Abstract
Prevention and treatment of non-communicable diseases (NCDs), including cardiovascular disease, diabetes, obesity, cancer, Alzheimer's and Parkinson's disease, arthritis, non-alcoholic fatty liver disease and various infectious diseases; lately most notably COVID-19 have been in the front line of research worldwide. Although targeting different organs, these pathologies have common biochemical impairments – redox disparity and, prominently, dysregulation of the inflammatory pathways. Research data have shown that diet components like polyphenols, poly-unsaturated fatty acids (PUFAs), fibres as well as lifestyle (fasting, physical exercise) are important factors influencing signalling pathways with a significant potential to improve metabolic homeostasis and immune cells' functions. In the present manuscript we have reviewed scientific data from recent publications regarding the beneficial cellular and molecular effects induced by dietary plant products, mainly polyphenolic compounds and PUFAs, and summarize the clinical outcomes expected from these types of interventions, in a search for effective long-term approaches to improve the immune system response.
Keywords: Inflammation, Polyphenols, Polyunsaturated fatty acids, Nutraceuticals
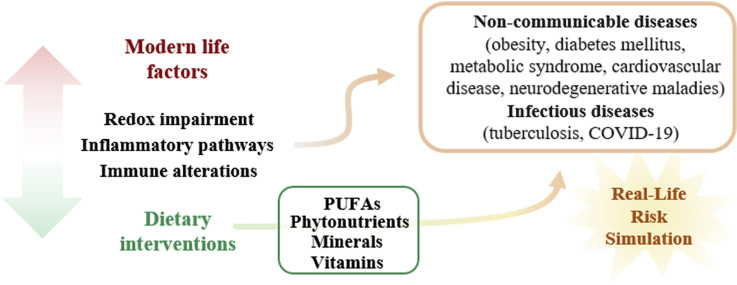
Graphical abstract
1. Introduction
Non-communicable diseases (NCDs), the silent epidemic, are responsible for the majority of deaths in developed countries and their prevalence at a younger age was observed increasingly in the last years (WHO, 2013, 2018). Cardiovascular disease (CVD), diabetes, obesity, cancer, Alzheimer's and Parkinson's disease, arthritis, non-alcoholic fatty liver disease (NAFLD) and chronic obstructive disease are some of the most common NCDs sharing common features. Research shows that redox impairments and chronic low-grade inflammation generate a vicious biochemical self-propagating cycle, constituting the molecular pathological root of these diseases. In the context of modern lifestyle, stress factors including malnutrition/overnutrition, smoking or sedentary routine are initiating factors for the impairment of inflammatory pathways contributing to the development of NCDs. Furthermore, in real-life scenarios, people experience uncontrolled simultaneous exposure to many environmental chemicals, hence novel methodological approaches simulating real-life exposures are being developed under the name real life risk simulation (RLRS) with the aim to assess the potential adverse health effects of long-term exposure to chemical mixtures (Hernandez et al., 2019; Hernandez and Tsatsakis, 2017; Tsatsakis et al., 2016, 2019a). According to WHO, 80% of NCDs-related deaths could be prevented by changes in these modifiable risk factors, and recent evidence identified unhealthy diet as the biggest risk factor for NCDs-related deaths (Collaborators, 2019; WHO, 2018).
Under physiological conditions, inflammation is a response to harmful stimuli (pathogens or tissue lesions), a cellular adaptive mechanism aiming to restore tissue homeostasis (Medzhitov, 2008). Inflammatory responses are self-limited through specific checkpoints that curb the progression and promote the resolution of inflammation (Basil and Levy, 2016; Serhan and Savill, 2005). Failure due to the deleterious alterations of the inflammatory pathways brings about the excessive release of pro-inflammatory molecules, leading to chronic low-grade inflammation and fibrosis (Norling and Serhan, 2010; Russell and Schwarze, 2014). The persistence of this usually short-term defence mechanism leads to a chronic inflammatory state, transitioning from solution to cause, becoming in fact a lesion-inducing factor for the affected tissues. This may be a result of the dysregulation of several cellular pathways involving cyclooxygenase-2 (COX-2), signal transducer and activator of transcription 3 (STAT3), matrix metalloproteinase-9 (MMP-9), nuclear factor kappa-B (NF-κB), cytokines with inflammatory outcome: interleukins (IL-1, IL-6, IL-8), tumour necrosis factor alpha (TNF-α), cell adhesion molecules and chemokines, etc. Of note, the resolution of the inflammatory process cannot be simply switched off by restricting the synthesis of the pro-inflammatory molecules, requiring cellular intervention through anti-inflammatory and pro-resolving molecules (Minihane et al., 2015; Ortega-Gomez et al., 2013; Serhan et al., 2008).
Mitigating the pathological pathways associated with chronic low-grade inflammation through pharmacological agents but, more importantly, through diet and lifestyle changes might constitute an effective strategy in the prevention of NCD and NCD-related deaths. In the current review, we overview recent facts from molecular and animal studies to human clinical reports regarding the intricate pathways that are affected by some of our dietary habits, also discussing the next steps that ought to be taken in addressing these parameters.
2. Cellular and molecular inflammatory-related mechanisms
In physiological conditions, NF-κB (a heterotrimer with p65 and p50 subunits associated with the IκBα inhibitory subunit) is localized to the cytoplasm. Under the effect of inflammatory stimuli (for instance cytokines – IL-8, IL-1β, IL-6, or TNF-α, UV exposure, etc), the heterodimer dissociates, IκBα is degraded, and the two components, p50 and p65, translocate into the nucleus binding the promoter regions from different genes that are involved in initiating several cellular pathways linked to chronic diseases, tumorigenesis, angiogenesis and metastasis. Among the genes regulated by NF-κB are the ones for the expression of TNF-α, COX-2, MMP-9, nitric oxide synthase – the inducible form (iNOS), cytokines (IL-1, IL-6 and IL-8), 5-lipooxigenase (5-LOX), vascular endothelial growth factor (VEGF); all of these genes, when up-regulated fire-up the vicious circle constituted from oxidative stress and inflammation (Aggarwal, 2009; Kawabata et al., 2012; Kunnumakkara et al., 2018; Nimigean et al., 2018, 2019; Poll et al., 2018a, 2018b; Reuter et al., 2010). Interestingly, the NF-κB cascade is also activated by some factors that affect the circadian rhythm, such as aging or sleep deprivation. In animal models, high-fat diets as well as obesity – pro-inflammatory states, are directly correlated with a decrease of the amplitude of circadian activity and rhythmic gene expression, thus, suggesting that the inflammatory pathways are directly responsible for influencing the circadian clock (Gachon et al., 2018; Kohsaka et al., 2007; Osorio et al., 2016).
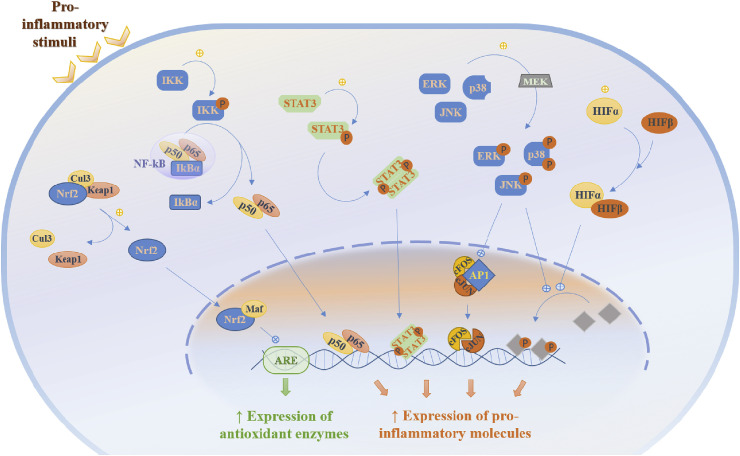
Another important inflammatory pathway involves STAT3, a cytoplasm protein that is phosphorylated by JAK 1, 2, and 3 (Janus-activated kinases), under the influence of inflammatory stimuli. STAT3 reaches the nucleus and functions as a transcriptional factor, stimulating the synthesis of inflammatory mediators (Pandurangan et al., 2015; Sung et al., 2012). The MAPK/ERK (mitogen-activated protein kinases) group, including stress activated protein-kinases p38, JNK (c-Jun N-terminal kinases) and ERK (extracellular signal-regulated kinases), is also involved in the inflammatory cascade as a response to a detrimental stimulus (Liang et al., 2016). Also, to the family of transcription factors we can comprise nuclear factor erythroid 2-related factor 2 (Nrf2), activator protein-1 (AP-1), nuclear factor of activated T cells (NFAT) or hypoxia-inducible factor-1α (HIF-1α), all being recognized for their role in stress response as well as in mediating inflammation (Panieri et al., 2020; Reuter et al., 2010) (Fig. 1 ).
Fig. 1.
Regulation of cellular pathways under the influence of pro-inflammatory stimuli (Keap1 – Kelch-like ECH-associated protein 1; Cul3 – Cullin 3; Nrf2 – Nuclear factor erythroid 2-related factor 2; IKK – IκB kinase; NF-κB – Nuclear factor kappa-light-chain-enhancer of activated B cells heterodimer, consisting of p50, p65 and IkBα proteins; STAT3 – Signal transducer and activator of transcription 3; ERK/MAPK – mitogen-activated protein kinases; JNK – c-Jun N-terminal kinases; MEK – Mitogen-activated protein kinases kinase; HIFα – Hypoxia-inducible factor α; HIFβ – Hypoxia-inducible factor β; AP1 – Activator protein 1, with its associated proteins cFOS - and cJUN; Maf – Transcription factor Maf; ARE – antioxidant response element).
Pro-inflammatory stimuli activate several regulatory cell processes. The activation of IKK (IκB kinase) causes the cleavage of NF-kβ, associated with nuclear translocation for p50 and p65, while that of MAPK directs the phosphorylation of p38, ERK and JNK. Also notable are the dimerization of STAT3 and the association of HIFα with HIFβ, all resulting in the activation of several transcription factors or direct stimulation of gene expression, targeting pro-inflammatory molecules. However, an increased expression of antioxidant enzymes can be encountered due to decreased degradation of Nrf2 and its activation of ARE, post-nuclear translocation and association with Maf. The activation of all the inflammation-related pathways, along the cellular and metabolic disturbances that follow, contributes to the high occurrence of obesity and associated pathology (diabetes mellitus, metabolic syndrome, CVD, Alzheimer's disease, etc), especially under the influence of modern life factors (malnutrition, smoking, pollution, low physical activity) (De Lorenzo et al., 2016; Georgescu et al., 2014; Georgescu, 2014; Gustafson et al., 2007; Libby, 2012; Ungurianu et al., 2017, 2019a; Wang et al., 2004; Zanfirescu et al., 2019). The obese state is characterized by low-grade systemic inflammation, with impaired synthesis of adipokines and activation of pro-inflammatory signalling pathways leading to insulin resistance. Adipose tissue inflammation is one of the determining factors of obesity complications, impairing the adipocyte secretory function and hormonal balance.
Physiologically, adipose tissue resident macrophages, displaying both a pro-inflammatory and anti-inflammatory phenotype, are involved in several housekeeping processes (differentiation of preadipocytes, abstraction of necrotic and apoptotic cells, angiogenesis adjustment, etc). The expansion of adipose tissue, due to long-lasting overnutrition, induces prolonged hypoxia (the activation of HIF-1α), and consequent inflammation as monocytes infiltrate in the hypoxic region and become pro-inflammatory macrophages, process during which TNF-α, monocyte chemotactic protein (MCP-1), IL-6, MMPs, IL-8, VEGF are released. Further, the inflammatory response elicited by dysfunctional adipocytes, hypoxia, adipocyte expansion, and impaired fatty acids storage is accelerated by formation of reactive species, either oxygen (ROS) or nitrogen (RNS) (Crewe et al., 2017; Demaria et al., 2014; Fujisaka et al., 2013; Margina et al., 2012; Pasarica et al., 2009; Paun et al., 2015; Schipper et al., 2012; Trayhurn, 2014).
Metabolic impairments associated with obesity may contribute to the release of inflammatory mediators (IL-18, IL-1β) due to the stimulation of the NLR (nucleotide-binding oligomerization domain (NOD)-like receptors) family pyrin domain-containing 3 (NLRP3) which forms a cytoplasmic complex known as the NLRP3 inflammasome, with direct modulating role on the innate immune system. This pathway is involved in obesity as well as associated inflammation, and among the endogenous danger signals activating it we can find glucose and ROS. Also, literature data states that IL-18 as well as IL-1β are produced as an effect of TLR (Toll-like receptors)-mediated NF-κB activation, thus pointing out to the interaction of different signalling pathways (Fettelschoss et al., 2011; Tschopp and Schroder, 2010; Zhou et al., 2010).
In the light of these pathways, consolidated research is needed to point out in ability of some dietary components, based on the RLRS approach, to reduce the expression of inflammatory molecules and resolve the ROS-inflammation cycle, in order to diminish the risk for long-time comorbidities associated with obesity/metabolic impairments.
3. Microenvironment originating inflammatory cues
The extracellular matrices (ECMs), are complex, multi-constituent meshes that surround and support cells in tissues, with a regulatory role in all biological processes, as well as in tissue organization (Hynes, 2009). The ECMs are composed of fibrillar proteins and proteoglycans, as well as glycosaminoglycans specifically organized as modules or domains. The ECM suprastructure can be envisaged as a “platform” receiving, and simultaneously, delivering a myriad of signals to cells that are crucial to homeostasis, but also contributing to the progression of various pathologies (Sifaki et al., 2006; Tzanakakis et al., 2018, 2019). Importantly, the inflammation-mediated alterations in the ECM result in release of active mediators crucial to disease progression (Kavasi et al., 2017; Neagu et al., 2019; Nikitovic et al., 2015). Noteworthy, the effects exerted by remodelled ECM are cell and tissue type dependent exerting thus, specific influence to discrete tissue compartments (Nikitovic et al., 2014a).
Recent developments highlighted the importance of ECM remodelling in metabolic disease and obesity as well as the associated inflammation (Ruiz-Ojeda et al., 2019). Indeed, it was suggested that both the specific remodelling of adipose tissue ECM organization and dysregulated intracellular signalling processes may be correlated with obesity-associated insulin resistance (Guzman-Ruiz et al., 2020). The main components of adipose tissue ECM are collagens, fibronectin and laminin (Mori et al., 2014). Minor constituents include osteopontin, hyaluronan (HA), thrombospondins, MMPs, as well as A disintegrin and metalloproteinase domain-containing protein (ADAMs), and contribute significantly to ECM remodelling and the regulation of adipose tissue functions (Lin et al., 2016).
The main characteristic of obesity is an increase in lipid tissue infiltration due to the hypertrophy of existing adipocytes, as well as due to the hyperplasia of adipocytes resulting from de novo adipogenesis from precursor stem cells (Schoettl et al., 2018). Indeed, it was postulated that the ECM, in a spatial as well as temporal manner, regulates adipogenesis (Soukas et al., 2001). In addition to adipocyte deposition, a notable migration of macrophages and vascular cells was correlated to changes in the ECM structure. This remodelling leads to the release of active mediators that can affect immune cells’ recruitment and activation, facilitating the inflammatory state of lipid tissue. Furthermore, the strong upregulation of obese adipose tissue ECM components, including collagens and osteopontin, was suggested to initiate the necrosis of adipocytes, enhance the infiltration of immune cells, leading to tissue inflammation and metabolic dysfunction (Catalan et al., 2012; Ruiz-Ojeda et al., 2019). Thus, the overexpression of endotrophin, resulted from the cleavage of the α-3 chain of collagen VI (Col6a3), facilitates the deposition of fibrotic collagen and initiates adipose tissue inflammation and insulin resistance (Sun et al., 2014). A recent study demonstrated that the expression of MMP14 is strongly upregulated in the adipose tissue of transgenic obese mice. Interestingly, MMP14 proteolytic activity results in the release of endotrophin with concurrent formation of enlarged adipocytes and increase in body weight, altered lipid metabolism and insulin resistance (Li et al., 2020). Furthermore, Springer et al. recently demonstrated a link between alterations in the ECM of obese women and breast cancer. Thus, enhanced adipose tissue interstitial fibrosis facilitates the generation of M2/M1 type macrophages pattern similar to that of tumour-associated macrophages, as well as the generation of associated inflammatory cues (Springer et al., 2019). Under these conditions a paracrine loop consisting of free fatty acids and TNF-α is established among adipocytes and infiltrating macrophages that enhances inflammation-mediated alterations in the adipose tissue (Engin, 2017). Recently, lumican, a small leucine-rich proteoglycan (Nikitovic et al., 2014b), was shown to be overexpressed in ECM of subcutaneous fat of insulin resistant obese individuals. Lumican was demonstrated to alter the organization of collagen I, dysregulate adipogenesis and trigger oxidative stress, facilitating the pathology of obesity-associated insulin resistance (Guzman-Ruiz et al., 2020). A separate study showed that the effect of lumican was diet-dependent and correlated to adipose tissue inflammation. Indeed, the same authors suggest that the ECM protein lumican could pose a convergent point among the ECM, the glucose homeostasis and the metabolic syndrome (Wolff et al., 2019).
Osteopontin, an ECM glycoprotein, excessively secreted by adipose tissue macrophages (Nomiyama et al., 2007) enhances adipose tissue inflammation and facilitates the onset of insulin resistance (Aouadi et al., 2013). Another important ECM component, the glycosaminoglycan HA, has been strongly correlated to increased inflammatory burden, including cancer-associated (Nikitovic et al., 2015) and sterile inflammation (Kavasi et al., 2017, 2019; Nikitovic et al., 2014b). The biologic role of HA is dependent on its size. Thus, high molecular weight HA (HMWHA), physiologically secreted by cells facilitates normal tissue stability (Kavasi et al., 2017). In contrast, low molecular weight HA (LMWHA) fragments, produced via enzymatic action or chemical reactions, are pro-inflammatory and have been characterized as a danger-associated molecular patterns (DAMP) (Kavasi et al., 2017, 2019; Nikitovic et al., 2014a). Indeed, the generated LMWHA fragments can trigger a Toll-like receptor 4 (TLR4)/NF-κB signalling pathway to regulate inflammatory genes transcription in immune cells (Kavasi et al., 2017; Termeer et al., 2002). Interestingly, HA levels were increased in various tissues of type-2 diabetes mellius (T2DM), but not in type-1 (T1DM) subjects, and independent of glycaemic control. Taking into account that T2DM, in contrast to T1DM, is linked with systemic inflammation, it was suggested that inflammatory factors and not hyperglycaemia upregulate HA levels (Nagy et al., 2019). Importantly, it was demonstrated that the expression of genes involved in the metabolism of HA was positively correlated to the process of adipocyte differentiation (Allingham et al., 2006). Recently, it was shown that HA exerts inhibitory effects in vitro regarding adipogenesis of 3T3-L1 cells, whereas downregulating HA prevented insulin resistance and NAFLD correlated to excess deposition of abdominal fat in HFD-feeding C57BL/6J mouse model (Ji et al., 2014). Moreover, treatment of HFD-fed obese mice with a stable hyaluronidase complex, where human recombinant hyaluronidase was Pegylated, was shown to decreases adiposity, adipose tissue inflammation and insulin resistance (Kang et al., 2013).
A hallmark of metabolic diseases is a high NADH/NAD+ ratio, originating from excessive electron supply. This dysregulation results in an altered mitochondrial function and sirtuin-3 (SIRT-3) activity, which result in oxidative stress and distorted fatty acid β-oxidation (Cortes-Rojo et al., 2020). Increased ROS production was shown to induce excessive remodelling of the ECM in a pathological milieu (Nikitovic et al., 2013). Thus, oxidative stress induced by high-glucose levels, in rat glomerular mesangial cells, resulted in an increased deposition of collagen IV and fibronectin, through the involvement of the TXNIP-NLRP3 inflammasome signalling (Wang et al., 2017). Importantly, the remodelling of renal ECM is involved in the progression of diabetic nephropathy, one of the most serious complications of diabetes mellitus. Treatment aimed at downregulating ROS generation, such as the utilization of dihydroquercetin (DHQ), an important natural dihydroflavone, attenuated the activation of NLRP3 inflammasome and the subsequent of increased deposition to ECM of renal fibrosis-associated proteins upon exposure of renal cells to high glucose levels (Ding et al., 2018).
These data highlight the complex interactions between the ECM, inflammation, and metabolic diseases. The reorganization of the ECM as well as ECM-originating pro-inflammatory cues needs to be taken account when designing efficient therapy for inflammation associated disease. Dietary measures might constitute important means to mitigating these pathological pathways.
4. Carbohydrate–restricted diets and their effects on inflammation
Postprandial hyperglycaemic spikes are linked to ROS generation and inflammation, as ROS, via the NF-κB pathway, promote the expression of pro-inflammatory molecules such as MCP-1, TNF-α, IL-6, IL-1β, along AP-1, as well as FOXO. These molecules interfere with the insulin signalling pathway, add to the insulin resistance progress (Lumeng et al., 2008; Weisberg et al., 2003) and affect blood levels of some inflammatory biomarkers more than chronic hyperglycaemia (Barrea et al., 2018; Della Corte et al., 2018). Healthy diets, based on low glycaemic index food, resulting in a lesser increase of glycemia and lipemia in postprandial settings, induced a lower production of pro-inflammatory molecules (Barrea et al., 2018; Della Corte et al., 2018). In preclinical studies, a strict restriction of carbohydrate intake was shown to promote inflammation and shorten lifespan in senescence-prone mice, increasing IL-6 and IL-1β, compared to diets rich in fats (He et al., 2019), with no alteration of serum glucose or insulin versus a standard diet (Nilsson et al., 2016).
However, a long-term carbohydrate-restricted, high-fat diet promoted a pro-inflammatory state (He et al., 2018), impairing glucose (Ellenbroek et al., 2014; He et al., 2018) and lipid metabolism (Garbow et al., 2011), affecting liver (Garbow et al., 2011) and pancreatic function (Ellenbroek et al., 2014; He et al., 2018). A high intake of saturated fats also led to an increase in pro-inflammatory molecules’ levels (IL-1β or leptin) (Andre et al., 2017), although a short-term diet enrichment with ketone diesters induced anti-inflammatory effects in NLRP3-mediated inflammatory maladies (Youm et al., 2015). Post-spinal cord injury, a ketogenic diet reduced oxidative stress as well as inflammation, suppressing the NF-κB pathway (Andre et al., 2017; Lu et al., 2018), while activating Nrf2, resulting in lowering TNF-α, IL-1β, IFN-γ expression (Lu et al., 2018). The highlights of these studies are presented in Table 1, Table 2 .
Table 1.
Clinical studies regarding the effect of high fibre intake on inflammatory markers in obesity and associated pathology.
| Design | Population | Dietary intervention | Outcome | Reference |
|---|---|---|---|---|
| Randomized cross-over trial | 50 Danish subjects with high risk of metabolic syndrome | two 8-week periods of whole grain intake (179 ± 50 g/day)/refined grain (maximum 13 ± 10 g/day of whole grain), divided by a washout period of ≥6 weeks. | ↓ body weight, serum inflammatory markers (IL-6, CRP) | Roager et al. (2019) |
| Double-blind, crossover, placebo-controlled, randomized study | 45 metabolic syndrome patients risk factors | galactooligosaccharide mixture intervention to increase dietary fibre content, with a 4-wk wash-out period between interventions | ↓ faecal calprotectin, CRP | Vulevic et al. (2013) |
| Randomized controlled trial | 143 individuals with metabolic syndrome | 12 weeks of rye and whole wheat was compared with a diet containing the equivalent amount of refined cereal foods | no significant effects on the expression of inflammatory markers' genes or insulin sensitivity | Giacco et al. (2013) |
| Randomized crossover study | 19 adults with metabolic syndrome | 4-week of arabinoxylan and resistant starch enriched diet versus Western-style, low-fibre diet | ↓ faecal calprotectin, IL-23A and NF-κB | Hald et al. (2016) |
| Crossover intervention study | 25 hypercholesterolemic subjects | 5-week intervention using low fibre and high fibre diet, separated by a 3-week washout. | ↓ CRP and fibrinogen | Johansson-Persson et al. (2014) |
| Randomized controlled trial | 68 overweight with prediabetes | 12 weeks of 45 g/d of high-amylose maize (RS2) versus an isocaloric amount of amylopectin (control) | ↓ TNF-α, no change in insulin sensitivity | Peterson et al. (2018) |
| Randomized controlled trial | 166 subjects with features of metabolic syndrome | 4-week using healthy diet (fruits and vegetables, berries, whole-grain products, rapeseed oil, three fish meals per week) compared to an regular Nordic diet | Control diet: ↑ IL-1 Ra (versus healthy diet group) | Uusitupa et al. (2013) |
| Crossover study | 10 healthy subjects | Subjects received either 910calorie high- carbohydrate/high-fat meal or a standard meal according to American Heart Association (based on fruit and fibre) during the first visit and the other meal during the second visit | ↑ oxidative stress (bloodlevels of TBARS, LPS, FFA) and proinflammatory markers (TNFα, and IL-1β) | Dandona et al. (2015) |
| Randomized controlled trial | 28 T2DM patients | Subjects received brown rice (n = 14) or white rice (n = 14) diet for 8 weeks | ↓ CRP in brown rice group | Kondo et al. (2017) |
| Parallel design, dietary intervention trial | 104 subjects with metabolic syndrome risk | Subjects received Healthy Diet (n = 44), a whole-grain-enriched diet (n = 42) or a control (n = 45) diet, | Healthy Diet group: ↓ E-selectin Healthy Diet and whole grain group: ↓ CRP |
de Mello et al. (2011) |
| Cross-over, randomized, placebo-controlled, double-blind, study | 12 overweight and obese subjects | Subjects received 20 g/day of inulin (high-fermentable fibre) and cellulose (low-fermentable fibre) for 42 days | IPE: ↓ IL-8 levels (versus cellulose)Inulin: no effect on the inflammatory markers | Chambers et al. (2019) |
| Crossover clinical study | 18 subjects at low-to-moderate cardiometabolic risk | Subjects received breakfast either rich in fibre, unsaturated fatty acids (unSFA) or saturated fatty acids (SFA) for 4 weeks | SFA: ↑ IL-1β unSFA: ↓IL-6 | Monfort-Pires et al. (2018) |
| Interventional diet study | 21 overweight/obese children | Subjects were placed on a regimen of low-fat, high-fibre diet and daily exercise for 2 weeks | ↓ PAI-1, TNF-α, IL-6, IL-8, resistin, insulin, amylin, leptin, and IL-1ra ↑ adiponectin |
Izadpanah et al. (2012) |
| Randomized, placebo-controlled study | 31 hemodialysis patients | Patients received either resistant starch or placebo supplementation, for 4 weeks | ↓ IL-6 and TBARS | Esgalhado et al. (2018) |
| Randomized controlled clinical trial | 55 women with T2DM | Subjects received 10 g resistant dextrin/day or a similar amount of maltodextrin for 8 weeks | ↓ IL-6, TNF-α and MDA ↑ Insulin sensitivity |
Aliasgharzadeh et al. (2015) |
| Randomized cross-over double-blind placebo-controlled trial | 17 obese knee osteoarthritis patients | Patients received freeze-dried strawberries or placebo for 2 periods of 12 weeks with 2 weeks of wash-out | ↓ TNF-α and 4-HNE | Basu et al. (2018) |
| Randomized study | 59 T2DM patients | Patients received metformin, acarbose and either a high fibre or a low fibre diet intervention for 8 weeks | Low fibre group: ↓ IL-18 | Nowotny et al. (2015) |
| Crossover study | 33 healthy, middle-aged adults | Patients received either high or low in in wholegrain intervention for 6-week periods, separated by a 4-week washout. | Whole grain: a slight decrease of IL-10 and CRP | Ampatzoglou et al. (2016) |
| Observational study | 8 subjects with impaired fasting glucose | subjects received (1) high-fibre formula; (2) high-monounsaturated fatty acid formula or (3) control formula | High fibre group: ↓ NF-κB in PBMCs | Kim et al. (2013) |
| Randomized controlled clinical trial | 60 females with T2DM | Patients received 10 g/d resistant starch or placebo for 8 weeks, respectively | ↓TNF-α, no effect on IL-6 or CRP | Gargari et al. (2015) |
| Crossover clinical trial | 80 overweight subjects | Subjects received two isocaloric breakfast interventions -one rich in saturated fat and one in unsaturated fatty acids and fibres for 4 weeks with a 2-weeks washout. | Fibre group: ↓ IF-γ and TNF-α | Monfort-Pires et al. (2018) |
| Observational study | 49 T2DM females | Patients received either 10 g/day inulin or maltodextrin/day for 8 weeks | Inulin: ↓CRP, TNF-α and LPS | Dehghan et al. (2014a) |
| Randomized controlled clinical trial | 52 overweight/obese women with T2DM | Patients received either 10 g/d of oligofructose-enriched inulin or maltodextrin (control) for 8 weeks | oligofructose-enriched-Inulin: ↓ CRP, TNF-α and LPS | Dehghan et al. (2014b) |
| Randomized crossover clinical trial | 44 overweight/obese girls 8–15 years old | Subjects received either whole-grain or control for 2 periods of 6 weeks with 4-week washout period | Whole grain: ↓ CRP, ICAM-1 and leptin | Hajihashemi et al. (2014) |
Table 2.
