Abstract
Purpose:
The purpose of this study was to evaluate the safety and efficacy of mechanical thrombectomy with a direct aspiration first-pass technique (ADAPT) using large-bore catheters in patients with acute ischemic stroke due to large vessel occlusion (LVO) in a hospital in Vietnam.
Methods:
This was a retrospective review of patients with acute ischemic stroke due to LVO who were diagnosed and underwent mechanical thrombectomy using ADAPT with large-bore catheters at Bach Mai Hospital from January 2017 to June 2018.
Results:
Seventy-three patients (47.9% female; age: 61.29 ± 14.49 years) met study criteria. The average procedure duration was 45.09 ± 38.26 min. Successful recanalization post-ADAPT (thrombolysis in cerebral infarction 2b-3) was achieved in 72.6% (53/73) of patients. Good functional outcome (Modified Rankin Scale 0–2) at 3 months was achieved in 50.7% (37/73), with poor functional outcome in 24.7% (18/73). The 90-day mortality rate was 24.7% (18/73). The hemorrhagic transformation rate was 31.6%, in which 19.2% were symptomatic. Vessel perforation occurred in 5.5% (4/73) of patients but in all cases was associated with the guidewire and not the reperfusion catheter. Vessel dissection occurred in 1.4% (1/73) and vasospasm in 5.5% (4/73) of patients.
Conclusion:
Mechanical thrombectomy using ADAPT with large-bore catheters for acute ischemic stroke due to LVO is a method that yielded good results in recanalization and clinical recovery in a Vietnamese patient population.
Keywords: Acute ischemic stroke, Bach Mai Hospital, mechanical thrombectomy, thrombosis
Introduction
Acute ischemic stroke is a leading cause of death worldwide.[1] Risk factors for acute ischemic stroke include history of diabetes, heart disease, hypertension, or dyslipidemia.[1] In Vietnam with increasing living standards and life expectancy, accompanied by the increase in cardiovascular disease and diabetes, the risk of stroke is increasing. The goal of treating ischemic stroke is to recanalize blood flow to ischemic areas as soon as possible.
Currently, there are two main methods that are being implemented in many health-care facilities throughout Vietnam: intravenous fibrinolytic therapy and intravascular mechanical thrombectomy. However, only about 3%–10% of patients with acute ischemic stroke are treated with intravenous fibrinolysis due to out-of-treatment window or contraindications.[2] Given the limitations of intravenous fibrinolysis, mechanical thrombectomy is a useful alternative with a wider treatment window and high rates of successful recanalization.
At Bach Mai Hospital, the technique of mechanical thrombectomy using stent retrievers was introduced in May 2012, and aspiration thrombectomy using the Penumbra System (Penumbra, Inc.) was introduced in 2015. While the safety and efficacy of mechanical thrombectomy using stent retrievers and aspiration with large-bore catheters has been demonstrated in several recent studies in North America and Europe (e.g., Schramm et al., Turk et al., and Lapergue et al.[3,4,5]), there are few studies reporting the safety and efficacy of aspiration thrombectomy in Asian populations[6,7,8,9] and limited data using larger bore aspiration catheters. Therefore, we conducted this study to evaluate outcomes of mechanical thrombectomy using a direct aspiration first-pass technique (ADAPT) with large-bore aspiration catheters in cases of acute ischemic stroke due to large vessel occlusion (LVO) in a Vietnamese hospital setting.
Methods
Study design
This study is a retrospective review of patients with acute ischemic stroke undergoing aspiration thrombectomy at Bach Mai Hospital from January 2017 to June 2018.
Participants
Inclusion criteria were patients with acute LVO identified by digital subtraction angiography (DSA) and patients undergoing aspiration thrombectomy using the Penumbra System within 24 h of clinical symptom onset. Exclusion criteria included patients treated with stent retrievers.
