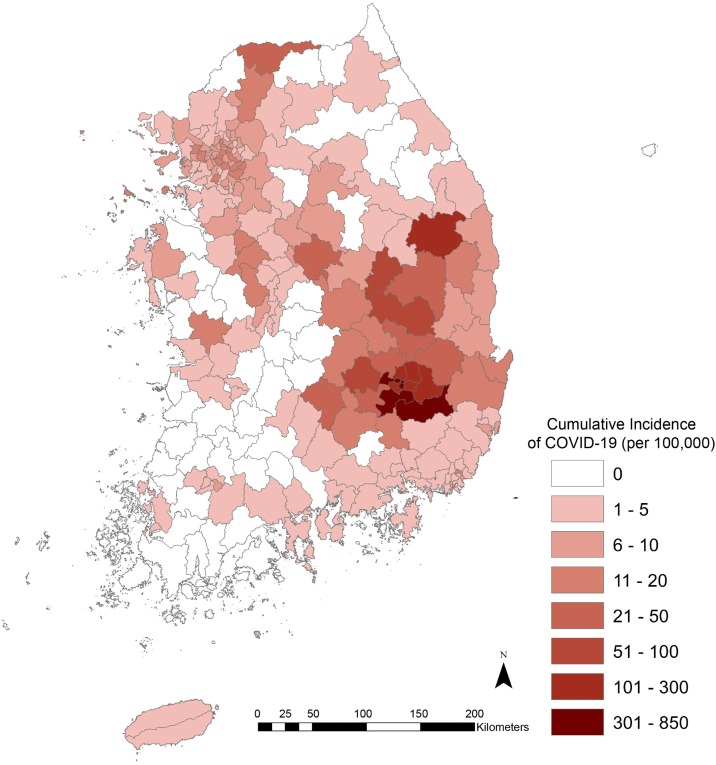
Figure 2 shows the geographical distribution of COVID-19 cumulative incidence per 100 000 population (daily cases aggregated from January 20 to May 31, 2020). The distribution showed strong spatial autocorrelation, with a global Moran's I coefficient of 0.784 (p = 0.0001).
Figure 2.
Cumulative incidence of COVID-19 cases per 100 000 people by district, South Korea, January 20 to May 31, 2020.
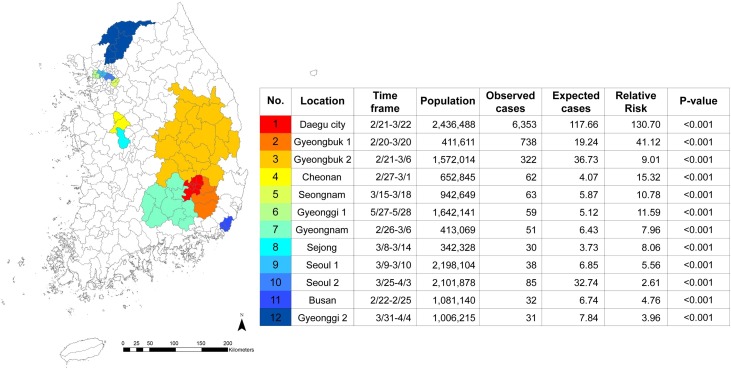
The space-time scan statistics identified 12 statistically significant clusters, without spatial overlap and recurrence (Figure 3). Clusters were color-coded in order from the highest log-likelihood ratio to the lowest, and the same color key is used in Figure 1, Figure 3. The most likely cluster (number 1) was located in Daegu City (eight small districts). The city had more than 700 daily cases within the duration of the cluster, resulting in 6353 cases in total and a relative risk of 130.70. This cluster occurred early (February 21 to March 22, 2020) and had the longest duration, 31 days. The second-longest cluster (number 2) spanned 30 days, was located in Gyeongbuk Province (three neighboring districts of Daegu City), and was adjacent to cluster number 1.
Figure 3.
Location and characteristics of spatiotemporal clusters of COVID-19 in South Korea.
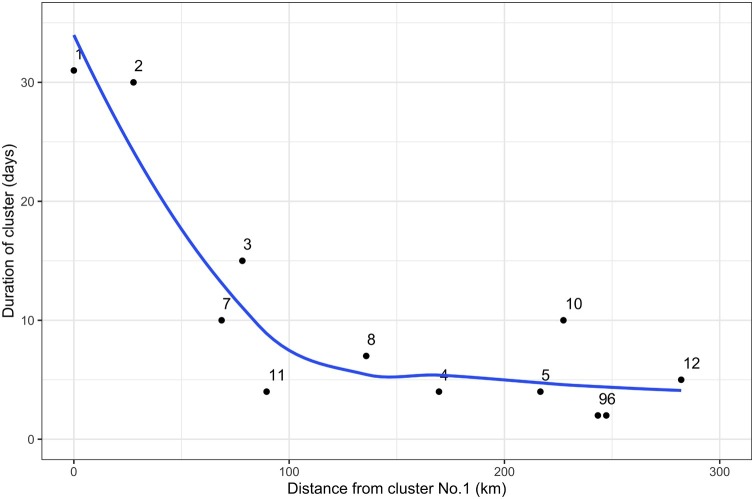
Clusters 1, 2, 3, and 7 overlapped in time, and were adjacent, while clusters 11 and 4 also overlapped in time with the previous four clusters, but did not share borders. The most recent cluster (number 6) captured the new outbreak in Gyeonggi Province that arose from group infections in Coupang logistics centers following the relaxation of social distancing measures. Progressively, the duration of clusters became shorter, and their location further from Daegu (cluster number 1), as shown in Figure 4 .
