Abstract
Background:
Patient reported outcomes (PROs) are a valid measure of results following revision anterior cruciate ligament (ACL) reconstruction. Revision ACL reconstruction has been documented to have worse outcomes compared with primary ACL reconstructions. Understanding positive and negative predictors of PROs will allow surgeons to modify and potentially improve outcome for these patients.
Hypothesis/Purpose:
The purpose of this study was to describe PROs following revision ACL reconstruction and test the hypothesis that patient and technique specific variables are associated with these outcomes.
Study Design:
Cohort study
Methods:
Revision ACL reconstruction patients were identified and prospectively enrolled by 83 surgeons over 52 sites. Data collected included baseline demographics, surgical technique and pathology, and a series of validated PRO instruments (IKDC, KOOS, WOMAC and Marx activity rating score). Patients were followed up at 2 years, and asked to complete the identical set of outcome instruments. Multivariate regression models were used to control for a variety of demographic and surgical factors, in order to determine both the positive and negative predictors of PRO scores at 2 years following revision surgery.
Results:
1205 patients met the inclusion criteria and were successfully enrolled. 697 (58%) were males, with a median cohort age of 26 years. The median time since their last ACL reconstruction was 3.4 years. Two-year questionnaire follow-up was obtained on 989 subjects (82%).
The most significant positive predictors of 2-year IKDC scores were a high baseline IKDC score, high baseline Marx activity level, male gender, and having a longer time between a patient’s last ACL reconstruction, while negative predictors included having a previous lateral meniscectomy prior to the revision ACL reconstruction or having Grades 3/4 chondrosis in either the trochlear groove or medial tibial plateau at the time of the revision surgery. For KOOS, having a high baseline score and having a longer time between their last ACL reconstruction and revision surgery were significant positive predictors for having better (i.e. higher) 2-year KOOS scores, while having a previous lateral meniscectomy prior to the revision ACL reconstruction was a consistent predictor for having significantly worse (i.e. lower) 2-year KOOS scores. Statistically significant positive predictors for 2-year Marx activity levels included higher baseline Marx activity levels, younger age, male gender, and being a non-smoker. Negative 2-year activity level predictors included having an allograft or a biologic enhancement at the time of revision surgery.
Conclusions:
PROs following revision ACL reconstruction are associated with a variety of patient and surgeon related variables. Understanding positive and negative predictors of PROs will allow surgeons to guide patient expectation as well as potentially improve outcome for these patients.
Keywords: ACL reconstruction, revision, outcomes, IKDC, KOOS, Marx
INTRODUCTION
Revision anterior cruciate ligament (ACL) reconstruction has been noted to have worse outcomes than primary ACL reconstructions by a variety of measures, including graft failure rates and patient reported outcomes.7,9,26,28,27 The reasons for these worse outcomes have not been readily apparent and unfortunately the medical literature is replete with lower level retrospective series and few Level 1 or 2 studies. Based on this lack of understanding of this significant clinical problem, the Multicenter ACL Revision Study (MARS) consortium was developed to attempt to better understand the contributors and predictors for these worse outcomes.16
Previous analyses of this cohort by the MARS Group have been performed to assess the impact of graft choice, meniscal and chondral factors, rehabilitation variables, surgeon technical issues and cross-cultural comparisons that impact outcome, but no previous analysis has combined all available, practical variables into a common analysis to stratify the predictors.1–4,8,10–16 Patient reported outcomes (PROs) have become accepted and popular in medicine and subsequently in orthopaedics.17,18,23–25 Identifying predictors of these measures following revision ACL reconstruction will identify opportunities for counseling and care for patients undergoing this surgery. The purpose of this study was to describe PROs following revision ACL reconstruction and test the hypothesis that patient and technique specific variables are associated with these outcomes.
METHODS
The MARS Group was assembled with the aim of determining what impacts outcome in an ACL revision setting, and to identify potentially modifiable factors that could improve these outcomes. This collaboration consists of a group of 83 sports medicine fellowship trained surgeons across 52 sites. Surgeons are a near equal mix of academic and private practitioners. After obtaining approval from respective institutional review boards (IRBs), this multicenter consortium began patient enrollment in 2006 and ended in 2011, during which time 1205 revision ACL reconstruction patients were enrolled in this prospective longitudinal cohort. The study enrolled patients undergoing revision of a previously failed ACL reconstruction who agreed to participate, signed an informed consent, and completed a series of patient-reported outcome instruments. Indications for the revision ACL reconstruction included functional instability, abnormal laxity testing or an MRI indicating graft tear. Multi-ligament reconstructions were excluded. Surgeon inclusion criteria included maintenance of an active IRB approval, completion of a training session that integrated articular cartilage and meniscus agreement studies, review of the study design and patient inclusion criteria, and a review of the surgeon questionnaire. Surgical technique was at the discretion of the treating surgeon. All allografts were obtained from a single allograft supplier (Musculoskeletal Transplant Foundation; Edison, NJ).
Data Sources and Measurement
After obtaining informed consent, the patient filled out a 13-page questionnaire that included questions regarding demographics, sports participation, injury mechanism, comorbidities and knee injury history, as previously described.16 Within this questionnaire, each participant also completed a series of validated general and knee-specific outcome instruments, including the Knee Injury and Osteoarthritis Outcome Score (KOOS), the International Knee Documentation Committee Subjective form (IKDC) and the Marx activity rating scale. Contained within the KOOS was the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Surgeons filled out a 42-page questionnaire that included the impression of the etiology (traumatic, technical and/or biologic) of the previous failure, physical exam findings, surgical technique utilized, the intra-articular findings and surgical management of meniscal and chondral damage.
