Abstract
Follicular unit extraction (FUE) is a popular hair transplant technique, which involves extraction of follicular grafts from the donor area, usually occipital area of scalp. We have described few cases where non-scarring alopecia patches appeared at donor area similar to that of alopecia areata clinically, after 2–3 weeks of surgery. Even trichoscopically, findings were similar to alopecia areata showing exclamation marks, black dots. However, on histopathology, there were dilated blood vessels, mucin deposition, and only few lymphocytes, which mimic histopathology of healing wound. We hypothesize that compromised blood supply and trauma to the existing hairs after harvesting can lead to post-hair transplant effluvium, which is probably due to anagen effluvium.
Keywords: Alopecia areata simulator, complications of hair transplantation, donor area acute effluvium, follicular unit extraction complications, shock loss alopecia
INTRODUCTION
Follicular unit extraction (FUE) is minimally invasive hair transplant procedure where follicular grafts are harvested from the donor area with the help of micropunches of 0.7–1 mm in size.[1] The technique has become popular after first being described by Rassman et al.[2] in 2002 due to least donor-site morbidity. The suggested density of extraction of graft from the donor area is almost 1:3, that is, one unit of every three units can be extracted.[3] If there is extensive harvesting, it leads to compromised blood supply to the existing hair after hair transplant at the donor area, which can lead to the necrosis at recipient area as reported by Karaçal et al.[4] The reduced blood supply can lead to post-hair transplant donor area effluvium, where patches of alopecia are present at donor area mimicking clinically and dermoscopically to alopecia areata as seen in our patients. Apart from extensive harvesting, excessive use of adrenaline in tumescent anesthesia can also affect the vascularity of scalp at donor area, further compromising the blood supply. Usually alopecia improves in a few weeks to few months but can cause anxiety to the patient as well as the transplant surgeon.
CASE SERIES
A case series of four patients is summarized in Table 1. All patients are male. Age of onset varied from 28 to 55 years (mean, 38.75 years). No patient had a history of cigarette smoking. Two patients had a history of taking alcohol occasionally. Two patients were grade 2 on Hamilton classification of male pattern hair loss, one was grade 3, and one was grade 6.[5] The number of extracted grafts from the donor occipital and parietal area was 2200–3500 (mean, 2975), and the mean extracted graft to grafts density was 1:3.25. In all the patients, adrenaline was used in the tumescence as well as anesthesia. No case had postoperative infection. The alopecic patches appeared at the donor area after 2–3 weeks of procedure. The SALT (Severity of Alopecia Tool) score was 4.2–27.6 (mean, 14) [Figures 1 and 2]. Hair pull test was positive in all the patients. On trichoscopy, multiple black dots, exclamation mark, and coudability sign were present (Dino-Lite AM4113ZT Video-dermoscope, Taiwan) [Figure 3]. Histopathologic examination showed dilated capillaries around hair follicles, mucin deposition around arrector muscles, dermal edema, and only few lymphocytes [Figure 4]. No patient had a past or family history of alopecia areata. There was moderate to good improvement in all patients with intralesional triamcinolone.
Table 1.
Summary of four cases
| Case | Age | Sex | AGA grade | Number of extracted graft | Graft extraction density | Appearance of patches after surgery | SALT score | Response to intralesional steroids |
|---|---|---|---|---|---|---|---|---|
| 1 | 30 | M | 3 | 3200 | 1:3 | 3 weeks | 27.6 | Yes |
| 2 | 55 | M | 6 | 3000 | 1:3 | 2 weeks | 13.5 | Yes |
| 3 | 28 | M | 2 | 2200 | 1:4 | 2 weeks | 4.2 | Yes |
| 4 | 42 | M | 2 | 3500 | 1:3 | 2 weeks | 10.8 | Yes |
AGA = androgenetic alopecia, M = male
Figure 1.
Case 1. (A) The alopecic patches at donor area after FUE (donor area acute effluvium). (B) Improvement after treatment with intralesional corticosteroids
Figure 2.
Case 2. (A) Donor area acute effluvium. (B) Improvement after treatment with intralesional corticosteroids
Figure 3.

Trichoscopy showing multiple black dots, exclamation mark, and coudability sign (×50, Dino-Lite AM4113ZT Video-dermoscope)
Figure 4.