Figure 4.
Distance from the Daegu cluster (number 1) to each spatiotemporal cluster and the respective duration of the cluster. Each point is labeled following cluster numbers shown in Figure 3. The blue line was fitted in R using locally weighted least squares regression (LOESS).
Discussion
This study provides an overview of the spatiotemporal patterns of COVID-19 in South Korea at the district level. Spatial autocorrelation analysis indicated a pattern of spatial clustering of COVID-19 across the country. Considering both space and time, 12 statistically significant clusters were identified. Most of the likely clusters happened early, had a longer duration, and were mainly concentrated in Daegu City and neighboring districts. The majority of the recent clusters were located in the Seoul metropolitan region (Seoul City and Gyeonggi Province) and had a shorter duration. Clusters persisted for 10.3 days, on average, ranging from 2 to 31 days.
According to the time frame and the geographical distribution of spatiotemporal clusters, as well as epidemiological investigation, clusters 1, 2, 3, 7, and 11 were related to Shincheonji church gathering events. The long duration and high relative risks of these early clusters indicate the impact of a series of super-spreading events (Lloyd-Smith et al., 2005) prior to the implementation of appropriate containment measures. The most recent clusters (numbers 5, 6, 9, 10, and 12) were located in Seoul City (the capital of South Korea, with a population of nearly 10.5 million people, one-fifth of the national population) and its neighboring districts, suggesting that densely populated districts are more likely to have clusters once the infection spreads in the region, due to the transmission dynamics of COVID-19.
After implementing social distancing measures and consolidating the 3T strategy during the Daegu City outbreak, Korea did not observe another large-scale outbreak. Progressively, the location of clusters moved from Daegu to Seoul metropolitan region and had a much smaller spatial extent and shorter duration, suggesting that containment measures play a role in both early detection and mitigation. Indeed, all 12 clusters detected by the scan statistic were linked to areas highlighted in the KCDC epidemiological investigation records.
Although the containment strategies adopted by Korea were successful, there could be challenges to replicating them in other countries due to privacy issues. For example, aggressive contact tracing (real-time) utilizing credit card transaction history, mobile phone GPS data, and CCTV footage raises concerns about overexposure of private information on people's movements. This requires public trust in the government, and cannot be implemented suddenly. South Korea learned the importance of preparedness through its own failure in responding to the Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in 2015 (Oh et al., 2018). The legislation for current contact-tracing methods – enacting the government's authority to collect credit card and mobile phone data, and sharing the recent course of confirmed patients – was established in the aftermath of the MERS-CoV outbreak by amending the Infectious Disease Control and Prevention Act (Korea Legislation Research Institute, 2019) to effectively control an outbreak and to ensure the public's right to know (KCDC division of COVID-19 National Emergency Response Center, 2020).
The MERS-CoV experience certainly helped Korea to improve disease prevention and control, and these measures could not have been enacted without the previous failure (Normile, 2020). In fact, the restriction on the freedom of movement of patients and their contacts, as well as rigorous contact tracing, has been imperative in minimizing further outbreaks and in preserving the freedom of movement of the rest of society. In addition, prompt epidemiological investigation helped not only to control the epidemic but also to avoid unnecessary costly interventions (Lipsitch et al., 2020). Furthermore, as a result of early detection and treatment, the demand for intensive care unit (ICU) resources and the case fatality rate of COVID-19 have been kept relatively low (Davies et al., 2020).
With regard to imported cases, these were mostly introduced by Koreans returning to the country (87.5%). Of the 1259 imported cases, 533 were from the Americas (42.3%), 473 from Europe (37.6%), and 19 from China (1.5%). The study data, however, did not include information indicating which cases were imported, and therefore it was not possible to assess the potential role of importation on the observed spatial and temporal patterns of COVID-19 in South Korea. Yet, according to the KCDC, the number of imported cases has increased rapidly since mid-March and most have been Koreans returning from Europe or the Americas (Korea Centers for Disease Control and Prevention, 2020). Therefore, it is likely that importation was associated with Korean international students and expatriates returning home (mostly in Seoul and Gyeonggi Province).