Preclinical reports regarding the relationship between carbohydrate intake and inflammation.
| Diet | Species | Treatment | Observed effects | References |
|---|---|---|---|---|
| Carbohydrate-restricted diet | Senescence-accelerated prone mice (SAMP8) | 8-week treatment:
|
CRD: ↑ IL-6 and IL-1β, ↓cecum short-chain fatty acids | He et al. (2019) |
| Scandinavian low-carbohydrate high-fat (LCHF) diet | Female C57BL/6J mice (n = 7/group) | 4-week treatment:
|
LCHF: no change in glycemia, TG, insulin, or non-esterified fatty acid plasma levels | Nilsson et al. (2016) |
| Ketogenic diet | Sprague-Dawley Rats with spinal cord injury (n = 18/group) | 4-week treatment:
|
KD: ↓ IL-1β, TNF-α, IFN-γ expression | Lu et al. (2018) |
| Ketogenic diet | Male C57BL/6J mice | 22-weeks diet intervention:
|
KD: ↑ triglycerides, cholesterol, leptin, MCP-1, IL-6, IL-1β, ↓ α- and β-cell mass |
Ellenbroek et al. (2014) |
| Ketogenic versus Western diet | C57BL/6J mice | 12-week treatment:
|
KD: euglycaemia and hypoinsulinemia + liver lipid accumulation (different pattern compared to WD) KD: systemic glucose intolerance, steatosis, cellular injury, endoplasmic reticulum stress (in liver), and macrophage accumulation, maintaining whole-body insulin responsiveness |
Garbow et al. (2011) |
| High-saturated fat diet (HFD) | male C57BL/6J mice | 3-week treatment:
|
HFD: ↑ leptin, IL-1β | Andre et al. (2017) |
| Diet supplemented with ketones | Knockout mice model for Muckle-Wells Syndrome and Familial Cold Autoinflammatory syndrome | 1-week treatment:
|
Study group: ↓ IL-1β release and caspase-1 activity | Youm et al. (2015) |
| High fat high sucrose diet (HFD) | C57BL/6 J (wild type; WT) male mice | 8-week treatment:
|
HFD led to β-cell failure in aged mice, enhanced expression of pro-inflammatory cytokines and macrophage transformation to a more pro-inflammatory phenotype | He et al. (2018) |
On the other hand, long-term diets abundant in highly processed and high glycaemic index products seem also to induce a pro-inflammatory metabolic profile (Gomes et al., 2020; Luz et al., 2018). These recent reports suggest that not only the quantity, but also the type of carbohydrates and fats consumed is the major influencing factor of systemic inflammatory status. Thus, clinically, even a 4-day low-carbohydrate diet intervention improved the insulin and fasting plasma glucose levels in T2DM patients (Myette-Cote et al., 2018). When comparing low-carb to low-fat diets in diabetics, some older studies reported a similar effects on cardiovascular risk markers (Davis et al., 2011), while more recent ones asserted the beneficial effects of restricting carbohydrates on the systemic low-grade inflammation, reducing IL-6 (Asle Mohammadi Zadeh et al., 2018; Jonasson et al., 2014), resistin, leptin (Asle Mohammadi Zadeh et al., 2018), E-selectin, sICAM (Davis et al., 2011) and increasing adiponectin (Asle Mohammadi Zadeh et al., 2018). Furthermore, the improvement of systemic inflammatory status was also reported in obese adults, with no T2DM or CVD (Hu et al., 2015).
Switching to a very strict low-carb diet was associated with an increase of systemic inflammation in apparently healthy subjects (Rosenbaum et al., 2019), while in subjects with metabolic syndrome or obesity, a short-term ketogenic diet yielded beneficial cardiometabolic effects (Gyorkos et al., 2019; Ruth et al., 2013). In T2DM patients, a one-year nutritional ketosis intervention resulted in a lower cardiovascular risk (Bhanpuri et al., 2018). Importantly, these beneficial effects are amplified by physical exercises (Alves et al., 2016; Asle Mohammadi Zadeh et al., 2018; Myette-Cote et al., 2018), and by the diet supplementation with nuts (Hou et al., 2018), soy (Kani et al., 2017), or even carefully choosing the types of ingested carbohydrates. In obese and overweight adolescents and adults, a diet based on low glycaemic index food improved inflammation, metabolic as well as cardiovascular risk factors (Rouhani et al., 2016), while the addition of functional foods resulted in further benefits (Izadi et al., 2018). Also, the consumption of complex carbohydrates led to a decline of pro-inflammatory molecules’ level in pregnant women (Hernandez et al., 2016). The results of most recent clinical studies concerning the link between low-carb diet and systemic inflammation are summarized in Table 3 .
Table 3.
Recent reports regarding the relationship between carbohydrate intake and inflammation.
| Diet type | Design | Population | Intervention | Effects | Ref. |
|---|---|---|---|---|---|
| Low-carbohydrate versus high-fat diet | Randomized crossover study | 11 T2DM patients | 4-day diet intervention:
|
Glycemia and circulating proinsulin were significantly lower in groups 2 and 3 versus 1; | Myette-Cote et al. (2018) |
| Low-carbohydrate versus low-fat diet | Randomized controlled feeding study | 33 obese T2DM patients | 8-week diet intervention:
|
After the 24-week period: LCD: ↓ IL-6, resistin, leptin, glucose, insulin, cholesterol, TG, ↑ HDL LFD: ↓ TNF-α, LDL, HOMA-IR, ↑ adiponectin |
Asle Mohammadi Zadeh et al. (2018) |
| Low-carbohydrate versus low-fat diet | Randomised controlled trial | 51 T2DM patients | 6-month diet intervention:
|
LCD: ↓ sICAM, E-selectin LFD: ↓ CRP |
Davis et al. (2011) |
| Low-carbohydrate versus low-fat diet | Randomised controlled trial | 51 T2DM patients | 6-month diet intervention:
|
LCD: ↓ IL-1Ra, IL-6 | Johansson-Persson et al. (2014) |
| Low-carbohydrate versus low-fat diet | Clinical trial | 148 obese adults (no diabetes and CVD) | 12-month diet intervention:
|
LCD: ↑ adiponectin ↓ICAM | Hu et al. (2015) |
| Low-carbohydrate + nuts | Randomised controlled trial | 51 T2DM patients | 3-month diet intervention:
|
Improved glycaemic profile versus baseline, no difference between groups regarding IL-5 serum levels | Hou et al. (2018) |
| Low-Calorie, Low-Carbohydrate Soy Diet | Parallel randomized clinical trial | 45 patients with NAFLD | 8-week diet intervention:
|
LCS: ↓ glycaemic indices, CRP | Kani et al. (2017) |
| Switching to an isocaloric ketogenic diet (KD) | Clinical study | 17 men (BMI: 25–35 kg/m2) | Transitioning from a normal diet (4 weeks–35% fat, 15% protein, 50% carbohydrate) to 4 weeks of an isocaloric KD (80% fat, 5% carbohydrate, 15% protein) | KD: ↑glycerol, free fatty acids, glucagon, adiponectin, gastric inhibitory peptide, TC, LDL, CRP ↓Fasting insulin, C-peptide, triglycerides and fibroblast growth factor 21 |
Rosenbaum et al. (2019) |
| Carbohydrate-restricted Paleolithic-based diet | Randomized crossover trial | 12 subjects with metabolic syndrome | 4-week diet intervention:
|
PD-S + PD-Ex: ↓ Glycaemia, TG, fasting insulin, insulin resistance, CRP, TNF-α, IL-6, ICAM-1 | Gyorkos et al. (2019) |
| Low carbohydrate high fat, diet | Randomised controlled trial | 55 obese subjects | 12-week diet intervention:
|
HFLC: ↓ CRP,TG ↑ adiponectin, HDL | Ruth et al. (2013) |
| Nutritional ketosis | Randomised controlled trial | 262 patients with T2DM | 12-month diet intervention:
|
↓ CRP | Bhanpuri et al. (2018) |
| Moderate-carbohydrate versus low-fat diet | Randomised controlled trial | 122 overweight and obese adults | 6-month diet intervention:
|
LGI vs LF: ↓ fasting insulin, ↑ HOMA No significant differences among groups regarding lipid profiles, inflammatory and metabolic risk markers (IL-6, MCP-1, Leptin, ICAM-1). |
Juanola-Falgarona et al. (2014) |
| Low-glycemic-index diet | Randomised controlled trial | 90 subjects | 12-week diet intervention:
|
LGI + FF vs. control: ↓CRP, TNF-α LGI + FF vs. LGI: ↑ adiponectin |
Izadi et al. (2018) |
| Low glycaemic index diet | Randomised controlled trial | 50 obese and overweight adolescent girls | 10-week diet intervention:
|
↓ IL-6, CRP | Rouhani et al. (2016) |
| Low- carbohydrate high-fat diet versus higher-complex carbohydrate lower-fat | Randomized controlled feeding study | 12 overweight and obese women with gestational (31 weeks) diabetes mellitus | 31-week diet intervention:
|
CHOICE: ↓ expression of proinflammatory genes (IL-1β, TNF- α) | Hernandez et al. (2016) |
| Regular diet | Observational study | 95 postmenopausal women | Participants classified according to CRP - lower or ≥3 mg/L. Sedentary lifestyle was described by walking ≤6000 steps/day; diet was evaluated using a validated food frequency questionnaire. | CRP was higher for women with sedentary lifestyle and higher glycaemic load | Alves et al. (2016) |
| Low-fructose diet | Comparative study | 28 patients with chronic kidney disease | 6-week of low-fructose diet (LFD), followed by 6 weeks of regular diet | ↓ insulin, CRP sICAM (decrease of insulin and sICAM persistent, while CRP did not when resuming regular diet) | Brymora et al. (2012) |
ICAM – intercellular adhesion molecule-1; HOMA – homeostatic model assessment of β cell function; MCP-1 – Monocyte chemotactic protein-1.
So, adding high-fiber and exercise to a low-index carbohydrate diet has beneficial effects on inflammatory profile of T2DM and obese patients while low-carb and low-fat diets induce the same type of effects on cardiovascular risk markers of diabetes patients.
5. Mediterranean diet and the impact on inflammation
The Mediterranean diet (MD) is based on the dietary pattern found in the Mediterranean basin (Greece, southern regions of Italy and Spain), and includes high amounts of fresh vegetables and fruits, seeds, nuts, along with olive oil and whole grain cereals. Milk, cheese, yogurt, eggs, fish and poultry are consumed in moderate amounts, as is wine (especially red), with low amounts of red meat and sugary deserts (Martinez-Gonzalez et al., 2014; Tosti et al., 2018). This diet is abundant in minerals and vitamins, antioxidants and phytochemicals (Tosti et al., 2018). Although several of its components exerted beneficial actions, most likely their combined synergistic effects contribute to reducing the systemic inflammatory burden (Tosti et al., 2018). Some authors posit that MD exerts a hormetic effect, similar to caloric restriction, highlighting the Nrf2 pathway, regulating the pro-/anti-inflammatory processes equilibrium (Martucci et al., 2017). Epigenetic regulation was also hypothesized, especially due to components found in nuts and extra virgin olive oil, which were reported to alter the methylation of some genes related to inflammation, metabolism and signal transduction (Arpon et al., 2016, 2017).
In healthy subjects, even one MD-style meal was shown to reduce the expression of pro-inflammatory molecules (De Lorenzo et al., 2017), with no differences between sexes regarding effects on systemic inflammatory status (Bedard et al., 2015). In elderly individuals, a MD intervention lead to lower glycoxidative impairment (Lopez-Moreno et al., 2018) and inflammatory response (Camargo et al., 2012; Yubero-Serrano et al., 2012), paralleled to a diet based on saturated fatty acids (Fig. 2 ).
Fig. 2.
Diets rich in proteins, lipids and carbohydrates induce the production of pro-inflammatory molecules that lead to the activation of several inflammatory pathways including JAK/STAT pathway, NF-Kβ pathway and MAPK kinase cascade. These pathways lead to oxidative stress, as wells as, COX-2, TNF-α, and interleukins production via transcriptional regulation ultimately leading to chronic inflammation. Oxidative stress either directly or via metabolic dysfunctions causing e.g insulin resistance, as well as the rest of the inflammatory molecules as a result of unhealthy diet promote the onset of several chronic diseases including CVD, neurodegenerative diseases, autoimmunity, pulmonary diseases and are-related frailty; (NF-kβ – nuclear factor kappa-light-chain-enhancer of activated B cells heterodimer, consisting of p50, p65 and IkBα proteins; STAT3 – Signal transducer and activator of transcription 3; ERK/MAPK – mitogen-activated protein kinases; JNK – c-Jun N-terminal kinases; COX-2 – cyclooxygenase 2; TNF-α – Tumour necrosis factor alpha; IL-1/6/8 – interleukin 1/6/8).
A marked reduction of inflammatory molecules (C reactive protein – CRP, E-selectin, P-selectin, TNF-α, IL-1β, IL-6) and of mRNAs of pro-inflammatory genes was reported in overweight and obese individuals which adhered a classic or modified MD (Bekkouche et al., 2014; Marques-Rocha et al., 2016; Paoli et al., 2015; Rallidis et al., 2017; Tripp et al., 2019). Furthermore, in diabetics and patients with high cardiovascular risk, MD determined a significant reduction of serum levels of CRP, interleukins and adhesion molecules (Casas et al., 2014; Ceriello et al., 2014; Maiorino et al., 2016; Mayr et al., 2018). In a group of asthmatic children, MD supplemented with 150g cooked fish twice a week resulted in significantly improved pulmonary function and markedly increased docosahexaenoic acid (DHA) levels and improved omega-6 to omega-3 ratio (Papamichael et al., 2019). The recent clinical trials addressing the relationship between MD and inflammation are summarized in Table 4 .
Table 4.
Recent reports concerning Mediterranean diet and inflammation.
| Design | Population | Intervention | Effects | Reference |
|---|---|---|---|---|
| Feeding study | 25 subjects | One-meal intervention:
|
↓ expression of inflammation-related genes | De Lorenzo et al. (2017) |
| Controlled feeding study | 35 men and 27 women |
|
MD induced the same type of response regarding hs-CRP both in males and females | Bedard et al. (2015) |
| Randomized Controlled Trial | 1142 subjects | 12-month diet intervention:
|
Slowed the decline of bone mineral density only in the femoral neck in subjects with osteoporosis | Jennings et al. (2018) |
| Randomized Controlled Trial | 20 elderly subjects | 4-week diet intervention:
|
MD, MD-Q10: ↓ expression of p65, IKK-b, MMP-9, IL-1b (versus SFAD) MD-Q: marked decrease of P65 and IKK-b (versus the other diets) |
Yubero-Serrano et al. (2012) |
| Randomized Controlled Trial | 20 elderly people | 4-week diet intervention:
|
MD-O: ↓ expression of inflammation-related genes (versus SFAD: p65, MCP-1; versus LFHC-PUFA: p65, TNF-α) | Camargo et al. (2012) |
| Randomized Controlled Crossover Trial | 20 elderly subjects | isocaloric diets for successive periods of 4 weeks in a crossover design: MD, MD + CoQ, Western diet | ↓ AGE, RAGE | Lopez-Moreno et al. (2018) |
| Randomized Controlled Trial | 34 male overweight subjects | 4-week diet intervention:
|
KMD: ↓ TNF-α KMD-O3: ↓ IL-1β, IL-6, TNF-α, ↑ adiponectin |
Paoli et al. (2015) |
| Controlled feeding study | 50 overweight and obese subjects | 13-week diet intervention: Caloric restriction, MD + dietary supplementation | ↓ CRP (versus baseline) | Tripp et al. (2019) |
| Clinical Trial | 90 subjects with abdominal obesity | 2-month diet intervention:
|
MD: ↓ CRP, P-selectin, E-selectin (versus baseline) | Rallidis et al. (2017) |
| Clinical Trial | 40 subjects with metabolic syndrome | 8-week diet hypocaloric MD intervention | ↓ mRNA associated with the regulation of inflammatory genes | Marques-Rocha et al. (2016) |
| Randomized Controlled Trial | 36 subjects with metabolic syndrome | 3-month MD intervention | ↓ CRP, insulin | Bekkouche et al. (2014) |
| Randomized Controlled Trial | 24 T2DM patients | 3-month diet intervention:
|
MD: ↓ IL-6, ICAM-1, ↑ GLP-1 stimulated insulin secretion | Ceriello et al. (2014) |
| Randomized Controlled Trial | 215 T2DM (newly diagnosed) | 12-month diet intervention:
|
MD: ↓ CRP (37%), ↑ adiponectin (43%) | Maiorino et al. (2016) |
| Randomized Controlled Trial | 56 coronary heart disease patients | 6-month diet intervention:
|
↓ dietary inflammatory index (including IL-1b, IL-4, IL-6, IL-10, TNF-α, CRP) | Mayr et al. (2018) |
| Randomized Controlled Trial | 164 subjects with high cardiovascular risk | 12-month diet intervention:
|
MD-O: ↓ CRP (45%), IL-6 (35%), sICAM-1 (50%), P-selectin (27%) MD-N: ↓ CRP (45%), IL-6 (35%) (versus LFD) |
Casas et al. (2014) |
In recent years, the effects of a diet similar to MD started to be investigated: the Nordic diet (ND). Similarly, ND is based on fruits, especially berries, and vegetables, fish, whole grains, and includes low amounts of processed red meat and is almost lacking saturated fats. As olive oil is specific for the Mediterranean basin, the ND includes canola oil (Lankinen et al., 2019; Magnusdottir et al., 2017). Literature reports are reviewed elsewhere (Lankinen et al., 2019) and although scarce, they indicated that ND exerted anti-inflammatory effects, as it was able to reduce the serum levels of CRP (de Mello et al., 2011; Lankinen et al., 2019).
Dietary interventions based on Mediterranean/Nordic style induce positive effects on both inflammation and redox stress, both in healthy patients and in those with metabolic impairments (diabetes mellitus, obesity, metabolic syndrome). The hormetic effects induced at the level of the immune system is pointed out by the positive results induced by MD on people with inflammatory phenomena impacting the respiratory system, including children with asthma.
6. Polyunsaturated fatty acids in the inflammation hallmark
Literature data mentions two main groups of polyunsaturated fatty acids (PUFAs), of plant or animal origin: omega-3 (n-3) and omega-6 (n-6). The most discussed molecules of each group are α-linolenic acid (ALA) and linoleic acid (LA), respectively. Functionally, notable among the omega-3 fatty acids are the eicosapentaenoic acid (EPA) and the docosahexaenoic acid (DHA) (Calder, 2015), although docosapentaenoic acid (DPA) is materializing as an important member of the n-3 family (Kaur et al., 2011). In human diets, the two essential PUFAs, LA, and ALA are usually derived from plant sources (such as seeds, nuts, seed oils and derived products), as only plants synthesize them (Calder, 2011). Linseeds and their oil habitually contain 45–55% of n-3 PUFAs, mainly ALA, whereas soybean or rapeseed oil, and walnuts only about 10% ALA (Kris-Etherton et al., 2002).
Another important food source of n-3 PUFAs are fatty fish and also other seafood or derived products, known as “fish oils”. All these products contain significant quantities of DPA, EPA and DHA, as a result of plankton and algae consumption and not as a result of endogenous synthesis (Poudyal et al., 2011). Noteworthy, the dominant PUFAs in fish, as well as fish oils, vary between species. For instance, cod liver oil contains more EPA than DHA, whereas tuna oil has a higher content of DHA (Calder, 2012). One portion of fish could bring into diet between 200 and 300 mg n-3 PUFAs, while 1 g of fish oil contains almost 30% EPA and DHA, highlighting the importance of diets including seafood. In the absence of fish or derived products, the daily intake of n-3 PUFAs in most adults is below 200 mg/day (Meyer et al., 2003). As plants produce much more LA than ALA, the former is the most customary PUFA in Western diets (Blasbalg et al., 2011). The daily dietary intake of ALA is 0.5–2 g, while of LA greatly increased in the last 50–60 years, along with a significant change of n-6/n-3 ratio (Calder, 2017), reaching as high as 20 in some Western-type diets (Calder, 2011).
LA and ALA share a common metabolic pathway in animals and humans (Poudyal et al., 2011). LA is metabolised by Δ6-desaturase to γ-linolenic acid (GLA), and later by elongase and Δ5-desaturase to arachidonic acid (ARA), while ALA is converted by the same enzymes into EPA, subsequently to DPA then, finally, to DHA. The rate of transformation from ALA to EPA and later to DHA is affected by several factors such as age, sex, or genetics (Baker et al., 2016). In addition, levels of ALA, LA and DHA are affected by chronic diseases as shown in a study comparing lipid levels between patients with autoimmune diseases and healthy controls (Tsoukalas et al., 2019b).
The conversion of dihomo-gamma-linolenic acid (DGLA) to ARA is regulated by insulin and ARA/EPA ratio is a sensitive marker for insulin resistance, a common denominator of most chronic inflammatory diseases. In a study of healthy adult volunteers AA to EPA ratio and the ARA precursor – DGLA, significantly changed with age (Tsoukalas et al., 2019a). The metabolism of n-6 PUFAs is more prevalent compared with n-3 PUFA, due to the fact that LA is much more common in actual diets (Blasbalg et al., 2011), although ALA, and not LA, is the preferred substrate for Δ6-desaturase (Calder, 2015).
Noteworthy, LA, ARA, EPA and DHA are important constituents of membrane phospholipids and have important roles in membrane function, which greatly influences cell activity (Burdge and Calder, 2015). The proportion of PUFAs found in the membrane is dependent on cell type, dietary intake and metabolism (Calder, 2017). For example, in healthy subjects receiving a typical Western diet, the percentages of DHA, EPA, and ARA, in mononuclear cells were 2.5, 0.5 and, respectively, 20% of total fatty acids (Calder, 2011).
The effects exerted by n-3 PUFAs are arbitrated either by the fatty acid molecules or by their bioactive metabolites from one of the three categories: protectins, resolvins, and maresins. The E-resolvins (such as E1, E2, and E3), are produced from EPA, while the D-series resolvins including D1, D2, D3, D4 and D5, neuroprotectins/protectins (NPD1/PD1), and the maresins (MaR1), are biosynthesized from DHA (Dalli et al., 2013; Serhan and Petasis, 2011). The biotransformation of n-3 PUFAs involves the COX and LOX pathways. S-resolvins, S-protectins, and S-maresins are produced from DHA and EPA via LOX pathway, while R-resolvins and R-protectins are derived from aspirin-activated COX-2 or cytochrome P450 metabolic transformation of DHA and EPA (Calder, 2015). In most cell types, ARA is highly predominant and exhibits direct links to inflammatory pathways, since it constitutes the substrate for enzymes such as cytochrome P450, cyclooxygenase or lipoxygenase, yielding mediators from the eicosanoid family. Indeed, the synthesis of pro-resolving mediators is increased when the diet is rich in n-3 PUFAs. Thus, in healthy subjects, a daily supplement for 3 weeks of 1 g DHA and 1.5 g EPA, quantified measurable levels of resolvins D1, D2, and 17-R resolvin D1 (>25 pg/ml plasma) (Mas et al., 2012). In obese women treated for 3 months with a daily supplement of 1.8 g EPA and DHA, DHA-derived pro-resolvins mediators were measured and found to be increased (RvD1 and RvD2 > 60 pg/ml plasma) (Polus et al., 2016).
6.1. Inflammatory-resolving effects induced by PUFAs
Nowadays, the mechanisms of action by which n-3 PUFAs regulate the inflammatory processes are widely investigated. The suppression of inflammation by n-3 PUFAs is associated with one of the following mechanisms (1) competitive inhibition of n-6 PUFA pathway; (2) modification of cell membrane composition; (3) affecting the formation of rafts or (4) direct anti-inflammatory effect of their bioactive metabolites (resolvins, protectins, and maresins) (Poudyal et al., 2011).
