Abstract
Objectives
We sought to identify the epidemiological characteristics of the first case series of patients with COVID-19 in Oman.
Methods
We included national surveillance data of patients with laboratory-confirmed COVID-19 from 24 February to 17 April 2020. Analyses were performed using descriptive and univariate statistics.
Results
Of the 1304 patients studied, the mean age was 37.0±13.0 years old, 80.3% were males, and 35.8% were Omanis. The other mostly affected nationalities were Indian (29.1%), Bangladeshi (20.0%), and Pakistani (10.7%). Out of the total, 80.1% were from the Muscat governorate. Omani patients were significantly more likely to be males than females and aged between 20 and 59 years old (p < 0.001). On presentation, 95.9% cases were mild, 3.6% moderate, and 0.5% severe. The case fatality rate was 0.5%. All deaths were from Muscat governorate; four from Mutrah, one from A'Seeb, and one from Bawshar.
Conclusions
This case series provides epidemiological characteristics as well as the early outcomes of patients with laboratory-confirmed COVID-19.
Keywords: COVID-19, Epidemiology, Coronavirus, Oman
Introduction
On the 31 December 2019, the World Health Organization (WHO) was notified about a cluster of pneumonia cases of unknown cause in Wuhan, China. A novel coronavirus disease, COVID-19, caused by severe acute respiratory syndrome coronavirus 2 virus (SARS-CoV-2) was identified in the cluster. The disease rapidly progressed into a pandemic.1,2 As of 22 May 2020, it has affected 5 106 686 individuals globally with 333 003 deaths and a 6.5% fatality rate.3
Nationwide, as of 22 May 2020, an aggregate of 6370 cases has been reported, with 1821 cases recovered and 30 deaths giving a mortality rate of 0.5%.3,4 The first two cases were reported on 24 February from the Muscat governorate, the capital of Oman, linked to travel to Iran. In this study, we characterize the epidemiological aspects of the first 1304 laboratory-confirmed cases in Oman.
Methods
All patients with laboratory-confirmed COVID-19 by SARS-CoV-2 real-time reverse transcriptase-polymerase chain reaction (RT-PCR) were enrolled between 24 February and 17 April 2020. The COVID-19 diagnosis was based on the national case definition and confirmed COVD-19 interim guidance.5
The data was retrieved from published national surveillance data6 and included the demographic characteristics (gender, age, place of residency, and nationality), patients’ outcomes (including recovery, hospitalization, and mortality), and severity of illness (including mild, moderate, and severe) based on the WHO definition.7
Descriptive statistics were used to describe the data. For categorical variables, frequencies and percentages were reported. Differences between groups were analyzed using Pearson’s chi-squared tests (or Fisher’s exact tests for expected cells < 5). For continuous variables, mean and standard deviation were used to present the data, while analyses were performed using a Student’s t-test. An a priori two-tailed level of significance was set at 0.05. Statistical analyses were conducted using STATA version 16.1.
This study was approved by the internal institutional review board and adhered to the Declaration of Helsinki.
Results
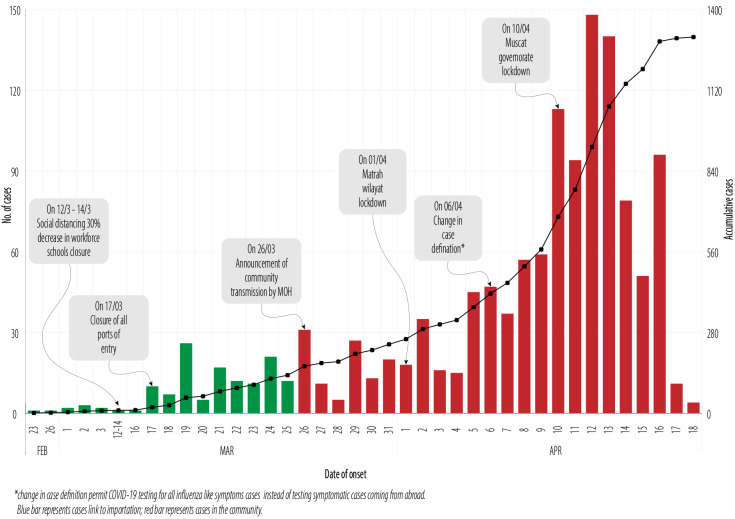
Over the study period, 1304 COVID-19 patients were laboratory-confirmed [Figure 1]. The overall mean age was 37.0±13.0 years, and 80.3% (n = 1047) were males. Omani COVID-19 patients were significantly more likely to be male than female and aged 20–59 years old (p < 0.001) [Figure 2]. As illustrated in Figure 3, a total of 35.8% (n = 467) of the diagnosed patients were of Omani nationality. The three other prevalent nationalities affected were Indian (29.1%; n = 380), Bangladeshi (20.0%; n = 261), and Pakistani (10.7%; n = 140). A further 28 patients were from Afghanistan (n = 2), UK (n = 2), Burundi (n = 2), Egypt (n = 2), Ireland (n = 2), Panama (n = 2), Saudi Arabia (n = 2), American Samoa (n = 1), Bahrain (n = 1), Colombia (n = 1), UAE (n = 1), Ethiopia (n = 1), Greece (n = 1), Indonesia (n= 1), Libya (n = 1), Malaysia (n = 1), Morocco (n = 1), Sierra Leone (n = 1), Sri Lanka (n = 1), Syria (n = 1), and Tunisia (n = 1). A total of 9.4% (n = 98) of the patients had traveled in from out of Oman with most from the UK (21.4%; n = 21) followed by India (15.3%; n = 15), and the UAE (11.2%; n = 11).