This study has some limitations. First, the date of diagnosis was used instead of the date of symptom onset, due to data availability. However, the lag between symptom onset and diagnosis has been estimated to be about 7 days (Korean Society of Infectious Diseases et al., 2020), and therefore we do not expect this to have compromised the study results. Second, underestimation of the incidence is expected due to undetected asymptomatic cases, despite intense testing (as of May 31, 2020, the test positivity rate was 1.3%; 11 468 had tested positive and 876 060 had tested negative). Korea is conducting nationwide COVID-19 antibody testing (expected to be completed in the near future, according to the KCDC) (Yonhap News, 2020). Nevertheless, as we modeled spatiotemporal clusters of disease, undetected asymptomatic cases would likely not change the study conclusions. Third, daily confirmed cases for some districts were aggregated at the city level due to data availability (e.g., eight districts were aggregated as one Daegu City) for the space–time cluster analysis. The results reflect the spatial scale used. More detailed information, if available, would offer the opportunity to fine-tune the analysis at a much finer spatial detail. Broadly, however, it is unlikely that the location of clusters would be radically different.
South Korea's universal healthcare was the backbone of the country's successful COVID-19 containment, corroborating the importance of target 3.8 of WHO Sustainable Development Goal 3 (World Health Organization, 2017). However, Korea's successful containment strategy, while keeping borders open and preserving the free movement of people (except those who tested positive and their contacts), demonstrates that the epidemic can be contained effectively without lockdowns, blanket entry bans, the suspension of international traffic, and travel restrictions (Chinazzi et al., 2020). Many countries turned inward to shield themselves in response to COVID-19 and implemented lockdowns that resulted in significant socio-economic costs. Projections from the International Monetary Fund (International Monetary Fund, 2020) indicate GDP losses of around 6% (as high as 9.1% in Italy), while in South Korea the loss is estimated at 1.2% of GDP (Argente et al., 2020).
South Korea's response cannot be easily adopted by most countries. Furthermore, it would not have been possible had the country not learned the lessons of the MERS-CoV outbreak, and had the government not been trusted by the population. South Korea's case sends a message that there is a chance to overcome the devastation of pandemics without severely impacting the economy. It requires universal healthcare, intense and comprehensive surveillance, and trust in the government. Currently, very few countries match these criteria.
Ethical approval
This study did not require ethical approval as the analysis was based on publicly available data.
Conflict of interest
The authors declare no conflicts of interest.
Author contributions
S.K. was responsible for the study design, data collection, analysis, and interpretation, and production of the manuscript. M.C.C. was responsible for the overall supervision of the study, data analysis and interpretation, and production of the manuscript. Both authors contributed to the revision of the manuscript.
References
- Anselin L., Syabri I., Kho Y., GeoDa: An introduction to spatial data analysis. Geogr Anal. 2006;38(1):5–22. [Google Scholar]
- Argente D.O., Hsieh C.-T., Lee M. National Bureau of Economic Research; 2020. The cost of privacy: welfare effect of the disclosure of COVID-19 cases [Internet] (Working Paper Series). Report No.: 27220. Available from: http://www.nber.org/papers/w27220. [Google Scholar]
- Besag J., Diggle P.J. Simple Monte Carlo tests for spatial pattern. J R Stat Soc Ser C. 1977;26(3):327–333. [Google Scholar]
- Chinazzi M., Davis J.T., Ajelli M., Gioannini C., Litvinova M., Merler S. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(April (6489)):395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi S., Ki M. Estimating the reproductive number and the outbreak size of COVID-19 in Korea. Epidemiol Health [Internet] 2020;(March):42. doi: 10.4178/epih.e2020011. Available from: http://www.parasitol.or.kr/journal/view.php?number=1078 [cited 05.06.20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies N.G., Kucharski A.J., Eggo R.M., Gimma A., Edmunds W.J., Jombart T. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health [Internet] 2020;(June) doi: 10.1016/S2468-2667(20)30133-X. Available from: http://www.sciencedirect.com/science/article/pii/S246826672030133X [cited 10.06.20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- DS4C . 2020. COVID-19 dataset in South Korea [Internet] Available from: https://kaggle.com/kimjihoo/coronavirusdataset [cited 01.06.20]. [Dataset] [Google Scholar]
- Dwass M. Modified randomization tests for nonparametric hypotheses. Ann Math Stat. 1957;28(March (1)):181–187. [Google Scholar]
- ESRI, Inc . 2018. Esri support ArcMap 10.6 (10.6.1) [Internet] Available from: https://support.esri.com/en/products/desktop/arcgis-desktop/arcmap/10-6-1 [cited 01.06.20] [Google Scholar]
