Abstract
INTRODUCTION
Sepsis is a life-threatening emergency. Together, early recognition and intervention decreases mortality. Protocol-based resuscitation in the emergency department (ED) has improved survival in sepsis patients, but guideline-adherent care is less common in low-volume EDs. This study examined the association between provider-to-provider telemedicine and adherence with sepsis bundle components in rural community hospitals.
METHODS
This is a prospective cohort study of adults presenting with sepsis or septic shock in community EDs participating in rural telemedicine networks. The primary outcome was adherence to four sepsis bundle requirements: lactate measurement within three hours, blood culture before antibiotics, broad-spectrum antibiotics, and adequate fluid resuscitation. Multivariable generalized estimating equations estimated the association between telemedicine and adherence.
RESULTS
In this cohort (n=655), 5.6% of subjects received ED telemedicine consults. The telemedicine group was more likely to be male and have a higher severity of illness. After adjusting for severity and chief complaint, total sepsis bundle adherence was higher in the telemedicine group compared to the non-telemedicine group (aOR 17.27 [95%CI 6.64 – 44.90], p<0.001). Telemedicine consultation was associated with higher adherence with three of the individual bundle components: lactate, antibiotics, and fluid resuscitation.
DISCUSSION
Telemedicine patients were more likely to receive initial blood lactate measurement, timely broad-spectrum antibiotics, and adequate fluid resuscitation. In rural, community EDs, telemedicine may improve sepsis care and potentially reduce disparities in sepsis outcomes at low-volume facilities. Future work should identify specific components of telemedicine-augmented care that improve performance with sepsis quality indicators.
Keywords: sepsis, emergency department, telemedicine, sepsis bundle compliance
INTRODUCTION
Sepsis is a time-sensitive emergency condition that affects 750,000 people each year in the U.S. and has a mortality of 29%.1 Recognition and early management has been shown to improve patient outcomes, with 4% higher mortality for each hour of delay in sepsis care.2 Hospitals that have implemented protocol-based care for sepsis patients have improved treatment guideline adherence and improved survival.3, 4 Accurate recognition and resuscitation in the emergency department (ED) are critical for improving sepsis outcomes.
Telemedicine in the ED (teleED) has improved triage and management of time-sensitive emergency conditions, such as ischemic stroke, acute myocardial infarction, and trauma.5–7 Each of these emergency conditions has common characteristics: they benefit from timely care, have better outcomes in high volume EDs, and care has been extensively standardized.5 TeleED supports protocol-based care, supplements local care with expert clinicians who regularly treat uncommon emergencies, and facilitates triage and inter-hospital transfer.5, 8, 9
While the use of teleED has gained popularity, its use for sepsis care remains novel. In small hospitals, teleED may improve sepsis care and prevent costly and potentially avoidable transfer.10, 11 Previous reports of teleED for sepsis have been limited to a small pilot study and single-center before-after study.12, 13 While the vague and nonspecific symptoms that may indicate sepsis represent a diagnostic challenge for teleED sepsis programs, 14 the time-sensitive nature of early sepsis treatment, the ability to provide care in any ED even without advanced procedural capability, and the clear benefit of expert consultation on sepsis outcomes suggest that sepsis could be the perfect application for teleED care.2, 14
The objectives of this study are to evaluate the impact of telemedicine on adherence to sepsis bundle requirements in the ED. This study will assess the impact of telemedicine on process measures to better elucidate what role it might have in impacting rural health care systems.
METHODS
Study Design & Setting
This is a prospective cohort study of sepsis and septic shock patients presenting to EDs in six teleED networks between November 2015 and December 2017. All teleED networks participated in the Evidence-Based Tele-Emergency Network Grant Program (EB TNGP) for the purposes of comparative effectiveness studies of provider-to-provider telemedicine interventions in rural EDs. The six teleED networks service 65 spoke hospitals, which are 91% rural and a median ED annual volume of 8,427 visits.15 The EB TNGP was funded by the Health Resources & Services Administration (HRSA), Federal Office of Rural Health Policy (FORHP) to generate data on the impact of telemedicine programs on rural communities. These provider-to-provider networks use hub-and-spoke architecture to connect rural ED clinicians with a hub physician by high-definition video telemedicine. Each network prospectively collected data in all participating EDs using the Tele-Emergency Performance Assessment Reporting Tool (T-PART), which has been reported previously.15 The study was approved by the local Institutional Review Board at each participating telemedicine hub and the data coordinating and analysis center (the Rural Telehealth Research Center funded by FORHP and HRSA), and it is reported according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) Statement guidelines.16 Additionally, this analysis reports results of a comparative effectiveness analysis of clinical effectiveness, consistent with the National Quality Forum recommendations for measure development in telehealth.9
Study Population
Subjects were eligible for inclusion in the study cohort if they were adults (≥ 18 years) and presented to the ED with sepsis or septic shock in one of the participating telemedicine networks. Sepsis or septic shock was defined as an ED patient with (1) a presenting complaint of sepsis or septic shock, or (2) a diagnosis code (i.e. ICD-10-CM) related to sepsis or septic shock (i.e. A021, A227, A267, A327, A400, A401, A403, A408, A409, A4101, A4102, A411–414, A4150–53, A4159, A4181, A4189, A419, A427, A5486, B377, R6520, R6521). TeleED cases and non-teleED controls were selected from each participating network.
