Abstract
Purpose
To describe methods used to identify the timing of transfer from pediatric to adult care within health administrative data and to identify the advantages and limitations of each method to guide future research.
Study Design and Settings
We conducted a scoping review to identify studies, summarized challenges of identifying the timing of transfer, and proposed methodological approaches for each.
Results
Studies use the following approaches to capture individuals who transfer from pediatric to adult care by 1) defining the timing of transfer by the last pediatric and first adult care visit last and 2) defining transfer to adult care based on a specific age.
Conclusion
There are important limitations of administrative data that must be recognized in designing studies examining the transfer to adult care.
Keywords: transfer to adult care, administrative data, chronic disease
Introduction
Approximately 15% of youth have a chronic health condition that will ultimately require the transfer from pediatric to adult care.1 The ultimate goal of transition care is to provide healthcare that is coordinated, uninterrupted, and developmentally-appropriate and to promote skills in decision-making and self-care.2–5 However, patients with chronic health conditions and providers report inadequate support and services during the transition to adult care.6–9 Emerging adulthood (18–30 years) is a particularly challenging period for people living with a chronic health condition because of the change in type and characteristics of healthcare provision, decreased parental involvement, and the developmental changes emerging adults are undergoing including; emotional, physical, financial, occupational, and social changes within a short period of time.10,11 These combined challenges result in an increased risk of inadequate medical follow-up, poor self-management, emergency department visits and hospitalizations.12–15
Although the importance of transition care is well recognized, empiric data about transition outcomes remain limited. There continues to be a paucity of research on the magnitude of the problem, on factors that may mitigate the risk of complications around the transition period as well as a lack of intervention trials.16–19 It is important to establish rigorous methods to identify the time of transfer to adult care in order to: 1) understand patterns of healthcare visits to pediatric and adult care providers for transition-age youth (eg, delays in leaving pediatric care, time gaps between final pediatric and first adult visits, and continuity of care after transfer to adult care), and 2) examine the associations of patterns of care during transition-age and important health outcomes.
Health administrative data are powerful tools in health services research to efficiently assess disease burden, healthcare utilization and outcomes in adolescents with chronic illnesses, particularly around the high-risk transition period. Specifically, using administrative data for identifying the time of transfer and for assessing outcome measures such as emergency department visits and hospitalizations may be preferable to alternatives such as self-reports, which are burdensome, may not be feasible, and may have recall bias. Further, administrative data may be useful as a supplement to patient-reported experience and outcome measures that are focused on other aspects of transition. Finally, there are benefits to understanding these issues on a population-level.
However, identifying the timing of transfer from pediatric to adult care can be difficult within health administrative data. An accurate definition for identifying this transfer is essential in reducing the risk of misclassification bias. Recognizing that health systems and administrative data sources vary between settings, it is not possible to design a single definition to identify the time of transfer that is applicable to all contexts. However, there are likely a few general approaches that could be used to measure desired variables depending on local context. Developing standardized methods would increase the quality and reproducibility of data as well as the ability to meaningfully compare results across studies. As such, our aims are to 1) describe the methods used to identify the timing of transfer to adult care within administrative health data and 2) identify the challenges with these methods as well as propose methodological approaches to overcome the challenges.
Methods
We conducted a scoping review to identify studies that used administrative data to identify the time of transfer to adult care for young adults with a chronic health condition.20 We searched Embase (OVID) and Medline and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily (OVID) from the inception of the databases to August 22, 2019. The search included two broad concepts: 1) youth transferring to adult care, and 2) health administrative data. Search terms were identified through known articles on this topic, subject experts on the team, and a librarian with expertise in database searching. The search terms included combinations of controlled vocabulary specific to the databases (ie, EmTree or MeSH) and keyword terms searched in the title, abstract or author keyword fields. The search was limited only to English language articles. Search strategies are available in Appendix A. We included papers that 1) determined the time of transfer from pediatric to adult care, and 2) used administrative data; routinely collected data about health services use (eg, physician billing data and hospital and emergency department visits). All study designs were eligible and studies of any chronic condition requiring transfer to adult care were included.