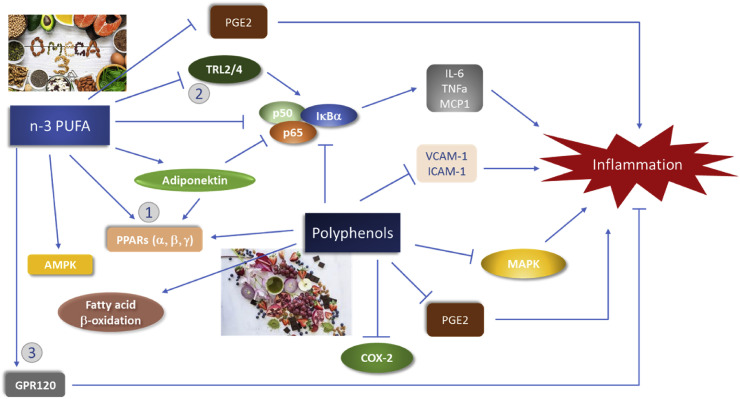
It has been demonstrated that the dietary supplementation with DHA and EPA from fish increases in a dose-response manner the content of DHA and EPA in the cell inflammation-responsible phospholipids (Calder, 2017); increased content of DHA or EPA in different tissues, such as adipose tissue or heart was also observed in correlation with their intake (Calder, 2015) (Fig. 3 ).
Fig. 3.
The effect of omega-3 fatty acids and polyphenols in the regulation of the inflammatory response. Omega-3 fatty acids inhibit the inflammatory response by inhibiting PGE2 which promotes inflammation and NF-κB either directly, via the interaction with the transcriptional factors PPARs, or by inhibiting TLR2/4 which normally activates NF-κB. Moreover, omega-3 fatty acids regulate inflammation by activating MAPK and GPR120 which in turn inhibits inflammation. Polyphenols inhibit the inflammatory response by directly inhibiting NF-κB, or via the PPARs. They also promote fatty acid b-oxidation and inhibit VCAM-1, ICAM-1, MAPK pathway, PGE2 and COX-2 that all promote chronic inflammation (PGE2 –prostaglandin 2; NF-κB – nuclear factor kappa-light-chain-enhancer of activated B cells; PPARs – peroxisome proliferator-activated receptors; TLR2/4– toll-like receptor; MAPK – mitogen-activated protein kinase; GPR120 – G-protein coupled receptor 120; VCAM-1 – vascular cell adhesion molecule 1; ICAM-1 – intracellular cell adhesion molecule 1; COX-2 – cyclooxygenase 2; TNF-α – tumour necrosis factor alpha; MCP-1 – monocyte chemoattractant protein 1; AMPK – AMP kinase).
These n-3 PUFAs frequently substitute n-6 PUFAs like ARA, resulting in decreased availability of ARA for eicosanoid synthesis. EPA also inhibits ARA metabolism as a competitive substrate for COX-2, decreasing prostaglandin E2 (PGE2) production. In rats, dietary supplementation with ALA inhibits PG biosynthesis from ARA, while equivalent quantities of ALA and LA decreased up to 40% n-6 PUFAs incorporation in phospholipids (Calder, 2017). Furthermore, Rees et al. observed that a daily EPA intake of 2.7 g or 4.05 g for 3 months decreases the PGE2 production by lipopolysaccharide-stimulated mononuclear cells, while a lower dose of 1.35 g did not. EPA was integrated in a linear dose-dependent manner into mononuclear cell phospholipids and plasma. This study suggested a daily threshold in the range of 1.35–2.7 g EPA for the anti-inflammatory action (Rees et al., 2006).
Besides decreasing production of PGE2, DHA and EPA are also substrates for the biosynthesis of lipid derivatives, but the EPA-derived mediators as series-3 prostaglandins (PGD3) or series-5 leukotrienes are typically less biologically potent, having a lower ability to interact with relevant eicosanoid receptors (Calder, 2015). For example, EPA-derived leukotriene B5 (LTB5) is almost 100 times less active as a leukocyte chemoattractant than ARA-derived LTB4 (Calder, 2017). However, in some cases, EPA-derived mediators have similar potency with ARA-derived mediators. It appears that EPA-derived PGD3 inhibits the effect of the ARA-derived PGD2, due to a stronger interaction with the DP1 receptor compared to PGD2 (Wada et al., 2007). In other cases, EPA-derived mediators exhibited a similar magnitude of effect (e.g. inhibition of TNF-α production by blood monocytes) (Dooper et al., 2002).
6.2. Molecular targets of PUFAs
There are several pharmacological studies suggesting molecular targets for the anti-inflammatory effects of n-3 PUFAs and their metabolites: PPAR-γ, GPR120, CMKLR1 (known as ChemR23), BLT1(leukotriene B4 receptor 1), GPR32 and ALX/FPR2 (Im, 2012). Thus, resolvins E1 and D1 exhibited a higher affinity for these receptors compared to EPA or DHA. Chem R23 and BLT1 are receptors of resolvin E1, while GPR32 and ALX/FPR2, bind to lipoxin A4 and resolvin D1 with high affinity. GPR120 was reported to be a receptor of EPA and DHA (EC50 ~ 1–10 μM), while ALX/FPR2 to annexin I and lipoxin A4 (Serhan and Petasis, 2011). Furthermore, some studies on GPR120 KO mice suggest that n-3 PUFAs that activate GPR120, interact with β-arrestin 2, and suppress NF-κB activation and macrophage-mediated inflammatory responses (Oh et al., 2010). However, it is important to highlight that the in vivo anti-inflammatory effects of n-3 PUFAs in humans are minor and might only occur at high n-3 PUFA levels, it was demonstrated in vitro that BSA-conjugated n-3 PUFA are incapable of activating GPR120 (Im, 2012).
DHA and EPA are weaker agonists of PPAR-γ (EC50 ~ 10–100 μM), while their oxidized metabolites (such as protectin D1) are much more potent (Yamamoto et al., 2005). Also, ALA or ARA has a similar potency to DHA or EPA for on PPAR-γ, and higher for PPAR-α (Calder, 2015). As PPAR-γ activation reduces inflammatory responses, via the NF-κB pathway, this mechanism could partially explain the anti-inflammatory effects of n-3 PUFAs. Furthermore, n-3 PUFAs were reported to suppress NF-κB activation in a PPAR-γ-independent manner by binding to TLR-4 under certain conditions (Im, 2012). Taking into account all these reports, it looks like three mechanisms are employed by n-3 PUFAs to suppress inflammatory signalling via NF-κB: (1) preventing NF-κB nuclear translocation via PPAR-γ activation, (2) interfering with membrane activation of NF-κB via TLR4 and (3) interaction with GPR120 initiating an anti-inflammatory signalling cascade (Calder, 2015).
Resolvin D1 is a potent agonist to GPR32 and ALX/FPR2 (EC50 = 8.8 pM and 1.2 pM), while Resolvin E1 strongly binds to Chem R23 (Kd = 4.5 nM), reducing IL-12 production (Krishnamoorthy et al., 2010) and is a partial agonist to BLT1, so it induces NF-κB activation via BLT1, inhibiting neutrophil migration (Arita et al., 2007). For the other resolvins, protectins or maresins, the molecular targets are not yet identified.
Isolated n-3 PUFAs and their bioactive mediators were extensively examined in animal models of colitis or arthritis or using specific transgenic models. n-3 PUFAs and RvD1, RvD5, PD1 and MaR1 administration proved effective in animal models of colitis, decreasing inflammation and chemically induced colonic damage. The beneficial effects are, in all cases, correlated with the reduction of ARA-derived mediators in the colonic mucosa (Bosco et al., 2013; Charpentier et al., 2018; Gobbetti et al., 2017; Marcon et al., 2013). Surprisingly, aspirin-triggered resolvin D1 (AT-RvD1) displayed a stronger anti-inflammatory effect than RvD2 in experimental colitis, through lipoxin A4 receptor (ALX) activation (Bento et al., 2011). Furthermore, n-3 PUFAs as fish oil has shown not just anti-inflammatory effects in peripheral tissues, but several beneficial effects in obesity-induced animal models, such as improved lipid profile, decreased hepatic steatosis and insulin resistance (Bargut et al., 2015; Pimentel et al., 2013). Indeed, beneficial effects of DHA and EPA in adipose tissue were reported in mice fed a high-fructose diet, including modulating pro- and anti-inflammatory markers and ameliorating adipocyte abnormalities. The effects were significantly higher for DHA compared to EPA (Bargut et al., 2017).
Additionally to anti-inflammatory effects, correlated with down-regulation of IL-6 and TNF-α expression in liver, n-3 PUFAs also exhibited triglyceridemia lowering effects in diabetic rats via modulation of PPAR-α (Devarshi et al., 2013; Ghadge et al., 2016). Additionally, Lee et al. demonstrated that a diet with a high n-6/n-3 PUFAs ratio (~9) induced dysbacteriosis of the gut microbiota in obesity-induced T2DM or high-fat-diet treated rats, while a low ratio (~3) enhanced blood glucose homeostasis (Lee et al., 2019). The outcomes of the most recent animal studies are summarized in Table 5 .
Table 5.
Mittigating inflammation in animal model studies – effects of PUFAs.
| Tested compound(s) | Animal model | Main anti-inflammatory findings | References |
|---|---|---|---|
| n-3 PUFA (fish oil or mix fish and olive oil or flaxseed oil) | TNBS colitis | ↓IL-1β; IL-12p70; ↓IL-6; ↓TNFα; ↑PGE3,↑ TXB3; ↑ LTB5 | Bosco et al. (2013) |
| TNBS colitis | ↓colon iNOS, ↓COX-2 expression, ↓IL-6, ↓LTB4, ↓TNFα production | Charpentier et al. (2018) | |
| DSS colitis | ↓TNF-α; ↓ COX-2; ↑anti-inflammatory PG; | Sharma et al. (2019) | |
| Carrageenan induced inflammation | ↓TNF-α; ↓ IL-6 | Zadeh-Ardabili and Rad (2019) | |
| STZ- diabetic rats | ↑ gene expression PPRγ; ↓ NF-κB activity | Ghadge et al. (2016) | |
| STZ- diabetic rats | ↓TNF-α; ↓ IL-6 | Lee et al. (2019) | |
| STZ-NIC diabetic rats | ↑ PPAR-α only by flaxseed oil; both (flaxseed oil and fish oil):↑ D5 and D6 desaturases; ↓TNF-α; ↓ IL-6; | Devarshi et al. (2013) | |
| STZ-NIC diabetic rats | ↑ renal SOD-1; ↑ GPx-1 expression; ↑ CAT; ↓ renal AGEs formation ↓AGE protein expression; ↓ IL-6; ↓ NF-κB expression | Jangale et al. (2016) | |
| STZ-NIC diabetic rats | ↓ IL-1β; ↓TNFα; ↓IL-6; ↓IL-17 A; ↓MDA | Zhu et al. (2020) | |
| Wistar rats | ↓ IL-6; ↓ TNF-α; ↓IL- 10 receptor | Pimentel et al. (2013) | |
| C57BL/6 mice | ↓ NF-κB expression; ↓ IL-6; ↓ TNF-α | Bargut et al. (2015) | |
| EPA monogliceride | DSS colitis | ↓PMN infiltration; ↓ NF-κB activity; ↓IL-1β; ↓TNF-α; ↓ IL-6; ↓expression of COX2 in colon | Morin et al. (2016) |
| ALA | TNBS colitis | ↓ IP-8, ↓ LTB4, ↓ colon NF-κB DNA binding activity | Hassan et al. (2010) |
| EPA vs. DHA | high-fructose fed C57BL/6J mice | ↓ TNF-alpha and IL-6 gene expressions; ↓MCP-1 pERK and NFkB protein expressions | Bargut et al. (2017) |
| EPA free fatty acid | APCMin/+ FAP model | ↓ COX-2 expression; ↑ EPA tissue uptake; ↓ lipid peroxidation | Fini et al. (2010) |
| CAC model C57BL/6J mouse | ↓PGE2; ↑ EPA tissue uptake | Piazzi et al. (2014) | |
| Endogenous conversion n-6 into n-3 PUFA | CAC model Fat-1 mouse |
↓ COX-2 expression; ↓ NF-κB activity; ↓PGE2 | Han et al. (2016) |
| Chronic arthritis Fat-1 mouse vs WT mouse |
↓ IL-17; ↑mRNA expression of Foxp3 (in Fat-1 mouse) | Kim et al. (2018) | |
| AT-RvD1 | DSS colitis/TNBS colitis | ↓PMN infiltration; ↓ NF-κB activity and mRNA expression; ↓IL-1β; ↓MIP-2; ↓mRNA expression of VCAM-1, ICAM-1 | Bento et al. (2011) |
| Adjuvant-induced arthritis | ↓TNF-α; IL-1β | Lima-Garcia et al. (2011) | |
| RvD2 | DSS colitis | ↓IL-1β; ↓ murine KC (IL-8 human homolog) | Campbell et al. (2010) |
| TNBS colitis | ↓PMN infiltration; ↓ NF-κB activity and mRNA expression; ↓IL-1β; ↓MIP-2; ↓mRNA expression of VCAM-1, ICAM-1 | Bento et al. (2011) | |
| RvE1 | DSS colitis | ↓PMN infiltration; ↓TNF-α; ↓mRNA expression of IL-6, TNFα, IL-1β | Ishida et al. (2010) |
| Collagen-induced arthritis | No statistical significant effect on TNF-α | de Molon et al. (2019) | |
| RvD5 | DSS colitis | ↓PMN infiltration; ↓TNF-α; ↓ IL-6; ↓IL-1β; | Gobbetti et al. (2017) |
| MaR1 | DSS colitis/TNBS colitis | ↓PMN infiltration; ↓ NF-κB activity; ↓IL-1β; ↓TNF-α; ↓ IL-6; ↓mRNA expression of ICAM-1 | Marcon et al. (2013) |
| PD1 | DSS colitis | ↓PMN infiltration; ↓IL-1β only partially | Gobbetti et al. (2017) |
CAC – colitis associated cancer; CAT – catalase DSS – dextran sulfate sodium; GPx – glutathione peroxidase NIC – Nicotinamide; PD – protectin; SOD – superoxide dismutase; STZ – Streptozotocin; TNBS – trinitrobenzene sulphonic acid; EPA – Eicosapentaenoic Acid; DHA – Docosahexaenoic Acid; TNF – α-Tumour Necrosis Factor alpha; LTB – Leukotriene, PPAR – peroxisome proliferator-activated receptor; COX – cyclooxygenase; AGE – advanced glycation end products; TXB – Thromboxane; PG – prostaglandins; ICAM – Intercellular Adhesion Molecule; VCAM – Vascular Cell Adhesion molecule; IL – Interleukin; NF-κB, nuclear factor kappa B; PMN – polymorphonuclear leukocyte; MIP-2 –macrophage inflammatory protein 2; IP-8 – Isoprostane-8; Foxp3 – Forkhead box P3; pERK – protein kinase RNA-like endoplasmic reticulum kinase; MCP-1 – Monocyte chemoattractant protein-1; murine KC – murine chemokine.
6.3. n-3 PUFAs effects in humans
In healthy subjects, different daily doses of EPA and DHA up 1800 mg, administered up to 5 months, showed no significant effects on the CPR, IL-6, and TNF-α (Asztalos et al., 2016; Flock et al., 2014; Muldoon et al., 2016). A comparable conclusion was drawn by other authors. According to Rangel-Huerta's meta-analysis, consumption of 900 mg–2000 mg n-3 PUFAs does not change inflammatory biomarkers in healthy subjects (Rangel-Huerta et al., 2012). On the other hand, doses between 1250 and 2400 mg n-3 PUFA for 4 months lowered inflammation in sedentary and overweight middle-aged and older adults (Kiecolt-Glaser et al., 2012). Lp-PLA2, another anti-inflammatory marker was significantly reduced by a high dose of EPA (1800 mg) but not by DHA (Asztalos et al., 2016). Interestingly, only DHA modified the lipid profile by decreasing postprandial triglyceride concentrations and significantly increasing low-density lipoprotein cholesterol, with no significant changes in inflammatory biomarkers (Asztalos et al., 2016). In elderly subjects, daily supplementation with 2500 mg EPA and DHA, for 8 weeks, significantly reduced the plasma levels of fatty acids, IL-1β, IL-6, and TNF-α (Tan et al., 2018). Similarly, in obese patients who received different doses of combined n-3 PUFAs (380–1290 mg DHA and 360–460 mg EPA) for 2–3 months, the intervention reduced the expression of proinflammatory genes in adipocytes and systemic inflammatory markers sVCAM-1, CRP, IL-6, and TNF-α (Itariu et al., 2012; Polus et al., 2016). Furthermore, other relevant metabolic findings connected with n-3 PUFA treatment were reported, such as decreasing fasting triglycerides and insulin (Allaire et al., 2016; Polus et al., 2016) or decreasing fasting blood glucose in obese diabetics (Ellulu et al., 2016). Partially, these results are in line with the modest reduction in waist circumference and body-weight found in a meta-analysis (Bender et al., 2014). The authors indicated that the effect regarding waist circumference produced by fish intake or fish oil supplementation and might be greater in men than in women. The beneficial effect in overweight and obese adults concerning waist circumference and triglyceridemia was confirmed by two other meta-analyses (Du et al., 2015; Zhang et al., 2017).
As most of the cited trials utilize a mixture of DHA and EPA which may mask the effects of each compound, the individual effects of DHA or EPA in obese patients were also investigated, but the results were inconclusive. A significant reduction in serum IL-18 and adiponectin with DHA than with EPA was observed in one study (Allaire et al., 2016), while no differences between DHA and EPA in the expression of pro-inflammatory genes were observed in another study (Vors et al., 2017).
In patients with impaired glucose metabolism and T2DM in almost all studies, none of the combined EPA and DHA doses had any effect on IL-6, IL-1β, CRP, VCAM, and sICAM (Clark et al., 2016; Mocking et al., 2012; Sawada et al., 2016). Further, no effects on glycated haemoglobin (HbA1c) (Sawada et al., 2016; Wong et al., 2010), insulin (Clark et al., 2016) or lipid profile (Veleba et al., 2015) were found. Only Veleba et al. (2015), observed that HbA1c decreased significantly, and fasting blood glucose increased after n-3 PUFAs treatment for 24 weeks, but no other key findings. An overview of the most recent human studies where the inflammatory biomarkers as a result of PUFAs treatments, were assessed as the main outcome, is summarized in Table 6 .
Table 6.
Clinical effects induced by PUFAs.
| Intervention | (n) | Main anti-inflammatory findings | Other relevant findings | References |
|---|---|---|---|---|
| Healthy subjects | ||||
4-month intervention:
|
138 | ↓TNF-α and ↓ IL-6 for both low and high dose groups | ↓ n-6:n-3 ratio for both low and high dose groups | Kiecolt-Glaser et al. (2012) |
6-week intervention:
|
121 | No effect on hsCRP, TNF-α, IL-6, VCAM-1, ICAM-1 and fibrinogen | Only High dose EPA ↓ Lp-PLA2; DHA: ↓ TG; ↑ LDL No effect of low dose EPA |
Asztalos et al. (2016) |
| 18-week intervention:1000 mg EPA + 400 mg DHA/day vs. placebo | 261 | No effect on serum CRP and IL-6 | – | Muldoon et al. (2016) |
5-month intervention:
|
125 | No significant effect on IL-6 or CPR; Marginal effect on TNF-α observed at the highest dose (1800 mg) |
Higher RBC DHA was associated with lower TNF-α concentrations. | Flock et al. (2014) |
| 8-week intervention:2500 mg EPA + DHA/day vs. placebo | 35 | ↓IL-6, IL-1β and TNFα | – | Tan et al. (2018) |
| Obese patients | ||||
2-month intervention:
|
55 | ↓IL-6 ↓ inflammatory gene expression in adipose tissue ↑release of anti-inflammatory eicosanoids in adipose tissue |
↓TG | Itariu et al. (2012) |
| 3-month intervention: 360 mg EPA and 1290 mg DHA/day vs. placebo | 59 | ↓ VCAM-1; ↓ PECAM-1; ↓ hsCRP No effect on IL-6 | ↓ TG; ↓insulin. No effect on TC, HDL, LDL, NEFA, FBG |
Polus et al. (2016) |
10-week intervention:
|
154 | ↓ IL-18 and ↑ adiponectin (DHA > EPA) No difference between EPA and DHA regarding effect on CRP, IL-6, TNFα |
↓ TG; ↑ HDL (DHA > EPA) ↑ LDL by DHA only in men |
Allaire et al. (2016) |
10-week intervention:
|
154 | EPA: ↑TRAF3 and PPARα expression DHA: ↑ PPARα and TNFα expression both ↓CD14 expression |
No significant difference between EPA and DHA. | Vors et al. (2017) |
12-week intervention:
|
29 | LSM & n-3 PUFA ↑ adiponectin in comparison to LSM No effect on IL6 |
No effect on leptin, LIF, follistatin, BDNF, and fasting triacylglycerol | Sedláček et al. (2018) |
| Hypertensive and/or diabetic obese patients | ||||
| 8-week intervention:300 mg EPA + 200 mg DHA/day vs. control | 64 | ↓CRP | ↓ FBG; ↓TG | Ellulu et al. (2016) |
| Impaired glucose metabolism patients | ||||
| 6-month intervention:1800 mg EPA/day vs. placebo | 107 | ↓ CRP but similar effects in placebo | ↑ HDL and ↓fasting TG; No effect on HbA1c and FBG | Sawada et al. (2016) |
| 9-month intervention:2388 mg EPA +1530 mg DHA/day vs placebo | 36 | No effect in IL-1B, IL-6, hsCRP, ICAM and VCAM | No effect on FBG, insulin, HOMA-IR. | Clark et al. (2016) |
| Type 2 diabetes mellitus | ||||
| 12-week intervention: 4000 mg (42% EPA + 25%DHA)/day vs. placebo | 91 | No significant effect on CPR | ↓ TG; No effect on LDL, HDL, HbA1c | Wong et al. (2010) |
| 12-week intervention: 900 mg EPA/day vs. placebo | 24 | No effect on CRP, IL-6 and TNFα | ↑ HDL and ↑ total cholesterol | Mocking et al. (2012) |
| 8-week intervention: 2700 mg EPA + DHA/day | 84 | ↓ IL-2 and ↓ TNFα No effect on CRP |
None tested | Malekshahi Moghadam et al. (2012) |
12-weeks intervention:
|
60 | No effect on serum CRP and MDA | No effect on body weight, BMI or fat mass | Azizi-Soleiman et al. (2013) |
24-week intervention:
|
60 | No effect on SOD, TBARS, GSSG/GSH | ↑ HbA1c; ↑FBG No effect on TG, TC, HDL, LDL, NEFA, Leptin, Adiponectin |
Veleba et al. (2015) |
| 3-month intervention: 1000 mg EPA + 1000 mg DHA/day vs. placebo | 74 | No effect on hsCRP, IL-6, TNF-α, ICAM-1, VCAM-1 | No effect on insulin, HbA1c, adiponectin, leptin, and lipid levels | Poreba et al. (2017) |
| Metabolic syndrome | ||||
90-day intervention:
|
102 | No effect on CPR | No effect on TG, TC, HDL, LDL, FBG, insulin, HOMA-IR | Venturini et al. (2015) |
| Inflammatory bowel disease | ||||
| 8-week intervention: 3400–3600 mg n-3 PUFA (as salmon)/day | 12 | ↓ CPR, ↑ anti-inflammatory fatty acid index No effect TNF- α, MDA |
↑ n-3 PUFAs,↑ n-3/n-6 ratio in plasma and rectal biopsies; No effect on the fecal calprotectine | Grimstad et al. (2011) |
| 90-day intervention: 2000 mg EPA/day | 20 | ↑ IL-10 expression; HES1, SOCS3, and KLF4 | ↓ fecal calprotectine Partially redressed microbiota composition |
Prossomariti et al. (2017) |
| 6-month intervention: 1000 mg EPA/day vs.placebo | 60 | No effect on CPR | ↓ fecal calprotectine | Scaioli et al. (2018) |
EPA – Eicosapentaenoic Acid; DHA – Docosahexaenoic Acid; PG – Prostaglandins; LTB – Leukotriene; TNF-α – Tumour Necrosis Factor alpha; IL – Interleukin; CRP – C-Reactive Protein; ICAM – Intercellular Adhesion Molecule; VCAM – Vascular Cell Adhesion molecule; hsCRP – high sensitive C reactive protein; IL1RN – interleukin-1 receptor antagonist protein; LSM – lifestyle modification; NF-κB – nuclear factor-kappa B); PPAR – peroxisome proliferator-activated receptor; TRAF3 – TNF Receptor Associated Factor 3; Lp-PLA2 – lipoprotein-associated phospholipase A2; PECAM – platelet and endothelial cell adhesion molecule; COX – cyclooxygenase; LOX – lypoooxigenase; TBARS –thiobarbituric acid substances; SOD – superoxide dismutase; GSH – glutathione peroxidase; MDA – malonyldialdehyde; HOMA-IR – homeostasis model assessment of insulin resistance index; HES1 – transcription factor HES1; SOCCS3 – suppressor of cytokine signaling 3; KLF4 – Kruppel-like factor 4; HbA1c – Glycated haemoglobin; RBC – red blood cell; BDNF – Brain-derived neurotrophic factor; CD14 – cluster of differentiation 14; NEFA – Non-esterified fatty acids; TC – total cholesterol; TG – Triglycerides; LDL – low-density lipoproteins; HDL – high-density lipoproteins; FBG – fasting blood glucose; LIF – leukocyte inhibitory factor.
6.4. Dietary recommendations of n-3 LC-PUFA
Currently, the recommended daily intake of n-3 PUFAs varies as regarding expert committees, ranging from 250 to 500 mg for healthy adults (Flock et al., 2013). The European Food Safety Authority's (EFSA) recommendation is 250 mg/day n-3 PUFAs (EPA and DHA) for adult males and non-pregnant females, and supplementation of 100–200 mg/day of DHA in pregnancy (EFSA Panel on Dietetic Products, 2010). For children less than 2 years old, the daily recommendation corresponds to 100 mg DHA, while for children more than 2 years and in adolescents, the daily recommendation is similar to that for adults (EFSA Panel on Dietetic Products, 2010). The upper daily value of acceptable for EPA and DHA consumption has been set at 2000 mg, but higher doses used in clinical trials did not induce adverse effects (Rangel-Huerta et al., 2012).