Figure 1.
COVID-19 cases in Oman from 23 February to 18 April 2020, along with the dates of various strategies to minimize its spread.
Figure 2.

Frequency distribution of Omani COVID-19 patients by age categories and gender.
Figure 3.
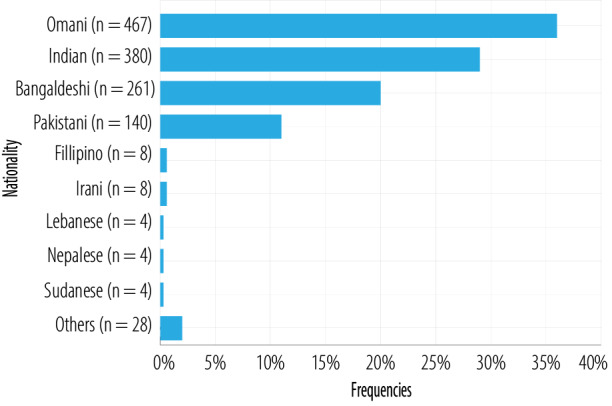
Distribution of COVID-19 patients in Oman by nationality.
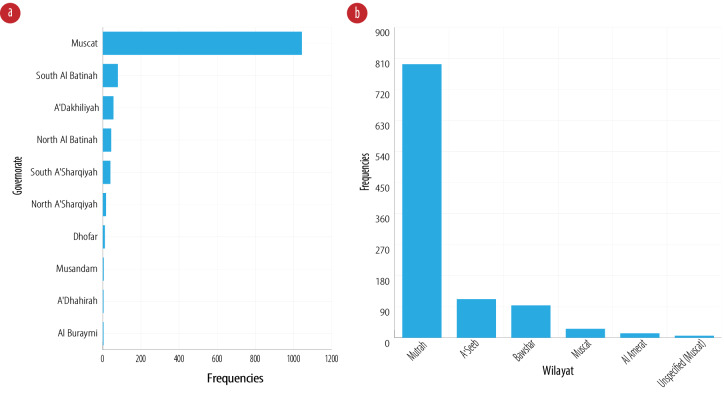
Figure 4a outlines COVID-19 patients by governorates with the majority (80.1%; n = 1044) from the Muscat governorate. The three other governorates mostly affected were South Al Batinah (6.1%; n = 79), A'Dakhiliyah (4.3%; n = 56), and North Al Batinah (3.4%; n = 44). Within the largest affected Muscat governorate, 76.0% (n = 793) of the affected patients were from the wilayat (district) of Mutrah. Apart from Mutrah, the three other prevalent wilayats in the Muscat governorate were A'Seeb (10.7%; n = 112), Bawshar (9.0%; n = 94), and Muscat (2.5%; n = 26) [Figure 4b].
Figure 4.
(a) Distribution of COVID-19 patients by governorate (n = 1304). (b) Distribution of COVID-19 patients by wilayat (n = 1044).
On presentation, 1250 (95.9%) cases were mild, 47 (3.6%) were moderate, and seven (0.5%) were severe. As of 23 April 2020, a total of 0.5% (n = 6) of COVID-19 patients died. All patients that died were from the Muscat governorate (Mutrah (n = 4), A'Seeb (n = 1), and Bawshar (n = 1)). Those who died were more likely to be older (61 vs. 37 years; p < 0.001) and specifically those aged between 60–69 years old (66.7%; n = 4) (p < 0.001). Although all those that died were males, no statistically significant results were attained regarding sex (0.6% vs. 0.0%; p = 0.224) largely due to the small sample size. There were, however, no significant differences in the mortality rate between Omani and non-Omani patients (0.4% vs. 0.5%; p = 0.899).