Two reviewers (R.S. and M.N.) independently screened the search results, obtained the full-text of potentially eligible studies, and determined their eligibility. Discrepancies were resolved by discussion. We described each study and identified methodological approaches used by each to address specific challenges related to identification of the timing of transfer within administrative data.
Results
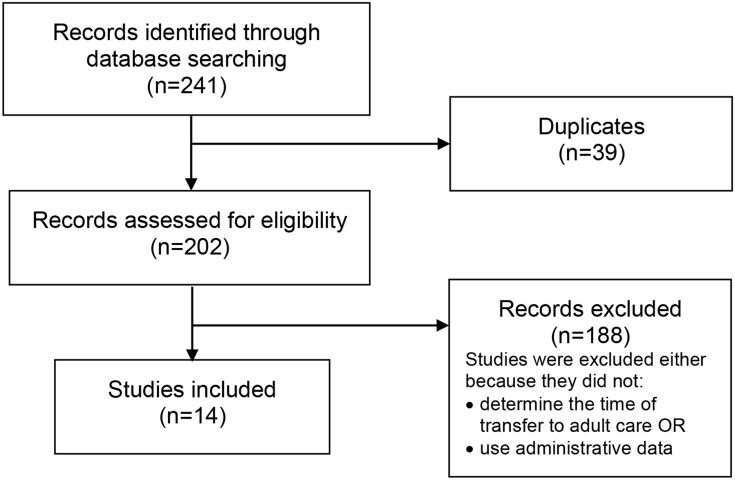
Among the 241 records identified through our database search, 14 studies were included (Figure 1). Table 1 describes the definitions used to identify the transfer to adult care using administrative health data. Five studies use a “transfer period” based on the date of last pediatric care visit and first adult care visit during which transfer to adult care is assumed to have occurred.21–25 These visits were defined based on the specialty of the provider. Nine other studies defined the timing of transfer based on a fixed age, assuming that transfer occurred at that age.13,15,26–32 In Table 2, we summarize the challenges in identifying the timing of transfer as well as the methods that can be used to address each challenge.
Figure 1.
Flow diagram.
Table 1.
Study Characteristics and Methods
| First Author and Year of Publication | Location | Data Source | Disease Focus | Study Design | Methodology |
|---|---|---|---|---|---|
| Studies that define time of transfer based on last pediatric and first adult visits | |||||
| Bollegala 201721 | Ontario, Canada | Population-based health administrative data | Inflammatory bowel disease (IBD) | Retrospective cohort | “pre-transfer”: 2 years before the last pediatric visit “transfer of care”: time between last pediatric visit and first adult visit occurring at age ≥18 “post-transfer”: time from the first adult visit onward for 2 years |
| Hale 201722 | England | Routine hospital administrative data | Diabetes | Retrospective cohort | “Successful transition” = any adult service contact within 6 months of last paediatric contact. “Successful retention” = first planned adult contact within 6 months of the last planned paediatric contact, and at least 2 further adult contacts within the next 2 years |
| Mannion 201623 | United States | National commercial insurance administrative claims database | Juvenile idiopathic arthritis (JIA) | Retrospective cohort | The first adult visit was defined as the transfer point; this resulted in 3 distinct intervals: pediatric, transfer, and adult |
| Wisk 201524 | United States | Harvard Pilgrim Health Care Claims Data | Children with chronic conditions and healthy children | Retrospective Cohort | Timing of transfer measured from 16 years to first adult-focused primary care provider visit Transfer date: date of first adult-focused primary care visit |
| Zhao 201825 | Ontario, Canada | Population-based health administrative data | Inflammatory bowel disease (IBD) | Retrospective cohort | Transfer period: time between first adult gastroenterologist visit and the last pediatric gastroenterologist visit. |
| Studies that defined time of transfer based on age | |||||
| Blinder 201526 | United States | 5 US State Medicaid databases | Sickle cell Disease | Retrospective cohort | 18th birthday was defined as the age of transfer |
| Cohen 201627 | Ontario, Canada | Population-based health administrative data | Chronic health conditions | Retrospective cohort | 18th birthday was defined as the age of transfer |
| Dickerson 201228 | United States | Administrative data from 25 children’s hospitals within the Pediatric Health Information System (PHIS), | Sickle cell disease | Retrospective cohort | 18th birthday was defined as the age of transfer |
| Nakhla 200913 | Ontario, Canada | Population-based health administrative data | Diabetes | Retrospective cohort | 18th birthday was defined as the age of transfer |
| Reilly 201729 | Sweden | Population-based Swedish Inpatient Register | Celiac Disease | Retrospective Cohort | Pre-transition age: 16–17 years Post-transition age:19–20 years |
| Shulman 201815 | Ontario, Canada | Population-based health administrative data | Diabetes | Retrospective cohort | Pre-transition age: 15–17 years Transition-age: 17–19 years Early adulthood: 19–26 years (end of study) |
| Singh 201930 | Wisconsin, United States | Medicaid Data | Sickle Cell Disease | Retrospective Cohort | Transition age: 19 years |
| Toulany 201931 | Ontario, Canada | Population-based health administrative data | Mental illness | Retrospective cohort | Pre-transition: 12–16 years During transition: 17–18 years After transition: 19–26 years |
