With increasing urbanization, exposure to environmental noise and air pollution is growing. A recent update to the World Health Organization's Environmental Noise Guidelines corroborates that noise poses a risk to public health, but also shows that high‐quality epidemiologic studies are still missing for several noise sources and health outcomes.1 The study by Shin et al in this issue of the Journal of the American Heart Association (JAHA) is a large retrospective cohort study that utilized the Ontario Population Health and Environment Cohort (ONPHEC), a cohort of Canadian‐born people of Ontario who were 35 years or older in 1996 with follow‐up data until 2014, to investigate the effects of road traffic noise on incident diabetes mellitus and hypertension.2 The current study was restricted to individuals who resided in Toronto for at least 5 years, and were free of hypertension (n=701 174) or type 2 diabetes mellitus (T2D; n=914 607). Using spatial random‐effects Cox proportional hazards models, with Toronto neighborhoods as random effects, Shin et al estimate that a 10 dBA increase in 24 hours road traffic noise was associated with an 8% elevated risk of diabetes mellitus and a 2% elevated risk of hypertension. These estimates were robust to adjustments for 2 common traffic pollutants: ultrafine particulate matter (UFP) and nitrogen dioxide (NO2).
The identified links of both hypertension and type 2 diabetes mellitus incidences with urban traffic noise are important because across the world, obesity and diabetes mellitus are increasing at alarming rates in developed and in developing countries.3 Although much research has been focused on the role of diet and physical activity,4 recent reports suggest that urbanization, accompanied by migration to more polluted areas5 (including with light6 and air7 pollution) and our modern 24‐hour lifestyle (wherein 35% of adults sleep less than the recommended 7 to 8 hours sleep per night8, 9) could be significant factors fueling the worldwide increase in CVD and type 2 diabetes mellitus.10, 11, 12 The current study contributes to our understanding that noise is an environmental factor that exerts a significant effect on our biology (Figure). Mechanistically, it is thought that (as depicted) noise stimulates an auditory afferent that activates the amygdala, and subsequent efferent output from the autonomic nervous system includes both release of corticotropic releasing hormone (hypothalamus) and increased cortisol (adrenal cortex) and neurally‐triggered catecholamine release (adrenal medulla). Likewise, both pulmonary and olfactory sensory afferents are implicated in mediating air pollution exposure‐dependent central nervous system activation with efferents likely including both autonomic nervous system stimulation (shared pathway with noise) and release of circulating inflammatory mediators. Collectively, these efferents mediate systemic “stress responses” that may increase insulin resistance, inflammation, disturb sleep, etc.
Figure 1.
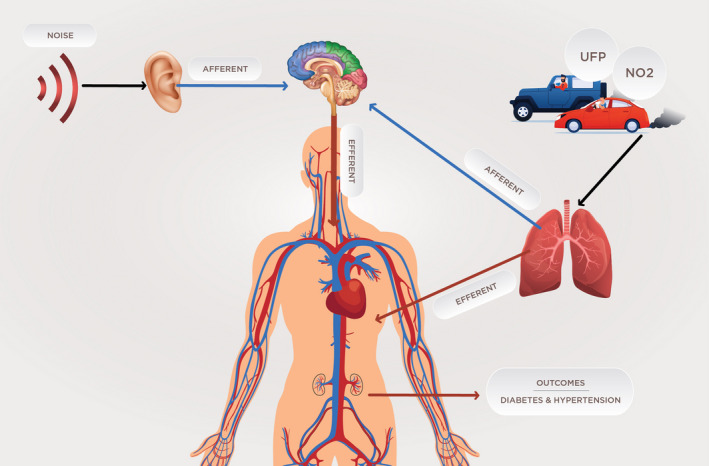
Environmental determinants of cardiometabolic disease include noise and traffic‐derived air pollutants (ultrafine particles, UFP; nitrogen dioxide, NO 2). Noise had a stronger effect on hypertension and type 2 diabetes mellitus (T2D) during the nighttime than during the daytime or when levels of UFP and NO 2 were higher. Individual level (personal domain) risk factors (obesity, smoking) did not substantially alter these associations. This study clearly suggests that the effects of chronic noise on incident T2D and hypertension depend on the levels of UFP and NO 2, but the exact nature of this relationship warrants further investigation. Future prospective, longitudinal studies with noise as the primary exposure of interest (and not just as an afterthought) as well as animal studies using appropriate chronic noise exposure conditions are required to disentangle the effects of simultaneous exposures to air pollution and noise. Arrows represent environmental determinants (black) and pathways into (afferent; blue) and away from (efferent; red) the central nervous system (CNS: brain and spinal cord) that may contribute to cardiometabolic disease. As depicted, it is thought that noise stimulates an auditory afferent that activates the amygdala, and subsequent efferent output from the autonomic nervous system (ANS) includes both (1) release of corticotropic releasing hormone (hypothalamus) and then increased cortisol (adrenal cortex); and, (2) neurally‐triggered catecholamine release (adrenal medulla). Likewise, both pulmonary and olfactory sensory afferents are implicated in mediating air pollution exposure–dependent CNS activation with efferents likely including both ANS stimulation (a shared pathway with noise) and release of circulating inflammatory mediators. Collectively, these efferents mediate systemic “stress responses” that may increase insulin resistance, inflammation, disturb sleep, etc. It is possible that answers to the questions about how these determinants actually promote cardiometabolic disease may well be found “in the noise.”
