Abstract
Background
Irish health services have been repurposed in response to the COVID-19 pandemic. Critical care services have been re-focused on the management of COVID-19 patients. This presents a major challenge for specialities such as cardiothoracic surgery that are reliant on intensive care unit (ICU) resources.
Aim
The aim of this study was to evaluate the impact of the COVID-19 pandemic on activity at the cardiothoracic surgical care at the National Cardiothoracic Surgery and Transplant Centre.
Methods
A comparison was performed of cardiac surgery and transplant caseload for the first 4 months of 2019 and 2020 using data collected prospectively on a customised digital database.
Results
Cardiac surgery activity fell over the study period but was most impacted in March and April 2020. Operative activity fell to 49% of the previous years’ activity for March and April 2020. Surgical acuity changed with 61% of all cases performed as inpatient transfers after cardiology admission in contrast with a 40% rate in 2019. Valve surgery continued at 89% of the expected rate; coronary artery bypass surgery was performed at 61% of the expected rate and major aortic surgery at 22%. Adult congenital heart cases were not performed in March or April 2020. One heart and one lung transplant were performed in this period.
Conclusions
In March and April of 2020, the spread of COVID-19 and the resultant focus on its management resulted in a reduction in cardiothoracic surgery service delivery.
Keywords: Cardiac surgery, Coronavirus, COVID-19, Pandemic, Transplant
Background
The COVID-19 pandemic included Ireland from March 1, 2020. The state’s health services were re-tooled to address this with dramatic changes in resource allocation and utilisation. Cardiac surgery and heart and lung transplant services were particularly challenged. There were three considerations: intensive care availability; patient COVID-19 exposure and the impact of that on the risk of concurrent major surgery; and patient willingness to attend hospital for surgery. In the transplant domain, there were also three challenges: the confirmation of a safe donor, the vulnerability of the immunocompromised recipient and intensive care unit (ICU) resource utilisation. The objective of this paper was to analyse activity patterns at the National Centre for Cardiothoracic Surgery and Transplantation and to discuss the impact of this change on the provision of cardiac and transplant surgical care going forward.
Methods
Data regarding cardiothoracic operative activity in the Mater Misericordiae University Hospital is collected prospectively on a standardised cardiothoracic digital database: Patient Advocate Tracking System (PATS). A retrospective review of that prospectively collected data was performed for the first 4 months of the years 2019 and 2020. The number and nature of all cases, as well as patient demographic and profile data, were reviewed. All cases were referred through the public sector. However, some of the surgery took place in private institutions as per the agreement between the state and the private hospitals as part of the pandemic emergency response. The relative reduction in 2020 was expressed as a percentage of the caseload in 2019. This study was approved by the institutional review board (Ref. Code: 1/378/2149 TMR).
Results
The number of major cardiac surgery procedures performed in the first 4 months of 2020 was 136 cases. The same time point achieved in 2019 had 180 major cases. In 2020, only 75% of the expected case activity was achieved. The first 2 months were on trend with 2019, with most of the change occurring in March and April (Fig. 1). Looking at March and April in particular: in 2019, 95 cases were performed in contrast with only 47 in 2020. If that overall trend continues, instead of performing an expected 540 major cardiac cases in 2020, the service will deliver only 324 major cardiac cases or 60% of the expected total. The waiting list currently is already 197 cases.
Fig. 1.
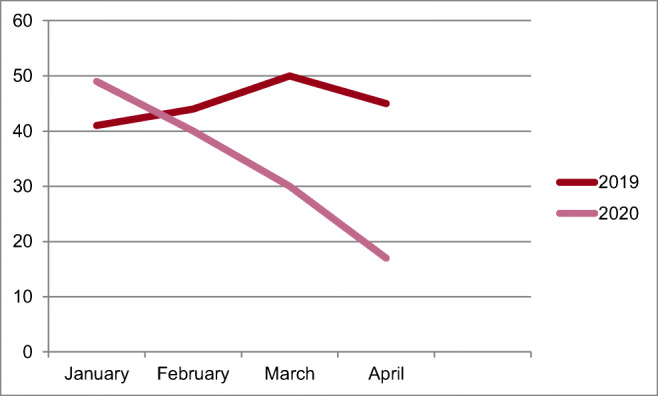
Total cardiac and transplant cases performed January to May 2019 and 2020
Procedures classed as urgent were the most commonly performed priority class (defined as surgery performed during admission for acute event such as a non-ST elevation myocardial infarction). In 2020, 54.5% of cases were classed as urgent, in contrast with 44% in 2019. Looking more closely at March and April, 61% of 2020 cases were urgent, in contrast with 40% in the period in 2019. Elective cases did not stop completely as elective cardiac cases are still time sensitive, but they represented only 21% of activity in 2020 in comparison with 43% in 2019. Although transplant activity had reduced significantly, the relative proportion of transplant activity remained at 10% throughout the study period for both 2019 and 2020, including March and April 2019 and 2020.