Key Outcome Measures & Measurements
Patients whose ED care involved teleED consultation, defined as one of the spoke site providers having meaningful, audio/video interaction with the hub site (including a clinician interaction), were considered teleED subjects. The primary outcome was adherence to all four sepsis bundle components while in the ED based on the National Hospital Inpatient Quality Measures Sepsis-1 (SEP-1) measure, defined as: (1) lactate collection within three hours after presentation of sepsis; (2) blood culture collection within three hours after presentation AND before administration of antibiotics; (3) antibiotics administration intravenously within three hours after presentation (antibiotics must have been from the SEP-1 approved list);17 and (4) fluid resuscitation of at least 30 mL/kg within three hours after presentation. Fluid resuscitation was recorded for all patients based on the current SEP-1 measure at the time the data collection tool was distributed.17 A second analysis was conducted of the composite measure, excluding fluid resuscitation. The primary outcome was complete bundle adherence, defined as adherence to the four components (i.e. lactate, blood culture, antibiotics, and fluid resuscitation). Bundle adherence was secondarily defined without the fluid resuscitation component, as some sepsis patients may not have had hypotension or elevated lactate to prompt fluid resuscitation, according to the revised SEP-1 definition.17 Individual component adherence was also evaluated as a secondary outcome.
Covariates were selected for risk adjustment and description of the study cohort and included: age, sex, race, ethnicity, chief complaint, ED arrival time and day, primary payer, and Current Procedural Terminology (CPT) code. ED arrival time was categorized into business hours (0730 – 1730) and non-business hours. The CPT code was defined as the highest level of emergency department Evaluation and Management (E&M) CPT code (e.g. 99281 to 99285, 99291, and 99292) associated with the ED visit and used as a proxy measure for severity of illness. Chief complaint, the reason for ED visit, was the subject’s documented symptoms or reason for visit on arrival at the ED. Chief complaint was recorded in the T-PART using 15 general categories (e.g.. abdominal pain, cough, fever or suspected infection, etc.) plus an “other” write-in option. Finally, ED principal diagnosis was the diagnosis established after the visit to be chiefly responsible for the ED visit. This diagnosis was categorized by Clinical Classification Software (CCS) into diagnosis categories.
Data Sources/Measurement
All variables, including exposure and outcome, were abstracted according to a detailed data dictionary from electronic medical records by research staff at each of the telemedicine networks. Data were recorded in the T-PART, a standardized data abstraction form designed for this study.15
Data Analysis
Subject characteristics and bundle adherence are presented as descriptive statistics for the total cohort and by teleED exposure with chi-square tests used to compare by exposure status. A multivariable generalized estimating equation (GEE) with a binomial distribution and logit link identified the factors most associated with teleED use. To estimate association of teleED use with sepsis bundle adherence, univariable and multivariable GEE models (binomial distribution and logit link) were constructed for six outcomes: each of the four individual bundle components (blood lactate measurement, blood cultures, antibiotic administration, and fluid resuscitation), total bundle adherence (i.e. all four components), and total bundle adherence excluding fluid resuscitation (i.e. lactate, blood culture, and antibiotic administration). For each model, purposeful selection was used to build multivariable models beginning with covariates hypothesized to be associated with teleED use and bundle adherence based on previous literature and theory. Covariates found not to be associated (p>0.10) with teleED in univariable tests were not considered for model inclusion; only teleED (primary exposure) was forced into the model. To identify the most parsimonious model, backwards selection guided by change in the coefficient of the primary variable of interest (i.e. teleED exposure) and minimization of the Akaike Information Criterion (AIC) were used. For the model predicting total bundle adherence with fluid resuscitation, there was evidence for overfitting of the model due to the relatively low number of cases, so only the two most significant covariates were included in the final model. Robust standard errors, clustered on ED facility with an exchangeable covariance matrix, were used. Analysis was conducted with STATA SE (version 15.0, StataCorp LP, College Station, TX).
RESULTS
Participants & Descriptive Characteristics
There were 655 cases of sepsis or septic shock identified(Figure 1). Eleven subjects were missing CPT code and were excluded from the multivariable analyses. Of the 644 subjects with sepsis included in the study cohort, 5.6% (n=36) utilized teleED (Table 1). There were no significant differences in patient age distribution, race, ethnicity, primary payer, arrival time, or day of the week between the two groups. However, in the non-teleED group, the cohort was 55% male vs 78% male in the teleED group (p=0.008). E&M CPT codes (i.e. amount of provider evaluation and management utilized) were different between the teleED and non-tele ED groups (p=0.005).
Figure 1.