Completed data forms were mailed from each participating site to the data coordinating center. Data from both the patient and surgeon questionnaires were scanned with Teleform™ software (OpenText; Waterloo, Ontario, Canada) utilizing optical character recognition, and the scanned data was verified and exported to a master database. A series of logical error and quality control checks were subsequently performed prior to data analysis.
Patient Follow-up
Two-year patient follow-up was completed by mail with re-administration of the same questionnaire as the one they completed at baseline. Patients were also contacted by phone to determine whether any subsequent surgery had occurred to either knee since their initial revision ACL reconstruction. If so, operative reports were obtained, whenever possible, in order to document pathology and treatment.
Statistical Analysis
To describe our patient sample, we summarized continuous variables as percentiles (i.e., 25th, 50th, and 75th), and categorical variables with frequencies and percentages. Multivariable regression analyses were constructed to examine which baseline risk factors were independently associated with each outcome variable. The primary outcome variables of interest were the 2-year outcome scores of the IKDC, KOOS, WOMAC and Marx activity level. These primary outcome variables were all treated as continuous. Regression analysis was used to control for age, gender, body mass index (BMI), activity level, smoking status, number of years of education, baseline outcome scores, surgeon, revision number, time from previous ACL reconstruction, and a variety of previous and current surgical variables, in order to assess the demographic and surgical risk factors for clinical outcomes 2 years after revision surgery. To stay within the allowable degrees of freedom, each continuous variable was tested for a non-linear relationship with a p-value < 0.05 significance level. Statistical analysis was performed using open source R statistical software (www.r-project.org; Version 3.0.3).
RESULTS
Study Population and Follow-up
A total of 1205 patients (697 [58%] males) met the inclusion criteria and were successfully enrolled. The median age was 26 years, and median time since the patients’ last ACL reconstruction was 3.4 years. At 2 years, questionnaire follow-up was obtained on 82% (989/1205).
All outcome scores showed significant improvement from baseline to 2 years, with the exception of the WOMAC stiffness subscale (p<0.001; Table 1). The IKDC, KOOS, and WOMAC pain and ADL subscales all significantly improved at 2 years, while activity level significantly dropped at 2 years as compared to their baseline measure.
Table 1.
Median (25%, 75% quartile) Outcome Scores over Time
| Scale | Baseline (T0)a | 2-Year Follow-upb | |
|---|---|---|---|
| IKDCc | 0–100 | 52 (38,63) | 77 (61,86) |
| KOOSd | 0–100 | ||
| WOMACf | 0–100 | ||
| Marx activity level | 0–16 | 11 (4,16) | 7 (2,12) |
T0 = time at revision ACL reconstruction surgery
scores all significantly changed as compared to baseline (p<0.001), with the exception of the WOMAC stiffness scale.
IKDC = International Knee Documentation Committee “subjective” form
KOOS = Knee injury and Osteoarthritis Outcome Score
ADL = activities of daily living
WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index
Positive and Negative Predictors of 2-Year Outcome Scores
IKDC
The most significant drivers of 2-year IKDC scores were a patient’s, 1) baseline IKDC score (p<0.001); 2) baseline Marx activity level (p<0.001); 3) gender (p<0.001); and, 4) time since their last ACL reconstruction (p=0.003). Specifically, having a high baseline IKDC score, high baseline Marx activity level, male gender, and having a longer time between their last ACL reconstruction were significant positive predictors for having better (i.e. higher) 2-year IKDC scores. A summary of all individual significant positive and negative predictors of 2-year IKDC scores are listed in Table 2.
Table 2.
Significant Predictors for 2-Year IKDC Scores
| Variable | Odds Ratio | 95% CI | p value | |
|---|---|---|---|---|
| Positive Predictors (improved scores) | • Baseline IKDC score | 3.1 | (2.5, 3.7) | <0.001 |
| • Baseline Marx activity level | 2.2 | (1.6, 3.2) | <0.001 | |
| • Time since last ACL Reconstruction (years) | 1.9 | (1.3, 2.8) | 0.003 | |
| • Femoral fixation (interference screw) | 1.8 | (1.0, 3.1) | 0.047 | |
| • Male gender | 1.6 | (1.3, 2.1) | <0.001 | |
| • Tibial fixation (interference screw) | 1.6 | (1.1, 2.2) | 0.007 | |
| • LFC chondrosis (grade 2) | 1.5 | (1.1, 2.2) | 0.023 | |
| • Current graft source: soft tissue | 1.5 | (1.1, 2.2) | 0.025 | |
| Negative Predictors (worse scores) | • MTP chondrosis (grades 3/4) | 0.45 | (0.21, 0.97) | 0.042 |
| • Trochlear chondrosis (grades 3/4) | 0.53 | (0.35, 0.80) | 0.003 | |
| • Previous lateral meniscectomy | 0.59 | (0.41, 0.86) | 0.005 | |
| • Current graft type: allograft | 0.76 | (0.59, 0.99) | 0.045 |
Key: LFC = lateral femoral condyle; MTP = medial tibial plateau
KOOS
The variables that consistently influenced all 2-year KOOS scores were, 1) a patient’s baseline score; 2) the time since their last ACL reconstruction; and, 3) having a previous lateral meniscectomy prior to their revision ACL reconstruction. Specifically, having a high baseline score and having a longer time between a patient’s last ACL reconstruction were significant positive predictors for having better (i.e. higher) 2-year KOOS scores, while having a previous lateral meniscectomy prior to the revision ACL reconstruction was a consistent predictor for having significantly worse (i.e. lower) 2-year KOOS scores across all subscales. Having a high baseline activity level significantly predicted higher 2-year KOOS activities of daily living (ADL), sports and recreation, and quality of life (QOL) scores. Patients who had an interference screw for their tibial fixation also had significantly higher 2-year KOOS scores in four of the five subscales (symptoms, pain, ADL, and sports/recreation). Choosing an autograft for the revision ACL reconstruction predicted significantly higher KOOS sports/recreation and QOL scores at 2 years. Conversely, having Grade 3–4 trochlear groove chondrosis predicted significantly lower 2-year KOOS scores in four of the five subscales (symptoms, pain, ADL, and sports/recreation). A summary of these significant positive and negative predictors of 2-year KOOS scores are listed in Table 3.