In the initial management stages, it was suggested that alternative options be explored for patients with an anticipated long ICU postoperative stay in particular. On that basis, we assessed the patient profile, but we observed no notable difference in patient profile between 2019 and 2020. From January to April 2019, the median age was 62.5 years (17–90) compared with 65.5 (18–82) for 2020. Focusing on March and April, the median age in 2019 was 62.5 years (22–90) against 66 years (22–82) in 2020.
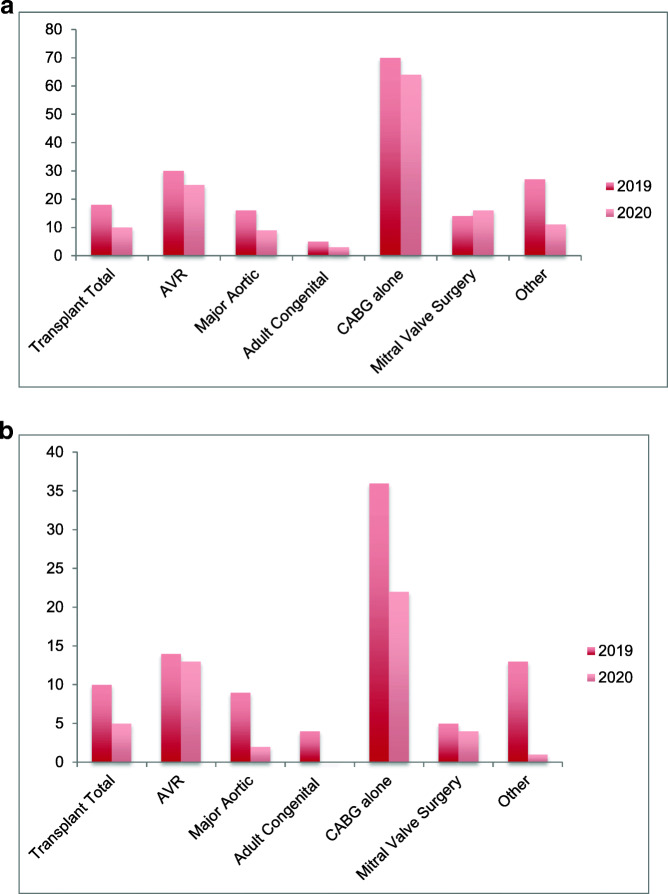
We wanted to determine if there was a change in the pattern of practise, as well as volume, and analyse the cases based on type.
Valve surgeries (left-sided)
A surgery for left-sided valvular heart disease, including aortic valve replacements and mitral valve replacement or repair (with or without concomitant coronary artery bypass grafting (CABG)), was not as dramatically affected as other procedures. A 6% reduction (44 vs. 41 cases) was seen in the 4-month period. Focusing on March and April 2020, surgery continued at 90% rate of expected cases (17 vs. 19).
Coronary bypass surgery
Looking at coronary artery bypass surgery alone, we noted a 9% reduction in the number of CABG cases performed between 2019 and 2020 (70 vs. 64). However again, the drop-off is focused on the 2 months of March and April. In this time window of 2020, activity continued at 61% expected activity (36 vs. 22) (Fig. 2a and 2b).
Fig. 2.
a Comparison of breakdown of cases in January to May 2019 and 2020. b Comparison of breakdown of cases in March and April 2019 versus 2020
Major aortic surgery
Major aortic surgery, such as aortic root, ascending aortic or arch replacement, was seen to have an overall decrease in numbers by 44% (16 vs. 9). Focusing on the period of March and April 2020, activity continued at 22% of the expected rate (9 vs. 2).
Adult congenital heart surgery
The case numbers of adult congenital operations had initially increased in January and February between 2019 and 2020 (1 vs. 3). However, three cases were performed in March and April of 2019, whereas no congenital procedures took place in the same months of 2020 (Fig. 2a and 2b).
Heart and lung transplantation
The study included cases of heart transplant, lung transplant and primary ventricular assist device (VAD) and observed a 28% reduction overall and a 50% reduction since the onset of the pandemic (Fig. 2b).
Others
Other procedures included epicardial permanent pacemaker placement, central cannulation for extracorporeal membrane oxygenation (ECMO), myxoma excision, emergency sternotomy for cardiac trauma and myomectomy. The incidence of such cases had reduced by 92% since the pandemic restrictions were put in place, with 13 cases performed in March and April 2019 while only one of these cases was performed in 2020.