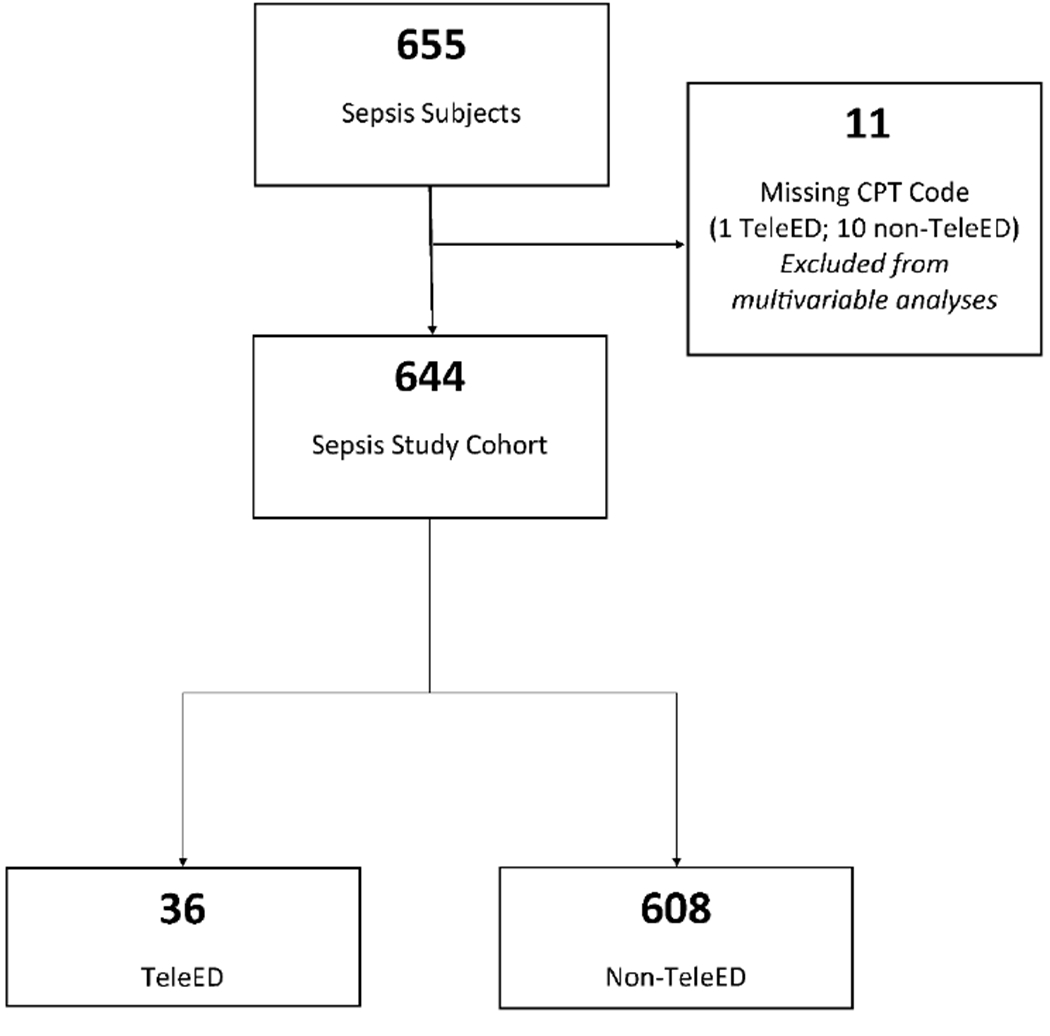
Flowchart of Study Subjects.
CPT = Current Procedural Terminology; TeleED= Emergency department telemedicine
Table 1.
Characteristics of Study Population by TeleED Exposure Status.
| Total N=644 | TeleED N=36 | Non-TeleED N=608 | p-value | |
|---|---|---|---|---|
| Age | 0.290 | |||
| 18-24 | 9 ( 1.4%) | 0 ( 0.0%) | 9 ( 1.5%) | |
| 25-44 | 50 ( 7.8%) | 1 ( 2.8%) | 49 ( 8.1%) | |
| 45-64 | 145 (22.5%) | 11 (30.6%) | 134 (22.0%) | |
| 65-74 | 158 (24.5%) | 12 (33.3%) | 146 (24.0%) | |
| 75 or older | 282 (43.8%) | 12 (33.3%) | 270 (44.4%) | |
| Sex | 0.008 | |||
| Female | 280 (43.5%) | 8 (22.2%) | 272 (44.7%) | |
| Male | 364 (56.5%) | 28 (77.8%) | 336 (55.3%) | |
| Race | 0.890 | |||
| White | 537 (83.4%) | 29 (80.6%) | 508 (83.6%) | |
| American Indian/Alaska Native | 88 (13.7%) | 6 (16.7%) | 82 (13.5%) | |
| Black/African American | 5 ( 0.8%) | 0 ( 0.0%) | 5 ( 0.8%) | |
| Unknown | 14 ( 2.2%) | 1 ( 2.8%) | 13 ( 2.1%) | |
| Ethnicity | 0.830 | |||
| Hispanic/Latino | 4 ( 0.6%) | 0 ( 0.0%) | 4 ( 0.7%) | |
| Not Hispanic/Latino | 615 (95.5%) | 35 (97.2%) | 580 (95.4%) | |
| Unknown | 25 ( 3.9%) | 1 ( 2.8%) | 24 ( 3.9%) | |
| Chief Complainta | <0.001 | |||
| Abdominal pain | 40 ( 6.2%) | 0 ( 0.0%) | 40 ( 6.6%) | |
| Cough | 58 ( 9.0%) | 0 ( 0.0%) | 58 ( 9.5%) | |
| Fever or suspected infection | 106 (16.5%) | 8 (22.2%) | 98 (16.1%) | |
| Nausea or vomiting | 39 ( 6.1%) | 1 ( 2.8%) | 38 ( 6.3%) | |
| Shortness of breath (dyspnea) | 87 (13.5%) | 4 (11.1%) | 83 (13.7%) | |
| Weakness | 50 ( 7.8%) | 6 (16.7%) | 44 ( 7.2%) | |
| ED Arrival Time | 0.690 | |||
| Business hrs. (0730-1730) | 355 (55.1%) | 21 (58.3%) | 334 (54.9%) | |
| Not business hrs. | 289 (44.9%) | 15 (41.7%) | 274 (45.1%) | |
| ED Arrival Day of Week | 0.510 | |||
| Monday | 91 (14.1%) | 4 (11.1%) | 87 (14.3%) | |
| Tuesday | 94 (14.6%) | 8 (22.2%) | 86 (14.1%) | |
| Wednesday | 103 (16.0%) | 6 (16.7%) | 97 (16.0%) | |
| Thursday | 83 (12.9%) | 7 (19.4%) | 76 (12.5%) | |
| Friday | 81 (12.6%) | 2 ( 5.6%) | 79 (13.0%) | |
| Saturday | 85 (13.2%) | 5 (13.9%) | 80 (13.2%) | |