| Wijlaars 201832 | England | Hospital Episode Statistics Admitted Patient Care data | Long-term conditions (LTCs) (defined using the International Classification of Diseases) | Cross-sectional study | Pre-transition (ages 10–15 years) and after transition (19–24 years) |
Table 2.
Approaches to Identifying the Timing of Transfer to Adult Care Within Health Administrative Data
| Challenges of Identifying the Timing of Transfer to Adult Care | Methodological Approaches to Address Each Specific Challenge of Identifying the Time of Transfer |
|---|---|
| Identifying timing of transfer based on pediatric and adult visits |
|
| Identifying the timing of transfer for individuals who have “shared care” ie a pediatric visit occurring after the first adult visit | |
| Measuring disease onset, exposures, and outcomes relative to the timing of transfer |
|
| Accounting for individuals who never successfully transfer to adult care |
|
| Other Limitations of Administrative Data | Methodological Approaches |
|
|
Risk of selection bias caused by disease severity:
|
|
Non-comprehensive outcome data:
|
|
Identifying Time of Transfer Based on Pediatric and Adult Visits
Using the number and timing of pediatric and adult visits is one strategy that has been used to identify the time of transfer. To define the time of transfer studies have specified the number of visits to an adult and a pediatric provider, established a minimum time before and after the first adult visit, set a maximum time in the transfer period, and set a minimum number of visits to an adult provider.22,23,25,33 To measure continuity of care after transfer, Hale et al defined successful retention as having the first adult contact within six months of the last paediatric contact and then at least two subsequent adult contacts within the next two years.22 To address the challenge of identifying pediatric vs adult visits, Wisk et al used provider specialty codes from claims data to categorize providers as pediatric- or adult-focused primary care providers and then defined the time of transfer as the first adult-focused visit and the transfer gap as the time from last pediatric-focused visit to first adult-focused visit.24 To ensure that transfer of care was due to age and not geographic relocation, Mannion et al set a minimum age for inclusion at the time of transfer.23
Identifying Time of Transfer in Shared Care Models
Identifying the timing of transfer based on pediatric and adult care visits and specifically for individuals who have “shared care” defined as a pediatric visit occurring after the first adult visit presents researchers with many methodologic dilemmas on how to accurately identify transfer. Defining a transfer period is one approach used to identify the time of transfer for individuals who have a shared care model. For example, Zhao et al defined a transfer period as the time between the first adult visit and the last pediatric visit. If during this period there was shared care from both a pediatric and adult provider, the transfer period duration was assigned as the number of days from the first adult visit to the final pediatric visit.25 To identify individuals who had shared care, Mannion et al required that individuals have a pediatric visit followed by an adult visit and without a subsequent pediatric visit.23
Measuring Disease Onset, Exposures, and Outcomes Relative to the Time of Transfer
To ensure that individuals were diagnosed with a chronic condition requiring transfer to adult care, longitudinal data are needed to capture diagnoses prior to transfer to ensure that the condition existed prior to receipt of adult care. Depending on the nature of the chronic condition, this may require in-patient and/or outpatient data.32 Measuring outcomes after a washout period that starts after the first adult visit ensures that events after transfer were due to the transfer and not due to clinical status during the washout period. Sensitivity analyses can be conducted to vary the length of the washout period.25 Another approach is to measure exposures and outcomes immediately before and after a specific assumed date of transfer (eg, 18th birthday)13,26–28 or a period of time within which transfer is assumed to occur (eg, age 17 to 18 years).15,29–31
Accounting for Individuals Who Never Successfully Transfer to Adult Care
If the definition of the transfer period requires an adult visit, create a comparator group, “lost to adult follow-up” for those who never have an adult visit within the study period. Outcomes can be measured during an empirically set post-transfer period after the last pediatric visit.21
Risk of Selection Bias Caused by Disease Severity and Age at Diagnosis