Of the 47 cases completed in the March and April 2020 period, 32 cases were performed on-site at the Mater Misericordiae University Hospital, while 15 were performed at outsourced locations. One of these cases would prove to be COVID-19 swab positive. This was associated with a prolonged ICU stay, and their care continues at the time of writing.
Discussion
The COVID-19 pandemic has challenged the nation’s health service. It has proven adaptable and flexible and has radically altered its profile and resource allocation. In the context of the needs of the time, major cardiac surgery dropped in priority. This was driven by the three factors: the need to re-distribute heath service resources in the emergency, the need to balance risk of delayed surgery with perioperative COVID-19 infection and the altered pattern of emergency department presentation and outpatient investigations.
The findings of this review demonstrate a significant drop in major cardiac surgery procedures. There was a 50% reduction in cardiac and transplant surgery for March and April 2020. This occurred despite the utilisation of the private capacity contracted by the state in the emergency. These findings are consistent internationally with those observed by Salenger et al. [1], who saw a 54% decrease in cardiac surgical volumes once restrictions were implemented. The study used mathematical modelling to estimate a future delay of up to 8 months due to backlog of cases. Although this study discusses a different healthcare system, there will inevitably be a backlog for Irish patients, and there are a number of patients on the elective waiting list for surgery within this speciality for whom this delay may be critical.
We know from previously published data that the mortality on the Irish heart transplant waiting list is 24% for every 6 months on the list [2]. Equally, patients listed for lung transplant often have an estimated survival of 2 years without transplant [3]. The mortality risk for more general cases on a waiting list is also real. There is a pattern in the profile of the delayed patients. The service was able to protect CABG surgery and valve surgery to some extent. There was a significant reduction in the numbers of major aortic cases performed, which was mainly due to the drop-off in elective aortic cases for patients with aortic aneurysms, as opposed to emergency procedures for dissection. The potential for backlog of cases in the current climate presents a serious threat to patients with aortic diameters > 6 cm, who have an estimated rate of death, risk or rupture of approximately 15% per year [4]. However, other groups such as adult congenital cases and transplant recipients would seem to have had their opportunity delayed.
One review from the Netherlands [5] on the impact of COVID-19 on transplant services considered that a reduction in potential donation offers was likely due to a reduction in road traffic accidents as more people worked from home. At the time of writing, the Irish police force (Gardaí) had reported an increase in both total collisions and case fatalities in 2020 when compared with those in 2019, including 25 fatalities in March and April 2020 as opposed to 20 in the same months of 2019 [6]. However, an ICU focusing on addressing this new pandemic may not be in a position to focus on the donation process. The moratorium on visitors may also compromise the quality of the interaction between family and the ICU team. Strict criteria were also developed to protect the recipient that mandated tight and secure clearance of COVID-19 possibilities regarding a donor. This may have excluded a number of potential donors. Although initial case report data suggested acceptable outcomes of COVID-19 for solid organ transplant recipients [7, 8], larger scale observational data suggests seriously raised morbidity and mortality in patients with heart transplants and COVID-19 [9]. One consideration for patients awaiting heart transplant may be a temporising ventricular assist device (VAD), which avoids immunosuppression, while taking into account the support and care these patients require in the community and the capacity to provide this amidst the pandemic. The small numbers of reported outcomes of lung transplant recipients post-COVID-19 infected is mixed [7, 10, 11].
There were no adult congenital operations performed in March or April of 2020. These patients may be younger and without chronic hypertension and diabetes and may be among the lowest risk cardiac surgery group, but there are currently no available studies with a focus on their COVID-19 outcomes [12].
At the time of writing this review, Ireland had the thirteenth highest number of cases in the European Union (EU), despite only ranking 19 in the EU in terms of population [13]. Despite this, the number of cases in Ireland has not surpassed the available ICU resources [14] and consequently, the Irish government has proposed phased reopening of the country from May 18, 2020 [15]. This presents a quandary for cardiothoracic services such as those provided in the Mater Hospital, where there is no dedicated separate cardiac ICU: what patients should be selected for cardiac surgery while the ICU continues to care for patients with the virus?
Cardiac surgery patients are of particular relevance when discussing the COVID-19 pandemic. They have high rates of hypertension and diabetes, two adverse risk factors for mortality with coronavirus infection [16]. They require mechanical ventilation in the hours to days after surgery, necessitating ICU level care. This means potentially more COVID-19 risk then cocooning at home. The risks therefore must be balanced between surgery delay and COVID-19 exposure, at a time of imperfect knowledge of the disease.