This study continues a trend of studies that leverage large existing health databases to investigate the effects of noise on diverse health outcomes. However, these studies often lack spatial precision (eg, locations only available at zip‐code level13) and relevant confounders at the individual level.14 While the former leads to exposure misclassification that biases the results towards the null, the latter introduces ecologic features that can also produce a bias away from the null. This study stands out as it addresses some of these shortcomings with multilevel analysis to account for correlated factors within neighborhoods and various sensitivity analyses, including indirect adjustments of smoking and obesity. While leveraging existing data sets is a cost‐effective and commendable approach in general, noise exposure is always an afterthought in these studies (ie, they were not designed with noise as the main exposure of interest in mind). To our knowledge, a large prospective cohort study that is primarily dedicated to the effects of environmental noise exposure on health is still missing.
Despite the fact that daytime and nighttime noise levels were highly correlated, at the same average noise level, the study by Shin et al finds stronger effects for nighttime road noise exposure compared with daytime exposure.2 Overall, this is in line with previous epidemiologic studies.15 Part of this difference may be explained by the fact that people spend more time at home during the night, ie, fewer exposure misclassifications. Moreover, it also emphasizes the importance of undisturbed sleep of sufficient duration for health and well‐being.16 Different noise scenarios may calculate to the same average noise level but differ in the physiologic reactions they elicit. Laboratory and field studies have demonstrated that single event metrics (eg, the maximum sound pressure level of an aircraft) outperform average noise levels in predicting the degree of sleep disturbance.17 Future studies should investigate whether the steadiness of the noise (eg, intermittency ratio18) or even the predicted degree of sleep disturbance are better predictors of health outcomes relative to average noise levels.
Because noise and air pollution levels also are typically correlated, especially for road traffic noise, it is important to disentangle the individual contributions. In stratified analyses, this study finds that the effect of noise exposure on both diabetes mellitus and hypertension prevalence decreases with increasing UFP and NO2 exposure levels. While the latter 2 measures only partly represent air pollution (traffic pollution is a complex mixture of particles and gases, including PM2.5 and volatile organic compounds), the finding is intriguing because it suggests that the health effects of noise depend on the degree of air pollution, and likely vice versa. Prior studies have shown that both noise and air pollution independently contribute to negative health outcomes,19 yet little is known about whether these effects are additive, less than additive, or even synergistic. This study suggests that noise plays a less important role if air pollution levels are high, and the authors will hopefully follow up with a publication that more closely investigates the complex relationship between noise and air pollution measures relative to cardiometabolic health risks.
In conclusion, epidemiological studies indicate that 60% to 70% of the premature mortality attributed to exposure to ambient air pollution are cardiovascular deaths, and with increased urbanization,7 the disease burden of air pollution is likely to increase.20 Thus, in future prospective studies, analyses to address important questions about the nature of interactions between myriad environmental determinants should be incorporated. Similarly, animal models can be used to disentangle the influences of noise and air pollution effects as well as address the mechanistic bases of these pathways. However, it will be important to use realistic chronic noise exposure models rather than models that use short and extreme exposures in an effort to reduce cost and time. Finally, the authors are commended for their sophisticated approach to overcome limitations in the data, including validated traffic noise and pollution estimates, and for raising awareness of the potential cardiometabolic effects of noise above the din.
Sources of Funding
Research funding was received from the National Institutes of Health (P20GM127607, R01HL122676, U54HL120163).