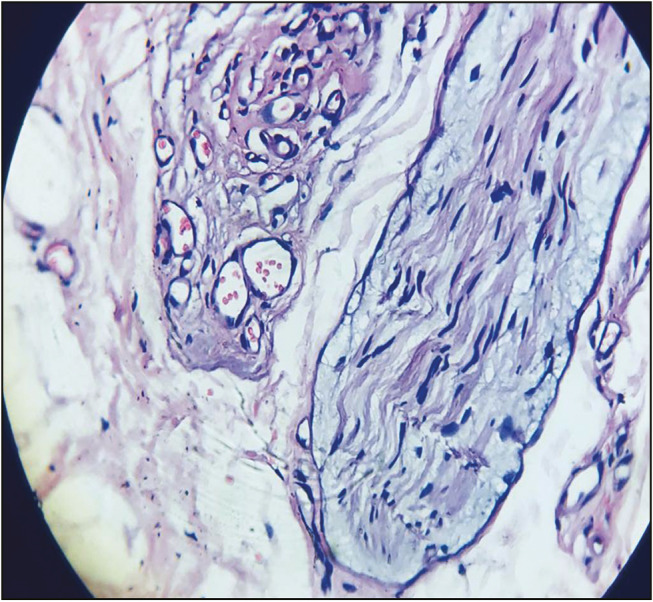
Histopathologic examination showing dilated capillaries around hair follicles, mucin deposition around arrector muscles, dermal edema, and only few lymphocytes (hematoxylin and eosin, ×40)
DISCUSSION
Hair transplantation for androgenetic alopecia is one of the commonly performed cosmetic procedures. FUE has advantage of no linear scar at the donor area in comparison to follicular unit transplant.[6] Extraction of the grafts from the donor area in FUE technique is a skillful procedure. After local anesthesia and tumescent infiltration, scoring of follicular graft is carried out with the help of motorized micropunches. The reported donor site complications are donor-site depletion, buried grafts, and epithelial cysts.[6] Our patients presented with alopecic patches after FUE in the donor area clinically. On trichoscopy, there were broken hairs and exclamation marks. On histopathological examination, dilation of blood vessel, mucin deposition, and few lymphocytes were present, which is similar to the histopathology of healing wound in proliferative phase.[7] Patchy hair loss with the aforementioned trichoscopic features can be seen in alopecia areata, which is a self-limiting autoimmune condition. As these cases developed alopecic patches within two week after procdure, with no past or family history of alopecia areata, and no histopathological features in favor of it; hence, alopecia areata is the less likely diagnosis. Similar trichoscopic features can be due to anagen effluvium where trauma can be a precipitating factor.[8,9,10]
After hair transplantation, donor area effluvium, also known as shock loss,[6] is reported in FUT as well, wherein tightness of suture, edema, and inflammation can compromise vascular supply. This leads to donor shock loss above and below the line of incision but is usually temporary, and full recovery is almost always observed in the following 3–4 months.[6,11] A dramatic hair loss may be seen in accidental major vascular damage.[6] It is mentioned that topical minoxidil helps in faster recovery.[11] In our patients, we hypothesized that the reduced blood supply due to injury to blood vessels may be the reason behind the posttransplant appearance of alopecic patches termed as shock loss, probably due to anagen effluvium. Few of our patients responded to intralesional triamcinolone.
CONCLUSION
Patchy hair loss at the donor hair in a patient, who had undergone follicular unit extraction, should raise the suspicion of posttransplant effluvium, and dermatologist should not confuse it with alopecia areata.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.James AH. New methodology and instrumentation for follicular unit extraction: lower follicle transection rates and expanded patient candidacy. Dermatol Surg. 2008;32:56–62. doi: 10.1111/1524-4725.2006.32006. [DOI] [PubMed] [Google Scholar]
- 2.Rassman WR, Bernstein RM, McClellan R, Jones R, Worton E, Uyttendaele H. Follicular unit extraction. Dermatol Surg. 2002;28:720–8. doi: 10.1046/j.1524-4725.2002.01320.x. [DOI] [PubMed] [Google Scholar]
- 3.Humayun Mohmand M, Ahmad M. Effect of follicular unit extraction on the donor area. World J Plast Surg. 2018;7:193–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Karaçal N, Uraloğlu M, Dindar T, Livaoğlu M. Necrosis of the donor site after hair restoration with follicular unit extraction (FUE): a case report. J Plastic Reconstruct Aesthet Surg. 2012;65:e87–9. doi: 10.1016/j.bjps.2011.06.040. [DOI] [PubMed] [Google Scholar]
- 5.Gupta M, Mysore V. Classifications of patterned hair loss: a review. J Cutan Aesthet Surg. 2016;9:3–12. doi: 10.4103/0974-2077.178536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerure AS, Patwardhan N. Complications in hair transplantation. J Cutan Aesthet Surg. 2018;11:182–9. doi: 10.4103/JCAS.JCAS_125_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gantwerker EA, Hom DB. Skin: histology and physiology of wound healing. Facial Plast Surg Clin North Am. 2011;19:441–53. doi: 10.1016/j.fsc.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Anagen effluvium—an overview. 2010. [Last accessed 2019 April 12]. ScienceDirect Topics Sciencedirect.com Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/anagen-effluvium .
- 9.Danko C, Suszko J, Fett N. Localized anagen effluvium and cataract development following an extended fluoroscopic interventional procedure. Dermatol Online J. 2016;22:13030/qt7fb2c1hc. [PubMed] [Google Scholar]
- 10.Mehta P, Malakar S, Malakar S. Tulipoid hair: anagen effluvium marker! Int J Trichol. 2018;10:188. doi: 10.4103/ijt.ijt_98_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garg A, Garg S. Donor area complications of strip harvesting. In: Mysore V, editor. Hair transplantation. 1st ed. New Delhi, India: Jaypee Brothers Medical Publishers; 2016. pp. 282–87. [Google Scholar]