There are also some additional recommendations in patients with high and extremely high fasting-triglyceride levels. The American Heart Association (AHA) recommends a daily intake of 500 mg–1000 mg DHA and EPA in patients with borderline levels (150–199 mg/dl), 1000–2000 mg in patients with high levels, and 2000–4000 mg in patients with very high triglyceride levels (>500 mg/dl) (Kris-Etherton et al., 2002). Importantly, further research should be conducted before any definitive daily recommendation or on the routine use of n-3 PUFAs in other chronic inflammatory diseases.
Studies show that n-3 PUFAs do not impact in a positive manner the metabolic profile of healthy subjects and induce variable effect on diabetes mellitus cases (no important effects on inflammation but a constant ability to increase the HDL level); on the other hand, a reduction of inflammation is obese and ageing patients as well as in those with metabolic syndrome.
7. Role of polyphenols in counteracting inflammatory phenomena
Literature data demonstrates that there are approximately 8000 different polyphenolic structures, classified into more than ten classes depending on structural characteristics. Regardless of their differences in chemical behaviour, they are all characterized by having an aromatic ring carrying one or more hydroxyl groups (Bravo, 1998; Del Rio et al., 2013). The polyphenolic molecules originating from diet are involved as key components in counteracting inflammation, mitigating oxidative stress and protecting endogenous compounds from oxidative lesions, regulating the metabolism and promoting a protective phenotype, in improving the endothelial function as well as the platelet function, among several other beneficial actions (Kaliora et al., 2006; Morita et al., 2017; Nitulescu et al., 2017, 2019).
Polyphenols are key dietary components extensively studied for their involvement in preventing CVD, comorbidities of metabolic syndrome, malignancies, etc, all these diseases having an important etiological inflammatory component. For example, a central stage in the expansion of atherosclerosis is dyslipidemia, which together with increased ROS formation leads to LDL oxidation, which was correlated with the activation of pro-inflammatory pathways in the vascular wall. Likewise, it is well established that ROS and pro-inflammatory molecules generate a microenvironment predisposing to endothelial dysfunction. The increased expression of adhesion molecules (VCAM-1, ICAM-1, E-selectin) favours the adherence of monocytes to the endothelium and their infiltration within the vascular wall. As a result, of monocyte diapedesis pro-inflammatory molecules are released (TNF-α, IFNγ, MCP-1), NFκB is up-regulated, interleukins (IL-6 and IL-8) and metalloproteinases (MMPs) are synthesized (Gradinaru et al., 2017, 2018; Hansson and Libby, 2006; Libby, 2012; Libby et al., 2014; Ungurianu et al., 2019).
7.1. Cellular effects
Polyphenols interfere with the inflammatory process in multiple pathways. For example, they alter the enzymatic processes involved in the proliferation and activation of B- and T-cells, as key components of the inflammatory pathway (by inhibiting tyrosine and serine-threonine protein kinases). Likewise, polyphenols blunt the synthesis of pro-inflammatory mediators such as cytokines, chemokines (IL-8, IL-6, TNF-α, VCAM-1 and ICAM-1), and angiogenic factors, NF-кB or iNOS. Further, an inhibitory effect on several pro-inflammatory enzymes was reported, such as COX-2, MAPK or protein kinase-C (PKC) (Alvarez-Suarez et al., 2017; Gasparrini et al., 2017; Hussain et al., 2016). Thus, studies performed on macrophages proved that resveratrol inhibited the IFN-γ-induced NO production and down-regulated the IFN-γ inducible genes. In this respect, resveratrol decreased STAT1 activation (an important transcription factor for IFN-γ-induced genes) and hindered JAK-2 activation (Chung et al., 2011).
Experimental studies arguing the involvement of polyphenols in mitigating inflammation are either performed on cell line models, animal models or have direct clinical implications. In a study exposing human endothelial cells to the effect of Negroamaro and Primitivo extracts or pure compounds - stilbenes (trans-resveratrol, trans-piceid), hydroxycinnamic acids (p-coumaric, caffeic, and caftaric acids) flavonols (kaempferol, quercetin, myricetin) – before stimulation with lipopolysaccharide (LPS), an inhibition in the expression of adhesion molecules was demonstrated. The anti-inflammatory effect was sustained by a reduction of VCAM-1, ICAM-1, E-selectin, MCP-1 and macrophage colony-stimulating factor (M-CSF), ROS intracellular levels with a correlated attenuation of NF-κB and AP-1 activation. Trans-resveratrol also significantly reduced the endothelial expression and release of M-CSF. All tested compounds reduced the adhesion of monocytes to stimulated endothelial cells, this being a key element in the development of atherosclerosis (Calabriso et al., 2016). The treatment of CCD-18Co myofibroblasts cells with red wine extract reduced mRNA levels of ICAM-1, VCAM-1, NF-κB, and PECAM-1, induced by LPS the anti-inflammatory mechanism being dependent on miR-126 (Angel-Morales et al., 2012).
Another study tested the effects induced by a mixture of four main catechins found in green tea (epicatechin – EC, epigallocatechin – EGC, epigallocatechin gallate – EGCG, epicatechin gallate – GCG), as well as each one alone, on neutrophils isolated from healthy subjects. The catechin compounds induced anti-inflammatory effect (reduction of IL-1β and IL-6, TNF-α, HOCl synthesis and mieloperoxisase), together with the stimulation of antioxidant enzyme activities and Nrf2, along calcium release as well as increased phagocytic capacity, thus proving anti-inflammatory and immunomodulatory actions (Marinovic et al., 2015). In a separate study, EGCG reduced ICAM-1, NF-ĸB and IĸB expressions and reduced ROS levels upon TNF-α-induced inflammation in human retinal pigment epithelial cells. The results suggest the possible therapeutic involvement of EGCG in blocking TNF-α-mediated eye inflammation (Thichanpiang and Wongprasert, 2015). Moreover, in a study evaluating the effect of epicatechin and catechin on arachidonic acid-activated platelets and, respectively, on platelet-HUVEC interaction, the tested compounds induced a reduction of sICAM1, sVCAM1, and sE-selectin levels, as well as an increase of NO bioavailability, proving an anti-inflammatory effect and the ability to counteract endothelial dysfunction, but only when platelets were harvested from peripheral artery disease patients and not from healthy subjects (Carnevale et al., 2014).
Ellagic acid (EA) was tested for its ability to inhibit MIF-induced chemotactic migration of PBMCs, showing a failure to inhibit this response when PBMCs were stimulated with MIP-1α, but high specificity for MIF-induced effect (Sarkar et al., 2015). Chlorogenic acid exerted a dose depended anti-inflammatory effect showed by the reduction of IL-1β, TNF-α and IL-6 levels as well as the inhibition of NO synthesis and expression of COX-1 and iNOS in LPS-stimulated murine macrophages and microglial cells (Hwang et al., 2014).
An in vitro experiment evaluated the results induced by various flavonoids on the arachidonic acid release from rat neutrophils; kaempferol, luteolin, quercetin and amentoflavone reduced the inflammatory response and inhibited the activity of β-glucuronidase and lysozyme (Tordera et al., 1994). Furthermore, the positive outcome of Brassica oleracea extracts (water and methanol respectively) for CVD risk were examined; for this purpose, HUVECs were exposed to the extracts (24 h) and then to TNF-α stimulation. Exposure to the extracts from Brassica oleracea significantly reduced the TNF-α induced expression of E-selectin, ICAM-1 and VCAM-1 (Kuntz and Kunz, 2014). Another study demonstrated the capacity of extracts from Mango (Mangifera indica L.) to counteract TNF-α effects on HUVECs, through the inhibition of IL-6, IL-8, COX-2 and ICAM-1, while restoring the expression of eNOS usually down-regulated by TNF-α (Mura et al., 2015). Interestingly, in an animal model, for example, supplementation of standard chow with cacao phenolic compounds in apolipoprotein E-deficient mice, lead to an anti-inflammatory effect justified by a reduction of VCAM-1 and ICAM-1 expressions, a decrease of oxidative stress markers and a reduction of cholesterol accumulation in plaque compared to control (Natsume and Baba, 2014). Likewise, propolis (green, red or brown) treatment induced a reduction of MCP-1, VCAM, PECAM, FGF, PDGF, VEGF, MMP-9 and upregulated tissue inhibitor of metalloproteinases 1 (TIMP-1) in initial atherosclerotic lesions in LDL receptor gene knockout mice fed a diet rich in cholesterol for inducing atherosclerotic lesions; only red propolis upregulated heme oxygenase 1 (HO-1) and TIMP-1 in advanced atherosclerotic lesions (Daleprane et al., 2012).
7.2. Anti-inflammatory potential of polyphenols in humans
The anti-inflammatory effects induced by polyphenols in human studies with dietary interventions and weight related outcomes are heterogeneous, as summarized from recent literature (Table 7 ). Thus, in a clinical study with double-blind, randomized, cross-over design, the effect of a commercially available polyphenols rich extract was tested, the study including patients having more than two metabolic risk factors. Results showed a reduction of MCP-1 and MIF, but not of other markers of CVD risk (CRP, IL-6, HDL, adiponectin and oxidized LDL) (Broekhuizen et al., 2011). In a separate clinical study with cross-over design, overweight patients consumed a high-carbohydrate, moderate-fat meal supplemented with strawberry/placebo juice. The anthocyanin supplementation blunted the postprandial inflammatory response (reduced CRP level) induced by the high fat diet and reduced the postprandial insulin response (Edirisinghe et al., 2011). Furthermore, a double-blind study focused on hypercholesterolemia subjects, receiving a purified anthocyanin mixture, resulted in a reduction of their CRP, sVCAM-1 and IL-1β levels. Similar results were obtained for HepG2 and porcine iliac artery endothelial cells exposed to the same purified anthocyanin mixture (reduction of LPS-induced VCAM-1 secretion) (Zhu et al., 2013). Patients with early atherosclerosis, received simple or EGCG-enriched olive oil. Independent of EGCG addition, olive oil reduced inflammatory markers and endothelial dysfunction (sICAM, white blood cells, monocytes, lymphocytes and platelets) (Widmer et al., 2013).
Table 7.
Clinical data regarding the efficacy of polyphenols on inflammatory phenomena.
| Design | Population | Type of intervention | Inflammatory outcome | Reference |
|---|---|---|---|---|
| Randomised, double-blind, cross-over study | 34 subjects with two or more metabolic risk factors | 4-week intervention: 500 mg polyphenols/day vs. placebo | ↓MCP-1 and MIF, unchanged levels of HDL, adiponectin, CRP | Broekhuizen et al. (2011) |
| Cross-over study | 24 overweight adults | high-carbohydrate, moderate-fat meal together with a strawberry beverage (SB) or placebo | SB:↓ CRP and postprandial insulin | Edirisinghe et al. (2011) |
| Randomised, double-blind | 150 hypercholesterolemic subjects | 24-week intervention: 640 mg purified Anthocyanin/day | ↓ CRP, sVCAM-1 and IL-1β | Zhu et al. (2013) |
| Randomised, double-blind | 52 patients with early atherosclerosis, | 4-month intervention: 30 mL olive oil or 30 ml of EGCG-supplemented olive oil | ↓ sICAM, white blood cells, monocytes, lymphocytes and platelets | Widmer et al. (2013) |
| Single-centre, randomised, two-arm, double-blinded, placebo-controlled study | 36 pre-hypertension patients, randomized to control or treatment groups | 6-week intervention: grape seed extract, 150 mgx2/day | ↓BP (SBP, DBP) ↑ fasting insulin and insulin sensitivity No change of sICAM-1 |
Park et al. (2016) |
| Single blinded crossover trial | 38 patients with untreated mild hypertension | 8-week intervention: 300 mL/day cold-pressed 100% chokeberry juice and 3 g/day chokeberry powder | ↓IL-10 and TNF-α | Loo et al. (2016) |
| Randomized, double-blind, placebo-controlled clinical trial | 50 hyperlipidemic patients | 4-week intervention: V. arctostaphylos fruit extract x2/day | no effects on HDL and CRP ↓ total cholesterol, LDL-C, TG, MDA |
Soltani et al. (2014) |
| Placebo controlled study | 20 study subjects and 19 placebo | 4-week intervention: 361 mg polyphenols and 120 mg vitamin C x2/day | No significant effects on apolipoproteins, adiponectin, CRP, ICAM-1, E-Selectin or t-PA | Mullan et al. (2016) |
| Placebo controlled study | 16 trained cyclists | 7-day intervention: 30 mL of Montmorency tart cherry concentrate x 2/day | ↓lipid hydroperoxides, IL-6 and hsCRP | Bell et al. (2014) |
| Double-blind crossover study | 49 healthy male subjects with APOE genotype | 8-week intervention: 150 mg/day quercetin or placebo (3 phases, three-week washout periods) | ↓ waist circumference and postprandial SBP, moderately increased levels of TNFα | Pfeuffer et al. (2013) |
| Randomised, double-blind, placebo-controlled, cross-over trial | 18 healthy volunteers | One-tine administration of 51 mg of oleuropeine | ↓of IL8 production | Lockyer et al. (2015) |
| Cross-sectional study | 1997 females | Frequency questionnaires assessment of total intake of flavonoids | Higher anthocyanin and flavone intake were associated with significantly lower peripheral insulin resistance Higher anthocyanin intake was also associated with lower CRP concentrations Higher anthocyanin-rich intake was associated with lower insulin and inflammation |
Jennings et al. (2014) |
| Randomized, controlled dietary study | 27 subjects with metabolic syndrome | 400 g fresh bilberries/days vs. control diet | ↓ CRP, IL-6, IL-12, | Kolehmainen et al. (2012) |
The effects of grape seed extract on pre-hypertension patients were tested. Results of the study in question, showed a reduction of blood pressure (both systolic and diastolic), with improved fasting insulin and insulin sensitivity after 6 weeks of supplementation, but no significant change in sICAM-1 plasma concentration (Park et al., 2016). Furthermore, in a single blinded crossover trial including patients with untreated mild hypertension, cold-pressed chokeberry juice and dried chokeberry powder induced a reduction of IL-10 and TNF-α levels (Loo et al., 2016).
On the other hand, there are studies that do not confirm the positive effects of natural compounds on inflammatory markers regarding cardiovascular risk, especially on CRP, even if they prove to yield other beneficial outcomes (for example, on LDL). Thus, Soltani et al. examined the effects of a Vaccinium arctostaphylosfruit extract on hyperlipidemic adult patients and even if no significant effects were observed regarding HDL and CRP, a significant reduction of total cholesterol, LDL, triglycerides and malondialdehyde (MDA) levels was obtained (Soltani et al., 2014). Furthermore, Mullan et al. showed that administering a vitamin C and polyphenol-rich beverage didn't induce a reduction of metabolic or inflammatory markers (apolipoproteins, CRP, ICAM-1, E-selectin) (Mullan et al., 2016).
Results regarding the effect of polyphenols on inflammation were obtained not only in metabolically impaired patients, but also in healthy subjects. Thus, in a placebo-controlled study, the effect induced by Montmorency tart cherry concentrate on the inflammatory and redox status markers in subjects simulating road cycle racing was examined. Trained cyclists received the concentrate or placebo for 7 days, after which their oxidative stress and inflammatory markers (IL-6 and CRP) were reduced, highlighting the ability of the tested extract to improve the stress response in physical exercise conditions (Bell et al., 2014).
Furthermore, in a study with crossover, double-blind design, 49 healthy males with APOE genotype received 150 mg/day quercetin or placebo for 8 weeks, in three phases, separated by three-week washout periods. Quercetin administration led to a decrease of waist circumference and postprandial systolic blood pressure, as well as a moderately increased levels of TNFα (Pfeuffer et al., 2013). In a separate study with cross-over, double-blind, randomized, placebo-controlled design including 18 healthy subjects, the effect of oleuropeine (51 mg) on a single occasion was tested. Blood of the subjects was collected and cells were stimulated with LPS, showing a significant decrease of IL-8 production (Lockyer et al., 2015).
Flavonoid-rich products have also been discussed for their beneficial effect on insulin resistance-related metabolic complications possibly via the upregulation of genes involved in insulin sensitivity (Engin et al., 2018). In a recent review, the beneficial effect of flavonoid-rich products in a cross-sectional study including 1997 females aged 18–76 years, the correlation between the total flavonoid intake as well as their subclasses (assessed from food questionnaires) and insulin resistance/inflammation was evaluated. Results showed higher anthocyanin and flavone intake were associated with significantly lower peripheral insulin resistance and CRP concentrations (Jennings et al., 2014). In a randomized controlled dietary study, results showed that consuming a high anthocyanins diet is associated with the reduction of CRP, IL-6, IL-12, and LPS concentrations indicating a positive effect on the long term cardiometabolic risk (Kolehmainen et al., 2012).
According to literature data, polyphenols blunt the inflammatory response in clinical setting, thus reducing the cardio-vascular risk factors for hypertensive, obese or diabetes mellitus patients. Positive effects on inflammation and redox stress markers were also obtained in healthy subjects and, moreover in trained athletes, who seem to benefit from the metabolic point of view from receiving polyphenols supplements.
Just a small number of published studies investigated if n-3 PUFAs may interact with the polyphenols and if a combined diet may have an enhanced beneficial impact. Until now only the beneficial effects on HDL-levels (as a “surrogate” for the anti-inflammatory effect) were identified (Ahn et al., 2020; Annuzzi et al., 2014; Bub et al., 2019).
In an 8-week randomized controlled dietary study on overweight patients, a combined diet of high polyphenols and marine PUFAs- diet showed beneficial, although non-additive effects on plasma triglycerides. Also, the reduction in oxidative stress (measured by urinary 8-isoprostane) was observed, probably as an effect of polyphenols. A negative interaction between PUFAs and polyphenols was observed for some variables (chylomicron cholesterol and apo B-48 in large VLDLs), which suggest a possible kinetic interaction between PUFAs and polyphenols (Annuzzi et al., 2014). This kinetic finding is also in line with some preclinical data that suggested that dietary polyphenols interact with the metabolism of n-3 PUFAs and increase blood EPA and DHA level (Toufektsian et al., 2011).
Recently, in a three monocentric, parallel-arm, double-blind, randomised, dietary intervention trial, 250 mg DHA and 320 mg grape anthocyanins administered as bioactive-enriched foods, for 4 weeks, had positive effects on serum triglyceride or HDL levels (Bub et al., 2019). These results are partially in line with a later cross-sectional analysis in the Korean population that suggested beneficial effects exhibited only in men by high amounts of proanthocyanidins or n-3 PUFAs on HDL levels. In addition, n-3 PUFAs intake increased polyphenols uptake (Ahn et al., 2020).
In conclusion, large-scale cohort studies with a combined diet PUFAs + polyphenols are needed to confirm the limited available data and to investigate possible additive effects.
8. Metabolic disorder and inflammation in COVID-19
Metabolic disarray and inflammation are important factors in the pathogenesis of acute diseases. COVID-19, severe respiratory disease, is an adverse clinical outcome of the ongoing severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) pandemic (Docea et al., 2020; Goumenou et al., 2020; Shi et al., 2020), and has recently been correlated to obesity-dependent inflammation (Petrakis et al., 2020). Indeed, in its most severe form, it entails a bilateral interstitial pneumonia requiring intensive care unit (ICU) ventilation support and has concomitant high mortality rate due to and multi-organ failure. Clinical reports have demonstrated that the most common comorbidities are CVD, hypertension and T2DM, age also being an important risk factor (Grasselli et al., 2020; Zhou et al., 2020). Lifestyle-associated factors, such as smoking, have also been associated with rapid disease progression (Farsalinos et al., 2020; Mesnage et al., 2020; Tsatsakis et al., 2020). A recent US study indicates that obesity is an underappreciated risk factor for COVID-19 (Kass et al., 2020). The authors found, in a cohort of 265 hospitalized patients, that age and the body-mass index (BMI) were inversely correlated with risk, hence indicating that younger obese patients were more likely to be admitted to hospital. Kass et al. concluded that a higher prevalence of obesity in each population will result in a higher COVID-19 incidence in younger individuals than previously reported. In addition to a mechanical impediment of ventilation, obesity was correlated with lower immune response to viral infection (Honce and Schultz-Cherry, 2019). Moreover, besides obesity, metabolic disarray and inflammation were suggested to contribute to COVID-19 pathogenesis (Petrakis et al., 2020). Indeed, specific fat-resident regulatory T cells (Treg) and enhancement of TH17 (T-cell sub-lineage)-biased immunity (Poutahidis et al., 2013; Winer et al., 2009) could be positively correlated to COVID-19 prevalence and increased mortality risk in obese individuals (Petrakis et al., 2020; Skalny et al., 2020). The “obese” pattern of immune cells subtypes was correlated to increased secretion of pro-inflammatory mediators including IL-6, IL-23/IL-17, TNF-α and macrophage inflammatory protein-1α (Sumarac-Dumanovic et al., 2009). Importantly, these inflammatory mediators were proved to disrupted tight junctions of the respiratory epithelium, which facilitates pathogen entry (Wittekindt, 2017).
COVID-19 is impacting to a greater extent the patients having underlying metabolic impairments (diabetes mellitus and/or obesity), as WHO is pointing out. On the other hand, increased levels of inflammatory markers cytokines with pro-inflammatory outcomes constitute predictors of adverse outcome in COVID-19 patients (Skalny et al., 2020).
Thus, reducing the inflammatory pathways, through the long-term employment of lifestyle changes (dietary measures, smoking cessation, moderate but constant physical activity, etc) could contribute to a better reaction of the immune system when affected by aggressive pathogens, such as SarsCov2. Improving diet (such as adding polyphenols, PUFAs, fibres, etc) can contribute to a reduction of inflammation, thus increasing the chances for a better response of patients affected by the virus (Butler and Barrientos, 2020; Rajkumar, 2020; WHO, 2020).