| Sunday | 107 (16.6%) | 4 (11.1%) | 103 (16.9%) | |
| Primary Payer | 0.870 | |||
| Medicare only | 477 (74.1%) | 29 (80.6%) | 448 (73.7%) | |
| Private Insurance | 94 (14.6%) | 3 ( 8.3%) | 91 (15.0%) | |
| Medicaid only | 32 ( 5.0%) | 1 ( 2.8%) | 31 ( 5.1%) | |
| Self-pay/uninsured | 19 ( 3.0%) | 2 ( 5.6%) | 17 ( 2.8%) | |
| Indian Health Service | 13 ( 2.0%) | 1 ( 2.8%) | 12 ( 2.0%) | |
| Other | 9 ( 1.4%) | 0 ( 0.0%) | 9 ( 1.5%) | |
| CPT Code for Evaluation and Management | 0.005 | |||
| 99281/92282 | 5 ( 0.8%) | 0 ( 0.0%) | 5 ( 0.9%) | |
| 99283 | 20 ( 3.1%) | 2 ( 5.6%) | 18 ( 3.0%) | |
| 99284 | 200 (31.1%) | 9 (25.0%) | 191 (31.4%) | |
| 99285 | 406 (63.0%) | 21 (58.3%) | 385 (63.3%) | |
| 99291 | 5 ( 0.8%) | 2 ( 5.6%) | 3 ( 0.5%) | |
| 99292 | 8 ( 1.2%) | 2 ( 5.6%) | 6 ( 1.0%) | |
| ED Discharge Disposition | <0.001 | |||
| Admitted to local inpatient facility | 477 (74.2%) | 11 (30.6%) | 466 (76.8%) | |
| Transferred to another inpatient facility | 157 (24.4%) | 24 (66.7%) | 133 (21.9%) | |
| Other | 9 (1.4 %) | 1 ( 2.8%) | 8 ( 1.3%) | |
| ED Principal Diagnosis (By CCS) | <0.001 | |||
| Certain Infectious and Parasitic Diseases | 631 (98.0%) | 34 (94.4%) | 597 (98.2%) | |
| Other | 13 (2.1 %) | 2 ( 5.6%) | 11 ( 1.8%) |
Top six most common chief complaints listed to ensure confidentiality. Other chief complaints included chest pain, injury/trauma, sepsis, stroke symptoms, and weakness/lethargy.
Main Results
Overall, bundle adherence was 6.7% for all four components and 51.9% when excluding fluid resuscitation. TeleED consultation was associated with adherence to bundle elements of lactate measurement, early antibiotic administration, and adequate fluid resuscitation plus the number of bundle elements received (Table 2). Considering complete bundle adherence, 43.2% of patients in the teleED group received care in accordance with guidelines compared to 4.5% of non-teleED patients (p<0.001). When adequate fluid resuscitation was removed from the bundle, complete adherence rose to 75.7% in the teleED vs. 50.5% in the non-teleED group (p=0.003).
Table 2.