Table 3.
Significant Predictors for 2-Year KOOS Scores
| Variable | Symptoms | Pain | ADL | Sports/Rec | QOL |
|---|---|---|---|---|---|
| Positive Predictors | |||||
| • Baseline score | 3.9 (3.1, 4.8); p<0.001 |
3.8 (3.1, 4.8); p<0.001 |
5.1 (3.8, 6.8); p<0.001 |
3.0 (2.4, 3.6); p<0.001 |
2.1 (1.8, 2.6); p<0.001 |
| • Time since last ACL reconstruction (years) | 1.7 (1.1, 2.5); p=0.001 |
1.9 (1.3, 2.8); p=0.001 |
1.9 (1.3, 2.8); p<0.001 |
2.0 (1.4, 3.0); p=0.008 |
1.8 (1.3, 2.7); p=0.003 |
| • Baseline Marx activity level | 1.6 (1.1, 2.4); p=0.007 |
1.8 (1.3, 2.6); p=0.001 |
2.0 (1.4, 2.9); p<0.001 |
||
| • Lateral Meniscus treatment: no treatment for tear | 2.5 (1.3, 4.7); p=0.008 |
||||
| • Femoral fixation (interference screw) | 2.2 (1.3, 4.0); p=0.006 |
||||
| • Tibial fixation (interference screw) | 1.5 (1.1, 2.1); p=0.013 |
1.6 (1.1, 2.2); p=0.007 |
2.0 (1.1, 3.7); p=0.024 |
1.5 (1.0, 2.1) p=0.033 |
|
| • Current graft: autograft | 1.3 (1.0, 1.7) p=0.037 |
1.3 (1.0, 1.7); p=0.031 |
|||
| • Current graft type: soft tissue | 1.5 (1.1, 2.3); p=0.029 |
||||
| Negative Predictors | |||||
| • Current smoker | 0.6 (0.4, 0.9); p=0.012 |
||||
| • Previous ACL Reconstruction on the contralateral knee | 0.7 (0.5, 0.98); p=0.037 |
||||
| • 2nd Revision ACL Reconstruction | 0.6 (0.4, 0.9); p=0.019 |
||||
| • Previous medial meniscectomy | 0.7 (0.5, 0.95); p=0.022 |
0.7 (0.5, 0.9); p=0.006 |
|||
| • Previous lateral meniscectomy | 0.6 (0.4, 0.8); p=0.002 |
0.7 (0.5, 0.9); p=0.019 |
0.6 (0.4, 0.9); p=0.024 |
0.7 (0.5, 0.96); p=0.029 |
0.5 (0.3, 0.7); p<0.001 |
| • Trochlear groove chondrosis (grades 3/4) | 0.6 (0.4, 0.9); p=0.019 |
0.6 (0.4, 0.9); p=0.014 |
0.4 (0.2, 0.6); p<0.001 |
0.5 (0.3, 0.8); p=0.003 |
|
| • MTP chondrosis (grades 3/4) | 0.3 (0.2, 0.7); p=0.002 |
||||
| • LTP chondrosis (grade 2) | 0.7 (0.5, 1.0) p=0.046 |
||||
| • MFC chondrosis (grade 4) | 0.5 (0.3, 0.9); p=0.011 |
||||
| • Surgeon’s opinion on cause of failure: tibial tunnel malposition | 0.4 (0.2, 0.9); p=0.037 |
0.3 (0.1, 0.9); p=0.026 |
|||
Key: numbers listed in each cell are ones which were statistically significant. Listed in the order of Odds Ratio; (95% Confidence Intervals); p-value. MTP = medial tibial plateau; LTP = lateral tibial plateau; MFC = medial femoral condyle; ADL = activities of daily living; Sports/Rec = sports and recreation; QOL = quality of life.
WOMAC
The variables that consistently influenced all 2-year WOMAC scores were, 1) a patient’s baseline WOMAC score; 2) the time since their last ACL reconstruction; 3) having an interference screw for their tibial fixation, and 4) having a previous lateral meniscectomy prior to their revision ACL reconstruction. Specifically, having a high baseline score, a longer time between their last ACL reconstruction, and having an interference screw for tibial fixation were the most consistent significant positive predictors for having better (i.e. higher) 2-year WOMAC scores, while having a previous lateral meniscectomy prior to the revision ACL reconstruction was the most consistent predictor for having significantly worse (i.e. lower) 2-year WOMAC scores.
A summary of individual significant positive and negative predictors of 2-year WOMAC scores are listed in Table 4.
Table 4.
