Abstract
Aims and objectives
The aim of the 2019 EAHP Medicines Shortages Survey was to collect information on reasons and management strategies for medicines shortages as well as details on their impact on patients. The survey targeted hospital pharmacists (HPs), physicians (PHYs), nurses (NRS) and other healthcare professionals (OHCPs). A separate set of questions addressed patients (PTNs).
Methods
A 28-question survey was conducted by EAHP, collecting information from European HPs, PTNs, NRS, PHYs and OHCPs on the shortage situation in their respective countries. The survey ran from 7 November 2019 to 13 January 2020. The results were analysed by EAHP.
Results
There were 2136 HP responses to the 2019 survey compared with 1666 in 2018. While 95% of HPs and 89% of OHCPs consider medicine shortages a current problem, only 71% of PHYs and 62% of NRS state the same. Shortages of active pharmaceutical ingredients (72%), manufacturing (72%) and supply chain problems (49%) are leading causes of shortages according to HPs, while PHYs (40%) and NRS (37%) consider the pricing to be their driver. Antimicrobials and oncology medicines were most affected by shortages in 2019. Compared to 2018, the percentage of respondents who reported shortages of oncology medicines increased from 39% to 47% in 2019. HPs (42%), PHYs (36%) and OHCPs (38%) consider delays in care as the main consequence of medication shortages. The satisfaction with reporting systems for medicine shortages decreased from 56% in 2018 to 48% in 2019 for HPs, while they remain low for PHYs (36%).
Conclusions
Medicines shortages affect patient care and healthcare professionals’ everyday tasks. Better enforcing of the mandatory early notification of shortages and structured mitigation response is recognised by all respondents as best strategy to tackle shortages.
Keywords: drug procurement; drug manufacturing / preparation / compounding; health policy; pharmacy management (organisation, financial); health & safety
Introduction
Medicine shortages are on the rise globally, occurring every day across healthcare settings and affecting all stakeholders involved in delivering and managing patients' treatment.1–3 Their impact on patient care has been repeatedly confirmed, yet a comprehensive and holistic solution to avoid and successfully mitigate shortages is not on the horizon.4–6 Recent reports from healthcare professional associations and health authorities confirm aggravation of shortages, seriously impacting patients' health.7–9
The European Association of Hospital Pharmacists’ (EAHP) 2014, 2018 and 2019 medicines shortage surveys were conducted to provide an overview of the European medicine shortages landscape and its effect on patient care along with potential solutions to ameliorate shortages.5 10 In 2014, there were 86% hospital pharmacists (HPs) who responded 'yes', confirming shortages to be a problem, compared with 90% in 2018 and 95% in 2019. Moreover, 89% other healthcare professionals (OHCPs) confirmed the same.
Ongoing gathering of information on shortages is of vital importance when assessing alternatives, making changes in healthcare-related IT systems and communicating with patients, clinicians and hospital management.11 Shortage management of a healthcare facility depends on the infrastructure established, aimed at preventing shortages before their occurrence so as to contain adverse effects on patient care and accompanying healthcare-related costs.11 12
The 2019 EAHP Survey on Medicines Shortages explored issues linked to communication of medicines shortages within hospitals and the reasons for shortages as well as their impact on patients. In addition, current management strategies were collected by asking how survey participants would like to see medicines shortages handled and/or resolved.
Methods
EAHP created and conducted the 2019 Survey on Medicines Shortages using Survey Monkey (https://www.surveymonkey.com/r/EAHP2019MedicinesShortagesSurvey). The online questionnaire, along with its objectives and timeline, was distributed via a continuous advertising campaign on social media (Facebook, Instagram, LinkedIn and Twitter) and via the EU Monitor to engage individual HPs, PTNs, physicians (PHYs), nurses (NRS) and OHCPs across Europe to collect information on shortages in their respective country (https://www.eahp.eu/sites/default/files/eahp_2019_medicines_shortages_report.pdf). The 28-question survey ran from 7 November 2019 to 13 January 2020. Questions on tendering were not posed to NRS and PHYs. A separate set of questions was addressed to PTNs. The results were analysed by EAHP. Due to the difference in questions, only a limited comparison with the results of the 2014 and 2018 survey was possible.
Results
2136 responses from HPs were submitted to the 28 questions posed by the 2019 Medicines Shortages Survey (compared with 1666 responses of 2018 and 607 of 2014). The table below breaks down the responses of the three survey years by country. The response rate increased by 28% from 2018 (n=1666) to 2019, with increases in France, Germany, the Czech Republic and Slovakia (table 1). For the first time, data from PHYs (209), NRS (149), PTNs (385) and OHCPs (289) were collected.