- International Monetary Fund . IMF; 2020. World economic outlook, April 2020: the great lockdown [Internet] Available from: https://www.imf.org/en/Publications/WEO/Issues/2020/04/14/weo-april-2020 [cited 08.06.20] [Google Scholar]
- KCDC division of COVID-19 National Emergency Response Center Contact transmission of COVID-19 in South Korea: novel investigation techniques for tracing contacts. Osong Public Health Res Perspect. 2020;11(February (1)):60–63. doi: 10.24171/j.phrp.2020.11.1.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korea Centers for Disease Control and Prevention . KCDC; 2020. The updates on COVID-19 in Korea as of 31 May [Internet] Available from: http://www.cdc.go.kr [cited 31.05.20] [Google Scholar]
- Korea Legislation Research Institute . 2019. Infectious disease control and prevention act [Internet] Available from: https://elaw.klri.re.kr/eng_mobile/ganadaDetail.do?hseq=50700&type=abc&key=INFECTIOUS%20DISEASE%20CONTROL%20AND%20PREVENTION%20ACT¶m=I [cited 03.06.20] [Google Scholar]
- Korean Society of Infectious Diseases, Korean Society of Pediatric Infectious Diseases, Korean Society of Epidemiology, Korean Society for Antimicrobial Therapy, Korean Society for Healthcare-associated Infection Control and Prevention, Korea Centers for Disease Control and Prevention Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci [Internet] 2020;35(March (10)) doi: 10.3346/jkms.2020.35.e112. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7073313/ [cited 05.06.20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulldorff and Information Management Services, Inc . 2018. SaTScan version 9.6: software for the spatial, temporal, and space-time scan statistics [Internet] Available from: https://www.satscan.org/ [cited 01.06.20] [Google Scholar]
- Kulldorff M. A spatial scan statistic. Commun Stat – Theory Methods. 1997;26(6):1481–1496. [Google Scholar]
- Kulldorff M., Athas W.F., Feurer E.J., Miller B.A., Key C.R. Evaluating cluster alarms: a space-time scan statistic and brain cancer in Los Alamos, New Mexico. Am J Public Health. 1998;88(September (9)):1377–1380. doi: 10.2105/ajph.88.9.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulldorff M., Nagarwalla N. Spatial disease clusters: detection and inference. Stat Med. 1995;14(April (8)):799–810. doi: 10.1002/sim.4780140809. [DOI] [PubMed] [Google Scholar]
- Linton S.L., Jennings J.M., Latkin C.A., Gomez M.B., Mehta S.H. Application of space-time scan statistics to describe geographic and temporal clustering of visible drug activity. J Urban Health Bull N Y Acad Med. 2014;91(October (5)):940–956. doi: 10.1007/s11524-014-9890-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19 – studies needed. N Engl J Med. 2020;382(March (13)):1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- Lloyd-Smith J.O., Schreiber S.J., Kopp P.E., Getz W.M. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438(November (7066)):355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Normile D. Coronavirus cases have dropped sharply in South Korea. What’s the secret to its success? [Internet] Science AAAS. 2020 Available from: https://www.sciencemag.org/news/2020/03/coronavirus-cases-have-dropped-sharply-south-korea-whats-secret-its-success [cited 08.06.20] [Google Scholar]
- Oh M., Park W.B., Park S.-W., Choe P.G., Bang J.H., Song K.-H. Middle East respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea. Korean J Intern Med. 2018;33(March (2)):233–246. doi: 10.3904/kjim.2018.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seoul Metropolitan Government . 2020. COVID-19 cases by district in Seoul city [Internet] Available from: https://www.seoul.go.kr/coronaV/coronaStatus.do [cited 31.05.20] [Google Scholar]
- Statistics Korea . 2020. Population by district and shapefiles of South Korea [Internet] Available from: http://kostat.go.kr/portal/eng/index.action [cited 01.06.20] [Google Scholar]
- World Health Organization . WHO. World Health Organization; 2017. Strengthening health systems for universal health coverage and sustainable development [Internet] Available from: http://www.who.int/bulletin/volumes/95/7/16-187476/en/ [cited 08.06.20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . WHO. World Health Organization; 2020. Coronavirus disease 19 (COVID-19) first report: pneumonia of unknown cause-China [Internet] Available from: http://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ [cited 15.04.20] [Google Scholar]
- World Health Organization . 2020. Coronavirus disease 19 (COVID-19): situation report – 132 [Internet] Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [cited 01.06.20] [Google Scholar]
- World Health Organization . 2020. WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020 [Internet] Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [cited 15.04.20] [Google Scholar]
- Yonhap News S. Korea to conduct coronavirus antibody tests in late May [Internet] Yonhap News Agency. 2020 Available from: https://en.yna.co.kr/view/AEN20200510003700320 [cited 09.06.20] [Google Scholar]