Significant Predictors for 2-Year WOMAC Scores
| Variable | Stiffness | Pain | ADL | |
|---|---|---|---|---|
| Positive Predictors (improved scores) | • Baseline score | 4.3 (3.4, 5.6); p<0.001 |
4.0 (3.0, 5.3); p<0.001 |
5.1 (3.8, 6.8); p<0.001 |
| • Time since last ACL Reconstruction (years) | 1.8 (1.2, 2.6); p=0.003 |
1.7 (1.1, 2.6); p=0.001 |
1.9 (1.3, 2.8); p=0.050 |
|
| • Baseline Marx activity level | 1.6 (1.1, 2.4); p=0.007 |
|||
| • Lateral meniscus treatment: no treatment for tear | 2.5 (1.3, 4.7); p=0.008 |
|||
| • Femoral fixation (interference screw) | 1.8 (1.1, 3.1); p=0.032 |
|||
| • Tibial fixation (interference screw) | 1.7 (1.2, 2.3); p=0.029 |
1.4 (1.0, 2.0); p=0.040 |
2.0 (1.1, 3.7); p=0.024 |
|
| • Surgeon’s years of experience | 1.3 (1.0, 1.6); p=0.022 |
|||
| Negative Predictors (worse scores) | • Previous medial meniscectomy | 0.7 (0.5, 0.9); p=0.010 |
||
| • Previous lateral meniscectomy | 0.7 (0.4, 0.9); p=0.021 |
0.6 (0.4, 0.9); p=0.022 |
0.6 (0.4, 0.9); p=0.024 |
|
| • Trochlear groove chondrosis (grades 3/4) | 0.6 (0.4, 0.96); p=0.030 |
0.4 (0.2, 0.6); p<0.001 |
||
| • Patellar chondrosis (grades 3/4) | 0.6 (0.4, 0.9); p=0.017 |
|||
| • Surgeon’s opinion on cause of failure: traumatic | 0.4 (0.1, 0.96); p=0.042 |
|||
| • Surgeon’s opinion on cause of failure: tibial tunnel malposition | 0.4 (0.2, 0.9); p=0.037 |
Key: ADL = activities of daily living
Marx Activity Level
The significant drivers of 2-year Marx activity levels were a patient’s, 1) baseline Marx activity level; 2) age; and 3) gender (all p<0.001; Table 5). Specifically, having a high baseline Marx activity level, younger age, and male gender were the most significant positive predictors for having a higher 2-year Marx activity level. Other positive predictive variables for 2-year activity levels were being a non-smoker, while negative predictors included having an allograft and a biologic enhancement (typically platelet rich plasma).
Table 5.
Significant Predictors for 2-Year Marx Activity Level
| Variable | Odds Ratio | 95% CI | p value | |
|---|---|---|---|---|
| Positive Predictors (improved scores) | • Baseline Marx activity level | 5.8 | (4.0, 8.4) | <0.001 |
| • Younger age | 2.2 | (1.4, 3.2) | <0.001 | |
| • Male gender | 1.8 | (1.4, 2.3) | <0.001 | |
| • Non-smoker | 1.7 | (1.1, 2.7) | 0.018 | |
| • Surgeon’s own failure | 1.5 | (1.1, 2.2) | 0.017 | |
| Negative Predictors (worse scores) | • Current graft type: allograft | 0.30 | (0.13, 0.70) | 0.005 |
| • Surgeon’s opinion of failure: “traumatic” | 0.33 | (0.12, 0.92) | 0.033 | |
| • Biologic enhancement | 0.55 | (0.33, 0.90) | 0.019 | |
| • Having a previous ACL Reconstruction on the contralateral knee | 0.67 | (0.45, 0.99) | 0.047 | |
| • Prior graft type: autograft | 0.69 | (0.50, 0.96) | 0.027 |
A summary of individual significant positive and negative predictors of 2-year Marx activity level are listed in Table 5 and Figure 1.
Figure 1.
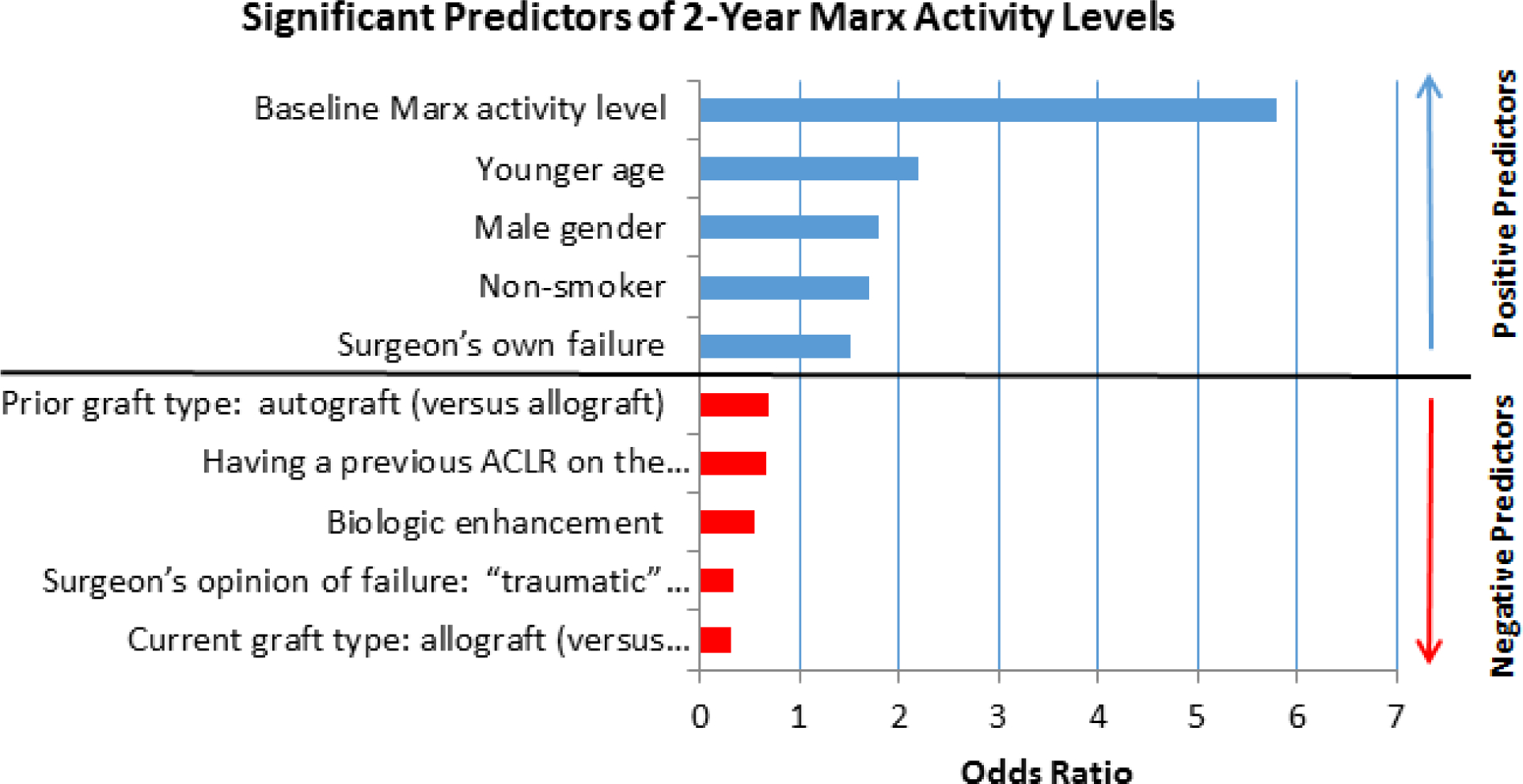
Significant predictors of 2-year Marx activity levels. ACLR, anterior cruciateligament reconstruction.