Table 1.
Response rate of hospital pharmacists (n=2136) to EAHP’s Medicines Shortages Surveys conducted in 2014, 2018 and 2019 grouped by country
| Country | Responses (2019) | Responses (2018) | Responses (2014) | Country | Responses (2019) | Responses (2018) | Responses (2014) |
| Albania | 2 | 1 | 0 | Lithuania | 2 | 1 | 8 |
| Andorra | 3 | 0 | 0 | Luxembourg | 7 | 3 | 0 |
| Austria | 44 | 29 | 21 | Malta | 3 | 6 | 11 |
| Belgium | 135 | 90 | 94 | Montenegro | 6 | 4 | 0 |
| Bosnia & Herzegovina | 26 | 19 | 9 | The Netherlands | 29 | 20 | 11 |
| Bulgaria | 9 | 3 | 6 | North Macedonia | 34 | 14 | 4 |
| Croatia | 23 | 26 | 25 | Norway | 21 | 21 | 11 |
| Cyprus | 2 | 2 | 1 | Poland | 12 | 32 | 13 |
| Czech Republic | 114 | 26 | 4 | Portugal | 129 | 85 | 42 |
| Denmark | 2 | 10 | 25 | Romania | 69 | 24 | 2 |
| Estonia | 12 | 17 | 15 | Russia | 1 | 1 | 0 |
| Finland | 12 | 33 | 1 | Serbia | 77 | 20 | 8 |
| France | 358 | 192 | 3 | Slovakia | 100 | 23 | 16 |
| Germany | 207 | 78 | 10 | Slovenia | 22 | 18 | 5 |
| Greece | 110 | 84 | 14 | Spain | 198 | 190 | 105 |
| Hungary | 37 | 33 | 12 | Sweden | 77 | 5 | 0 |
| Iceland | 2 | 9 | 4 | Switzerland | 83 | 67 | 7 |
| Ireland | 43 | 51 | 47 | Turkey | 8 | 61 | 5 |
| Italy | 34 | 73 | 41 | United Kingdom | 83 | 291 | 7 |
| Latvia | 0 | 4 | 2 |
Medicine shortages and their extent
Compared with 90% (n=1493) in 2018, 95% (n=2036) of HPs answered 'yes' when asked if shortages of medicines are a current problem in delivering the best care to PTNs. While the majority of OHCPs (89%/n=258) agreed that medicine shortages are a problem, only 62% (n=92) of NRS and 71% (n=150) of PHYs shared this view.
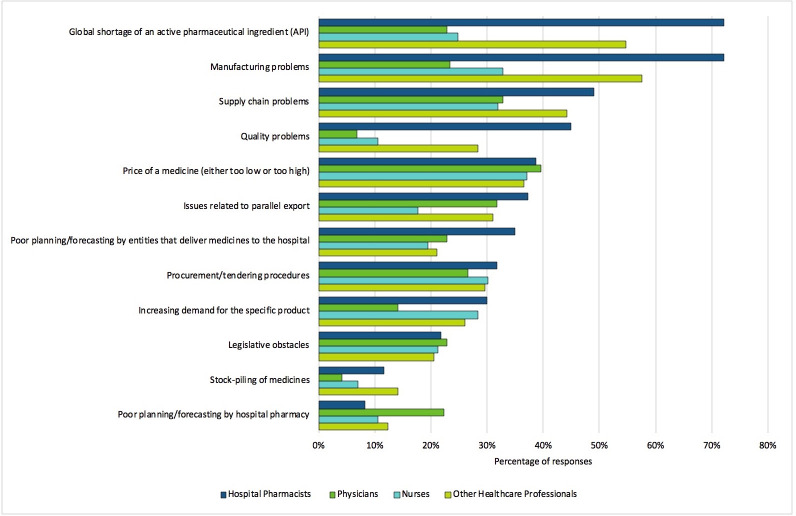
Answers were diverse among the survey groups when asked what they believed to be the possible reasons for medicine shortages. For HPs, global shortage of an active pharmaceutical ingredient (API) (72%), manufacturing problems (72%) and supply chain problems (49%) ranked the highest among the shortage causes, while leading issues for PHYs included pricing of a medicine (40%), supply chain problems (33%) and issues related to parallel export (32%). NRS selected the price of a medicine (37%), manufacturing problems (33%) and supply chain problems (32%) (figure 1).
Figure 1.
Reasons for shortages by participant. Percentage of responses by hospital pharmacists (n=2075) for question 4, physicians (n=192) for question 33, nurses (n=113) for question 54 and other healthcare professionals (n=219) for question 84 ‘What do you see as possible reasons of shortages in your hospital?’, grouped by profession. (Note that this was a tick all that apply question).