Clinical information was collected by an emergency physician. Preoperative diagnosis based on multislice computed tomography (CT) or magnetic resonance imaging (MRI) diffusion-weighted imaging (DWI), time-of-flight (TOF) angiography, and fluid-attenuated inversion recovery (FLAIR) was used for the determination of LVO and parenchymal injury assessment (based on the Alberta Stroke Program Early CT Score [ASPECTS] or posterior circulation ASPECTS). Intravenous fibrinolysis was given if the patient arrived within 4.5 h of symptom onset, the injured region was small, and the patient had no contraindications. During the course of mechanical thrombectomy, the patient was awake or given endotracheal intubation depending on the clinical condition, and blood oxygen and blood pressure were strictly controlled. Noncontrast MRI or CT scanner was performed at 24 h postprocedure to exclude bleeding and to decide on the next anticoagulant therapy.
An indication of mechanical thrombectomy in LVO associated with severe localized neurological symptoms was determined by the National Institutes of Health Stroke Scale (NIHSS) score (>6 points) and previous Modified Rankin Scale (mRS) score (≤2). At our institution, ADAPT was considered for patients without severe stenosis, more proximal LVO location (e.g., M1 segment, T-internal carotid artery [ICA], and basilar artery trunk), and lack of severe tortuosity. We followed the American Heart Association/American Stroke Association 2018 guidelines for late window (>6 h) LVO, in which thrombectomy is indicated for reasonable patients based on the DAWN and DEFUSE-3 criteria.[10] Contraindications included bleeding or evidence of cerebral infarction on CT scanner/MRI, symptom onset >24 h, or end-stage diseases.
Relatives of patients explained the procedure and provided written consent to participate in treatment. The study was approved by the ethics committee.
Clinical data
Clinical information was collected at admission, including age, sex, medical history of stroke, and NIHSS score. Clinical outcome (mRS) and mortality after 3 months (90 days) were collected from medical records or direct contact with the patients. Good clinical outcome was defined as mRS ≤2.
Intervention data
Intervention data including the use of combination therapy, duration of treatment (time from symptom onset to femoral artery accession), duration of intervention (time from femoral artery access to recanalization), devices used in each case (ACE 64 or ACE 68), and complications postintervention were obtained.
All procedures were performed under a DSA monoplane (Philips Allura Xper FD20). Procedures were performed with an 8F guide catheter with or without an intermediate catheter. For aspiration, ACE 64 or ACE 68 reperfusion catheters were advanced to the blood clot with the help of a microcatheter (Rebar 2.7F) and microguidewire (Transcend 0.014”). When an intracranial stent was required, antiplatelet therapy is used in the acute phase. If an intracranial stent was placed and there was no hemorrhagic complication on the study imaging, patients were started on dual antiplatelet therapy with aspirin 81 mg/day and clopidogrel 75 mg/day for 3 months and aspirin 81 mg/day for life.
Imaging data
Recanalization status was evaluated by a neuroradiologist using thrombolysis in cerebral infarction (TICI) score based on DSA. Successful recanalization was defined as modified TICI 2b-3.
Intracranial hemorrhage (ICH) was classified according to clinical criteria and noncontrast CT. Symptomatic ICH was determined by noncontrast CT with symptomatic defined by having symptom headache, deterioration in neurological status (NIHSS score), or mass effect on brain tissue outside the infarct. Complications related to the procedure including perforation of the arteries, defined as extravasation of the contrast material during intervention, vessel dissection, and vasospasms, were recorded.
Statistical analysis
Data were analyzed using standard descriptive statistics, including the number of observations, mean, median, standard deviation, minimum and maximum for continuous variables, and counts and percentages for discrete variables.
Results
During the study period (from January 2017 to June 2018), the records of 86 patients with acute LVO and treated with thrombectomy intervention using ADAPT were obtained, and 73 patients (35 females) met study criteria. Thirteen patients were excluded due to the use of stent retrievers during the procedure. Baseline and procedure characteristics are reported in Table 1. The mean age was 61.29 ± 14.49 years (range: 33–89). Patients showed marked neurological deficits with an average NIHSS score of 17.1 ± 5.3. Of these, 32.9% had a history of hypertension, 19.2% had a history of cerebrovascular disease, and 49.3% had atrial fibrillation at admission. Most of the patients with atrial fibrillation were not on anticoagulants leading to embolic stroke.
Table 1.