Bundle Adherence by TeleED Status.
| Adherence Component | Total N=655 | TeleED N=37 | Non-TeleED N=618 | p-value |
|---|---|---|---|---|
| Individual Components | ||||
| Blood lactate within 3 hours | 536 (81.8%) | 35 (94.6%) | 501 (81.1%) | 0.038 |
| Blood culture before antibiotics | 563 (86.0%) | 33 (89.2%) | 530 (85.8%) | 0.56 |
| Antibiotics within 3 hours | 409 (62.4%) | 31 (83.8%) | 378 (61.2%) | 0.006 |
| Adequate Fluid Resuscitation | 58 ( 8.9%) | 20 (54.1%) | 38 ( 6.1%) | <0.001 |
| # of Bundle Items Received | ||||
| 0 | 40 ( 6.1%) | 1 ( 2.7%) | 39 ( 6.3%) | <0.001 |
| 1 | 61 ( 9.3%) | 1 ( 2.7%) | 60 ( 9.7%) | |
| 2 | 201 (30.7%) | 3 ( 8.1%) | 198 (32.0%) | |
| 3 | 309 (47.2%) | 16 (43.2%) | 293 (47.4%) | |
| 4 | 44 ( 6.7%) | 16 (43.2%) | 28 ( 4.5%) | |
| Complete Bundle Adherence | 44 ( 6.7%) | 16 (43.2%) | 28 ( 4.5%) | <0.001 |
| Complete Bundle Adherence (Excluding Fluid Resuscitation) | 340 (51.9%) | 28 (75.7%) | 312 (50.5%) | 0.003 |
Data are presented as n (%).
When individual element and complete bundle adherence rates were adjusted for chief complaint and CPT code, total bundle adherence was more likely in the teleED group (aOR 17.27, CI 6.64-44.90, p<0.001). Similar results were observed when bundle adherence was re-defined without fluid resuscitation (Table 3). TeleED subjects were more likely to receive adherent care with respect to lactate measurement (aOR 7.85, CI 2.64-23.34, p<0.001), timely antibiotic administration (aOR 4.01, CI 1.16-13.87, p=0.028) and fluid resuscitation (aOR 20.29, CI 6.75-60.95, p<0.001) (Table 3). There was no difference in adherence with blood culture collection between the teleED and non-teleED groups (aOR 1.72, CI 0.61-4.85, p=0.311) (Table 3).
Table 3.
Unadjusted and Adjusted Measures of Association between TeleED and Bundle Adherence.
| Adherence Measure | uOR | 95%CI | p-value | aOR | 95%CI | p-value | ||
|---|---|---|---|---|---|---|---|---|
|
Individual Bundle Components:
Adjusted for Reason for ED Visit and CPT Code | ||||||||
|
| ||||||||
| Blood lactate within 3 hours | 6.89 | 2.97 | 16.12 | <0.001 | 7.85 | 2.64 | 23.34 | <0.001 |
| Blood culture before antibiotics | 1.95 | 0.65 | 5.87 | 0.232 | 1.72 | 0.61 | 4.85 | 0.311 |
| Antibiotics within 3 hours | 5.21 | 1.38 | 19.69 | 0.015 | 4.01 | 1.16 | 13.87 | 0.028 |
| Adequate Fluid Resuscitation^ | 24.29 | 6.69 | 88.23 | <0.001 | 20.29 | 6.75 | 60.95 | <0.001 |
|
| ||||||||
|
Complete Bundle Adherence:
Adjusted for CPT Code ^ | ||||||||
|
| ||||||||
| 20.49 | 8.33 | 50.41 | <0.001 | 17.27 | 6.64 | 44.90 | <0.001 | |
|
| ||||||||
|
Complete Bundle Adherence (excluding fluid resuscitation): Adjusted for Reason for ED Visit and CPT Code | ||||||||
|
| ||||||||
| 6.17 | 2.86 | 13.33 | <0.001 | 5.47 | 2.05 | 14.73 | 0.001 | |
Adjusted only for CPT due to concern for overfitting.