Disclosures
Dr M. Basner is currently president of the International Commission of Biological Effects of Noise (ICBEN); he has consulted for the World Health Organization on the effects of noise on sleep; and, he has consulted and is consulting in legal cases related to the health effects of noise.
Acknowledgments
We thank A. Langan for preparation of the figure.
J Am Heart Assoc. 2020;9:e016048 DOI: 10.1161/JAHA.120.016048.
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1. World Health Organization . Environmental Noise Guidelines for the European Region. Copenhagen, Denmark: WHO Regional Office for Europe; 2018. [Google Scholar]
- 2. Shin S, Bai L, Oiamo TH, Burnett RT, Weichenthal S, Jerrett M, Kwong JC, Goldberg MS, Copes R, Kopp A, Chen H. Association between road traffic noise and incidence of diabetes mellitus and hypertension in Toronto, Canada: a population‐based cohort study. J Am Heart Assoc. 2020;9:e013021 DOI: 10.1161/JAHA.119.013021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Global Burden of Metabolic Risk Factors for Chronic Diseases C . Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2:634–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gaesser GA. Exercise for prevention and treatment of cardiovascular disease, type 2 diabetes, and metabolic syndrome. Curr Diab Rep. 2007;7:14–19. [DOI] [PubMed] [Google Scholar]
- 5. United Nations DoEaSA, Population Division . World Urbanization Prospects: the 2018 Revision. 2019:103.
- 6. Chepesiuk R. Missing the dark: health effects of light pollution. Environ Health Perspect. 2009;117:A20–A27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Han L, Zhou W, Li W, Qian Y. Urbanization strategy and environmental changes: an insight with relationship between population change and fine particulate pollution. Sci Total Environ. 2018;642:789–799. [DOI] [PubMed] [Google Scholar]
- 8. Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of healthy sleep duration among adults—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65:137–141. [DOI] [PubMed] [Google Scholar]
- 9. Schoenborn CA, Adams PE. Health behaviors of adults: United States, 2005–2007. Vital Health Stat 10. 2010;245:1–132. [PubMed] [Google Scholar]
- 10. Pearson JF, Bachireddy C, Shyamprasad S, Goldfine AB, Brownstein JS. Association between fine particulate matter and diabetes prevalence in the U.S. Diabetes Care. 2010;33:2196–2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Navara KJ, Nelson RJ. The dark side of light at night: physiological, epidemiological, and ecological consequences. J Pineal Res. 2007;43:215–224. [DOI] [PubMed] [Google Scholar]
- 12. Hutcheson R, Rocic P. The metabolic syndrome, oxidative stress, environment, and cardiovascular disease: the great exploration. Exp Diabetes Res. 2012;2012:271028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Correia AW, Peters JL, Levy JI, Melly S, Dominici F. Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: multi‐airport retrospective study. BMJ. 2013;347:f5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hansell AL, Blangiardo M, Fortunato L, Floud S, de Hoogh K, Fecht D, Ghosh RE, Laszlo HE, Pearson C, Beale L, Beevers S, Gulliver J, Best N, Richardson S, Elliott P. Aircraft noise and cardiovascular disease near Heathrow airport in London: small area study. BMJ. 2013;347:f5432. [DOI] [PubMed] [Google Scholar]
- 15. Hume KI, Brink M, Basner M. Effects of environmental noise on sleep. Noise Health. 2012;14:297–302. [DOI] [PubMed] [Google Scholar]
- 16. Basner M, McGuire S. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health. 2018;15:E519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Basner M, Müller U, Griefahn B. Practical guidance for risk assessment of traffic noise effects on sleep. Appl Acoust. 2010;71:518–522. [Google Scholar]
- 18. Wunderli JM, Pieren R, Habermacher M, Vienneau D, Cajochen C, Probst‐Hensch N, Roosli M, Brink M. Intermittency ratio: a metric reflecting short‐term temporal variations of transportation noise exposure. J Expo Sci Environ Epidemiol. 2016;26:575–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gan WQ, Davies HW, Koehoorn M, Brauer M. Association of long‐term exposure to community noise and traffic‐related air pollution with coronary heart disease mortality. Am J Epidemiol. 2012;175:898–906. [DOI] [PubMed] [Google Scholar]
- 20. Pope CA III, Turner MC, Burnett RT, Jerrett M, Gapstur SM, Diver WR, Krewski D, Brook RD. Relationships between fine particulate air pollution, cardiometabolic disorders, and cardiovascular mortality. Circ Res. 2015;116:108–115. [DOI] [PubMed] [Google Scholar]