DISCUSSION
Revision ACL reconstruction unfortunately does not always result in outcomes equivalent to a patient’s results from the primary reconstruction. The current study reports two-year PROs for a large, prospective cohort of revision ACL reconstructions and identifies predictors for these outcomes. In general PROs at two years were improved over baseline both statistically and clinically. Marx activity score was the real exception to improvement with decreased activity at two years (Table 1). Higher baseline scores were associated with higher two year outcomes scores for all of the PROs included in this study. Longer time from previous ACL reconstruction predicted higher IKDC, KOOS and WOMAC scores while males were predicted to have higher IKDC and Marx scores. Previous partial lateral meniscectomy predicted lower WOMAC and KOOS scores at two-year follow-up.
The predictors for better or worse results become invaluable for surgeons managing these patients for two reasons; 1) counseling patients on expected outcome; and, 2) modifying the treatment plan when appropriate. These results allow improved care for both of these reasons. Obvious preoperative factors that portend a good or poor result can be communicated to the patient and technical factors identified can be incorporated into the surgical management to improve outcome.
The use of PROs for assessing patient outcome has become accepted in sports medicine as well as in the broader orthopaedic surgery community. This has not always been true. As recently as 2005, the use of PROs was editorialized as an invalidated assessment that was inferior to structural factors in determining outcome.21,29. This despite surgeon’s intuitive knowledge that asking a patient how they were functioning was as informative as measuring structural outcomes. As the use of PROs has become more mainstream, we have developed an increased understanding of their role and statistical integrity.17,18,23–25
The use of PROs has facilitated the development of large patient cohorts that creates the opportunity to assess a large number of variables that are involved in patient treatment. In revision ACL reconstruction this has included as many as 80 variables in an analysis of > 1000 patients. While it lacks ability to provide some of the data available from physical exams and imaging, it serves a valuable role in assessing innumerable factors and with modern sophisticated statistical methods, independent predictors can be determined for a variety of outcomes.
This study is unique in the field of revision ACL reconstruction. No previous studies have had the ability to assess outcome predictors due to lack of adequate numbers of subjects for analysis. Previous primary ACL reconstruction studies have looked at these predictors, but as health care professionals know the revision setting is a different and more complex reconstruction scenario. Thus, comparing and contrasting our findings with other studies is difficult. To put our PRO results in perspective, an analysis of median PRO scores in Table 1 finds that the median KOOS subscale scores are at the definition of a “symptomatic knee” as described by Wasserstein et al.22 and defined by Englund et al. as a KOOS QOL score ≤ 87.5, and two or more of the following: 1.) KOOS Pain ≤ 86.1, 2.) KOOS Symptoms ≤ 85.7, 3.) KOOS ADL ≤ 86.8, 4.) KOOS Sports/Recreation ≤ 85.0.6 Our median scores would meet these criteria for the KOOS QOL (56), KOOS Symptoms (79), and KOOS Sports/Recreation (75) subscale scores. Thus at least 50% of our patients may meet the criteria for a symptomatic knee at 2-year follow up.
Dunn et al. in analyzing the predictors of activity level at 2 years in the MOON cohort found that higher baseline activity (Marx score), and lower baseline BMI predicted higher (more active) scores.5 Predictors for lower activity level scores included female gender, smoking and interestingly, revision ACL reconstruction. Similar to the findings in the current study were that meniscus and cartilage status did not predict 2-year activity level scores. In the current revision cohort, male gender and being a nonsmoker predicted increased activity level scores at 2 years. A variety of factors specific to the revision setting were impactful, but would not be involved with a primary reconstruction.
Spindler et al. in a MOON study analyzing predictors of activity and sports function at six years following ACL reconstruction found the use of an allograft predicted poorer IKDC, KOOS Sports/Recreation and KOOS QOL scores.20 Higher baseline BMI predicted poorer IKDC and KOOS Sports/Recreation scores at 6 years, and baseline smoking predicted poorer IKDC scores at 6 years. Lateral meniscus status predicted the KOOS Sports/Recreation and KOOS QOL scores. If the patient had undergone a revision ACL reconstruction, poorer IKDC, MARX and all KOOS subscales were predicted. Early acknowledgement of the impact of revision ACL reconstruction in the MOON cohort was the impetus for the development of MARS.