DISCUSSION
This project was a prospective evaluation of the effect of real-world implementation of high-definition video telemedicine for sepsis patients in telemedicine networks of rural hospitals. In this cohort, ED telemedicine consultation was associated with improved sepsis bundle adherence. This evaluation is unique because it provides the first evidence that telemedicine can be a scalable intervention for sepsis care in rural EDs. The use of telemedicine to improve protocol-based sepsis care has demonstrated feasibility and improved sepsis guideline adherence in intensive care units (ICUs)18, 19 and tertiary EDs.12, 13 However, the impact of health interventions are often different when they expand to scale, and telemedicine programs may function very differently from one another.20, 21
Guideline adherence is a commonly used surrogate for quality and timeliness of sepsis care,2, 22–25 and our findings are surprisingly similar to other telehealth sepsis interventions. Telemedicine-based interventions in ICUs have shown that adding a telemedicine provider to monitor sepsis-related interventions improved adherence with international sepsis guidelines. In a study by Deisz, et al., adding scheduled clinical rounds by critical care physicians in academic and community ICUs was associated with doubling adherence with the 3-hour (p=0.010) and the 6-hour sepsis bundles (p=0.001).18 In that report, improving the proportion of patients with appropriate fluid administration, timely measurement of venous oxygen saturation, and repeat measurement of lactate accounted for most of the effect. In the ED setting, our study found a similar magnitude association between telemedicine use and increased bundle adherence, but the principal effect in our ED-based study was on the timeliness of appropriate antibiotic administration.18
Another study by Machado, et al. reported an ED-based sepsis intervention where a dedicated sepsis specialist provided consultation and guidance to the emergency care team. In that study, antibiotics were administered faster in cases where telemedicine was used (122 vs. 163 min, 0=0.043).12 However, other elements of guideline adherence were not affected. Two important differences between the Machado study and our current study may explain some of these differences: (1) the Machado study used critical care specialists, whereas emergency physicians provided sepsis recommendations in our study and (2) the implementation setting (1000-bed teaching hospital) was different from the rural hospital networks we studied.12
Previous telemedicine pilot studies12, 13 have added a provider, nurse, or a quality specialist to the care of patients with sepsis, an approach that has been shown to be very effective in a variety of acute conditions, including sepsis.26–28 The Surviving Sepsis Campaign has published multiple reports that dedicated quality improvement initiatives for sepsis patients are associated with improvements in guideline adherence and corresponding improvements in clinical outcomes.23, 29, 30 While the benefit of these quality improvement initiatives is well-supported, these practice changes have been challenging in low-volume rural hospitals. Further, nationally reported quality metrics exclude patients in low-volume centers and transferred patients, limiting the impact of existing system-based initiatives on the rural facilities that are included in our report.11, 31, 32
Sepsis could be a uniquely powerful use case for ED-based provider-to-provider telemedicine.10 Different from trauma care, myocardial infarction care, and stroke care, no specific procedural, equipment, or specialty capabilities are necessary to provide high-quality sepsis resuscitation. Further, quality care that is provided very early has a disproportionately stronger effect on patient outcomes.33, 34 Sepsis patients who are transferred to tertiary centers can face significant care delays,35 and little sepsis care is currently provided during inter-hospital transfer – a particularly vulnerable time in sepsis patients’ disease course.36 As such, sepsis could be one of the few diseases where early resuscitation may be more important than early transfer to regional centers. Even though a robust volume-outcome relationship exists,4, 11, 37 providing a sepsis specialist by telemedicine to guide evaluation and management may be one feasible way to provide high quality care in networks of low-volume rural hospitals.
Our study has several limitations. First, the prospective data collected from telemedicine-connected emergency departments does not include inpatient outcomes such as mortality, which would be a valuable patient-centered outcome. Second, we do not have a robust method of calculating severity of illness (e.g., APACHE-II score), which opens our analysis to selection bias in telemedicine-connected hospitals. We used administrative billing data to adjust for severity, but residual confounding may exist.38 Third, we are not able to differentiate between severe sepsis and septic shock patients to capture full guideline adherence after the SEP-1 guideline revision. However, teleED remained beneficial when fluid resuscitation was excluded from the definition of adherence. Finally, there may be some patients who are transferred early, where guideline-adherence was not achieved because of early transfer. The benefit of collecting data from a large number of rural hospitals, however, makes our findings important in that we selected care-associated measures which are reliably measured according to a national standard.
In conclusion, in this cohort of patients with sepsis in rural emergency departments, telemedicine use was associated with increased bundle adherence. Improved adherence was greatest through improved timeliness of appropriate antibiotics and fluid resuscitation. Future work should focus on tailoring a telemedicine intervention to rural hospitals, better elucidating the role of telemedicine in local provider ongoing clinical training and developing models to evaluate the cost-effectiveness of telehealth-enabled ED-based provider-to-provider rural sepsis screening.
Acknowledgements
The authors thank Amanda Bell (PI), Luke Mack, Amy Wittrock from Avera Health; Eric Pollard (PI), Martha Nikides from St. Vincent Healthcare; Stephanie Laws (PI), Hicham Rahmouni, Daniel Hardesty, Amanda O’Brien from Union Hospital; James Marcin (PI), Jamie Mouzoon from University of California-Davis; Roger Humphries (PI), Brian Dennis, Theresa Mims, Rob Sprang from University of Kentucky; and Nina Solenski (PI), Tracy Blount from University of Virginia for contributing data for these analyses.
Financial Support
This study was supported by the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services (HHS) to the Rural Telehealth Research Center under cooperative agreement #UICRH29074. The Evidence-Based Tele-Emergency Network Grant Program provided funding for delivering teleED services to grantees - Avera Health (PI – Amanda Bell, Grant No. GO1RH27868), Saint Vincent Healthcare (PI – Eric Pollard, Grant No. G01RH27870), Union Hospital (PI – Stephanie Laws, Grant No. G01RH27871), University of California – Davis (PI – James Marcin, Grant No. G01RH27872), University of Kentucky (PI – Roger Humphries, Grant No. G01RH27873), and University of Virginia (PI – Nina Solenski, Grant No. G01RH27869). The information, conclusions, and opinions expressed are those of the authors and no endorsement by FORHP, HRSA, or HHS is intended or should be inferred. Dr. Mohr is additionally supported by grant K08 HS025753 from the Agency for Healthcare Research and Quality (AHRQ). The findings and conclusions are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ.