Baseline and procedure characteristics (n=73)
| Variable | All patients |
|---|---|
| Age (years), mean±SD | 61.29±14.49 |
| Female, percentage (n/N) | 47.9 (35/73) |
| NIHSS score, mean±SD | 17.1±5.3 |
| History of hypertension, percentage (n/N) | 32.9 (24/73) |
| History of cerebrovascular disease, percentage (n/N) | 19.2 (14/73) |
| Atrial fibrillation, percentage (n/N) | 49.3 (36/73) |
| Intravenous fibrinolysis (tPA), percentage (n/N) | 28.8 (21/73) |
| Site of LVO, percentage (n/N) | |
| Anterior circulation | |
| Internal carotid artery | 45.2 (33/73) |
| Middle cerebral artery | 38.4 (28/73) |
| Posterior circulation | |
| Basilar artery | 13.7 (10/73) |
| Posterior cerebral artery | 2.7 (2/73) |
| Time from onset to admission (min), mean±SD | 118.14±84.96 |
| Time from admission to puncture (min), mean±SD | 88.49±40.33 |
| Time from onset to recanalization (min), mean±SD | 251.68±104.70 |
| Procedure duration (min), mean±SD | 45.09±38.26 |
SD – Standard deviation; NIHSS – National Institutes of Health Stroke Scale; tPA – Tissue plasminogen activator; LVO – Large vessel occlusion
The site of LVO was predominantly in the anterior circulation (82.6% of cases), with ICA occlusion in 45.2% of cases, and middle cerebral artery occlusion in 37.4% of cases.
The mean time from onset to admission was 118.14 ± 84.96 min. The mean intervention duration was 45.57 ± 38.23 min, and the shortest procedure was 5 min with success after the first-pass aspiration. Recanalization (TICI 2b-3) post-ADAPT was achieved in 72.6% of cases [Table 2].
Table 2.
Recanalization after intervention
| Level of recanalization based on TICI | Percentage (n/N) |
|---|---|
| Poor | |
| 0 | 12.3 (9/73) |
| 1 | 2.7 (2/73) |
| 2a | 12.3 (9/73) |
| Favorable | |
| 2b | 31.5 (23/73) |
| 3 | 41.1 (30/73) |
TICI – Thrombolysis in cerebral infarction
Complications are reported in Table 3. The hemorrhagic transformation rate was 31.6%, in which 19.2% were symptomatic (three cases did not have MRI performed after intervention due to severe status). Vessel perforation occurred in 5.5% (4/73) of patients but in all cases was associated with the guidewire and not the reperfusion catheter. Vessel dissection occurred in 1.4% (1/73) and vasospasm in 5.5% (4/73) of patients.
Table 3.
Complications
| Type of complication | Percentage (n/N) |
|---|---|
| Hemorrhage | |
| Asymptomatic ICH | 12.3 (9/73) |
| Symptomatic ICH | 19.2 (14/73) |
| Vessel perforation | 5.5 (4/73) |
| Vessel dissection | 1.4 (1/73) |
| Vasospasm | 5.5 (4/73) |
ICH – Intracranial hemorrhage
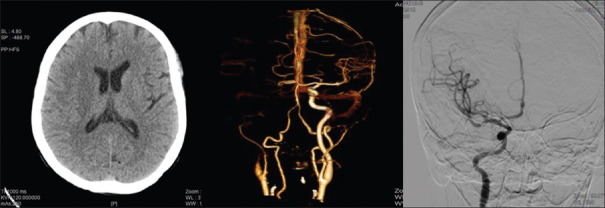
At 3 months after intervention, the rate of patients with good clinical outcome (mRS 0–2) was 51% [Table 4]. The 90-day mortality rate was 24.7%. An illustrated case is presented in Figure 1.
Table 4.
Clinical outcome after 3 months
| Clinical outcome | Percentage (n/N) |
|---|---|
| Good clinical outcome (mRS 0-2) | 50.7 (37/73) |
| Poor outcome (mRS 3-5) | 24.7 (18/73) |
| Death (mRS 6) | 24.7 (18/73) |
mRS – Modified Rankin Scale
Figure 1.