Adolescents with a chronic condition who never see a pediatric provider and only ever see an adult specialist may have less severe disease or differ in their access to specialized pediatric care. This situation poses a risk of selection bias by disease severity. To mitigate this risk, Zhao et al adjusted for unmeasured confounding factors such as disease severity by using a self-controlled case series (SCCS) design, in which patients act as their own controls.25 Related, if primary care in childhood is delivered by a family physician (without a pediatric specialist) there may not be a transfer to an adult provider. Further, individuals diagnosed with a chronic condition around the age of transfer who never see a pediatrician may not meet a case definition if that definition includes a visit(s) to a pediatrician.
Discussion
In this review, we highlight several methodological issues that should be considered in the design of studies that aim to identify the timing of transfer to adult care within administrative data. We highlight several limitations of existing administrative datasets and summarize methods that have been used to address each specific challenge.
There are additional limitations to identifying the time of transfer to adult care using administrative data that were not addressed by any of the papers included in the current study. For example, defining the timing of transfer based on the last pediatric and first adult care visits is challenging if non-physician visits are not captured by administrative data. Further, pediatrician and pediatric specialist physician visits may not be reliably captured by administrative datasets if physicians do not bill fee-for-service, such as those who are paid by salary or other payment mechanisms. Adolescents may also obtain health services that are not captured by administrative data if they move away for post-secondary education and use university health services, which may underestimate healthcare use after transfer. If these missing data cannot be collected from alternative data sources (eg, medical records or survey data), they should be recognized and acknowledged. Finally, although we did not identify any studies that used transfer-specific billing codes, if available, these could be used to identify the time of transfer to adult care. In addition, the exact age of transfer within and between health systems and for different conditions varies.32 A further complicating issue is that young adults may transfer some health services at one time, while other health services are transferred at a later time. For example, university students might access a new primary care provider through school before they transfer to adult oriented speciality care. Finally, administrative data do not holistically capture the transition experience (eg, patient-report experience and outcome measures and social/educational/vocational outcomes). If available and feasible, administrative data may be linked to novel data sources that contain such information such as community health surveys and employment data (via tax returns).
Based on our findings, further empiric work is needed to compare the accuracy and feasibility of differing approaches to identifying transfer. However, because none of the reported methodologies entirely overcome the challenges of identifying the time of transfer using administrative data, there is a need for integrated pediatric and adult health information systems that span this vulnerable life stage. This is important for both clinical care and for evaluation of health service interventions for transition processes and outcomes. Measuring healthcare utilization for preventive care (office visits) may not be enough to elucidate the success of transfer. Longitudinal data to measure continuity of care in early adulthood in addition to other quality indicators and qualitative data are needed to evaluate this complex process.34 Our results will inform the development of future transition care research using health administrative data.
Acknowledgment
The authors would like to thank Quenby Mahood for her assistance in developing and implementing the search strategy.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. Meranda Nakhla was funded by Chercheur-boursier clinicien Junior 2 from the Fonds de Recherche du Québec – Santé and the Ministère de la Santé et des Services Sociaux du Québec.
Author Contributions
All authors (Rayzel Shulman, Eyal Cohen, Eric I Benchimol, and Meranda Nakhla) made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors have no conflicts of interest to declare.