The vast majority of HPs (85%/n=1806) and OHCPs (77%/n=155), that chose to answer this question, reported experiencing a medicine shortage in 2019 when the medicine was only supplied by a single pharmaceutical company. 81% of HPs and 67% of OHCPs reported suffering such a shortage more than three times in 2019.
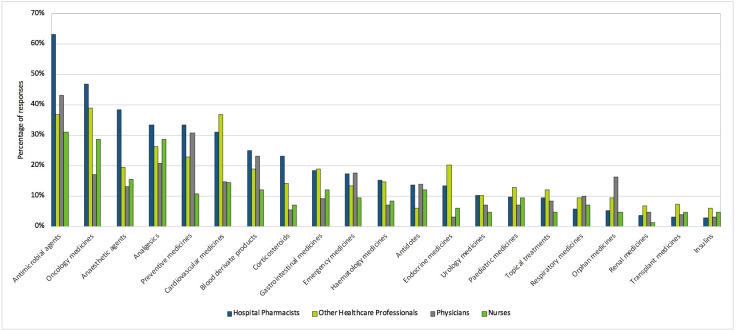
More than half of HPs (n=1158) responded that selected antimicrobial agents are most commonly in short supply, with oncology medicines second, followed by anaesthetic agents (38%) (figure 2). The findings for PHYs, NRSs and OHCPs differed from those for HPs. While PHYs (43%) and nurses (31%) identified antimicrobial agents those most commonly in short supply, OHCPs reported more shortages for oncology medicines (39%), with antimicrobial agents and cardiovascular medicines (both 37%) ranking second. For 31% of PHYs, preventive medicines were the second most common to experience a shortage. Nurses identified analgesics and oncology medicines (both 29%) as also frequently experiencing a shortage (figure 2).
Figure 2.
Medicine group most frequently affected by a shortage (by participant). Percentage of responses by hospital pharmacists (n=1837) for questions 22, physicians (n=53) for question 49, nurses (n=49) for question 71 and other healthcare professionals (n=60) for questions 106 ‘in which area of medicine does your hospital experience shortages most commonly?’, grouped by profession. (Note that this was a tick all question.)
Compared to the 2018 survey results, oncology medicines increased from 39% in 2018 to 47% in 2019, while anaesthetic agents remained stable at 39% in 2018 and 38% in 2019. After the increase to 77% in 2018 from 57% in 2014, the reports for antimicrobial agents decreased to 63%.
Reporting and managing medicine shortages
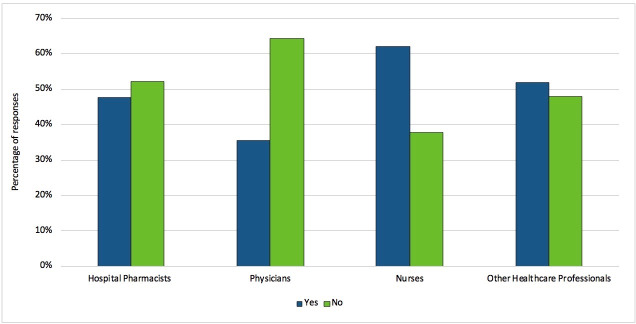
68% of HPs and 58% (n=109) of OHCPs answered ‘medicines agency’ as the body responsible for managing the public shortage reporting system (n=1254). In contrast, the answer selected mostly by PHYs and NRS was ‘I don’t know’ with 54% selecting this answer. Asked whether they found their national public reporting system on shortages to be useful and regularly updated, NRS were most likely to answer 'yes' (62%, n=36), with 52% (n=79) of all OHCPs. Only 36% (n=32) of PHYs and 48% (n=762) of HPs deemed their national public reporting system on shortages useful and regularly updated, representing a decrease compared with 56% in 2018 (figure 3).
Figure 3.
Percentage of responses by hospital pharmacists (n=1594) for question 11, PHY (n=90) for question 35, nurses (n=58) for question 56 and OHCP (n=152) for question 91 ‘Do you find that your national public reporting system on shortages is useful and regularly updated?’ (grouped by profession).
60% of HPs (n=950) indicated that manufacturers can report medicines shortages, while only 13% of PHYs (n=12) and 28% of NRS (n=16) did. PHYs (59%) and NRS (43%) were more likely to state that healthcare professionals are able to report via their public shortages reporting system: in comparison, only 24% of HPs and 26% of OHCPs said the same.