The patient presented within 4 h of symptom onset. Images include: Right internal carotid occlusion (center) and good recanalization (TICI 3) after the intervention (right)
Discussion
This study is one of the first to report the use of large-bore catheters for aspiration thrombectomy in a Vietnamese patient population. The results demonstrate the safety and efficacy of aspiration thrombectomy with ACE 64 and ACE 68 aspiration catheters using the Penumbra System in a Vietnamese hospital setting. In our study, the recanalization rate (TICI 2b-3) after aspiration thrombectomy was 72.6%, and the rate of good clinical outcome (mRS 0-2) at 3 months was 50.7%. The 90-day mortality was 24.7%.
The rate of good clinical outcome at 90 days in the current study (50.7%) is comparable to aspiration thrombectomy studies from North America and Europe (COMPASS,[4] ASTER,[5] Penumbra Separator 3D trial,[11] and COMPLETE[3]) and to two retrospective review studies in Japanese populations using aspiration thrombectomy;[8,9] however, the rate is higher than for two mechanical thrombectomy studies from China.[6,7] In the ACTUAL study, a retrospective stroke registry of endovascular therapies (mechanical thrombectomy, thromboaspiration, balloon dilation, stenting, intra-arterial thrombolysis, or various combinations of these approaches) conducted at 21 stroke centers across 10 provinces in China, good clinical outcome was achieved in 43.6% (304/698).[6] In a retrospective analysis of 68 patients with acute basilar artery occlusion treated with stent retrievers or ADAPT (n = 7), good clinical outcome (mRS 0–2) was reported in 45.6%.[7]
The successful recanalization rate in the current study (72.6%) is comparable to findings in historical studies of endovascular therapies in North America and Europe, such as ESCAPE (72.4%),[12] THERAPY (70%),[13] and MR CLEAN (58.7%)[14], and close to the reperfusion rate from the ACTUAL study in China (83%).[6,8] However, the rate is lower when compared to reperfusion rates for aspiration thrombectomy in PROMISE (93.1%),[3] ASTER (85.4%),[5] COMPASS (92%),[4] and two retrospective review studies in Japanese populations (86.3%[8] and 88%[9]). Varying inclusion/exclusion criteria or patient characteristics may account for the differences in reperfusion rates between studies, such as the inclusion of patients with posterior circulation occlusions and exclusion of patients treated with stent retrievers as rescue therapy.
For safety outcomes, the 90-day mortality rate of 24.7% in the current study is in line with previous aspiration thrombectomy trials in North America,[4] Europe,[5] and Asia.[6] The rate of symptomatic ICH (19.2%) is higher than that of North American and European trials where symptomatic ICH rates range from 2.9% to 6%;[3,4,5,11] however, it is more consistent with symptomatic ICH rates of 15.5% and 11.8% reported in two mechanical thrombectomy studies in China.[6,7] This high rate of symptomatic ICH is likely due to the different definitions of symptomatic ICH used in the current study, where patients with any symptoms were included, as compared to other studies that have defined symptomatic ICH based on a four-point or greater deterioration in the NIHSS within 24 h.[3,4,5,11] When using the definition NIHSS worsening four points or more, the symptomatic ICH rate in our study was 10.9% (8/73). The higher rate may also be partially explained by the fact that in our study, the predominant artery occlusion prevalence was the ICA which has the highest chance of bleeding.[15,16] Vessel perforation occurred in 5.5% (4/73) of patients, which is higher than other studies; however, all cases were associated with the guidewire and not the reperfusion catheter. Rates of vessel dissection and vasospasm are in line with published literature.
The findings are limited by the use of retrospective data, single-center study design, and lack of a control arm. Furthermore, we excluded patients who were treated with stent retrievers, which may limit the direct comparison with other studies. The major strengths of this study included the collection of data from real-world clinical practice by experienced interventionalists. The results of this study may be useful for guiding future multicenter prospective trials of mechanical thrombectomy in the Asian population. Finally, to date, this is the only study to our knowledge to report the safety and efficacy of aspiration thrombectomy in a Vietnamese patient population.