Interestingly, when examining PROs in that predominantly primary cohort at 6 years the scores are no worse and typically improved compared to the current MARS study findings at 2 years.19 The median IKDC score was identical at 77. The KOOS Sports/Recreation subscale score was 90 for MOON vs. 75 at 2 years for MARS. The KOOS QOL subscale score was 81 for MOON and 56 for MARS. Thus, at 2 years revision patients are doing significantly worse than primary ACL patients at 6 years with some but not all measures. The caveat is that the comparison is not adjusted for confounding factors such as patient age, gender, etc.
Consistent with all cohort studies there are limitations imposed by the study design. We do not have quantitative measures of laxity or arthritis at 2-year follow-up (e.g., KT-1000, radiographs). This will be addressed by onsite follow-up at 10 years. The strengths are that this is the largest prospectively enrolled revision ACL reconstruction cohort reported to date, validated PROs collected at baseline and two years and the generalizability of our cohort by including private and academic fellowship trained sports medicine physicians from a variety of geographic and practice settings.
CONCLUSIONS
This is the largest cohort to date reporting two-year PROs for patients undergoing revision ACL reconstruction. Factors associated with two-year PROs were identified, including baseline PRO scores, patient age and sex, time from previous ACL reconstruction and history of a previous partial lateral meniscectomy. Understanding predictors of these scores helps surgeons guide patient expectations and optimize surgical technique.
What is known about the subject:
Revision ACL reconstruction has worse results than primary reconstructions. Patient reported outcomes demonstrate these worse outcomes, but predictors of these worse outcomes have not been known.
What this study adds to existing knowledge: Negative and positive predictors for patient reported outcomes are demonstrated for a variety of PROs including KOOS, IKDC and Marx.
Acknowledgements:
This study received funding from the AOSSM, Smith & Nephew, National Football League Charities, and Musculoskeletal Transplant Foundation. This project was partially funded by grant No. 5R01-AR060846 from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Contributor Information
Laura J. Huston, Vanderbilt University, Nashville, TN USA;.
Amanda K. Haas, Washington University in St. Louis, St. Louis, MO USA;.
Christina R. Allen, University of California, San Francisco, San Francisco, California USA;.
Allen F. Anderson, Tennessee Orthopaedic Alliance, Nashville, TN USA;.
Daniel E. Cooper, W.B. Carrell Memorial Clinic, Dallas, TX USA;.
Thomas M. DeBerardino, The San Antonio Orthopaedic Group, San Antonio, TX USA;.
Warren R. Dunn, Reedsburg Area Medical Center, Reedsburg, WI USA;.
Brett (Brick) A. Lantz, Slocum Research and Education Foundation, Eugene, OR USA;.
Barton Mann, AOSSM, Rosemont, IL USA;.
Kurt P. Spindler, Cleveland Clinic, Cleveland, OH USA;.
Michael J. Stuart, Mayo Clinic, Rochester, MN USA;.
Samuel K. Nwosu, Vanderbilt University, Nashville, TN USA;.
John P. Albright, University of Iowa Hospitals and Clinics, Iowa City, IA USA,.
Annunziato (Ned) Amendola, Duke University, Durham, NC USA;.
Jack T. Andrish, Cleveland Clinic, Cleveland, OH USA;.
Christopher C. Annunziata, Commonwealth Orthopaedics & Rehabilitation, Arlington, VA USA;.
Robert A. Arciero, University of Connecticut Health Center, Farmington, CT USA;.
Bernard R. Bach, Jr, Rush University Medical Center, Chicago, IL USA;.
Champ L. Baker, III, The Hughston Clinic, Columbus, GA USA;.
Arthur R. Bartolozzi, 3B Orthopaedics, University of Pennsylvania Health System, Philadelphia, PA USA;.
Keith M. Baumgarten, Orthopedic Institute, Sioux Falls, SD USA;.
Jeffery R. Bechler, University Orthopaedic Associates LLC, Princeton, NJ USA;.
Jeffrey H. Berg, Town Center Orthopaedic Associates, Reston, VA USA;.
Geoffrey A. Bernas, State University of New York at Buffalo, Buffalo, NY;.
Stephen F. Brockmeier, University of Virginia, Charlottesville, VA USA;.
Robert H. Brophy, Washington University in St. Louis, St. Louis, MO USA;.
Charles A. Bush-Joseph, Rush University Medical Center, Chicago, IL USA;.
J. Brad Butler, V, Orthopedic and Fracture Clinic, Portland, OR USA;.
John D. Campbell, Bridger Orthopedic and Sports Medicine, Bozeman, MT USA;.
James L. Carey, University of Pennsylvania, Philadelphia, PA USA;.
James E. Carpenter, University of Michigan, Ann Arbor, MI USA;.
Brian J. Cole, Rush University Medical Center, Chicago, IL USA;.
Jonathan M. Cooper, HealthPartners Specialty Center, St. Paul, MN USA;.
Charles L. Cox, Vanderbilt University, Nashville, TN USA;.
R. Alexander Creighton, University of North Carolina Medical Center, Chapel Hill, NC USA;.
Diane L. Dahm, Mayo Clinic, Rochester, MN USA;.
Tal S. David, Synergy Specialists Medical Group, San Diego, CA USA;.
David C. Flanigan, The Ohio State University, Columbus, OH USA;.
Robert W. Frederick, The Rothman Institute/Thomas Jefferson University, Philadelphia, PA USA;.
Theodore J. Ganley, Children’s Hospital of Philadelphia, Philadelphia, PA USA;.
Elizabeth A. Garofoli, Washington University in St. Louis, St. Louis, MO USA;
Charles J. Gatt, Jr, University Orthopaedic Associates LLC, Princeton, NJ USA;.