9. Conclusions
Diet can play a major part in regulating various cellular pathways, as one is simultaneously and continually exposed to a myriad of ingested substances, which, in their minute doses can yield important long-term effects and influence the development of certain maladies, with their cumulative effects still being underestimated. Real-life risk simulation (RLRS) strategies are powerful tools for assessing not only the toxicological implications of joint effects for several molecules, but also their collective beneficial role as nutraceuticals in our diet intake. These kinds of analyses are important, as studies which separately assess the cellular and metabolic effects of certain compounds can posit their detrimental or protective actions and their potency, and thus can lead to erroneous conclusions regarding their long-term habitual consumption in lower, non-pharmacological doses, but alongside numerous other chemicals (Hernandez et al., 2020; Margină et al., 2019; Tsatsakis et al., 2019b). This type of approach will certainly play an important part in one of the most important health struggles nowadays, the prevention of NCD, and could prove itself beneficial even in the context of the present viral outbreak, since inflammation is the key component of the severe phenomena associated with the COVID-19 respiratory complications. There is an intense need for RLRS studies integrating dietary information with the inflammatory response in order to evaluate if the usual components of normal diet could contribute to regulating the immune response and reduce the sensitivity to complications.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Aggarwal B.B. Inflammation, a silent killer in cancer is not so silent! Curr. Opin. Pharmacol. 2009;9:347–350. doi: 10.1016/j.coph.2009.06.018. [DOI] [PubMed] [Google Scholar]
- Ahn S., Jun S., Joung H. Association of total flavonoid intake with hypo-HDL-cholesterolemia among Korean adults: effect modification by polyunsaturated fatty acid intake. Nutrients. 2020;12 doi: 10.3390/nu12010195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aliasgharzadeh A., Dehghan P., Gargari B.P., Asghari-Jafarabadi M. Resistant dextrin, as a prebiotic, improves insulin resistance and inflammation in women with type 2 diabetes: a randomised controlled clinical trial. Br. J. Nutr. 2015;113:321–330. doi: 10.1017/S0007114514003675. [DOI] [PubMed] [Google Scholar]
- Allaire J., Couture P., Leclerc M., Charest A., Marin J., Lépine M.C., Talbot D., Tchernof A., Lamarche B. A randomized, crossover, head-to-head comparison of eicosapentaenoic acid and docosahexaenoic acid supplementation to reduce inflammation markers in men and women: the Comparing EPA to DHA (ComparED) Study. Am. J. Clin. Nutr. 2016;104:280–287. doi: 10.3945/ajcn.116.131896. [DOI] [PubMed] [Google Scholar]
- Allingham P.G., Brownlee G.R., Harper G.S., Pho M., Nilsson S.K., Brown T.J. Gene expression, synthesis and degradation of hyaluronan during differentiation of 3T3-L1 adipocytes. Arch. Biochem. Biophys. 2006;452:83–91. doi: 10.1016/j.abb.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Alvarez-Suarez J.M., Carrillo-Perdomo E., Aller A., Giampieri F., Gasparrini M., Gonzalez-Perez L., Beltran-Ayala P., Battino M. Anti-inflammatory effect of Capuli cherry against LPS-induced cytotoxic damage in RAW 264.7 macrophages. Food Chem. Toxicol. 2017;102:46–52. doi: 10.1016/j.fct.2017.01.024. [DOI] [PubMed] [Google Scholar]
- Alves B.C., Silva T.R., Spritzer P.M. Sedentary lifestyle and high-carbohydrate intake are associated with low-grade chronic inflammation in post-menopause: a cross-sectional study. Rev. Bras. Ginecol. Obstet. 2016;38:317–324. doi: 10.1055/s-0036-1584582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ampatzoglou A., Williams C.L., Atwal K.K., Maidens C.M., Ross A.B., Thielecke F., Jonnalagadda S.S., Kennedy O.B., Yaqoob P. Effects of increased wholegrain consumption on immune and inflammatory markers in healthy low habitual wholegrain consumers. Eur. J. Nutr. 2016;55:183–195. doi: 10.1007/s00394-015-0836-y. [DOI] [PubMed] [Google Scholar]
- Andre C., Guzman-Quevedo O., Rey C., Remus-Borel J., Clark S., Castellanos-Jankiewicz A., Ladeveze E., Leste-Lasserre T., Nadjar A., Abrous D.N., Laye S., Cota D. Inhibiting microglia expansion prevents diet-induced hypothalamic and peripheral inflammation. Diabetes. 2017;66:908–919. doi: 10.2337/db16-0586. [DOI] [PubMed] [Google Scholar]
- Angel-Morales G., Noratto G., Mertens-Talcott S. Red wine polyphenolics reduce the expression of inflammation markers in human colon-derived CCD-18Co myofibroblast cells: potential role of microRNA-126. Food Funct. 2012;3:745–752. doi: 10.1039/c2fo10271d. [DOI] [PubMed] [Google Scholar]
- Annuzzi G., Bozzetto L., Costabile G., Giacco R., Mangione A., Anniballi G., Vitale M., Vetrani C., Cipriano P., Della Corte G., Pasanisi F., Riccardi G., Rivellese A.A. Diets naturally rich in polyphenols improve fasting and postprandial dyslipidemia and reduce oxidative stress: a randomized controlled trial. Am. J. Clin. Nutr. 2014;99:463–471. doi: 10.3945/ajcn.113.073445. [DOI] [PubMed] [Google Scholar]
- Aouadi M., Tencerova M., Vangala P., Yawe J.C., Nicoloro S.M., Amano S.U., Cohen J.L., Czech M.P. Gene silencing in adipose tissue macrophages regulates whole-body metabolism in obese mice. Proc. Natl. Acad. Sci. U. S. A. 2013;110:8278–8283. doi: 10.1073/pnas.1300492110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arita M., Ohira T., Sun Y.P., Elangovan S., Chiang N., Serhan C.N. Resolvin E1 selectively interacts with leukotriene B4 receptor BLT1 and ChemR23 to regulate inflammation. J. Immunol. 2007;178:3912–3917. doi: 10.4049/jimmunol.178.6.3912. [DOI] [PubMed] [Google Scholar]
- Arpon A., Milagro F.I., Razquin C., Corella D., Estruch R., Fito M., Marti A., Martinez-Gonzalez M.A., Ros E., Salas-Salvado J., Riezu-Boj J.I., Martinez J.A. Impact of consuming extra-virgin olive oil or nuts within a mediterranean diet on DNA methylation in peripheral white blood cells within the PREDIMED-Navarra randomized controlled trial: a role for dietary lipids. Nutrients. 2017;10 doi: 10.3390/nu10010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpon A., Riezu-Boj J.I., Milagro F.I., Marti A., Razquin C., Martinez-Gonzalez M.A., Corella D., Estruch R., Casas R., Fito M., Ros E., Salas-Salvado J., Martinez J.A. Adherence to Mediterranean diet is associated with methylation changes in inflammation-related genes in peripheral blood cells. J. Physiol. Biochem. 2016;73:445–455. doi: 10.1007/s13105-017-0552-6. [DOI] [PubMed] [Google Scholar]
- Asle Mohammadi Zadeh M., Kargarfard M., Marandi S.M., Habibi A. Diets along with interval training regimes improves inflammatory & anti-inflammatory condition in obesity with type 2 diabetes subjects. J. Diabetes Metab. Disord. 2018;17:253–267. doi: 10.1007/s40200-018-0368-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asztalos I.B., Gleason J.A., Sever S., Gedik R., Asztalos B.F., Horvath K.V., Dansinger M.L., Lamon-Fava S., Schaefer E.J. Effects of eicosapentaenoic acid and docosahexaenoic acid on cardiovascular disease risk factors: a randomized clinical trial. Metabolism. 2016;65:1636–1645. doi: 10.1016/j.metabol.2016.07.010. [DOI] [PubMed] [Google Scholar]
- Azizi-Soleiman F., Jazayeri S., Eghtesadi S., Rajab A., Heidari I., Vafa M.R., Gohari M.R. Effects of pure eicosapentaenoic and docosahexaenoic acids on oxidative stress, inflammation and body fat mass in patients with type 2 diabetes. Int. J. Prev. Med. 2013;4:922–928. [PMC free article] [PubMed] [Google Scholar]
- Baker E.J., Miles E.A., Burdge G.C., Yaqoob P., Calder P.C. Metabolism and functional effects of plant-derived omega-3 fatty acids in humans. Prog. Lipid Res. 2016;64:30–56. doi: 10.1016/j.plipres.2016.07.002. [DOI] [PubMed] [Google Scholar]
- Bargut T.C., Mandarim-de-Lacerda C.A., Aguila M.B. A high-fish-oil diet prevents adiposity and modulates white adipose tissue inflammation pathways in mice. J. Nutr. Biochem. 2015;26:960–969. doi: 10.1016/j.jnutbio.2015.04.002. [DOI] [PubMed] [Google Scholar]
- Bargut T.C.L., Santos L.P., Machado D.G.L., Aguila M.B., Mandarim-de-Lacerda C.A. Eicosapentaenoic acid (EPA) vs. Docosahexaenoic acid (DHA): effects in epididymal white adipose tissue of mice fed a high-fructose diet. Prostaglandins Leukot. Essent. Fatty Acids. 2017;123:14–24. doi: 10.1016/j.plefa.2017.07.004. [DOI] [PubMed] [Google Scholar]
- Barrea L., Marzullo P., Muscogiuri G., Di Somma C., Scacchi M., Orio F., Aimaretti G., Colao A., Savastano S. Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr. Res. Rev. 2018;31:291–301. doi: 10.1017/S0954422418000136. [DOI] [PubMed] [Google Scholar]
- Basil M.C., Levy B.D. Specialized pro-resolving mediators: endogenous regulators of infection and inflammation. Nat. Rev. Immunol. 2016;16:51–67. doi: 10.1038/nri.2015.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu A., Kurien B.T., Tran H., Byrd B., Maher J., Schell J., Masek E., Barrett J.R., Lyons T.J., Betts N.M., Hal Scofield R. Strawberries decrease circulating levels of tumor necrosis factor and lipid peroxides in obese adults with knee osteoarthritis. Food Funct. 2018;9:6218–6226. doi: 10.1039/c8fo01194j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedard A., Lamarche B., Corneau L., Dodin S., Lemieux S. Sex differences in the impact of the Mediterranean diet on systemic inflammation. Nutr. J. 2015;14:46. doi: 10.1186/s12937-015-0035-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekkouche L., Bouchenak M., Malaisse W.J., Yahia D.A. The Mediterranean diet adoption improves metabolic, oxidative, and inflammatory abnormalities in Algerian metabolic syndrome patients. Horm. Metab. Res. 2014;46:274–282. doi: 10.1055/s-0033-1363657. [DOI] [PubMed] [Google Scholar]
- Bell P.G., Walshe I.H., Davison G.W., Stevenson E., Howatson G. Montmorency cherries reduce the oxidative stress and inflammatory responses to repeated days high-intensity stochastic cycling. Nutrients. 2014;6:829–843. doi: 10.3390/nu6020829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender N., Portmann M., Heg Z., Hofmann K., Zwahlen M., Egger M. Fish or n3-PUFA intake and body composition: a systematic review and meta-analysis. Obes. Rev. 2014;15:657–665. doi: 10.1111/obr.12189. [DOI] [PubMed] [Google Scholar]
- Bento A.F., Claudino R.F., Dutra R.C., Marcon R., Calixto J.B. Omega-3 fatty acid-derived mediators 17(R)-hydroxy docosahexaenoic acid, aspirin-triggered resolvin D1 and resolvin D2 prevent experimental colitis in mice. J. Immunol. 2011;187:1957–1969. doi: 10.4049/jimmunol.1101305. [DOI] [PubMed] [Google Scholar]
- Bhanpuri N.H., Hallberg S.J., Williams P.T., McKenzie A.L., Ballard K.D., Campbell W.W., McCarter J.P., Phinney S.D., Volek J.S. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Cardiovasc. Diabetol. 2018;17:56. doi: 10.1186/s12933-018-0698-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blasbalg T.L., Hibbeln J.R., Ramsden C.E., Majchrzak S.F., Rawlings R.R. Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century. Am. J. Clin. Nutr. 2011;93:950–962. doi: 10.3945/ajcn.110.006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosco N., Brahmbhatt V., Oliveira M., Martin F.P., Lichti P., Raymond F., Mansourian R., Metairon S., Pace-Asciak C., Bastic Schmid V., Rezzi S., Haller D., Benyacoub J. Effects of increase in fish oil intake on intestinal eicosanoids and inflammation in a mouse model of colitis. Lipids Health Dis. 2013;12:81. doi: 10.1186/1476-511X-12-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo L. Polyphenols: chemistry, dietary sources, metabolism, and nutritional significance. Nutr. Rev. 1998;56:317–333. doi: 10.1111/j.1753-4887.1998.tb01670.x. [DOI] [PubMed] [Google Scholar]
- Broekhuizen L.N., van Wijk D.F., Vink H., Stalmach A., Crozier A., Hutten B.A., Kastelein J.J., Hugenholtz P.G., Koenig W., Stroes E.S. Reduction of monocyte chemoattractant protein 1 and macrophage migration inhibitory factor by a polyphenol-rich extract in subjects with clustered cardiometabolic risk factors. Br. J. Nutr. 2011;106:1416–1422. doi: 10.1017/S0007114511002431. [DOI] [PubMed] [Google Scholar]
- Brymora A., Flisinski M., Johnson R.J., Goszka G., Stefanska A., Manitius J. Low-fructose diet lowers blood pressure and inflammation in patients with chronic kidney disease. Nephrol. Dial. Transplant. 2012;27:608–612. doi: 10.1093/ndt/gfr223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bub A., Malpuech-Brugere C., Orfila C., Amat J., Arianna A., Blot A., Di Nunzio M., Holmes M., Kertesz Z., Marshall L., Nemeth I., Ricciardiello L., Seifert S., Sutulic S., Ulaszewska M., Bordoni A. A dietary intervention of bioactive enriched foods aimed at adults at risk of metabolic syndrome: protocol and results from PATHWAY-27 pilot study. Nutrients. 2019;11 doi: 10.3390/nu11081814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdge G.C., Calder P.C. Introduction to fatty acids and lipids. World Rev. Nutr. Diet. 2015;112:1–16. doi: 10.1159/000365423. [DOI] [PubMed] [Google Scholar]
- Butler M.J., Barrientos R.M. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav. Immun. 2020;87:53–54. doi: 10.1016/j.bbi.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabriso N., Scoditti E., Massaro M., Pellegrino M., Storelli C., Ingrosso I., Giovinazzo G., Carluccio M.A. Multiple anti-inflammatory and anti-atherosclerotic properties of red wine polyphenolic extracts: differential role of hydroxycinnamic acids, flavonols and stilbenes on endothelial inflammatory gene expression. Eur. J. Nutr. 2016;55:477–489. doi: 10.1007/s00394-015-0865-6. [DOI] [PubMed] [Google Scholar]
- Calder P.C. Fatty acids and inflammation: the cutting edge between food and pharma. Eur. J. Pharmacol. 2011;668(Suppl. 1) doi: 10.1016/j.ejphar.2011.05.085. S50-58. [DOI] [PubMed] [Google Scholar]
- Calder P.C. Long-chain fatty acids and inflammation. Proc. Nutr. Soc. 2012;71:284–289. doi: 10.1017/S0029665112000067. [DOI] [PubMed] [Google Scholar]
- Calder P.C. Marine omega-3 fatty acids and inflammatory processes: effects, mechanisms and clinical relevance. Biochim. Biophys. Acta. 2015;1851:469–484. doi: 10.1016/j.bbalip.2014.08.010. [DOI] [PubMed] [Google Scholar]
- Calder P.C. Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochem. Soc. Trans. 2017;45:1105–1115. doi: 10.1042/BST20160474. [DOI] [PubMed] [Google Scholar]
- Camargo A., Delgado-Lista J., Garcia-Rios A., Cruz-Teno C., Yubero-Serrano E.M., Perez-Martinez P., Gutierrez-Mariscal F.M., Lora-Aguilar P., Rodriguez-Cantalejo F., Fuentes-Jimenez F., Tinahones F.J., Malagon M.M., Perez-Jimenez F., Lopez-Miranda J. Expression of proinflammatory, proatherogenic genes is reduced by the Mediterranean diet in elderly people. Br. J. Nutr. 2012;108:500–508. doi: 10.1017/S0007114511005812. [DOI] [PubMed] [Google Scholar]
- Campbell E.L., MacManus C.F., Kominsky D.J., Keely S., Glover L.E., Bowers B.E., Scully M., Bruyninckx W.J., Colgan S.P. Resolvin E1-induced intestinal alkaline phosphatase promotes resolution of inflammation through LPS detoxification. Proc. Natl. Acad. Sci. U. S. A. 2010;107:14298–14303. doi: 10.1073/pnas.0914730107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnevale R., Loffredo L., Nocella C., Bartimoccia S., Bucci T., De Falco E., Peruzzi M., Chimenti I., Biondi-Zoccai G., Pignatelli P., Violi F., Frati G. Epicatechin and catechin modulate endothelial activation induced by platelets of patients with peripheral artery disease. Oxid. Med. Cell. Longev. 2014;2014 doi: 10.1155/2014/691015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casas R., Sacanella E., Urpi-Sarda M., Chiva-Blanch G., Ros E., Martinez-Gonzalez M.A., Covas M.I., Rosa Ma L.-R., Salas-Salvado J., Fiol M., Aros F., Estruch R. The effects of the mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease. A randomized trial. PLoS One. 2014;9 doi: 10.1371/journal.pone.0100084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalan V., Gomez-Ambrosi J., Rodriguez A., Fruhbeck G. Role of extracellular matrix remodelling in adipose tissue pathophysiology: relevance in the development of obesity. Histol. Histopathol. 2012;27:1515–1528. doi: 10.14670/HH-27.1515. [DOI] [PubMed] [Google Scholar]
- Ceriello A., Esposito K., La Sala L., Pujadas G., De Nigris V., Testa R., Bucciarelli L., Rondinelli M., Genovese S. The protective effect of the Mediterranean diet on endothelial resistance to GLP-1 in type 2 diabetes: a preliminary report. Cardiovasc. Diabetol. 2014;13:140. doi: 10.1186/s12933-014-0140-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers E.S., Byrne C.S., Morrison D.J., Murphy K.G., Preston T., Tedford C., Garcia-Perez I., Fountana S., Serrano-Contreras J.I., Holmes E., Reynolds C.J., Roberts J.F., Boyton R.J., Altmann D.M., McDonald J.A.K., Marchesi J.R., Akbar A.N., Riddell N.E., Wallis G.A., Frost G.S. Dietary supplementation with inulin-propionate ester or inulin improves insulin sensitivity in adults with overweight and obesity with distinct effects on the gut microbiota, plasma metabolome and systemic inflammatory responses: a randomised cross-over trial. Gut. 2019;68:1430–1438. doi: 10.1136/gutjnl-2019-318424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charpentier C., Chan R., Salameh E., Mbodji K., Ueno A., Coëffier M., Guérin C., Ghosh S., Savoye G., Marion-Letellier R. Dietary n-3 PUFA may attenuate experimental colitis. Mediat. Inflamm. 2018;2018:8430614. doi: 10.1155/2018/8430614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung E.Y., Kim B.H., Hong J.T., Lee C.K., Ahn B., Nam S.Y., Han S.B., Kim Y. Resveratrol down-regulates interferon-gamma-inducible inflammatory genes in macrophages: molecular mechanism via decreased STAT-1 activation. J. Nutr. Biochem. 2011;22:902–909. doi: 10.1016/j.jnutbio.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Clark L.F., Thivierge M.C., Kidd C.A., McGeoch S.C., Abraham P., Pearson D.W., Horgan G.W., Holtrop G., Thies F., Lobley G.E. Fish oil supplemented for 9 months does not improve glycaemic control or insulin sensitivity in subjects with impaired glucose regulation: a parallel randomised controlled trial. Br. J. Nutr. 2016;115:75–86. doi: 10.1017/S0007114515004274. [DOI] [PubMed] [Google Scholar]
- Collaborators G.D. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393:1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortes-Rojo C., Vargas-Vargas M.A., Olmos-Orizaba B.E., Rodriguez-Orozco A.R., Calderon-Cortes E. Interplay between NADH oxidation by complex I, glutathione redox state and sirtuin-3, and its role in the development of insulin resistance. Biochim. Biophys. Acta (BBA) - Mol. Basis Dis. 2020:165801. doi: 10.1016/j.bbadis.2020.165801. [DOI] [PubMed] [Google Scholar]
- Crewe C., An Y.A., Scherer P.E. The ominous triad of adipose tissue dysfunction: inflammation, fibrosis, and impaired angiogenesis. J. Clin. Invest. 2017;127:74–82. doi: 10.1172/JCI88883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daleprane J.B., Freitas Vda S., Pacheco A., Rudnicki M., Faine L.A., Dorr F.A., Ikegaki M., Salazar L.A., Ong T.P., Abdalla D.S. Anti-atherogenic and anti-angiogenic activities of polyphenols from propolis. J. Nutr. Biochem. 2012;23:557–566. doi: 10.1016/j.jnutbio.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Dalli J., Winkler J.W., Colas R.A., Arnardottir H., Cheng C.Y., Chiang N., Petasis N.A., Serhan C.N. Resolvin D3 and aspirin-triggered resolvin D3 are potent immunoresolvents. Chem. Biol. 2013;20:188–201. doi: 10.1016/j.chembiol.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dandona P., Ghanim H., Abuaysheh S., Green K., Batra M., Dhindsa S., Makdissi A., Patel R., Chaudhuri A. Decreased insulin secretion and incretin concentrations and increased glucagon concentrations after a high-fat meal when compared with a high-fruit and -fiber meal. Am. J. Physiol. Endocrinol. Metab. 2015;308:E185–E191. doi: 10.1152/ajpendo.00275.2014. [DOI] [PubMed] [Google Scholar]
- Davis N.J., Crandall J.P., Gajavelli S., Berman J.W., Tomuta N., Wylie-Rosett J., Katz S.D. Differential effects of low-carbohydrate and low-fat diets on inflammation and endothelial function in diabetes. J. Diabet. Complicat. 2011;25:371–376. doi: 10.1016/j.jdiacomp.2011.08.001. [DOI] [PubMed] [Google Scholar]
- De Lorenzo A., Bernardini S., Gualtieri P., Cabibbo A., Perrone M.A., Giambini I., Di Renzo L. Mediterranean meal versus Western meal effects on postprandial ox-LDL, oxidative and inflammatory gene expression in healthy subjects: a randomized controlled trial for nutrigenomic approach in cardiometabolic risk. Acta Diabetol. 2017;54:141–149. doi: 10.1007/s00592-016-0917-2. [DOI] [PubMed] [Google Scholar]
- De Lorenzo A., Soldati L., Sarlo F., Calvani M., Di Lorenzo N., Di Renzo L. New obesity classification criteria as a tool for bariatric surgery indication. World J. Gastroenterol. 2016;22:681–703. doi: 10.3748/wjg.v22.i2.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mello V.D., Schwab U., Kolehmainen M., Koenig W., Siloaho M., Poutanen K., Mykkanen H., Uusitupa M. A diet high in fatty fish, bilberries and wholegrain products improves markers of endothelial function and inflammation in individuals with impaired glucose metabolism in a randomised controlled trial: the Sysdimet study. Diabetologia. 2011;54:2755–2767. doi: 10.1007/s00125-011-2285-3. [DOI] [PubMed] [Google Scholar]
- de Molon R.S., Thurlings R.M., Walgreen B., Helsen M.M., van der Kraan P.M., Cirelli J.A., Koenders M.I. Systemic resolvin E1 (RvE1) treatment does not ameliorate the severity of collagen-induced arthritis (CIA) in mice: a randomized, prospective, and controlled proof of concept study. Mediat. Inflamm. 2019;2019 doi: 10.1155/2019/5689465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehghan P., Gargari B.P., Jafar-Abadi M.A., Aliasgharzadeh A. Inulin controls inflammation and metabolic endotoxemia in women with type 2 diabetes mellitus: a randomized-controlled clinical trial. Int. J. Food Sci. Nutr. 2014;65:117–123. doi: 10.3109/09637486.2013.836738. [DOI] [PubMed] [Google Scholar]
- Dehghan P., Pourghassem Gargari B., Asghari Jafar-abadi M. Oligofructose-enriched inulin improves some inflammatory markers and metabolic endotoxemia in women with type 2 diabetes mellitus: a randomized controlled clinical trial. Nutrition. 2014;30:418–423. doi: 10.1016/j.nut.2013.09.005. [DOI] [PubMed] [Google Scholar]
- Del Rio D., Rodriguez-Mateos A., Spencer J.P., Tognolini M., Borges G., Crozier A. Dietary (poly)phenolics in human health: structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxidants Redox Signal. 2013;18:1818–1892. doi: 10.1089/ars.2012.4581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Della Corte K.W., Perrar I., Penczynski K.J., Schwingshackl L., Herder C., Buyken A.E. Effect of dietary sugar intake on biomarkers of subclinical inflammation: a systematic review and meta-analysis of intervention studies. Nutrients. 2018;10 doi: 10.3390/nu10050606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demaria M., Ohtani N., Youssef S.A., Rodier F., Toussaint W., Mitchell J.R., Laberge R.M., Vijg J., Van Steeg H., Dolle M.E., Hoeijmakers J.H., de Bruin A., Hara E., Campisi J. An essential role for senescent cells in optimal wound healing through secretion of PDGF-AA. Dev. Cell. 2014;31:722–733. doi: 10.1016/j.devcel.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devarshi P.P., Jangale N.M., Ghule A.E., Bodhankar S.L., Harsulkar A.M. Beneficial effects of flaxseed oil and fish oil diet are through modulation of different hepatic genes involved in lipid metabolism in streptozotocin-nicotinamide induced diabetic rats. Genes Nutr. 2013;8:329–342. doi: 10.1007/s12263-012-0326-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding T., Wang S., Zhang X., Zai W., Fan J., Chen W., Bian Q., Luan J., Shen Y., Zhang Y., Ju D., Mei X. Kidney protection effects of dihydroquercetin on diabetic nephropathy through suppressing ROS and NLRP3 inflammasome. Phytomedicine. 2018;41:45–53. doi: 10.1016/j.phymed.2018.01.026. [DOI] [PubMed] [Google Scholar]