References
- 1.Michaud P-A, Suris J-C, Viner R. The Adolescent with a Chronic Condition: Epidemiology, Developmental Issues and Health Care Provision. World Health Organization; 2007. [Google Scholar]
- 2.Peters A, Laffel L; American Diabetes Association Transitions Working G. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society). Diabetes Care. 2011;34(11):2477–2485. doi: 10.2337/dc11-1723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White PH, Cooley WC; Transitions Clinical Report Authoring G, American Academy Of P, American Academy Of Family P, American College Of P. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2018;142(5):e20182587. doi: 10.1542/peds.2018-2587 [DOI] [PubMed] [Google Scholar]
- 4.Blum RW, Garell D, Hodgman CH, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14(7):570–576. doi: 10.1016/1054-139X(93)90143-D [DOI] [PubMed] [Google Scholar]
- 5.White PH, Cooley WC; Transitions Clinical Report Authoring Group; American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians. Supporting the Health Care Transition From Adolescence to Adulthood in the Medical Home. Pediatrics. 2018;142(5):e20182587. Pediatrics. 2019;143(2) [DOI] [PubMed] [Google Scholar]
- 6.Nakhla M, Bell LE, Wafa S, Dasgupta K. Improving the transition from pediatric to adult diabetes care: the pediatric care provider’s perspective in Quebec, Canada. BMJ Open Diabetes Res Care. 2017;5(1):e000390. doi: 10.1136/bmjdrc-2017-000390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Michaud S, Dasgupta K, Bell L, et al. Adult care providers’ perspectives on the transition to adult care for emerging adults with Type 1 diabetes: a cross-sectional survey. Diabet Med. 2018;35(7):846–854. doi: 10.1111/dme.13627 [DOI] [PubMed] [Google Scholar]
- 8.Garvey KC, Telo GH, Needleman JS, Forbes P, Finkelstein JA, Laffel LM. Health care transition in young adults with type 1 diabetes: perspectives of adult endocrinologists in the U.S. Diabetes Care. 2016;39(2):190–197. doi: 10.2337/dc15-1775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garvey KC, Foster NC, Agarwal S, et al. Health care transition preparation and experiences in a U.S. national sample of young adults with type 1 diabetes. Diabetes Care. 2017;40(3):317–324. doi: 10.2337/dc16-1729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.A Guideline for Transition from Paediatric to Adult Health Care for Youth with Special Health Care Needs: A National Approach. Canadian Association of Paediatric Health Centres (CAPHC); 2016. [Google Scholar]
- 11.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. doi: 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- 12.Garvey KC, Wolpert HA, Rhodes ET, et al. Health care transition in patients with type 1 diabetes: young adult experiences and relationship to glycemic control. Diabetes Care. 2012;35(8):1716–1722. doi: 10.2337/dc11-2434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics. 2009;124(6):e1134–e1141. doi: 10.1542/peds.2009-0041 [DOI] [PubMed] [Google Scholar]
- 14.Lotstein DS, Seid M, Klingensmith G, et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131(4):e1062–e1070. doi: 10.1542/peds.2012-1450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shulman R, Shah BR, Fu L, Chafe R, Guttmann A. Diabetes transition care and adverse events: a population-based cohort study in Ontario, Canada. Diabet Med. 2018;35(11):1515–1522. doi: 10.1111/dme.13782 [DOI] [PubMed] [Google Scholar]
- 16.Gabriel P, McManus M, Rogers K, White P. Outcome evidence for structured pediatric to adult health care transition interventions: a systematic review. J Pediatr. 2017;188:263–269 e215. doi: 10.1016/j.jpeds.2017.05.066 [DOI] [PubMed] [Google Scholar]
- 17.Schultz AT, Smaldone A. Components of interventions that improve transitions to adult care for adolescents with type 1 diabetes. J Adolesc Health. 2017;60(2):133–146. doi: 10.1016/j.jadohealth.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 18.Bhawra J, Toulany A, Cohen E, Moore Hepburn C, Guttmann A. Primary care interventions to improve transition of youth with chronic health conditions from paediatric to adult healthcare: a systematic review. BMJ Open. 2016;6(5):e011871. doi: 10.1136/bmjopen-2016-011871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crowley R, Wolfe I, Lock K, McKee M. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child. 2011;96(6):548–553. doi: 10.1136/adc.2010.202473 [DOI] [PubMed] [Google Scholar]