Steven R. Gecha, Princeton Orthopaedic Associates, Princeton, NJ USA;.
James Robert Giffin, Fowler Kennedy Sport Medicine Clinic, University of Western Ontario, London Ontario, Canada;.
Sharon L. Hame, David Geffen School of Medicine at UCLA, Los Angeles, CA USA;.
Jo A. Hannafin, Hospital for Special Surgery, New York, NY USA;.
Christopher D. Harner, University of Texas Health Center, Houston, TX USA;.
Norman Lindsay Harris, Jr, Grand River Health in Rifle, CO USA;.
Keith S. Hechtman, UHZ Sports Medicine Institute, Coral Gables, FL USA;.
Elliott B. Hershman, Lenox Hill Hospital, New York, NY USA;.
Rudolf G. Hoellrich, Slocum Research and Education Foundation, Eugene, OR USA;.
Timothy M. Hosea, University Orthopaedic Associates LLC, Princeton, NJ USA;.
David C. Johnson, National Sports Medicine Institute, Leesburg, VA USA;.
Timothy S. Johnson, National Sports Medicine Institute, Leesburg, VA USA;.
Morgan H. Jones, Cleveland Clinic, Cleveland, OH USA;.
Christopher C. Kaeding, The Ohio State University, Columbus, OH USA;.
Ganesh V. Kamath, University of North Carolina Medical Center, Chapel Hill, NC USA;.
Thomas E. Klootwyk, Methodist Sports Medicine, Indianapolis, IN USA;.
Bruce A. Levy, Mayo Clinic Rochester, MN USA;.
C. Benjamin Ma, University of California, San Francisco, CA USA;.
G. Peter Maiers, II, Methodist Sports Medicine Center, Indianapolis, IN USA;.
Robert G. Marx, Hospital for Special Surgery, New York, NY USA;.
Matthew J. Matava, Washington University in St. Louis, St. Louis, MO USA;.
Gregory M. Mathien, Knoxville Orthopaedic Clinic, Knoxville, TN USA;.
David R. McAllister, David Geffen School of Medicine at UCLA, Los Angeles, CA USA;.
Eric C. McCarty, University of Colorado Denver School of Medicine, Denver, CO USA;.
Robert G. McCormack, University of British Columbia/Fraser Health Authority, British Columbia, Canada;.
Bruce S. Miller, University of Michigan, Ann Arbor, MI USA;.
Carl W. Nissen, Connecticut Children’s Medical Center, Hartford, CT USA;.
Daniel F. O’Neill, Littleton Regional Healthcare, Littleton, NH USA;.
Brett D. Owens, Warren Alpert Medical School, Brown University, Providence, RI USA;.
Richard D. Parker, Cleveland Clinic, Cleveland, OH USA;.
Mark L. Purnell, Aspen Orthopedic Associates, Aspen, CO USA;.
Arun J. Ramappa, Beth Israel Deaconess Medical Center, Boston, MA USA;.
Michael A. Rauh, State University of New York at Buffalo, Buffalo, NY USA;.
Arthur C. Rettig, Methodist Sports Medicine, Indianapolis, IN USA;.
Jon K. Sekiya, University of Michigan, Ann Arbor, MI USA;.
Kevin G. Shea, Intermountain Orthopaedics, Boise, ID USA;.
Orrin H. Sherman, NYU Hospital for Joint Diseases, New York, NY USA;.
James R. Slauterbeck, Robert Larner College of Medicine, University of Vermont, Burlington, VT USA;.
Matthew V. Smith, Washington University in St. Louis, St. Louis, MO USA;.
Jeffrey T. Spang, University of North Carolina Medical Center, Chapel Hill, NC USA;.
LTC Steven J. Svoboda, Keller Army Community Hospital, United States Military Academy, West Point, NY USA;.
Timothy N. Taft, University of North Carolina Medical Center, Chapel Hill, NC USA;.
Joachim J. Tenuta, Albany Medical Center, Albany, NY USA;.
Edwin M. Tingstad, Inland Orthopaedic Surgery and Sports Medicine Clinic, Pullman, WA USA;.
Armando F. Vidal, University of Colorado Denver School of Medicine, Denver, CO USA;.
Darius G. Viskontas, Royal Columbian Hospital, New Westminster, BC Canada;.
Richard A. White, Fitzgibbon’s Hospital, Marshall, MO USA;.
James S. Williams, Jr, Cleveland Clinic, Euclid, OH USA;.
Michelle L. Wolcott, University of Colorado Denver School of Medicine, Denver, CO USA;.
Brian R. Wolf, University of Iowa Hospitals and Clinics, Iowa City, IA USA;.
James J. York, Orthopaedic and Sports Medicine Center, LLC, Pasedena, MD.