- Docea A.O., Tsatsakis A., Albulescu D., Cristea O., Zlatian O., Vinceti M., Moschos S.A., Tsoukalas D., Goumenou M., Drakoulis N., Dumanov J.M., Tutelyan V.A., Onischenko G.G., Aschner M., Spandidos D.A., Calina D. A new threat from an old enemy: Re-emergence of coronavirus (Review) Int. J. Mol. Med. 2020;45(6):1631–1643. doi: 10.3892/ijmm.2020.4555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooper M.M., Wassink L., M'Rabet L., Graus Y.M. The modulatory effects of prostaglandin-E on cytokine production by human peripheral blood mononuclear cells are independent of the prostaglandin subtype. Immunology. 2002;107:152–159. doi: 10.1046/j.1365-2567.2002.01474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du S., Jin J., Fang W., Su Q. Does fish oil have an anti-obesity effect in overweight/obese adults? A meta-analysis of randomized controlled trials. PLoS One. 2015;10 doi: 10.1371/journal.pone.0142652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edirisinghe I., Banaszewski K., Cappozzo J., Sandhya K., Ellis C.L., Tadapaneni R., Kappagoda C.T., Burton-Freeman B.M. Strawberry anthocyanin and its association with postprandial inflammation and insulin. Br. J. Nutr. 2011;106:913–922. doi: 10.1017/S0007114511001176. [DOI] [PubMed] [Google Scholar]
- EFSA Panel on Dietetic Products N., Allergi es (NDA) Scientific Opinion on Dietary Reference Values for fats, including saturated fatty acids, polyunsaturated fatty acids, monounsaturated fatty acids, trans fatty acids, and cholesterol. EFSA J. 2010;8:107. [Google Scholar]
- Ellenbroek J.H., van Dijck L., Tons H.A., Rabelink T.J., Carlotti F., Ballieux B.E., de Koning E.J. Long-term ketogenic diet causes glucose intolerance and reduced beta- and alpha-cell mass but no weight loss in mice. Am. J. Physiol. Endocrinol. Metab. 2014;306:E552–E558. doi: 10.1152/ajpendo.00453.2013. [DOI] [PubMed] [Google Scholar]
- Ellulu M.S., Khaza'ai H., Patimah I., Rahmat A., Abed Y. Effect of long chain omega-3 polyunsaturated fatty acids on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: a randomized controlled trial. Food Nutr. Res. 2016;60:29268. doi: 10.3402/fnr.v60.29268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engin A.B. Adipocyte-macrophage cross-talk in obesity. Adv. Exp. Med. Biol. 2017;960:327–343. doi: 10.1007/978-3-319-48382-5_14. [DOI] [PubMed] [Google Scholar]
- Engin A.B., Tsatsakis A.M., Tsoukalas D., Engin A. Do flavanols-rich natural products relieve obesity-related insulin resistance? Food Chem. Toxicol. 2018;112:157–167. doi: 10.1016/j.fct.2017.12.055. [DOI] [PubMed] [Google Scholar]
- Esgalhado M., Kemp J.A., Azevedo R., Paiva B.R., Stockler-Pinto M.B., Dolenga C.J., Borges N.A., Nakao L.S., Mafra D. Could resistant starch supplementation improve inflammatory and oxidative stress biomarkers and uremic toxins levels in hemodialysis patients? A pilot randomized controlled trial. Food Funct. 2018;9:6508–6516. doi: 10.1039/c8fo01876f. [DOI] [PubMed] [Google Scholar]
- Farsalinos K., Niaura R., Le Houezec J., Barboun i.A., Tsatsakis A., Kouretas D., Vantarakis A., Poulas K. Toxicology Reports. 2020. Nicotine and SARS-CoV-2: COVID-19 may be a disease of the nicotinic cholinergic system. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fettelschoss A., Kistowska M., LeibundGut-Landmann S., Beer H.D., Johansen P., Senti G., Contassot E., Bachmann M.F., French L.E., Oxenius A., Kundig T.M. Inflammasome activation and IL-1beta target IL-1alpha for secretion as opposed to surface expression. Proc. Natl. Acad. Sci. U. S. A. 2011;108:18055–18060. doi: 10.1073/pnas.1109176108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fini L., Piazzi G., Ceccarelli C., Daoud Y., Belluzzi A., Munarini A., Graziani G., Fogliano V., Selgrad M., Garcia M., Gasbarrini A., Genta R.M., Boland C.R., Ricciardiello L. Highly purified eicosapentaenoic acid as free fatty acids strongly suppresses polyps in Apc(Min/+) mice. Clin. Canc. Res. 2010;16:5703–5711. doi: 10.1158/1078-0432.CCR-10-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flock M.R., Harris W.S., Kris-Etherton P.M. Long-chain omega-3 fatty acids: time to establish a dietary reference intake. Nutr. Rev. 2013;71:692–707. doi: 10.1111/nure.12071. [DOI] [PubMed] [Google Scholar]
- Flock M.R., Skulas-Ray A.C., Harris W.S., Gaugler T.L., Fleming J.A., Kris-Etherton P.M. Effects of supplemental long-chain omega-3 fatty acids and erythrocyte membrane fatty acid content on circulating inflammatory markers in a randomized controlled trial of healthy adults. Prostaglandins Leukot. Essent. Fatty Acids. 2014;91:161–168. doi: 10.1016/j.plefa.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujisaka S., Usui I., Ikutani M., Aminuddin A., Takikawa A., Tsuneyama K., Mahmood A., Goda N., Nagai Y., Takatsu K., Tobe K. Adipose tissue hypoxia induces inflammatory M1 polarity of macrophages in an HIF-1alpha-dependent and HIF-1alpha-independent manner in obese mice. Diabetologia. 2013;56:1403–1412. doi: 10.1007/s00125-013-2885-1. [DOI] [PubMed] [Google Scholar]
- Gachon F., Yeung J., Naef F. Cross-regulatory circuits linking inflammation, high-fat diet, and the circadian clock. Genes Dev. 2018;32:1359–1360. doi: 10.1101/gad.320911.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbow J.R., Doherty J.M., Schugar R.C., Travers S., Weber M.L., Wentz A.E., Ezenwajiaku N., Cotter D.G., Brunt E.M., Crawford P.A. Hepatic steatosis, inflammation, and ER stress in mice maintained long term on a very low-carbohydrate ketogenic diet. Am. J. Physiol. Gastrointest. Liver Physiol. 2011;300:G956–G967. doi: 10.1152/ajpgi.00539.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gargari B.P., Namazi N., Khalili M., Sarmadi B., Jafarabadi M.A., Dehghan P. Is there any place for resistant starch, as alimentary prebiotic, for patients with type 2 diabetes? Compl. Ther. Med. 2015;23:810–815. doi: 10.1016/j.ctim.2015.09.005. [DOI] [PubMed] [Google Scholar]
- Gasparrini M., Forbes-Hernandez T.Y., Giampieri F., Afrin S., Alvarez-Suarez J.M., Mazzoni L., Mezzetti B., Quiles J.L., Battino M. Anti-inflammatory effect of strawberry extract against LPS-induced stress in RAW 264.7 macrophages. Food Chem. Toxicol. 2017;102:1–10. doi: 10.1016/j.fct.2017.01.018. [DOI] [PubMed] [Google Scholar]
- Georgescu M., Stan C., Marinescu A., Paun D. Nonorganic hearing loss. Malingering, factitious or conversion disorder? Rom. J. Leg. Med. 2014;22:35–40. [Google Scholar]
- Ghadge A., Harsulkar A., Karandikar M., Pandit V., Kuvalekar A. Comparative anti-inflammatory and lipid-normalizing effects of metformin and omega-3 fatty acids through modulation of transcription factors in diabetic rats. Genes Nutr. 2016;11:10. doi: 10.1186/s12263-016-0518-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacco R., Lappi J., Costabile G., Kolehmainen M., Schwab U., Landberg R., Uusitupa M., Poutanen K., Pacini G., Rivellese A.A., Riccardi G., Mykkanen H. Effects of rye and whole wheat versus refined cereal foods on metabolic risk factors: a randomised controlled two-centre intervention study. Clin. Nutr. 2013;32:941–949. doi: 10.1016/j.clnu.2013.01.016. [DOI] [PubMed] [Google Scholar]
- Gobbetti T., Dalli J., Colas R.A., Federici Canova D., Aursnes M., Bonnet D., Alric L., Vergnolle N., Deraison C., Hansen T.V., Serhan C.N., Perretti M. Protectin D1. Proc. Natl. Acad. Sci. U. S. A. 2017;114:3963–3968. doi: 10.1073/pnas.1617290114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomes J.A.S., Silva J.F., Marcal A.P., Silva G.C., Gomes G.F., de Oliveira A.C.P., Soares V.L., Oliveira M.C., Ferreira A.V.M., Aguiar D.C. High-refined carbohydrate diet consumption induces neuroinflammation and anxiety-like behavior in mice. J. Nutr. Biochem. 2020;77:108317. doi: 10.1016/j.jnutbio.2019.108317. [DOI] [PubMed] [Google Scholar]
- Goumenou M., Sarigiannis D., Tsatsakis A., Anesti O., Docea A.O., Petrakis D., Tsoukalas D., Kostoff R., Rakitskii V., Spandidos D.A., Aschner M., Calina D. COVID-19 in Northern Italy: an integrative overview of factors possibly influencing the sharp increase of the outbreak (Review) Mol. Med. Rep. 2020;22(1):20–32. doi: 10.3892/mmr.2020.11079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradinaru D., Khaddour H., Margina D., Ungurianu A., Borsa C., Ionescu C., Prada G.I., Usher J., Elshimali Y. Insulin-leptin Axis, cardiometabolic risk and oxidative stress in elderly with metabolic syndrome. Exp. Clin. Endocrinol. Diabetes. 2018 doi: 10.1055/s-0043-123825. [published online ahead of print, 2018 Feb 8] [DOI] [PubMed] [Google Scholar]
- Gradinaru D., Margina D., Borsa C., Ionescu C., Ilie M., Costache M., Dinischiotu A., Prada G.I. Adiponectin: possible link between metabolic stress and oxidative stress in the elderly. Aging Clin. Exp. Res. 2017;29:621–629. doi: 10.1007/s40520-016-0629-z. [DOI] [PubMed] [Google Scholar]
- Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., Cereda D., Coluccello A., Foti G., Fumagalli R., Iotti G., Latronico N., Lorini L., Merler S., Natalini G., Piatti A., Ranieri M.V., Scandroglio A.M., Storti E., Cecconi M., Pesenti A., Network C.-L.I., Nailescu A., Corona A., Zangrillo A., Protti A., Albertin A., Forastieri Molinari A., Lombardo A., Pezzi A., Benini A., Scandroglio A.M., Malara A., Castelli A., Coluccello A., Micucci A., Pesenti A., Sala A., Alborghetti A., Antonini B., Capra C., Troiano C., Roscitano C., Radrizzani D., Chiumello D., Coppini D., Guzzon D., Costantini E., Malpetti E., Zoia E., Catena E., Agosteo E., Barbara E., Beretta E., Boselli E., Storti E., Harizay F., Della Mura F., Lorini F.L., Donato Sigurta F., Marino F., Mojoli F., Rasulo F., Grasselli G., Casella G., De Filippi G., Castelli G., Aldegheri G., Gallioli G., Lotti G., Albano G., Landoni G., Marino G., Vitale G., Battista Perego G., Evasi G., Citerio G., Foti G., Natalini G., Merli G., Sforzini I., Bianciardi L., Carnevale L., Grazioli L., Cabrini L., Guatteri L., Salvi L., Dei Poli M., Galletti M., Gemma M., Ranucci M., Riccio M., Borelli M., Zambon M., Subert M., Cecconi M., Mazzoni M.G., Raimondi M., Panigada M., Belliato M., Bronzini N., Latronico N., Petrucci N., Belgiorno N., Tagliabue P., Cortellazzi P., Gnesin P., Grosso P., Gritti P., Perazzo P., Severgnini P., Ruggeri P., Sebastiano P., Covello R.D., Fernandez-Olmos R., Fumagalli R., Keim R., Rona R., Valsecchi R., Cattaneo S., Colombo S., Cirri S., Bonazzi S., Greco S., Muttini S., Langer T., Alaimo V., Viola U. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region, Italy [published online ahead of print, 2020 Apr 6] JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [published online ahead of print, 2020 Apr 6] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimstad T., Berge R.K., Bohov P., Skorve J., Gøransson L., Omdal R., Aasprong O.G., Haugen M., Meltzer H.M., Hausken T. Salmon diet in patients with active ulcerative colitis reduced the simple clinical colitis activity index and increased the anti-inflammatory fatty acid index--a pilot study. Scand. J. Clin. Lab. Invest. 2011;71:68–73. doi: 10.3109/00365513.2010.542484. [DOI] [PubMed] [Google Scholar]
- Gustafson B., Hammarstedt A., Andersson C.X., Smith U. Inflamed adipose tissue: a culprit underlying the metabolic syndrome and atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2007;27:2276–2283. doi: 10.1161/ATVBAHA.107.147835. [DOI] [PubMed] [Google Scholar]
- Guzman-Ruiz R., Tercero-Alcazar C., Rabanal-Ruiz Y., Diaz-Ruiz A., El Bekay R., Rangel-Zuniga O.A., Navarro-Ruiz M.C., Molero L., Membrives A., Ruiz-Rabelo J.F., Pandit A., Lopez-Miranda J., Tinahones F.J., Malagon M.M. Adipose tissue depot-specific intracellular and extracellular cues contributing to insulin resistance in obese individuals. Faseb. J. 2020;34(6):7520–7539. doi: 10.1096/fj.201902703R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyorkos A., Baker M.H., Miutz L.N., Lown D.A., Jones M.A., Houghton-Rahrig L.D. Carbohydrate-restricted diet and high-intensity interval training exercise improve cardio-metabolic and inflammatory profiles in metabolic syndrome: a randomized crossover trial. Cureus. 2019;11 doi: 10.7759/cureus.5596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajihashemi P., Azadbakht L., Hashemipor M., Kelishadi R., Esmaillzadeh A. Whole-grain intake favorably affects markers of systemic inflammation in obese children: a randomized controlled crossover clinical trial. Mol. Nutr. Food Res. 2014;58:1301–1308. doi: 10.1002/mnfr.201300582. [DOI] [PubMed] [Google Scholar]
- Hald S., Schioldan A.G., Moore M.E., Dige A., Laerke H.N., Agnholt J., Bach Knudsen K.E., Hermansen K., Marco M.L., Gregersen S., Dahlerup J.F. Effects of arabinoxylan and resistant starch on intestinal microbiota and short-chain fatty acids in subjects with metabolic syndrome: a randomised crossover study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0159223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Y.M., Jeong M., Park J.M., Kim M.Y., Go E.J., Cha J.Y., Kim K.J., Hahm K.B. The ω-3 polyunsaturated fatty acids prevented colitis-associated carcinogenesis through blocking dissociation of β-catenin complex, inhibiting COX-2 through repressing NF-κB, and inducing 15-prostaglandin dehydrogenase. Oncotarget. 2016;7:63583–63595. doi: 10.18632/oncotarget.11544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson G.K., Libby P. The immune response in atherosclerosis: a double-edged sword. Nat. Rev. Immunol. 2006;6:508–519. doi: 10.1038/nri1882. [DOI] [PubMed] [Google Scholar]
- Hassan A., Ibrahim A., Mbodji K., Coëffier M., Ziegler F., Bounoure F., Chardigny J.M., Skiba M., Savoye G., Déchelotte P., Marion-Letellier R. An α-linolenic acid-rich formula reduces oxidative stress and inflammation by regulating NF-κB in rats with TNBS-induced colitis. J. Nutr. 2010;140:1714–1721. doi: 10.3945/jn.109.119768. [DOI] [PubMed] [Google Scholar]
- He C., Wu Q., Hayashi N., Nakano F., Nakatsukasa E., Tsuduki T. Carbohydrate-restricted diet alters the gut microbiota, promotes senescence and shortens the life span in senescence-accelerated prone mice. J. Nutr. Biochem. 2019;78:108326. doi: 10.1016/j.jnutbio.2019.108326. [DOI] [PubMed] [Google Scholar]
- He W., Yuan T., Choezom D., Hunkler H., Annamalai K., Lupse B., Maedler K. Ageing potentiates diet-induced glucose intolerance, beta-cell failure and tissue inflammation through TLR4. Sci. Rep. 2018;8:2767. doi: 10.1038/s41598-018-20909-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez A.F., Buha A., Constantin C., Wallace D.R., Sarigiannis D., Neagu M., Antonijevic B., Hayes A.W., Wilks M.F., Tsatsakis A. Critical assessment and integration of separate lines of evidence for risk assessment of chemical mixtures. Arch. Toxicol. 2019;93:2741–2757. doi: 10.1007/s00204-019-02547-x. [DOI] [PubMed] [Google Scholar]
- Hernandez A.F., Docea A.O., Goumenou M., Sarigiannis D., Aschner M., Tsatsakis A. Application of novel technologies and mechanistic data for risk assessment under the real-life risk simulation (RLRS) approach. Food Chem. Toxicol. 2020;137:111123. doi: 10.1016/j.fct.2020.111123. [DOI] [PubMed] [Google Scholar]
- Hernandez A.F., Tsatsakis A.M. Human exposure to chemical mixtures: challenges for the integration of toxicology with epidemiology data in risk assessment. Food Chem. Toxicol. 2017;103:188–193. doi: 10.1016/j.fct.2017.03.012. [DOI] [PubMed] [Google Scholar]
- Hernandez T.L., Van Pelt R.E., Anderson M.A., Reece M.S., Reynolds R.M., de la Houssaye B.A., Heerwagen M., Donahoo W.T., Daniels L.J., Chartier-Logan C., Janssen R.C., Friedman J.E., Barbour L.A. Women with gestational diabetes mellitus randomized to a higher-complex carbohydrate/low-fat diet manifest lower adipose tissue insulin resistance, inflammation, glucose, and free fatty acids: a pilot study. Diabetes Care. 2016;39:39–42. doi: 10.2337/dc15-0515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honce R., Schultz-Cherry S. Impact of obesity on influenza A virus pathogenesis, immune response, and evolution. Front. Immunol. 2019;10:1071. doi: 10.3389/fimmu.2019.01071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou Y.Y., Ojo O., Wang L.L., Wang Q., Jiang Q., Shao X.Y., Wang X.H. A randomized controlled trial to compare the effect of peanuts and almonds on the cardio-metabolic and inflammatory parameters in patients with type 2 diabetes mellitus. Nutrients. 2018;10 doi: 10.3390/nu10111565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu T., Yao L., Reynolds K., Whelton P.K., Niu T., Li S., He J., Bazzano L.A. The effects of a low-carbohydrate diet vs. a low-fat diet on novel cardiovascular risk factors: a randomized controlled trial. Nutrients. 2015;7:7978–7994. doi: 10.3390/nu7095377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain T., Tan B., Yin Y., Blachier F., Tossou M.C., Rahu N. Oxidative stress and inflammation: what polyphenols can do for us? Oxid. Med. Cell. Longev. 2016;2016 doi: 10.1155/2016/7432797. 7432797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang S.J., Kim Y.W., Park Y., Lee H.J., Kim K.W. Anti-inflammatory effects of chlorogenic acid in lipopolysaccharide-stimulated RAW 264.7 cells. Inflamm. Res. 2014;63:81–90. doi: 10.1007/s00011-013-0674-4. [DOI] [PubMed] [Google Scholar]
- Hynes R.O. The extracellular matrix: not just pretty fibrils. Science. 2009;326:1216–1219. doi: 10.1126/science.1176009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im D.S. Omega-3 fatty acids in anti-inflammation (pro-resolution) and GPCRs. Prog. Lipid Res. 2012;51:232–237. doi: 10.1016/j.plipres.2012.02.003. [DOI] [PubMed] [Google Scholar]
- Ishida T., Yoshida M., Arita M., Nishitani Y., Nishiumi S., Masuda A., Mizuno S., Takagawa T., Morita Y., Kutsumi H., Inokuchi H., Serhan C.N., Blumberg R.S., Azuma T. Resolvin E1, an endogenous lipid mediator derived from eicosapentaenoic acid, prevents dextran sulfate sodium-induced colitis. Inflamm. Bowel Dis. 2010;16:87–95. doi: 10.1002/ibd.21029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itariu B.K., Zeyda M., Hochbrugger E.E., Neuhofer A., Prager G., Schindler K., Bohdjalian A., Mascher D., Vangala S., Schranz M., Krebs M., Bischof M.G., Stulnig T.M. Long-chain n-3 PUFAs reduce adipose tissue and systemic inflammation in severely obese nondiabetic patients: a randomized controlled trial. Am. J. Clin. Nutr. 2012;96:1137–1149. doi: 10.3945/ajcn.112.037432. [DOI] [PubMed] [Google Scholar]
- Izadi V., Haghighatdoost F., Moosavian P., Azadbakht L. Effect of low-energy-dense diet rich in multiple functional foods on weight-loss maintenance, inflammation, and cardiovascular risk factors: a randomized controlled trial. J. Am. Coll. Nutr. 2018;37:399–405. doi: 10.1080/07315724.2017.1412275. [DOI] [PubMed] [Google Scholar]
- Izadpanah A., Barnard R.J., Almeda A.J., Baldwin G.C., Bridges S.A., Shellman E.R., Burant C.F., Roberts C.K. A short-term diet and exercise intervention ameliorates inflammation and markers of metabolic health in overweight/obese children. Am. J. Physiol. Endocrinol. Metab. 2012;303:E542–E550. doi: 10.1152/ajpendo.00190.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jangale N.M., Devarshi P.P., Bansode S.B., Kulkarni M.J., Harsulkar A.M. Dietary flaxseed oil and fish oil ameliorates renal oxidative stress, protein glycation, and inflammation in streptozotocin-nicotinamide-induced diabetic rats. J. Physiol. Biochem. 2016;72:327–336. doi: 10.1007/s13105-016-0482-8. [DOI] [PubMed] [Google Scholar]
- Jennings A., Cashman K.D., Gillings R., Cassidy A., Tang J., Fraser W., Dowling K.G., Hull G.L.J., Berendsen A.A.M., de Groot L., Pietruszka B., Wierzbicka E., Ostan R., Bazzocchi A., Battista G., Caumon E., Meunier N., Malpuech-Brugere C., Franceschi C., Santoro A., Fairweather-Tait S.J. A Mediterranean-like dietary pattern with vitamin D3 (10 microg/d) supplements reduced the rate of bone loss in older Europeans with osteoporosis at baseline: results of a 1-y randomized controlled trial. Am. J. Clin. Nutr. 2018;108:633–640. doi: 10.1093/ajcn/nqy122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings A., Welch A.A., Spector T., Macgregor A., Cassidy A. Intakes of anthocyanins and flavones are associated with biomarkers of insulin resistance and inflammation in women. J. Nutr. 2014;144:202–208. doi: 10.3945/jn.113.184358. [DOI] [PubMed] [Google Scholar]
- Ji E., Jung M.Y., Park J.H., Kim S., Seo C.R., Park K.W., Lee E.K., Yeom C.H., Lee S. Inhibition of adipogenesis in 3T3-L1 cells and suppression of abdominal fat accumulation in high-fat diet-feeding C57BL/6J mice after downregulation of hyaluronic acid. Int. J. Obes. 2014;38:1035–1043. doi: 10.1038/ijo.2013.202. [DOI] [PubMed] [Google Scholar]
- Johansson-Persson A., Ulmius M., Cloetens L., Karhu T., Herzig K.H., Onning G. A high intake of dietary fiber influences C-reactive protein and fibrinogen, but not glucose and lipid metabolism, in mildly hypercholesterolemic subjects. Eur. J. Nutr. 2014;53:39–48. doi: 10.1007/s00394-013-0496-8. [DOI] [PubMed] [Google Scholar]
- Jonasson L., Guldbrand H., Lundberg A.K., Nystrom F.H. Advice to follow a low-carbohydrate diet has a favourable impact on low-grade inflammation in type 2 diabetes compared with advice to follow a low-fat diet. Ann. Med. 2014;46:182–187. doi: 10.3109/07853890.2014.894286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juanola-Falgarona M., Salas-Salvado J., Ibarrola-Jurado N., Rabassa-Soler A., Diaz-Lopez A., Guasch-Ferre M., Hernandez-Alonso P., Balanza R., Bullo M. Effect of the glycemic index of the diet on weight loss, modulation of satiety, inflammation, and other metabolic risk factors: a randomized controlled trial. Am. J. Clin. Nutr. 2014;100:27–35. doi: 10.3945/ajcn.113.081216. [DOI] [PubMed] [Google Scholar]
- Kaliora A.C., Dedoussis G.V., Schmidt H. Dietary antioxidants in preventing atherogenesis. Atherosclerosis. 2006;187:1–17. doi: 10.1016/j.atherosclerosis.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Kang L., Lantier L., Kennedy A., Bonner J.S., Mayes W.H., Bracy D.P., Bookbinder L.H., Hasty A.H., Thompson C.B., Wasserman D.H. Hyaluronan accumulates with high-fat feeding and contributes to insulin resistance. Diabetes. 2013;62:1888–1896. doi: 10.2337/db12-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kani A.H., Alavian S.M., Esmaillzadeh A., Adibi P., Haghighatdoost F., Azadbakht L. Effects of a low-calorie, low-carbohydrate soy containing diet on systemic inflammation among patients with nonalcoholic fatty liver disease: a parallel randomized clinical trial. Horm. Metab. Res. 2017;49:687–692. doi: 10.1055/s-0042-118707. [DOI] [PubMed] [Google Scholar]
- Kass D.A., Duggal P., Cingolani O. Obesity could shift severe COVID-19 disease to younger ages. Lancet. 2020;395(10236):1544–1545. doi: 10.1016/S0140-6736(20)31024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur G., Cameron-Smith D., Garg M., Sinclair A.J. Docosapentaenoic acid (22:5n-3): a review of its biological effects. Prog. Lipid Res. 2011;50:28–34. doi: 10.1016/j.plipres.2010.07.004. [DOI] [PubMed] [Google Scholar]
- Kavasi R.M., Berdiaki A., Spyridaki I., Corsini E., Tsatsakis A., Tzanakakis G., Nikitovic D. HA metabolism in skin homeostasis and inflammatory disease. Food Chem. Toxicol. 2017;101:128–138. doi: 10.1016/j.fct.2017.01.012. [DOI] [PubMed] [Google Scholar]
- Kavasi R.M., Berdiaki A., Spyridaki I., Papoutsidakis A., Corsini E., Tsatsakis A., Tzanakakis G.N., Nikitovic D. Contact allergen (PPD and DNCB)-induced keratinocyte sensitization is partly mediated through a low molecular weight hyaluronan (LMWHA)/TLR4/NF-kappaB signaling axis. Toxicol. Appl. Pharmacol. 2019;377:114632. doi: 10.1016/j.taap.2019.114632. [DOI] [PubMed] [Google Scholar]
- Kawabata K., Tung N.H., Shoyama Y., Sugie S., Mori T., Tanaka T. Dietary crocin inhibits colitis and colitis-associated colorectal carcinogenesis in male ICR mice. Evid. Based Complement. Alternat. Med. 2012;2012 doi: 10.1155/2012/820415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Belury M.A., Andridge R., Malarkey W.B., Hwang B.S., Glaser R. Omega-3 supplementation lowers inflammation in healthy middle-aged and older adults: a randomized controlled trial. Brain Behav. Immun. 2012;26:988–995. doi: 10.1016/j.bbi.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.Y., Kwon H.Y., Kim K.S., Kim M.K., Kwon O. Postprandial glucose and NF-kappaB responses are regulated differently by monounsaturated fatty acid and dietary fiber in impaired fasting glucose subjects. J. Med. Food. 2013;16:1168–1171. doi: 10.1089/jmf.2013.2781. [DOI] [PubMed] [Google Scholar]
- Kim J.Y., Lim K., Kim K.H., Kim J.H., Choi J.S., Shim S.C. N-3 polyunsaturated fatty acids restore Th17 and Treg balance in collagen antibody-induced arthritis. PLoS One. 2018;13 doi: 10.1371/journal.pone.0194331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohsaka A., Laposky A.D., Ramsey K.M., Estrada C., Joshu C., Kobayashi Y., Turek F.W., Bass J. High-fat diet disrupts behavioral and molecular circadian rhythms in mice. Cell Metabol. 2007;6:414–421. doi: 10.1016/j.cmet.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Kolehmainen M., Mykkanen O., Kirjavainen P.V., Leppanen T., Moilanen E., Adriaens M., Laaksonen D.E., Hallikainen M., Puupponen-Pimia R., Pulkkinen L., Mykkanen H., Gylling H., Poutanen K., Torronen R. Bilberries reduce low-grade inflammation in individuals with features of metabolic syndrome. Mol. Nutr. Food Res. 2012;56:1501–1510. doi: 10.1002/mnfr.201200195. [DOI] [PubMed] [Google Scholar]