ABBREVIATIONS
- AIC
Akaike Information Criterion
- aOR
Adjusted odds ratio
- CCS
Clinical classification software
- CPT
Current Procedural Terminology
- E&M
Evaluation and management
- EB TNGP
Evidence-Based Tele-Emergency Network Grant Program
- ED
Emergency department
- FORHP
Federal Office of Rural Health Policy
- GEE
Generalized estimating equation
- HRSA
Health Resources & Services Administration
- SEP-1
Sepsis-1 measure
- STROBE
STrengthening the Reporting of OBservational studies in Epidemiology
- T-PART
Tele-Emergency Performance Assessment Reporting Tool
- teleED
Telemedicine in the emergency department
Footnotes
CONFLICTS OF INTEREST
The authors report no conflicts of interest.
PRESENTATIONS
This work was presented at the National Telehealth Research Symposium in Chicago, IL on September 12, 2019.
REFERENCES
- 1.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29: 1303–1310. 2001/July/11. [DOI] [PubMed] [Google Scholar]
- 2.Seymour CW, Gesten F, Prescott HC, et al. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N Engl J Med 2017; 376: 2235–2244. 2017/May/23. DOI: 10.1056/NEJMoa1703058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goodwin AJ, Simpson KN and Ford DW. Volume-Mortality Relationships during Hospitalization with Severe Sepsis Exist Only at Low Case Volumes. Ann Am Thorac Soc 2015; 12: 1177–1184. 2015/June/19. DOI: 10.1513/AnnalsATS.201406-287OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kocher KE, Haggins AN, Sabbatini AK, et al. Emergency department hospitalization volume and mortality in the United States. Ann Emerg Med 2014; 64: 446–457 e446. 2014/July/22. DOI: 10.1016/j.annemergmed.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Ward MM, Jaana M and Natafgi N. Systematic review of telemedicine applications in emergency rooms. Int J Med Inform 2015; 84: 601–616. 2015/June/15. DOI: 10.1016/j.ijmedinf.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Baratloo A, Rahimpour L, Abushouk AI, et al. Effects of Telestroke on Thrombolysis Times and Outcomes: A Meta-analysis. Prehosp Emerg Care 2018; 22: 472–484. 2018/January/19. DOI: 10.1080/10903127.2017.1408728. [DOI] [PubMed] [Google Scholar]
- 7.Mohr NM, Vakkalanka JP, Harland KK, et al. Telemedicine Use Decreases Rural Emergency Department Length of Stay for Transferred North Dakota Trauma Patients. Telemed J E Health 2018; 24: 194–202. 2017/July/22. DOI: 10.1089/tmj.2017.0083. [DOI] [PubMed] [Google Scholar]
- 8.Mohr NM, Young T, Harland KK, et al. Telemedicine Is Associated with Faster Diagnostic Imaging in Stroke Patients: A Cohort Study. Telemed J E Health 2019; 25: 93–100. 2018/June/30. DOI: 10.1089/tmj.2018.0013. [DOI] [PubMed] [Google Scholar]
- 9.Creating a Framework to Support Measure Development for Telehealth. 2017. National Quality Forum. [Google Scholar]
- 10.Ilko SA, Vakkalanka JP, Ahmed A, et al. Central Venous Access Capability and Critical Care Telemedicine Decreases Inter-Hospital Transfer Among Severe Sepsis Patients: A Mixed Methods Design. Crit Care Med 20192019/February/08. DOI: 10.1097/CCM.0000000000003686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohr NM, Harland KK, Shane DM, et al. Inter-hospital transfer is associated with increased mortality and costs in severe sepsis and septic shock: An instrumental variables approach. J Crit Care 2016; 36: 187–194. 2016/November/05. DOI: 10.1016/j.jcrc.2016.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Machado SM, Wilson EH, Elliott JO, et al. Impact of a telemedicine eICU cart on sepsis management in a community hospital emergency department. J Telemed Telecare 2018; 24: 202–208. 2017/December/28. DOI: 10.1177/1357633X17691862. [DOI] [PubMed] [Google Scholar]
- 13.Agarwal AK, Gaieski DF, Perman SM, et al. Telemedicine REsuscitation and Arrest Trial (TREAT): A feasibility study of real-time provider-to-provider telemedicine for the care of critically ill patients. Heliyon 2016; 2: e00099. 2016/July/22. DOI: 10.1016/j.heliyon.2016.e00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock 2012. Crit Care Med 2013; 41: 580–637. DOI: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 15.Heppner S MN, Carter K, Ullrich F, Merchant KAS, Ward MM. HRSA’s Evidence-Based Tele-Emergency Network Grant Program: Multi-site prospective cohort analysis across six rural tele-emergency networks [submitted]. PLoS Medicine 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61: 344–349. DOI: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services Joint Commission. Specifications manual for national hospital inpatient quality measures., https://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx (2016).