Discussion
In this retrospective study, the number of confirmed COVID-19 cases was 1304 over a period of two months. The country has scaled up preparedness and response plans and implemented several multifaceted public health measures (including but not limited to intercity travel restriction, social distancing measures, home confinement, institutional quarantine, and scaling of diagnostic tests and medical resources). While these interventions slowed and helped in reducing the initial surge of cases, the confirmed cases rate continued to increase in the period following 5 April 2020. This is perhaps in part due to the limited availability of diagnostic tests initially, delays in diagnosis, and limited access to medical treatment in areas highly populated with labor workers. Without a rapid diagnosis, the risk of cross-infection in the community increases, and individuals are likely to infect family members and close contacts. It has been reported that 70% of the cluster transmission occurred in Mutrah; one of the six districts in the Muscat governorate that each exhibit unique demographic, socioeconomic, and community features as it exhibits the highest numbers of foreign-born population mostly single laborer men living in very crowded housing with poor living conditions.6
Among the confirmed COVID-19 cases, males had a higher rate of confirmed cases than females, this was similar to the data from Italy and USA where 82% and 67% of patients were male, respectively,8,9 but contrary to the data from China where more females were infected, but with lower disease severity.10 Similar to several other studies,8-11 we observed a higher crude fatality rate among men. Although the reasons for these differences are unknown, it is possible that men were more likely to be exposed at work and had a higher proportion of comorbid conditions that might worsen their prognosis. This is consistent with earlier reports, that stated mortality was higher in elderly people.8,9
The study has several limitations. Being retrospective prevents making causal associations. Second, data was extracted from the public reporting system, and information on other epidemiological variables and clinical characteristics was missing. Additionally, we have no parallel data on the number of diagnostic tests that were performed and the percentage of asymptomatic cases, which might explain the initial low numbers of confirmed COVID-19 cases.
Conclusion
Our results suggest that vigorous strategies should be implemented to protect and reduce transmission and symptom progression of COVID-19 in vulnerable populations, including both elderly people and foreign-born individuals living in crowded housing.
Disclosure
The authors declare no conflict of interest. No funding was received for this study.
References
- 1.Balkhair AA. COVID-19 Pandemic: A New Chapter in the History of Infectious Diseases. Oman Med J 2020. Apr;35(2):e123 . 10.5001/omj.2020.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Director-General’s opening remarks at the media briefing on COVID 19:11March 2020. [cited 2020 March 30]. Available from: https://www.who.int/dg/speeches/detail/ who-director-general-s-opening-remarks-at-themedia-briefing-on-covid-19---11-march-2020.
- 3.Wikipedia. COVID-19 pandemic by country and territory. [cited 2020 March 19]. Available from: https://en.wikipedia.org/wiki/COVID-19_pandemic_by_country_and_territory.
- 4.WHO. EMR Dashboard. [cited 2020 May 15]. Available from: https://app.powerbi.com/view?r=eyJrIjoiN2ExNWI3ZGQtZDk3My00YzE2LWFjYm QtNGMwZjk0OWQ1MjFhI iwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04M TBiLTNkYzI4MGFmYjU5MCIsImMiOjh9.
- 5.Oman MO. Human Infection with Novel Corona Virus (COVID-19). Interim Guideline – 7 for Hospitals, Primary and Private Health. [cited 2020 May 5]. Available from: https://www.moh.gov.om/documents/10194/3903020/Case+definition+6+April.pdf/5bb2988f-3af2-ce46-da34-80e27059b989.
- 6.Statements and Updates. Ministry of Health, Oman. [cited 2020 April 17]. Available from: https://www.moh.gov.om/en/-5.
- 7.WHO. Q&A on coronaviruses (COVID-19). [cited 2020 April 17]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-coronaviruses.
- 8.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. COVID-19 Lombardy ICU Network. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020. Apr;323(16):1574-1581 . 10.1001/jama.2020.5394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet 2020. Jun;395(10239):1763-1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020. Apr;323(19):1915-1923 . 10.1001/jama.2020.6130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). [cited 2020 March 2]. Available from: https://www.who.int/docs/defaultsource/ coronaviruse/who-china-joint-mission-oncovid-19-final-report.pdf.