- Kondo K., Morino K., Nishio Y., Ishikado A., Arima H., Nakao K., Nakagawa F., Nikami F., Sekine O., Nemoto K.I., Suwa M., Matsumoto M., Miura K., Makino T., Ugi S., Maegawa H. Fiber-rich diet with brown rice improves endothelial function in type 2 diabetes mellitus: a randomized controlled trial. PLoS One. 2017;12 doi: 10.1371/journal.pone.0179869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kris-Etherton P.M., Harris W.S., Appel L.J., Committee A.H.A.N. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. 2002;106:2747–2757. doi: 10.1161/01.cir.0000038493.65177.94. [DOI] [PubMed] [Google Scholar]
- Krishnamoorthy S., Recchiuti A., Chiang N., Yacoubian S., Lee C.H., Yang R., Petasis N.A., Serhan C.N. Resolvin D1 binds human phagocytes with evidence for proresolving receptors. Proc. Natl. Acad. Sci. U. S. A. 2010;107:1660–1665. doi: 10.1073/pnas.0907342107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunnumakkara A.B., Sailo B.L., Banik K., Harsha C., Prasad S., Gupta S.C., Bharti A.C., Aggarwal B.B. Chronic diseases, inflammation, and spices: how are they linked? J. Transl. Med. 2018;16:14. doi: 10.1186/s12967-018-1381-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntz S., Kunz C. Extracts from Brassica oleracea L. convar. acephala var. sabellica inhibit TNF-alpha stimulated neutrophil adhesion in vitro under flow conditions. Food Funct. 2014;5:1082–1090. doi: 10.1039/c3fo60562k. [DOI] [PubMed] [Google Scholar]
- Lankinen M., Uusitupa M., Schwab U. Nordic diet and inflammation-A review of observational and intervention studies. Nutrients. 2019;11 doi: 10.3390/nu11061369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.C., Yu S.C., Lo Y.C., Lin I.H., Tung T.H., Huang S.Y. A high linoleic acid diet exacerbates metabolic responses and gut microbiota dysbiosis in obese rats with diabetes mellitus. Food Funct. 2019;10:786–798. doi: 10.1039/c8fo02423e. [DOI] [PubMed] [Google Scholar]
- Li X., Zhao Y., Chen C., Yang L., Lee H.H., Wang Z., Zhang N., Kolonin M.G., An Z., Ge X., Scherer P.E., Sun K. Critical role of matrix metalloproteinase 14 in adipose tissue remodeling during obesity. Mol. Cell Biol. 2020;40 doi: 10.1128/MCB.00564-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Z., Xu Y., Wen X., Nie H., Hu T., Yang X., Chu X., Yang J., Deng X., He J. Rosmarinic acid attenuates airway inflammation and hyperresponsiveness in a murine model of asthma. Molecules. 2016;21 doi: 10.3390/molecules21060769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libby P. Inflammation in atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2012;32:2045–2051. doi: 10.1161/ATVBAHA.108.179705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libby P., Tabas I., Fredman G., Fisher E.A. Inflammation and its resolution as determinants of acute coronary syndromes. Circ. Res. 2014;114:1867–1879. doi: 10.1161/CIRCRESAHA.114.302699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima-Garcia J.F., Dutra R.C., da Silva K., Motta E.M., Campos M.M., Calixto J.B. The precursor of resolvin D series and aspirin-triggered resolvin D1 display anti-hyperalgesic properties in adjuvant-induced arthritis in rats. Br. J. Pharmacol. 2011;164:278–293. doi: 10.1111/j.1476-5381.2011.01345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, Chun T.H., Kang L. Adipose extracellular matrix remodelling in obesity and insulin resistance. Biochem. Pharmacol. 2016;119:8–16. doi: 10.1016/j.bcp.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockyer S., Corona G., Yaqoob P., Spencer J.P., Rowland I. Secoiridoids delivered as olive leaf extract induce acute improvements in human vascular function and reduction of an inflammatory cytokine: a randomised, double-blind, placebo-controlled, cross-over trial. Br. J. Nutr. 2015;114:75–83. doi: 10.1017/S0007114515001269. [DOI] [PubMed] [Google Scholar]
- Loo B.M., Erlund I., Koli R., Puukka P., Hellstrom J., Wahala K., Mattila P., Jula A. Consumption of chokeberry (Aronia mitschurinii) products modestly lowered blood pressure and reduced low-grade inflammation in patients with mildly elevated blood pressure. Nutr. Res. 2016;36:1222–1230. doi: 10.1016/j.nutres.2016.09.005. [DOI] [PubMed] [Google Scholar]
- Lopez-Moreno J., Quintana-Navarro G.M., Delgado-Lista J., Garcia-Rios A., Alcala-Diaz J.F., Gomez-Delgado F., Camargo A., Perez-Martinez P., Tinahones F.J., Striker G.E., Perez-Jimenez F., Villalba J.M., Lopez-Miranda J., Yubero-Serrano E.M. Mediterranean diet supplemented with coenzyme Q10 modulates the postprandial metabolism of advanced glycation end products in elderly men and women. J. Gerontol. A Biol. Sci. Med. Sci. 2018;73:340–346. doi: 10.1093/gerona/glw214. [DOI] [PubMed] [Google Scholar]
- Lu Y., Yang Y.Y., Zhou M.W., Liu N., Xing H.Y., Liu X.X., Li F. Ketogenic diet attenuates oxidative stress and inflammation after spinal cord injury by activating Nrf2 and suppressing the NF-kappaB signaling pathways. Neurosci. Lett. 2018;683:13–18. doi: 10.1016/j.neulet.2018.06.016. [DOI] [PubMed] [Google Scholar]
- Lumeng C.N., DelProposto J.B., Westcott D.J., Saltiel A.R. Phenotypic switching of adipose tissue macrophages with obesity is generated by spatiotemporal differences in macrophage subtypes. Diabetes. 2008;57:3239–3246. doi: 10.2337/db08-0872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luz A.B.S., Dos Santos Figueredo J.B., Salviano B., Aguiar A., Pinheiro L., Krause M.F.D., da Silva Camillo C., Ladd F.V.L., Bortolin R.H., Silbiger V.N., Maciel B.L.L., de Araujo Morais A.H. Adipocytes and intestinal epithelium dysfunctions linking obesity to inflammation induced by high glycemic index pellet-diet in Wistar rats. Biosci. Rep. 2018;38 doi: 10.1042/BSR20180304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusdottir O.K., Gunnarsdottir I., Birgisdottir B.E. Dietary guidelines in type 2 diabetes: the Nordic diet or the ketogenic diet? Curr. Opin. Endocrinol. Diabetes Obes. 2017;24:315–319. doi: 10.1097/MED.0000000000000361. [DOI] [PubMed] [Google Scholar]
- Maiorino M.I., Bellastella G., Petrizzo M., Scappaticcio L., Giugliano D., Esposito K. Mediterranean diet cools down the inflammatory milieu in type 2 diabetes: the MEDITA randomized controlled trial. Endocrine. 2016;54:634–641. doi: 10.1007/s12020-016-0881-1. [DOI] [PubMed] [Google Scholar]
- Malekshahi Moghadam A., Saedisomeolia A., Djalali M., Djazayery A., Pooya S., Sojoudi F. Efficacy of omega-3 fatty acid supplementation on serum levels of tumour necrosis factor-alpha, C-reactive protein and interleukin-2 in type 2 diabetes mellitus patients. Singap. Med. J. 2012;53:615–619. [PubMed] [Google Scholar]
- Marcon R., Bento A.F., Dutra R.C., Bicca M.A., Leite D.F., Calixto J.B. Maresin 1, a proresolving lipid mediator derived from omega-3 polyunsaturated fatty acids, exerts protective actions in murine models of colitis. J. Immunol. 2013;191:4288–4298. doi: 10.4049/jimmunol.1202743. [DOI] [PubMed] [Google Scholar]
- Margina D., Ilie M., Gradinaru D. Quercetin and epigallocatechin gallate induce in vitro a dose-dependent stiffening and hyperpolarizing effect on the cell membrane of human mononuclear blood cells. Int. J. Mol. Sci. 2012;13:4839–4859. doi: 10.3390/ijms13044839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margină D., Nițulescu G.M., Ungurianu A., Mesnage R., Goumenou M., Sarigianis D.A., Aschner M., Spandidos D.A., Renieri E.A., Hernandez A.F., Tsatsakis A. Overview of the effects of chemical mixtures with endocrine disrupting activity in the context of real-life risk simulation (RLRS): an integrative approach (Review) World Acad. Sci. J. 2019;1:157–164. doi: 10.3892/wasj.2019.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinovic M.P., Morandi A.C., Otton R. Green tea catechins alone or in combination alter functional parameters of human neutrophils via suppressing the activation of TLR-4/NFkappaB p65 signal pathway. Toxicol. Vitro. 2015;29:1766–1778. doi: 10.1016/j.tiv.2015.07.014. [DOI] [PubMed] [Google Scholar]
- Marques-Rocha J.L., Milagro F.I., Mansego M.L., Zulet M.A., Bressan J., Martinez J.A. Expression of inflammation-related miRNAs in white blood cells from subjects with metabolic syndrome after 8 wk of following a Mediterranean diet-based weight loss program. Nutrition. 2016;32:48–55. doi: 10.1016/j.nut.2015.06.008. [DOI] [PubMed] [Google Scholar]
- Martinez-Gonzalez M.A., Toledo E., Aros F., Fiol M., Corella D., Salas-Salvado J., Ros E., Covas M.I., Fernandez-Crehuet J., Lapetra J., Munoz M.A., Fito M., Serra-Majem L., Pinto X., Lamuela-Raventos R.M., Sorli J.V., Babio N., Buil-Cosiales P., Ruiz-Gutierrez V., Estruch R., Alonso A., Investigators P. Extravirgin olive oil consumption reduces risk of atrial fibrillation: the PREDIMED (Prevencion con Dieta Mediterranea) trial. Circulation. 2014;130:18–26. doi: 10.1161/CIRCULATIONAHA.113.006921. [DOI] [PubMed] [Google Scholar]
- Martucci M., Ostan R., Biondi F., Bellavista E., Fabbri C., Bertarelli C., Salvioli S., Capri M., Franceschi C., Santoro A. Mediterranean diet and inflammaging within the hormesis paradigm. Nutr. Rev. 2017;75:442–455. doi: 10.1093/nutrit/nux013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mas E., Croft K.D., Zahra P., Barden A., Mori T.A. Resolvins D1, D2, and other mediators of self-limited resolution of inflammation in human blood following n-3 fatty acid supplementation. Clin. Chem. 2012;58:1476–1484. doi: 10.1373/clinchem.2012.190199. [DOI] [PubMed] [Google Scholar]
- Mayr H.L., Thomas C.J., Tierney A.C., Kucianski T., George E.S., Ruiz-Canela M., Hebert J.R., Shivappa N., Itsiopoulos C. Randomization to 6-month Mediterranean diet compared with a low-fat diet leads to improvement in Dietary Inflammatory Index scores in patients with coronary heart disease: the AUSMED Heart Trial. Nutr. Res. 2018;55:94–107. doi: 10.1016/j.nutres.2018.04.006. [DOI] [PubMed] [Google Scholar]
- Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. doi: 10.1038/nature07201. [DOI] [PubMed] [Google Scholar]
- Mesnage R., Tsakiris I.N., Antoniou M.N., Tsatsakis A. Limitations in the evidential basis supporting health benefits from a decreased exposure to pesticides through organic food consumption. Curr. Opin. Toxicol. 2020;19:50–55. [Google Scholar]
- Meyer B.J., Mann N.J., Lewis J.L., Milligan G.C., Sinclair A.J., Howe P.R. Dietary intakes and food sources of omega-6 and omega-3 polyunsaturated fatty acids. Lipids. 2003;38:391–398. doi: 10.1007/s11745-003-1074-0. [DOI] [PubMed] [Google Scholar]
- Minihane A.M., Vinoy S., Russell W.R., Baka A., Roche H.M., Tuohy K.M., Teeling J.L., Blaak E.E., Fenech M., Vauzour D., McArdle H.J., Kremer B.H., Sterkman L., Vafeiadou K., Benedetti M.M., Williams C.M., Calder P.C. Low-grade inflammation, diet composition and health: current research evidence and its translation. Br. J. Nutr. 2015;114:999–1012. doi: 10.1017/S0007114515002093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mocking R.J., Assies J., Bot M., Jansen E.H., Schene A.H., Pouwer F. Biological effects of add-on eicosapentaenoic acid supplementation in diabetes mellitus and co-morbid depression: a randomized controlled trial. PLoS One. 2012;7 doi: 10.1371/journal.pone.0049431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monfort-Pires M., Crisma A.R., Bordin S., Ferreira S.R.G. Greater expression of postprandial inflammatory genes in humans after intervention with saturated when compared to unsaturated fatty acids. Eur. J. Nutr. 2018;57:2887–2895. doi: 10.1007/s00394-017-1559-z. [DOI] [PubMed] [Google Scholar]
- Mori S., Kiuchi S., Ouchi A., Hase T., Murase T. Characteristic expression of extracellular matrix in subcutaneous adipose tissue development and adipogenesis; comparison with visceral adipose tissue. Int. J. Biol. Sci. 2014;10:825–833. doi: 10.7150/ijbs.8672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin C., Blier P.U., Fortin S. MAG-EPA reduces severity of DSS-induced colitis in rats. Am. J. Physiol. Gastrointest. Liver Physiol. 2016;310:G808–G821. doi: 10.1152/ajpgi.00136.2015. [DOI] [PubMed] [Google Scholar]
- Morita M., Naito Y., Niki E., Yoshikawa T. Antioxidant action of fermented grain food supplement: scavenging of peroxyl radicals and inhibition of plasma lipid oxidation induced by multiple oxidants. Food Chem. 2017;237:574–580. doi: 10.1016/j.foodchem.2017.05.157. [DOI] [PubMed] [Google Scholar]
- Muldoon M.F., Laderian B., Kuan D.C., Sereika S.M., Marsland A.L., Manuck S.B. Fish oil supplementation does not lower C-reactive protein or interleukin-6 levels in healthy adults. J. Intern. Med. 2016;279:98–109. doi: 10.1111/joim.12442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullan A., Delles C., Ferrell W., Mullen W., Edwards C.A., McColl J.H., Roberts S.A., Lean M.E., Sattar N. Effects of a beverage rich in (poly)phenols on established and novel risk markers for vascular disease in medically uncomplicated overweight or obese subjects: a four week randomized placebo-controlled trial. Atherosclerosis. 2016;246:169–176. doi: 10.1016/j.atherosclerosis.2016.01.004. [DOI] [PubMed] [Google Scholar]
- Mura M., Palmieri D., Garella D., Di Stilo A., Perego P., Cravotto G., Palombo D. Simultaneous ultrasound-assisted water extraction and beta-cyclodextrin encapsulation of polyphenols from Mangifera indica stem bark in counteracting TNFalpha-induced endothelial dysfunction. Nat. Prod. Res. 2015;29:1657–1663. doi: 10.1080/14786419.2014.996753. [DOI] [PubMed] [Google Scholar]
- Myette-Cote E., Durrer C., Neudorf H., Bammert T.D., Botezelli J.D., Johnson J.D., DeSouza C.A., Little J.P. The effect of a short-term low-carbohydrate, high-fat diet with or without postmeal walks on glycemic control and inflammation in type 2 diabetes: a randomized trial. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018;315:R1210–R1219. doi: 10.1152/ajpregu.00240.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagy N., Sunkari V.G., Kaber G., Hasbun S., Lam D.N., Speake C., Sanda S., McLaughlin T.L., Wight T.N., Long S.R., Bollyky P.L. Hyaluronan levels are increased systemically in human type 2 but not type 1 diabetes independently of glycemic control. Matrix Biol. 2019;80:46–58. doi: 10.1016/j.matbio.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natsume M., Baba S. Suppressive effects of cacao polyphenols on the development of atherosclerosis in apolipoprotein E-deficient mice. Subcell. Biochem. 2014;77:189–198. doi: 10.1007/978-94-007-7920-4_16. [DOI] [PubMed] [Google Scholar]
- Neagu M., Constantin C., Popescu I.D., Zipeto D., Tzanakakis G., Nikitovic D., Fenga C., Stratakis C.A., Spandidos D.A., Tsatsakis A.M. Inflammation and metabolism in cancer cell-mitochondria key player. Front. Oncol. 2019;9:348. doi: 10.3389/fonc.2019.00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikitovic D., Corsini E., Kouretas D., Tsatsakis A., Tzanakakis G. ROS-major mediators of extracellular matrix remodeling during tumor progression. Food Chem. Toxicol. 2013;61:178–186. doi: 10.1016/j.fct.2013.06.013. [DOI] [PubMed] [Google Scholar]
- Nikitovic D., Mytilinaiou M., Berdiaki A., Karamanos N.K., Tzanakakis G.N. Heparan sulfate proteoglycans and heparin regulate melanoma cell functions. Biochim. Biophys. Acta. 2014;1840:2471–2481. doi: 10.1016/j.bbagen.2014.01.031. [DOI] [PubMed] [Google Scholar]
- Nikitovic D., Papoutsidakis A., Karamanos N.K., Tzanakakis G.N. Lumican affects tumor cell functions, tumor-ECM interactions, angiogenesis and inflammatory response. Matrix Biol. 2014;35:206–214. doi: 10.1016/j.matbio.2013.09.003. [DOI] [PubMed] [Google Scholar]
- Nikitovic D., Tzardi M., Berdiaki A., Tsatsakis A., Tzanakakis G.N. Cancer microenvironment and inflammation: role of hyaluronan. Front. Immunol. 2015;6:169. doi: 10.3389/fimmu.2015.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson J., Ericsson M., Joibari M.M., Anderson F., Carlsson L., Nilsson S.K., Sjodin A., Buren J. A low-carbohydrate high-fat diet decreases lean mass and impairs cardiac function in pair-fed female C57BL/6J mice. Nutr Metab. (Lond.) 2016;13:79. doi: 10.1186/s12986-016-0132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimigean V., Poll A., Minculescu C.A., Nimigean V.R., Moraru S.A., Vîrlan M.J.R., Bălăceanu R.A., Păun D.L. Immunohistochemical evaluation of autogenous mandibular bone grafts integration: an experimental study. Roman. Biotechnol. Lett. 2019;24:229–235. [Google Scholar]
- Nimigean V., Poll A., Nimigean V., Moraru S., Badita D., Paun D. The routine and specialised staining for the histologic evaluation of autogenous mandibular bone grafts an experimental study. Rev. Chem. 2018;69:1106–1109. [Google Scholar]
- Nitulescu G., Mihai D.P., Nicorescu I.M., Olaru O.T., Ungurianu A., Zanfirescu A., Nitulescu G.M., Margina D. Discovery of natural naphthoquinones as sortase A inhibitors and potential anti-infective solutions against Staphylococcus aureus. Drug Dev. Res. 2019;80:1136–1145. doi: 10.1002/ddr.21599. [DOI] [PubMed] [Google Scholar]
- Nitulescu G., Nicorescu I.M., Olaru O.T., Ungurianu A., Mihai D.P., Zanfirescu A., Nitulescu G.M., Margina D. Molecular docking and screening studies of new natural sortase A inhibitors. Int. J. Mol. Sci. 2017;18 doi: 10.3390/ijms18102217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomiyama T., Perez-Tilve D., Ogawa D., Gizard F., Zhao Y., Heywood E.B., Jones K.L., Kawamori R., Cassis L.A., Tschop M.H., Bruemmer D. Osteopontin mediates obesity-induced adipose tissue macrophage infiltration and insulin resistance in mice. J. Clin. Invest. 2007;117:2877–2888. doi: 10.1172/JCI31986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norling L.V., Serhan C.N. Profiling in resolving inflammatory exudates identifies novel anti-inflammatory and pro-resolving mediators and signals for termination. J. Intern. Med. 2010;268:15–24. doi: 10.1111/j.1365-2796.2010.02235.x. [DOI] [PubMed] [Google Scholar]
- Nowotny B., Zahiragic L., Bierwagen A., Kabisch S., Groener J.B., Nowotny P.J., Fleitmann A.K., Herder C., Pacini G., Erlund I., Landberg R., Haering H.U., Pfeiffer A.F., Nawroth P.P., Roden M. Low-energy diets differing in fibre, red meat and coffee intake equally improve insulin sensitivity in type 2 diabetes: a randomised feasibility trial. Diabetologia. 2015;58:255–264. doi: 10.1007/s00125-014-3457-8. [DOI] [PubMed] [Google Scholar]
- Oh D.Y., Talukdar S., Bae E.J., Imamura T., Morinaga H., Fan W., Li P., Lu W.J., Watkins S.M., Olefsky J.M. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell. 2010;142:687–698. doi: 10.1016/j.cell.2010.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega-Gomez A., Perretti M., Soehnlein O. Resolution of inflammation: an integrated view. EMBO Mol. Med. 2013;5:661–674. doi: 10.1002/emmm.201202382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osorio F.G., Soria-Valles C., Santiago-Fernandez O., Freije J.M., Lopez-Otin C. NF-kappaB signaling as a driver of ageing. Int. Rev. Cell Mol. Biol. 2016;326:133–174. doi: 10.1016/bs.ircmb.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Pandurangan A.K., Ismail S., Saadatdoust Z., Esa N.M. Allicin alleviates dextran sodium sulfate- (DSS-) induced ulcerative colitis in BALB/c mice. Oxid. Med. Cell. Longev. 2015;2015:605208. doi: 10.1155/2015/605208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panieri E., Buha A., Telkoparan-Akillilar P., Cevik D., Kouretas D., Veskoukis A., Skaperda Z., Tsatsakis A., Wallace D., Suzen S., Saso L. Potential Applications of NRF2 Modulators in Cancer Therapy. Antioxidants (Basel) 2020;vol. 9 doi: 10.3390/antiox9030193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paoli A., Moro T., Bosco G., Bianco A., Grimaldi K.A., Camporesi E., Mangar D. Effects of n-3 polyunsaturated fatty acids (omega-3) supplementation on some cardiovascular risk factors with a ketogenic Mediterranean diet. Mar. Drugs. 2015;13:996–1009. doi: 10.3390/md13020996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papamichael M.M., Katsardis C., Lambert K., Tsoukalas D., Koutsilieris M., Erbas B., Itsiopoulos C. Efficacy of a Mediterranean diet supplemented with fatty fish in ameliorating inflammation in paediatric asthma: a randomised controlled trial. J. Hum. Nutr. Diet. 2019;32:185–197. doi: 10.1111/jhn.12609. [DOI] [PubMed] [Google Scholar]
- Park E., Edirisinghe I., Choy Y.Y., Waterhouse A., Burton-Freeman B. Effects of grape seed extract beverage on blood pressure and metabolic indices in individuals with pre-hypertension: a randomised, double-blinded, two-arm, parallel, placebo-controlled trial. Br. J. Nutr. 2016;115:226–238. doi: 10.1017/S0007114515004328. [DOI] [PubMed] [Google Scholar]
- Pasarica M., Sereda O.R., Redman L.M., Albarado D.C., Hymel D.T., Roan L.E., Rood J.C., Burk D.H., Smith S.R. Reduced adipose tissue oxygenation in human obesity: evidence for rarefaction, macrophage chemotaxis, and inflammation without an angiogenic response. Diabetes. 2009;58:718–725. doi: 10.2337/db08-1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paun D.L., Vija L., Stan E., Banica A., Bobeica E., Terzea D., Poiana C., Badiu C., Paun S. Cushing syndrome secondary to ectopic adrenocorticotropic hormone secretion from a Meckel diverticulum neuroendocrine tumor: case report. BMC Endocr. Disord. 2015;15:72. doi: 10.1186/s12902-015-0070-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C.M., Beyl R.A., Marlatt K.L., Martin C.K., Aryana K.J., Marco M.L., Martin R.J., Keenan M.J., Ravussin E. Effect of 12 wk of resistant starch supplementation on cardiometabolic risk factors in adults with prediabetes: a randomized controlled trial. Am. J. Clin. Nutr. 2018;108:492–501. doi: 10.1093/ajcn/nqy121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrakis D., Margina D., Tsarouhas K., Tekos F., Stan M., Nikitovic D., Kouretas D., Spandidos D.A., Tsatsakis A. Obesity - a risk factor for increased COVID-19 prevalence, severity and lethality (Review) Mol. Med. Rep. 2020;22(1):9–19. doi: 10.3892/mmr.2020.11127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeuffer M., Auinger A., Bley U., Kraus-Stojanowic I., Laue C., Winkler P., Rufer C.E., Frank J., Bosch-Saadatmandi C., Rimbach G., Schrezenmeir J. Effect of quercetin on traits of the metabolic syndrome, endothelial function and inflammation in men with different APOE isoforms. Nutr. Metabol. Cardiovasc. Dis. 2013;23:403–409. doi: 10.1016/j.numecd.2011.08.010. [DOI] [PubMed] [Google Scholar]
- Piazzi G., D'Argenio G., Prossomariti A., Lembo V., Mazzone G., Candela M., Biagi E., Brigidi P., Vitaglione P., Fogliano V., D'Angelo L., Fazio C., Munarini A., Belluzzi A., Ceccarelli C., Chieco P., Balbi T., Loadman P.M., Hull M.A., Romano M., Bazzoli F., Ricciardiello L. Eicosapentaenoic acid free fatty acid prevents and suppresses colonic neoplasia in colitis-associated colorectal cancer acting on Notch signaling and gut microbiota. Int. J. Canc. 2014;135:2004–2013. doi: 10.1002/ijc.28853. [DOI] [PubMed] [Google Scholar]
- Pimentel G.D., Lira F.S., Rosa J.C., Oller do Nascimento C.M., Oyama L.M., Harumi Watanabe R.L., Ribeiro E.B. High-fat fish oil diet prevents hypothalamic inflammatory profile in rats. ISRN Inflamm. 2013;2013:419823. doi: 10.1155/2013/419823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poll A., Minculescu C., Nimigean V., Badita D., Balaceanu R., Paun D., Moraru S., Nimigean V. Experimental model for the study of autogenous mandibular bone grafts integration. Roman. Biotechnol. Lett. 2018;23:13681–13689. [Google Scholar]
- Poll A., Minculescu C.A., Nimigean V.R., Bădiță D., Bălăceanu R.A., Păun D.L., Moraru S.A., Nimigean V. Experimental model for the study of autogenous mandibular bone gras integration. Roman. Biotechnol. Lett. 2018;23:13681–13689. [Google Scholar]
- Polus A., Zapala B., Razny U., Gielicz A., Kiec-Wilk B., Malczewska-Malec M., Sanak M., Childs C.E., Calder P.C., Dembinska-Kiec A. Omega-3 fatty acid supplementation influences the whole blood transcriptome in women with obesity, associated with pro-resolving lipid mediator production. Biochim. Biophys. Acta. 2016;1861:1746–1755. doi: 10.1016/j.bbalip.2016.08.005. [DOI] [PubMed] [Google Scholar]
- Poreba M., Mostowik M., Siniarski A., Golebiowska-Wiatrak R., Malinowski K.P., Haberka M., Konduracka E., Nessler J., Undas A., Gajos G. Treatment with high-dose n-3 PUFAs has no effect on platelet function, coagulation, metabolic status or inflammation in patients with atherosclerosis and type 2 diabetes. Cardiovasc. Diabetol. 2017;16:50. doi: 10.1186/s12933-017-0523-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poudyal H., Panchal S.K., Diwan V., Brown L. Omega-3 fatty acids and metabolic syndrome: effects and emerging mechanisms of action. Prog. Lipid Res. 2011;50:372–387. doi: 10.1016/j.plipres.2011.06.003. [DOI] [PubMed] [Google Scholar]