- 18.Deisz R, Rademacher S, Gilger K, et al. Additional Telemedicine Rounds as a Successful Performance-Improvement Strategy for Sepsis Management: Observational Multicenter Study. J Med Internet Res 2019; 21: e11161. 2019/January/22. DOI: 10.2196/11161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rincon TA, Bourke G and Seiver A. Standardizing sepsis screening and management via a tele-ICU program improves patient care. Telemed J E Health 2011; 17: 560–564. 2011/July/02. DOI: 10.1089/tmj.2010.0225. [DOI] [PubMed] [Google Scholar]
- 20.Scaling up projects and initiatives for better health: from concepts to practice. In: World Health Organization E, (ed.). Copenhagen, Denmark: 2016. [Google Scholar]
- 21.Schoenfeld AJ, Davies JM, Marafino BJ, et al. Variation in Quality of Urgent Health Care Provided During Commercial Virtual Visits. JAMA Intern Med 2016; 176: 635–642. 2016/April/05. DOI: 10.1001/jamainternmed.2015.8248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrer R, Artigas A, Levy MM, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA 2008; 299: 2294–2303. 2008/May/22. DOI: 10.1001/jama.299.19.2294. [DOI] [PubMed] [Google Scholar]
- 23.Miller RR 3rd, Dong L, Nelson NC, et al. Multicenter implementation of a severe sepsis and septic shock treatment bundle. Am J Respir Crit Care Med 2013; 188: 77–82. 2013/May/02. DOI: 10.1164/rccm.201212-2199OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cardoso T, Carneiro AH, Ribeiro O, et al. Reducing mortality in severe sepsis with the implementation of a core 6-hour bundle: results from the Portuguese community-acquired sepsis study (SACiUCI study). Crit Care Med 2010; 14: R83. 2010/May/13. DOI: 10.1186/cc9008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Zanten AR, Brinkman S, Arbous MS, et al. Guideline bundles adherence and mortality in severe sepsis and septic shock. Crit Care Med 2014; 42: 1890–1898. 2014/March/29. DOI: 10.1097/CCM.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 26.Purvis T, Kilkenny MF, Middleton S, et al. Influence of stroke coordinators on delivery of acute stroke care and hospital outcomes: An observational study. Int J Stroke 2017; 13: 585–591. DOI: 10.1177/1747493017741382. [DOI] [PubMed] [Google Scholar]
- 27.(UK) NCGC. NICE Guideline, No. 40. Major Trauma: Service Delivery. 11, Continuity of care: the trauma coordinator role. London, UK: National Institute for Health and Care Excellence. National Clinical Guideline Centre (UK), 2016. [PubMed] [Google Scholar]
- 28.Thompson DS, Oberteuffer R and Dorman T. Sepsis alert and diagnostic system: integrating clinical systems to enhance study coordinator efficiency. Comput Inform Nurs 2003; 21: 22–26; quiz 27-28. 2003/January/25. [DOI] [PubMed] [Google Scholar]
- 29.Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med 2010; 36: 222–231. 2010/January/14. DOI: 10.1007/s00134-009-1738-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levy MM, Rhodes A, Phillips GS, et al. Surviving Sepsis Campaign: association between performance metrics and outcomes in a 7.5-year study. Intensive Care Med 2014; 40: 1623–1633. 2014/October/02. DOI: 10.1007/s00134-014-3496-0. [DOI] [PubMed] [Google Scholar]
- 31.Mohr NM, Harland KK, Shane DM, et al. Rural Patients With Severe Sepsis or Septic Shock Who Bypass Rural Hospitals Have Increased Mortality: An Instrumental Variables Approach. Crit Care Med 2017; 45: 85–93. 2016/September/10. DOI: 10.1097/CCM.0000000000002026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Medicare & Medicaid Services: Joint Commission. Specifications Manual for National Hospital Inpatient Quality Measures.
- 33.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345: 1368–1377. 2002/January/17. DOI: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 34.Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006; 34: 1589–1596. 2006/April/21. DOI: 10.1097/01.Ccm.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 35.Faine BA, Noack JM, Wong T, et al. Interhospital Transfer Delays Appropriate Treatment for Patients With Severe Sepsis and Septic Shock: A Retrospective Cohort Study. Crit Care Med 2015; 43: 2589–2596. 2015/October/23. DOI: 10.1097/ccm.0000000000001301. [DOI] [PubMed] [Google Scholar]
- 36.Froehlich A, Tegtmeier RJ, Faine BA, et al. Opportunities for achieving resuscitation goals during the inter-emergency department transfer of severe sepsis patients by emergency medical services: A case series. J Crit Care 2019; 52: 163–165. 2019/May/13. DOI: 10.1016/j.jcrc.2019.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gaieski DF, Edwards JM, Kallan MJ, et al. The relationship between hospital volume and mortality in severe sepsis. Am J Respir Crit Care Med 2014; 190: 665–674. 2014/August/15. DOI: 10.1164/rccm.201402-0289OC. [DOI] [PubMed] [Google Scholar]
- 38.Mohr NM, Dick-Perez R, Ahmed A, et al. Emergency department charges may be associated with mortality in patients with severe sepsis and septic shock: a cohort study. BMC Emerg Med 2018; 18: 62. 2018/December/31. DOI: 10.1186/s12873-018-0212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