For the service reconstruction phase, the potential to screen patients for planned surgery needs to be optimised. Methods such as clinical history, nasopharyngeal swab testing and computed tomography of the thorax have been proposed. Ideally, the hospital would be either a COVID-19-free hospital with no emergency department. Another model is a single campus with two hospital divisions: a COVID-19 and non-COVID-19 division with minimal cross-over between the two. This presents challenges for ICU organisation as it implies the need to two ICUs where the Irish model was previously one single unit. Patients have become very afraid and also have declined dates of surgery offered to them. It is too early for us all to be very definitive regarding that, but patient confidence will have to be restored and patients will need demonstrable reassurance that their COVID-19 exposure is being minimised.
Conclusion
The results of this study highlight the opportunity cost of the COVID-19 pandemic response and highlight where some of the future challenges lie.
Compliance with ethical standards
Ethical approval
This study was conducted in line with principles of the Declaration of Helsinki approved by the institutional review board of the Mater Hospital (Ref. Code: 1/378/2149 TMR).
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Salenger R, Etchill E, Ad N et al (2020) The surge after the surge: cardiac surgery post-COVID-19. Ann Thorac Surg. 10.1016/j.athoracsur.2020.04.018 [DOI] [PMC free article] [PubMed]
- 2.Healy, et al. Heart transplant candidates: factors influencing waiting list mortality. IMJ. 2005;98:235. [PubMed] [Google Scholar]
- 3.Weill D. Lung transplantation: indications and contraindications. J Thorac Dis. 2018;10:4574–4587. doi: 10.21037/jtd.2018.06.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davies R, Goldstein L, Coady M, et al. Yearly rupture or dissection rates for thoracic aortic aneurysms: simple prediction based on size. Ann Thorac Surg. 2002;73:17–28. doi: 10.1016/s0003-4975(01)03236-2. [DOI] [PubMed] [Google Scholar]
- 5.de Vries A, Alwayn I, Hoek R, et al. Immediate impact of COVID-19 on transplant activity in the Netherlands. Transpl Immunol. 2020;61:101304. doi: 10.1016/j.trim.2020.101304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.(2020) Roads Policing fatalities to date for 2020. In: Garda. https://www.garda.ie/en/roads-policing/statistics/roads-policing-fatalities-to-date-for-2020/. Accessed 16 May 2020
- 7.Aigner C, Dittmer U, Kamler M, Collaud S, Taube C. COVID-19 in a lung transplant recipient. J Heart Lung Transplant. 2020;39:610–611. doi: 10.1016/j.healun.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li F, Cai J, Dong N. First cases of COVID-19 in heart transplantation from China. J Heart Lung Transplant. 2020;39:496–497. doi: 10.1016/j.healun.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Latif F, Farr M, Clerkin K et al (2020) Characteristics and outcomes of recipients of heart transplant with coronavirus disease 2019. JAMA Cardiol. 10.1001/jamacardio.2020.2159 [DOI] [PMC free article] [PubMed]
- 10.Koczulla R, Sczepanski B, Koteczki A et al (2020) SARS-CoV-2 infection in two patients following recent lung transplantation. Am J Transplant. 10.1111/ajt.15998 [DOI] [PMC free article] [PubMed]
- 11.Farfour E, Picard C, Beaumont L, Lesprit P, Ballester MC, Ackermann F, Galliot R, Colin de Verdiere S, Cerf C, Vasse M, Sars-Cov-2 Foch Hospital study group COVID-19 in lung-transplanted and cystic fibrosis patients: be careful. J Cyst Fibros. 2020;19:e16–e17. doi: 10.1016/j.jcf.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tan W, Aboulhosn J. The cardiovascular burden of coronavirus disease 2019 (COVID-19) with a focus on congenital heart disease. Int J Cardiol. 2020;309:70–77. doi: 10.1016/j.ijcard.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.(2020) Coronavirus Update (Live): 3,248,684 Cases and 229,399 Deaths from COVID-19 Virus Pandemic - Worldometer. In: Worldometers.info. https://www.worldometers.info/coronavirus/. Accessed 30 May 2020
- 14.(2020) Epidemiology of COVID-19 in Ireland - daily reports, April 2020. In: Health Protection Surveillance Centre. https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/. Accessed 30 Apr 2020
- 15.(2020) Gov.ie - Roadmap for reopening society and business. In: Gov.ie. https://www.gov.ie/en/news/58bc8b-taoiseach-announces-roadmap-for-reopening-society-and-business-and-u/. Accessed 12 May 2020
- 16.Wu C, Chen X, Cai Y, Xia J’, Zhou X, Xu S, Huang H, Zhang L, Zhou X, du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Int Med. 10.1001/jamainternmed.2020.0994 [DOI] [PMC free article] [PubMed]