- Poutahidis T., Kleinewietfeld M., Smillie C., Levkovich T., Perrotta A., Bhela S., Varian B.J., Ibrahim Y.M., Lakritz J.R., Kearney S.M., Chatzigiagkos A., Hafler D.A., Alm E.J., Erdman S.E. Microbial reprogramming inhibits Western diet-associated obesity. PLoS One. 2013;8 doi: 10.1371/journal.pone.0068596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prossomariti A., Scaioli E., Piazzi G., Fazio C., Bellanova M., Biagi E., Candela M., Brigidi P., Consolandi C., Balbi T., Chieco P., Munarini A., Pariali M., Minguzzi M., Bazzoli F., Belluzzi A., Ricciardiello L. Short-term treatment with eicosapentaenoic acid improves inflammation and affects colonic differentiation markers and microbiota in patients with ulcerative colitis. Sci. Rep. 2017;7:7458. doi: 10.1038/s41598-017-07992-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. Ayurveda and COVID-19: where psychoneuroimmunology and the meaning response meet. Brain Behav. Immun. 2020;87:8–9. doi: 10.1016/j.bbi.2020.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rallidis L.S., Kolomvotsou A., Lekakis J., Farajian P., Vamvakou G., Dagres N., Zolindaki M., Efstathiou S., Anastasiou-Nana M., Zampelas A. Short-term effects of Mediterranean-type diet intervention on soluble cellular adhesion molecules in subjects with abdominal obesity. Clin. Nutr. ESPEN. 2017;17:38–43. doi: 10.1016/j.clnesp.2016.11.002. [DOI] [PubMed] [Google Scholar]
- Rangel-Huerta O.D., Aguilera C.M., Mesa M.D., Gil A. Omega-3 long-chain polyunsaturated fatty acids supplementation on inflammatory biomakers: a systematic review of randomised clinical trials. Br. J. Nutr. 2012;107(Suppl. 2):S159–S170. doi: 10.1017/S0007114512001559. [DOI] [PubMed] [Google Scholar]
- Rees D., Miles E.A., Banerjee T., Wells S.J., Roynette C.E., Wahle K.W., Calder P.C. Dose-related effects of eicosapentaenoic acid on innate immune function in healthy humans: a comparison of young and older men. Am. J. Clin. Nutr. 2006;83:331–342. doi: 10.1093/ajcn/83.2.331. [DOI] [PubMed] [Google Scholar]
- Reuter S., Gupta S.C., Chaturvedi M.M., Aggarwal B.B. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic. Biol. Med. 2010;49:1603–1616. doi: 10.1016/j.freeradbiomed.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roager H.M., Vogt J.K., Kristensen M., Hansen L.B.S., Ibrugger S., Maerkedahl R.B., Bahl M.I., Lind M.V., Nielsen R.L., Frokiaer H., Gobel R.J., Landberg R., Ross A.B., Brix S., Holck J., Meyer A.S., Sparholt M.H., Christensen A.F., Carvalho V., Hartmann B., Holst J.J., Rumessen J.J., Linneberg A., Sicheritz-Ponten T., Dalgaard M.D., Blennow A., Frandsen H.L., Villas-Boas S., Kristiansen K., Vestergaard H., Hansen T., Ekstrom C.T., Ritz C., Nielsen H.B., Pedersen O.B., Gupta R., Lauritzen L., Licht T.R. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut. 2019;68:83–93. doi: 10.1136/gutjnl-2017-314786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum M., Hall K.D., Guo J., Ravussin E., Mayer L.S., Reitman M.L., Smith S.R., Walsh B.T., Leibel R.L. Glucose and lipid homeostasis and inflammation in humans following an isocaloric ketogenic diet. Obesity (Silver Spring) 2019;27:971–981. doi: 10.1002/oby.22468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouhani M.H., Kelishadi R., Hashemipour M., Esmaillzadeh A., Surkan P.J., Keshavarz A., Azadbakht L. The impact of a low glycemic index diet on inflammatory markers and serum adiponectin concentration in adolescent overweight and obese girls: a randomized clinical trial. Horm. Metab. Res. 2016;48:251–256. doi: 10.1055/s-0042-100467. [DOI] [PubMed] [Google Scholar]
- Ruiz-Ojeda F.J., Mendez-Gutierrez A., Aguilera C.M., Plaza-Diaz J. Extracellular matrix remodeling of adipose tissue in obesity and metabolic diseases. Int. J. Mol. Sci. 2019;20 doi: 10.3390/ijms20194888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell C.D., Schwarze J. The role of pro-resolution lipid mediators in infectious disease. Immunology. 2014;141:166–173. doi: 10.1111/imm.12206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruth M.R., Port A.M., Shah M., Bourland A.C., Istfan N.W., Nelson K.P., Gokce N., Apovian C.M. Consuming a hypocaloric high fat low carbohydrate diet for 12 weeks lowers C-reactive protein, and raises serum adiponectin and high density lipoprotein-cholesterol in obese subjects. Metabolism. 2013;62:1779–1787. doi: 10.1016/j.metabol.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar S., Siddiqui A.A., Mazumder S., De R., Saha S.J., Banerjee C., Iqbal M.S., Adhikari S., Alam A., Roy S., Bandyopadhyay U. Ellagic acid, a dietary polyphenol, inhibits tautomerase activity of human macrophage migration inhibitory factor and its pro-inflammatory responses in human peripheral blood mononuclear cells. J. Agric. Food Chem. 2015;63:4988–4998. doi: 10.1021/acs.jafc.5b00921. [DOI] [PubMed] [Google Scholar]
- Sawada T., Tsubata H., Hashimoto N., Takabe M., Miyata T., Aoki K., Yamashita S., Oishi S., Osue T., Yokoi K., Tsukishiro Y., Onishi T., Shimane A., Taniguchi Y., Yasaka Y., Ohara T., Kawai H., Yokoyama M. Effects of 6-month eicosapentaenoic acid treatment on postprandial hyperglycemia, hyperlipidemia, insulin secretion ability, and concomitant endothelial dysfunction among newly-diagnosed impaired glucose metabolism patients with coronary artery disease. An open label, single blinded, prospective randomized controlled trial. Cardiovasc. Diabetol. 2016;15:121. doi: 10.1186/s12933-016-0437-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scaioli E., Sartini A., Bellanova M., Campieri M., Festi D., Bazzoli F., Belluzzi A. Eicosapentaenoic acid reduces fecal levels of calprotectin and prevents relapse in patients with ulcerative colitis. Clin. Gastroenterol. Hepatol. 2018;16:1268–1275. doi: 10.1016/j.cgh.2018.01.036. e1262. [DOI] [PubMed] [Google Scholar]
- Schipper H.S., Prakken B., Kalkhoven E., Boes M. Adipose tissue-resident immune cells: key players in immunometabolism. Trends Endocrinol. Metabol. 2012;23:407–415. doi: 10.1016/j.tem.2012.05.011. [DOI] [PubMed] [Google Scholar]
- Schoettl T., Fischer I.P., Ussar S. Heterogeneity of adipose tissue in development and metabolic function. J. Exp. Biol. 2018;221 doi: 10.1242/jeb.162958. [DOI] [PubMed] [Google Scholar]
- Sedláček P., Plavinová I., Langmajerová J., Dvořáková J., Novák J., Trefil L., Müller L., Buňatová P., Zeman V., Müllerová D. Effect of n-3 fatty acids supplementation during life style modification in women with overweight. Cent. Eur. J. Publ. Health. 2018;26:265–271. doi: 10.21101/cejph.a5259. [DOI] [PubMed] [Google Scholar]
- Serhan C.N., Chiang N., Van Dyke T.E. Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat. Rev. Immunol. 2008;8:349–361. doi: 10.1038/nri2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serhan C.N., Petasis N.A. Resolvins and protectins in inflammation resolution. Chem. Rev. 2011;111:5922–5943. doi: 10.1021/cr100396c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serhan C.N., Savill J. Resolution of inflammation: the beginning programs the end. Nat. Immunol. 2005;6:1191–1197. doi: 10.1038/ni1276. [DOI] [PubMed] [Google Scholar]
- Sharma M., Kaur R., Kaushik K., Kaushal N. Redox modulatory protective effects of ω-3 fatty acids rich fish oil against experimental colitis. Toxicol. Mech. Methods. 2019;29:244–254. doi: 10.1080/15376516.2018.1553220. [DOI] [PubMed] [Google Scholar]
- Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X., Bucci E., Piacentini M., Ippolito G., Melino G. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020;27:1451–1454. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sifaki M., Assouti M., Nikitovic D., Krasagakis K., Karamanos N.K., Tzanakakis G.N. Lumican, a small leucine-rich proteoglycan substituted with keratan sulfate chains is expressed and secreted by human melanoma cells and not normal melanocytes. IUBMB Life. 2006;58:606–610. doi: 10.1080/15216540600951605. [DOI] [PubMed] [Google Scholar]
- Skalny A.V., Rink L., Ajsuvakova O.P., Aschner M., Gritsenko V.A., Alekseenko S.I., Svistunov A.A., Petrakis D., Spandidos D.A., Aaseth J., Tsatsakis A., Tinkov A.A. Zinc and respiratory tract infections: Perspectives for COVID-19 (Review) Int. J. Mol. Med. 2020;46(1):17–26. doi: 10.3892/ijmm.2020.4575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltani R., Hakimi M., Asgary S., Ghanadian S.M., Keshvari M., Sarrafzadegan N. Evaluation of the effects of Vaccinium arctostaphylos L. Fruit extract on serum lipids and hs-CRP levels and oxidative stress in adult patients with hyperlipidemia: a randomized, double-blind, placebo-controlled clinical trial. Evid. Based Complement. Alternat. Med. 2014;2014 doi: 10.1155/2014/217451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soukas A., Socci N.D., Saatkamp B.D., Novelli S., Friedman J.M. Distinct transcriptional profiles of adipogenesis in vivo and in vitro. J. Biol. Chem. 2001;276:34167–34174. doi: 10.1074/jbc.M104421200. [DOI] [PubMed] [Google Scholar]
- Springer N.L., Iyengar N.M., Bareja R., Verma A., Jochelson M.S., Giri D.D., Zhou X.K., Elemento O., Dannenberg A.J., Fischbach C. Obesity-associated extracellular matrix remodeling promotes a macrophage phenotype similar to tumor-associated macrophages. Am. J. Pathol. 2019;189:2019–2035. doi: 10.1016/j.ajpath.2019.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumarac-Dumanovic M., Stevanovic D., Ljubic A., Jorga J., Simic M., Stamenkovic-Pejkovic D., Starcevic V., Trajkovic V., Micic D. Increased activity of interleukin-23/interleukin-17 proinflammatory axis in obese women. Int. J. Obes. 2009;33:151–156. doi: 10.1038/ijo.2008.216. [DOI] [PubMed] [Google Scholar]
- Sun K., Park J., Gupta O.T., Holland W.L., Auerbach P., Zhang N., Goncalves Marangoni R., Nicoloro S.M., Czech M.P., Varga J., Ploug T., An Z., Scherer P.E. Endotrophin triggers adipose tissue fibrosis and metabolic dysfunction. Nat. Commun. 2014;5:3485. doi: 10.1038/ncomms4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung B., Prasad S., Yadav V.R., Aggarwal B.B. Cancer cell signaling pathways targeted by spice-derived nutraceuticals. Nutr. Canc. 2012;64:173–197. doi: 10.1080/01635581.2012.630551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan A., Sullenbarger B., Prakash R., McDaniel J.C. Supplementation with eicosapentaenoic acid and docosahexaenoic acid reduces high levels of circulating proinflammatory cytokines in aging adults: a randomized, controlled study. Prostaglandins Leukot. Essent. Fatty Acids. 2018;132:23–29. doi: 10.1016/j.plefa.2018.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Termeer C., Benedix F., Sleeman J., Fieber C., Voith U., Ahrens T., Miyake K., Freudenberg M., Galanos C., Simon J.C. Oligosaccharides of Hyaluronan activate dendritic cells via toll-like receptor 4. J. Exp. Med. 2002;195:99–111. doi: 10.1084/jem.20001858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thichanpiang P., Wongprasert K. Green tea polyphenol epigallocatechin-3-gallate attenuates TNF-alpha-induced intercellular adhesion molecule-1 expression and monocyte adhesion to retinal pigment epithelial cells. Am. J. Chin. Med. 2015;43:103–119. doi: 10.1142/S0192415X1550007X. [DOI] [PubMed] [Google Scholar]
- Tordera M., Ferrandiz M.L., Alcaraz M.J. Influence of anti-inflammatory flavonoids on degranulation and arachidonic acid release in rat neutrophils. Z. Naturforsch. C J. Biosci. 1994;49:235–240. doi: 10.1515/znc-1994-3-412. [DOI] [PubMed] [Google Scholar]
- Tosti V., Bertozzi B., Fontana L. Health benefits of the mediterranean diet: metabolic and molecular mechanisms. J. Gerontol. A Biol. Sci. Med. Sci. 2018;73:318–326. doi: 10.1093/gerona/glx227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toufektsian M.C., Salen P., Laporte F., Tonelli C., de Lorgeril M. Dietary flavonoids increase plasma very long-chain (n-3) fatty acids in rats. J. Nutr. 2011;141:37–41. doi: 10.3945/jn.110.127225. [DOI] [PubMed] [Google Scholar]
- Trayhurn P. Hypoxia and adipocyte physiology: implications for adipose tissue dysfunction in obesity. Annu. Rev. Nutr. 2014;34:207–236. doi: 10.1146/annurev-nutr-071812-161156. [DOI] [PubMed] [Google Scholar]
- Tripp M.L., Dahlberg C.J., Eliason S., Lamb J.J., Ou J.J., Gao W., Bhandari J., Graham D., Dudleenamjil E., Babish J.G. A low-glycemic, mediterranean diet and lifestyle modification program with targeted nutraceuticals reduces body weight, improves cardiometabolic variables and longevity biomarkers in overweight subjects: a 13-week observational trial. J. Med. Food. 2019;22:479–489. doi: 10.1089/jmf.2018.0063. [DOI] [PubMed] [Google Scholar]
- Tsatsakis A., Goumenou M., Liesivuori J., Dekant W., Hernandez A.F. Toxicology for real-life risk simulation - editorial preface to this special issue. Toxicol. Lett. 2019;309:33–34. doi: 10.1016/j.toxlet.2018.12.003. [DOI] [PubMed] [Google Scholar]
- Tsatsakis A., Petrakis D., Nikolouzakis T., Docea A., Calina D., Vincet i.M., Goumenou M., Kostoff R., Mamoulakis C., Aschne r.M., Hernández A. COVID-19, an opportunity to reevaluate the correlation between long-term effects of anthropogenic pollutants on viral epidemic/pandemic events and prevalence. Food Chem. Toxicol. 2020;141 doi: 10.1016/j.fct.2020.111418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsatsakis A., Tyshko N.V., Docea A.O., Shestakova S.I., Sidorova Y.S., Petrov N.A., Zlatian O., Mach M., Hartung T., Tutelyan V.A. The effect of chronic vitamin deficiency and long term very low dose exposure to 6 pesticides mixture on neurological outcomes - a real-life risk simulation approach. Toxicol. Lett. 2019;315:96–106. doi: 10.1016/j.toxlet.2019.07.026. [DOI] [PubMed] [Google Scholar]
- Tsatsakis A.M., Docea A.O., Tsitsimpikou C. New challenges in risk assessment of chemicals when simulating real exposure scenarios; simultaneous multi-chemicals' low dose exposure. Food Chem. Toxicol. 2016;96:174–176. doi: 10.1016/j.fct.2016.08.011. [DOI] [PubMed] [Google Scholar]
- Tschopp J., Schroder K. NLRP3 inflammasome activation: the convergence of multiple signalling pathways on ROS production? Nat. Rev. Immunol. 2010;10:210–215. doi: 10.1038/nri2725. [DOI] [PubMed] [Google Scholar]
- Tsoukalas D., Alegakis A.K., Fragkiadaki P., Papakonstantinou E., Tsilimidos G., Geraci F., Sarandi E., Nikitovic D., Spandidos D.A., Tsatsakis A. Application of metabolomics part II: focus on fatty acids and their metabolites in healthy adults. Int. J. Mol. Med. 2019;43:233–242. doi: 10.3892/ijmm.2018.3989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsoukalas D., Fragoulakis V., Sarandi E., Docea A.O., Papakonstaninou E., Tsilimidos G., Anamaterou C., Fragkiadaki P., Aschner M., Tsatsakis A., Drakoulis N., Calina D. Targeted metabolomic analysis of serum fatty acids for the prediction of autoimmune diseases. Front. Mol. Biosci. 2019;6:120. doi: 10.3389/fmolb.2019.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzanakakis G., Kavasi R.M., Voudouri K., Berdiaki A., Spyridaki I., Tsatsakis A., Nikitovic D. Role of the extracellular matrix in cancer-associated epithelial to mesenchymal transition phenomenon. Dev. Dynam. 2018;247:368–381. doi: 10.1002/dvdy.24557. [DOI] [PubMed] [Google Scholar]
- Tzanakakis G., Neagu M., Tsatsakis A., Nikitovic D. Proteoglycans and immunobiology of cancer-therapeutic implications. Front. Immunol. 2019;10:875. doi: 10.3389/fimmu.2019.00875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungurianu A., Margina D., Gradinaru D., Bacanu C., Ilie M., Tsitsimpikou C., Tsarouhas K., Spandidos D.A., Tsatsakis A.M. Lipoprotein redox status evaluation as a marker of cardiovascular disease risk in patients with inflammatory disease. Mol. Med. Rep. 2017;15:256–262. doi: 10.3892/mmr.2016.5972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungurianu A., Seremet O., Gagniuc E., Olaru O.T., Gutu C., Gradinaru D., Ionescu-Tirgoviste C., Margina D., Danciulescu-Miulescu R. Preclinical and clinical results regarding the effects of a plant-based antidiabetic formulation versus well established antidiabetic molecules. Pharmacol. Res. 2019;150:104522. doi: 10.1016/j.phrs.2019.104522. [DOI] [PubMed] [Google Scholar]
- Ungurianu A., Seremet O., Gradinaru D., Ionescu-Tirgoviste C., Margina D., Danciulescu Miulescu R. Spectrophotometric versus spectrofluorometric assessment in the study of the relationships between lipid peroxidation and metabolic dysregulation. Chem. Biol. Drug Des. 2019;93(6):1026–1035. doi: 10.1111/cbdd.13474. [DOI] [PubMed] [Google Scholar]
- Uusitupa M., Hermansen K., Savolainen M.J., Schwab U., Kolehmainen M., Brader L., Mortensen L.S., Cloetens L., Johansson-Persson A., Onning G., Landin-Olsson M., Herzig K.H., Hukkanen J., Rosqvist F., Iggman D., Paananen J., Pulkki K.J., Siloaho M., Dragsted L., Barri T., Overvad K., Bach Knudsen K.E., Hedemann M.S., Arner P., Dahlman I., Borge G.I., Baardseth P., Ulven S.M., Gunnarsdottir I., Jonsdottir S., Thorsdottir I., Oresic M., Poutanen K.S., Riserus U., Akesson B. Effects of an isocaloric healthy Nordic diet on insulin sensitivity, lipid profile and inflammation markers in metabolic syndrome -- a randomized study (SYSDIET) J. Intern. Med. 2013;274:52–66. doi: 10.1111/joim.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veleba J., Kopecky J., Janovska P., Kuda O., Horakova O., Malinska H., Kazdova L., Oliyarnyk O., Skop V., Trnovska J., Hajek M., Skoch A., Flachs P., Bardova K., Rossmeisl M., Olza J., de Castro G.S., Calder P.C., Gardlo A., Fiserova E., Jensen J., Bryhn M., Pelikanova T. Combined intervention with pioglitazone and n-3 fatty acids in metformin-treated type 2 diabetic patients: improvement of lipid metabolism. Nutr Metab. (Lond.) 2015;12:52. doi: 10.1186/s12986-015-0047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venturini D., Simão A.N., Urbano M.R., Dichi I. Effects of extra virgin olive oil and fish oil on lipid profile and oxidative stress in patients with metabolic syndrome. Nutrition. 2015;31:834–840. doi: 10.1016/j.nut.2014.12.016. [DOI] [PubMed] [Google Scholar]
- Vors C., Allaire J., Marin J., Lépine M.C., Charest A., Tchernof A., Couture P., Lamarche B. Inflammatory gene expression in whole blood cells after EPA vs. DHA supplementation: results from the ComparED study. Atherosclerosis. 2017;257:116–122. doi: 10.1016/j.atherosclerosis.2017.01.025. [DOI] [PubMed] [Google Scholar]
- Vulevic J., Juric A., Tzortzis G., Gibson G.R. A mixture of trans-galactooligosaccharides reduces markers of metabolic syndrome and modulates the fecal microbiota and immune function of overweight adults. J. Nutr. 2013;143:324–331. doi: 10.3945/jn.112.166132. [DOI] [PubMed] [Google Scholar]
- Wada M., DeLong C.J., Hong Y.H., Rieke C.J., Song I., Sidhu R.S., Yuan C., Warnock M., Schmaier A.H., Yokoyama C., Smyth E.M., Wilson S.J., FitzGerald G.A., Garavito R.M., Sui d.X., Regan J.W., Smith W.L. Enzymes and receptors of prostaglandin pathways with arachidonic acid-derived versus eicosapentaenoic acid-derived substrates and products. J. Biol. Chem. 2007;282:22254–22266. doi: 10.1074/jbc.M703169200. [DOI] [PubMed] [Google Scholar]
- Wang C.C., Goalstone M.L., Draznin B. Molecular mechanisms of insulin resistance that impact cardiovascular biology. Diabetes. 2004;53:2735–2740. doi: 10.2337/diabetes.53.11.2735. [DOI] [PubMed] [Google Scholar]
- Wang S., Zhao X., Yang S., Chen B., Shi J. Salidroside alleviates high glucose-induced oxidative stress and extracellular matrix accumulation in rat glomerular mesangial cells by the TXNIP-NLRP3 inflammasome pathway. Chem. Biol. Interact. 2017;278:48–53. doi: 10.1016/j.cbi.2017.10.012. [DOI] [PubMed] [Google Scholar]
- Weisberg S.P., McCann D., Desai M., Rosenbaum M., Leibel R.L., Ferrante A.W., Jr. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Invest. 2003;112:1796–1808. doi: 10.1172/JCI19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2013. 10 Facts on Noncommunicable Diseases. [Google Scholar]
- WHO . 2018. Noncommunicable Diseases Fact Sheets. [Google Scholar]
- WHO . 2020. Nutrition Advice for Adults during the COVID-19 Outbreak. [Google Scholar]
- Widmer R.J., Freund M.A., Flammer A.J., Sexton J., Lennon R., Romani A., Mulinacci N., Vinceri F.F., Lerman L.O., Lerman A. Beneficial effects of polyphenol-rich olive oil in patients with early atherosclerosis. Eur. J. Nutr. 2013;52:1223–1231. doi: 10.1007/s00394-012-0433-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winer S., Paltser G., Chan Y., Tsui H., Engleman E., Winer D., Dosch H.M. Obesity predisposes to Th17 bias. Eur. J. Immunol. 2009;39:2629–2635. doi: 10.1002/eji.200838893. [DOI] [PubMed] [Google Scholar]
- Wittekindt O.H. Tight junctions in pulmonary epithelia during lung inflammation. Pflügers Archiv. 2017;469:135–147. doi: 10.1007/s00424-016-1917-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff G., Taranko A.E., Meln I., Weinmann J., Sijmonsma T., Lerch S., Heide D., Billeter A.T., Tews D., Krunic D., Fischer-Posovszky P., Muller-Stich B.P., Herzig S., Grimm D., Heikenwalder M., Kao W.W., Vegiopoulos A. Diet-dependent function of the extracellular matrix proteoglycan Lumican in obesity and glucose homeostasis. Mol. Metab. 2019;19:97–106. doi: 10.1016/j.molmet.2018.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C.Y., Yiu K.H., Li S.W., Lee S., Tam S., Lau C.P., Tse H.F. Fish-oil supplement has neutral effects on vascular and metabolic function but improves renal function in patients with Type 2 diabetes mellitus. Diabet. Med. 2010;27:54–60. doi: 10.1111/j.1464-5491.2009.02869.x. [DOI] [PubMed] [Google Scholar]
- Yamamoto K., Itoh T., Abe D., Shimizu M., Kanda T., Koyama T., Nishikawa M., Tamai T., Ooizumi H., Yamada S. Identification of putative metabolites of docosahexaenoic acid as potent PPARgamma agonists and antidiabetic agents. Bioorg. Med. Chem. Lett. 2005;15:517–522. doi: 10.1016/j.bmcl.2004.11.053. [DOI] [PubMed] [Google Scholar]
- Youm Y.H., Nguyen K.Y., Grant R.W., Goldberg E.L., Bodogai M., Kim D., D'Agostino D., Planavsky N., Lupfer C., Kanneganti T.D., Kang S., Horvath T.L., Fahmy T.M., Crawford P.A., Biragyn A., Alnemri E., Dixit V.D. The ketone metabolite beta-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat. Med. 2015;21:263–269. doi: 10.1038/nm.3804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yubero-Serrano E.M., Gonzalez-Guardia L., Rangel-Zuniga O., Delgado-Lista J., Gutierrez-Mariscal F.M., Perez-Martinez P., Delgado-Casado N., Cruz-Teno C., Tinahones F.J., Villalba J.M., Perez-Jimenez F., Lopez-Miranda J. Mediterranean diet supplemented with coenzyme Q10 modifies the expression of proinflammatory and endoplasmic reticulum stress-related genes in elderly men and women. J. Gerontol. A Biol. Sci. Med. Sci. 2012;67:3–10. doi: 10.1093/gerona/glr167. [DOI] [PubMed] [Google Scholar]
- Zadeh-Ardabili P.M., Rad S.K. Anti-pain and anti-inflammation like effects of Neptune krill oil and fish oil against carrageenan induced inflammation in mice models: current statues and pilot study. Biotechnol. Rep. (Amst.) 2019;22 doi: 10.1016/j.btre.2019.e00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanfirescu A., Ungurianu A., Tsatsakis A.M., Nitulescu G.M., Kouretas D., Veskoukis A., Tsoukalas D., Engin A.B., Aschner M., Margina D. A review of the alleged health hazards of monosodium glutamate. Compr. Rev. Food Sci. Food Saf. 2019;18:1111–1134. doi: 10.1111/1541-4337.12448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y.Y., Liu W., Zhao T.Y., Tian H.M. Efficacy of omega-3 polyunsaturated fatty acids supplementation in managing overweight and obesity: a meta-analysis of randomized clinical trials. J. Nutr. Health Aging. 2017;21:187–192. doi: 10.1007/s12603-016-0755-5. [DOI] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou R., Tardivel A., Thorens B., Choi I., Tschopp J. Thioredoxin-interacting protein links oxidative stress to inflammasome activation. Nat. Immunol. 2010;11:136–140. doi: 10.1038/ni.1831. [DOI] [PubMed] [Google Scholar]
- Zhu L., Sha L., Li K., Wang Z., Wang T., Li Y., Liu P., Dong X., Dong Y., Zhang X., Wang H. Dietary flaxseed oil rich in omega-3 suppresses severity of type 2 diabetes mellitus via anti-inflammation and modulating gut microbiota in rats. Lipids Health Dis. 2020;19:20. doi: 10.1186/s12944-019-1167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Ling W., Guo H., Song F., Ye Q., Zou T., Li D., Zhang Y., Li G., Xiao Y., Liu F., Li Z., Shi Z., Yang Y. Anti-inflammatory effect of purified dietary anthocyanin in adults with hypercholesterolemia: a randomized controlled trial. Nutr. Metabol. Cardiovasc. Dis. 2013;23:843–849. doi: 10.1016/j.numecd.2012.06.005. [DOI] [PubMed] [Google Scholar]