- 20.Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–1294. doi: 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- 21.Bollegala N, Benchimol EI, Griffiths AM, et al. Characterizing the posttransfer period among patients with pediatric onset IBD: the impact of academic versus community adult care on emergent health resource utilization. Inflamm Bowel Dis. 2017;23(9):1483–1491. doi: 10.1097/MIB.0000000000001200 [DOI] [PubMed] [Google Scholar]
- 22.Hale D, Hargreaves DS. Predictors and outcomes of successful transition in diabetes: a national study of system performance using routine hospital administrative data. Arch Dis Child. 2017;102(Supplement 1):A61–A62. [Google Scholar]
- 23.Mannion ML, Xie F, Baddley J, et al. Analysis of health care claims during the peri-transfer stage of transition from pediatric to adult care among juvenile idiopathic arthritis patients. Pediatr Rheumatol Online J. 2016;14(1):49. doi: 10.1186/s12969-016-0107-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wisk LE, Finkelstein JA, Sawicki GS, et al. Predictors of timing of transfer from pediatric- to adult-focused primary care. JAMA Pediatr. 2015;169(6):e150951. doi: 10.1001/jamapediatrics.2015.0951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao X, Bjerre LM, Nguyen GC, et al. Health services use during transition from pediatric to adult care for inflammatory bowel disease: a population-based study using health administrative data. J Pediatr. 2018;203:280–287.e284. doi: 10.1016/j.jpeds.2018.08.021 [DOI] [PubMed] [Google Scholar]
- 26.Blinder MA, Duh MS, Sasane M, Trahey A, Paley C, Vekeman F. Age-related emergency department reliance in patients with sickle cell disease. J Emerg Med. 2015;49(4):513–522.e511. doi: 10.1016/j.jemermed.2014.12.080 [DOI] [PubMed] [Google Scholar]
- 27.Cohen E, Gandhi S, Toulany A, et al. Health care use during transfer to adult care among youth with chronic conditions. Pediatrics. 2016;137(3):e20152734. doi: 10.1542/peds.2015-2734 [DOI] [PubMed] [Google Scholar]
- 28.Dickerson AK, Klima J, Rhodes MM, O’Brien SH. Young adults with SCD in US children’s hospitals: are they different from adolescents? Pediatr Blood Cancer. 2012;58(5):741–745. doi: 10.1002/pbc.23262 [DOI] [PubMed] [Google Scholar]
- 29.Reilly NR, Green PHR, Ludvigsson JF. No difference in emergency department visits before and after transition for coeliac disease. Gut. 2017;66(11):2039–2040. doi: 10.1136/gutjnl-2017-313882 [DOI] [PubMed] [Google Scholar]
- 30.Singh A, Yan K, Brandow AM, Panepinto JA. Longitudinal trend in emergency department reliance for pain among sickle cell disease patients in wisconsin. Blood Conf. 2017;130(Supplement 1):128. [DOI] [PubMed] [Google Scholar]
- 31.Toulany A, Stukel TA, Kurdyak P, Fu L, Guttmann A. Association of primary care continuity with outcomes following transition to adult care for adolescents with severe mental illness. JAMA Network Open. 2019;2(8):e198415. doi: 10.1001/jamanetworkopen.2019.8415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wijlaars L, Hardelid P, Guttmann A, Gilbert R. Emergency admissions and long-term conditions during transition from paediatric to adult care: a cross-sectional study using hospital episode statistics data. BMJ Open. 2018;8(6):e021015. doi: 10.1136/bmjopen-2017-021015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lawrence JM, Sidell M, Li X, Desai J, O’Connor PJ, Schmittdiel JA. Timing and impact of transition from pediatric to adult care on glycemic control among adolescents and young adults with diabetes: results from the SUPREME-DM pilot study. Pediatr Diabetes. 2014;19:93–94. [Google Scholar]
- 34.Got transition? Tools: six core elements of health care transition and health care transition index; 2014. Accessed 2015.