Conclusion
The findings suggest that aspiration thrombectomy in cases of LVO using large-bore catheters is a method that yields good results in recanalization and clinical recovery in a Vietnamese population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful to Amy Ross PhD, Vincent Ho MD, and Tatiana Ermakova MD MPH (Penumbra, Inc.) for their assistance during manuscript preparation.
References
- 1.Katan M, Luft A. Global burden of stroke. Semin Neurol. 2018;38:208–11. doi: 10.1055/s-0038-1649503. [DOI] [PubMed] [Google Scholar]
- 2.Naidech A. Hemorrhagic and Ischemic Stroke: Medical, Imaging, Surgical and Interventional Approaches. New York: Thieme; 2011. [Google Scholar]
- 3.Schramm P, Navia P, Papa R, Zamarro J, Tomasello A, Weber W, et al. ADAPT technique with ACE68 and ACE64 reperfusion catheters in ischemic stroke treatment: Results from the PROMISE study. J Neurointerv Surg. 2019;11:226–31. doi: 10.1136/neurintsurg-2018-014122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turk AS, 3rd, Siddiqui A, Fifi JT, De Leacy RA, Fiorella DJ, Gu E, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): A multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet. 2019;393:998–1008. doi: 10.1016/S0140-6736(19)30297-1. [DOI] [PubMed] [Google Scholar]
- 5.Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: The ASTER randomized clinical trial. JAMA. 2017;318:443–52. doi: 10.1001/jama.2017.9644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zi W, Wang H, Yang D, Hao Y, Zhang M, Geng Y, et al. Clinical effectiveness and safety outcomes of endovascular treatment for acute anterior circulation ischemic stroke in China. Cerebrovasc Dis. 2017;44:248–58. doi: 10.1159/000478667. [DOI] [PubMed] [Google Scholar]
- 7.Li C, Zhao W, Wu C, Shang S, Chen J, Ren M, et al. Outcome of endovascular treatment for acute basilar artery occlusion in the modern era: A single institution experience. Neuroradiology. 2018;60:651–9. doi: 10.1007/s00234-018-2011-7. [DOI] [PubMed] [Google Scholar]
- 8.Uno J, Kameda K, Otsuji R, Ren N, Nagaoka S, Maeda K, et al. A Direct Aspiration First Pass Technique in Japanese real-world clinical setting. Oper Neurosurg (Hagerstown) 2019;17:115–22. doi: 10.1093/ons/opy349. [DOI] [PubMed] [Google Scholar]
- 9.Matsumoto H, Nishiyama H, Tetsuo Y, Takemoto H, Nakao N. Initial clinical experience using the two-stage aspiration technique (TSAT) with proximal flow arrest by a balloon guiding catheter for acute ischemic stroke of the anterior circulation. J Neurointerv Surg. 2017;9:1160–5. doi: 10.1136/neurintsurg-2016-012787. [DOI] [PubMed] [Google Scholar]
- 10.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–110. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 11.Nogueira RG, Frei D, Kirmani JF, Zaidat O, Lopes D, Turk AS, 3rd, et al. Safety and efficacy of a 3-dimensional stent retriever with aspiration-based thrombectomy vs aspiration-based thrombectomy alone in acute ischemic stroke intervention: A Randomized Clinical Trial. JAMA Neurol. 2018;75:304–11. doi: 10.1001/jamaneurol.2017.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 13.Mocco J, Zaidat OO, von Kummer R, Yoo AJ, Gupta R, Lopes D, et al. Aspiration thrombectomy after intravenous alteplase versus intravenous alteplase alone. Stroke. 2016;47:2331–8. doi: 10.1161/STROKEAHA.116.013372. [DOI] [PubMed] [Google Scholar]
- 14.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 15.Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical thrombectomy for acute ischemic stroke: Final results of the multi MERCI trial. Stroke. 2008;39:1205–12. doi: 10.1161/STROKEAHA.107.497115. [DOI] [PubMed] [Google Scholar]
- 16.Penumbra Pivotal Stroke Trial Investigators. The penumbra pivotal stroke trial: Safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40:2761–8. doi: 10.1161/STROKEAHA.108.544957. [DOI] [PubMed] [Google Scholar]