The MARS Group:
BIBLIOGRAPHY
- 1.Borchers JR, Kaeding CC, Pedroza AD, et al. Intra-Articular Findings in Primary and Revision Anterior Cruciate Ligament Reconstruction Surgery: A Comparison of the Moon and Mars Study Groups. Am J Sports Med. 2011;39(9):1889–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brophy RH, Haas AK, Huston LJ, Nwosu SK, Group M, Wright RW. Association of Meniscal Status, Lower Extremity Alignment, and Body Mass Index with Chondrosis at Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2015;43(7):1616–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brophy RH, Wright RW, David TS, et al. Association between Previous Meniscal Surgery and the Incidence of Chondral Lesions at Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2012;40(4):808–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen JL, Allen CR, Stephens TE, et al. Differences in Mechanisms of Failure, Intraoperative Findings, and Surgical Characteristics between Single- and Multiple-Revision Acl Reconstructions: A Mars Cohort Study. Am J Sports Med. 2013;41(7):1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunn WR, Spindler KP. Predictors of Activity Level 2 Years after Anterior Cruciate Ligament Reconstruction (Aclr): A Multicenter Orthopaedic Outcomes Network (Moon) Aclr Cohort Study. Am J Sports Med. 2010;38(10):2040–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Englund M, Roos EM, Lohmander LS. Impact of Type of Meniscal Tear on Radiographic and Symptomatic Knee Osteoarthritis: A Sixteen-Year Followup of Meniscectomy with Matched Controls. Arthritis Rheum. 2003;48(8):2178–2187. [DOI] [PubMed] [Google Scholar]
- 7.George MS, Dunn WR, Spindler KP. Current Concepts Review: Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2006;34(12):2026–2037. [DOI] [PubMed] [Google Scholar]
- 8.MARS Group. Factors Influencing Graft Choice in Revision Anterior Cruciate Ligament Reconstruction in the Mars Group. Journal of Knee Surgery. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamath GV, Redfern JC, Greis PE, Burks RT. Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2011;39(1):199–217. [DOI] [PubMed] [Google Scholar]
- 10.Magnussen RA, Granan LP, Dunn WR, et al. Cross-Cultural Comparison of Patients Undergoing Acl Reconstruction in the United States and Norway. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Magnussen RA, Trojani C, Granan LP, et al. Patient Demographics and Surgical Characteristics in Acl Revision: A Comparison of French, Norwegian, and North American Cohorts. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2339–2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MARS Group. Effect of Graft Choice on the Outcome of Revision Anterior Cruciate Ligament Reconstruction in the Multicenter Acl Revision Study (Mars) Cohort. Am J Sports Med. 2014;42(10):2301–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MARS Group. Meniscal and Articular Cartilage Predictors of Clinical Outcome Following Revision Anterior Cruciate Ligament Reconstruction. American Journal of Sports Medicine. 2016;44(7):1671–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MARS Group. Radiographic Findings in Revision Anterior Cruciate Ligament Reconstructions from the Mars Cohort. J Knee Surg. 2013;26(4):239–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MARS Group, Allen CR, Anderson AF, et al. Surgical Predictors of Clinical Outcomes after Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2017;45(11):2586–2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MARS Group, Wright RW, Huston LJ, et al. Descriptive Epidemiology of the Multicenter Acl Revision Study (MARS) Cohort. Am J Sports Med. 2010;38(10):1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith MV, Calfee RP, Baumgarten KM, Brophy RH, Wright RW. Upper Extremity-Specific Measures of Disability and Outcomes in Orthopaedic Surgery. J Bone Joint Surg Am. 2012;94(3):277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith MV, Klein SE, Clohisy JC, Baca GR, Brophy RH, Wright RW. Lower Extremity-Specific Measures of Disability and Outcomes in Orthopaedic Surgery. J Bone Joint Surg Am. 2012;94(5):468–477. [DOI] [PubMed] [Google Scholar]
- 19.Spindler KP, Huston LJ, Wright RW, et al. The Prognosis and Predictors of Sports Function and Activity at Minimum 6 Years after Anterior Cruciate Ligament Reconstruction: A Population Cohort Study. Am J Sports Med. 2011;39(2):348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr. Anterior Cruciate Ligament Reconstruction Autograft Choice: Bone-Tendon-Bone Versus Hamstring: Does It Really Matter? A Systematic Review. Am J Sports Med. 2004;32(8):1986–1995. [DOI] [PubMed] [Google Scholar]
- 21.Spindler KP, Warren TA, Callison JC Jr., Secic M, Fleisch SB, Wright RW. Clinical Outcome at a Minimum of Five Years after Reconstruction of the Anterior Cruciate Ligament. J Bone Joint Surg Am. 2005;87(8):1673–1679. [DOI] [PubMed] [Google Scholar]
- 22.Wasserstein D, Huston LJ, Nwosu S, et al. Koos Pain as a Marker for Significant Knee Pain Two and Six Years after Primary Acl Reconstruction: A Multicenter Orthopaedic Outcomes Network (Moon) Prospective Longitudinal Cohort Study. Osteoarthritis Cartilage. 2015;23(10):1674–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wright RW. Knee Injury Outcomes Measures. J Am Acad Orthop Surg. 2009;17(1):31–39. [DOI] [PubMed] [Google Scholar]
- 24.Wright RW. Knee Sports Injury Outcome Measures. J Knee Surg. 2005;18(1):69–72. [DOI] [PubMed] [Google Scholar]
- 25.Wright RW, Baumgarten KM. Shoulder Outcomes Measures. J Am Acad Orthop Surg. 2010;18(7):436–444. [DOI] [PubMed] [Google Scholar]
- 26.Wright RW, Dunn WR, Amendola A, et al. Anterior Cruciate Ligament Revision Reconstruction: Two-Year Results from the Moon Cohort. J Knee Surg. 2007;20(4):308–311. [DOI] [PubMed] [Google Scholar]
- 27.Wright RW DW, Amendola A, Andrish JT, Bergfeld JA, Flanigan DC, Jones M, Kaeding CC, Marx RG, Matava MJ, McCarty EC, Parker RD, Vidal A, Wolcott M, Wolf BRSK. Anterior Cruciate Ligament Revision Reconstruction: Two Year Results from the Moon Cohort. J Knee Surgery. 2007;20(4):308–311. [DOI] [PubMed] [Google Scholar]
- 28.Wright RW, Gill CS, Chen L, et al. Outcome of Revision Anterior Cruciate Ligament Reconstruction: A Systematic Review. J Bone Joint Surg Am. 2012;94(6):531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zarins B Are Validated Questionnaires Valid? J Bone Joint Surg Am. 2005;87(8):1671–1672. [DOI] [PubMed] [Google Scholar]