45% of HPs (n=839), 45% of PHYs (n=61), 50% of NRS (n=45) and 40% of OHCPs (n=61) answered that they did not know if feedback from national authorities was provided when reporting a shortage. All groups identified email and phone communication as the most commonly used means to communicate with their counterparts on shortages and alternatives. 29% of HPs have a protocol on managing medicines shortages vs 61% that do not. All professionals specifically noted exchanges within the Drug and Therapeutics Committee DTC) to be an infrequently used medium.
HPs (70%/n=1299) and OHCPs (59%/n=90) stated that a no medicine prescribing/dispensing IT system was automatically fed with information on ongoing shortages and potential alternatives in their hospital.
Medicine shortages impact on patient care
More than half of the HPs (63%/n=1153) indicated that shortages had an impact on patient care in their hospital (similar to PHYs (58%/n=75) and OHCPs (52%/n=78)).
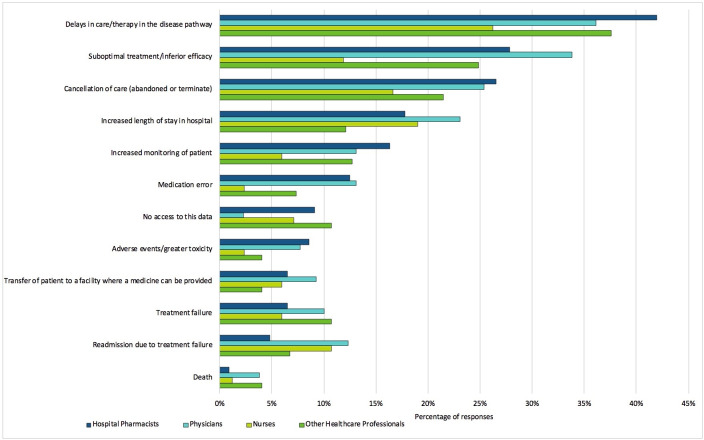
In 2018, 59% of HPs (n=555) identified delays in care or therapy, which fell to 42% (n=771) in 2019. In 2018, suboptimal treatment/inferior efficacy (25%/n=239) and cancellation of care (31%/n=297) were cited as the main consequences of medicine shortages (rising to 28%/n=512 and lowering to 27%/n=488, respectively). PHYs and OHCPs named the same consequences among their top three in the survey (figure 4). Medication errors stemming from shortages (25%/n=241) were listed as the third most common problem in 2018, ranking sixth in the 2019 Medicines Shortages Survey, where 12% (n=229) of HPs declared shortages having consequences on patient care.
Figure 4.
The impact of medicine shortages on patients (by participant). Percentage of responses by hospital pharmacists (n=1837) for question 24, physicians (n=130) for question 47, nurses (n=84) for question 69 and other healthcare professionals (n=149) for question 104 ‘Please choose the type of impact medicines shortages had on patient care in your hospital’, grouped by profession. (Note that this was a tick all question.)
38% (n=56) of OHCPs selected delays in care or therapy, 25% (n=37) suboptimal treatment and 21% (n=32) cancellation of care (figure 4). For NRS, increased length of hospital stay was the second most common cause identified (19%/n=16), ranking fourth for HPs (18%/n=326) and PHYs (23%/n=30) and fifth for OHCPs (12%/n=18) (figure 4). 27% (n=22) of NRS, when asked whether medicines shortages had affected the administration of medicines in their hospital, reported that shortages had led to non-administration/delays of administration due to non-recognition of the replacement medicine, while 42% (n=35) noted no effect and 31% (n=26) answered that they did not know.
For treatment affected by medicine shortages, half of HPs in 2019 (n=910) needed to prioritise medicine provision to PTNs based on their disease/clinical status. For 46%, this prioritisation affected a larger group of PTNs. NRS were able to do so in 58% of cases, while both PHYs and OHCPs could in only 41%. Shortages affected a larger group of patients as stated by 41% of PHYs, 42% of OHCPs and 49% of NRS.
Only 10% (n=177) of HPs and 13% (n=19) of OHCPs carried out risk assessments under a shortage, while 21% (n=382) and 46% (n=67), respectively, reported not knowing whether they had applied it.
EAHP also collected feedback from patients for the first time on their experiences with shortages. 47% of PTNs (n=169) reported experiencing shortages themselves or by a family member, where 46% (74) of them had been informed as to the reason. Only 29% (n=46), having experienced a shortage, felt that their problem was correctly handled.
65% (n=68) of PTNs reported shortages affecting their care in hospitals. Responding to impact, 30% (n=48) of respondents reported their care to be delayed as a consequence of a shortage, 12% (n=20) experienced a failure in treatment and 11% (n=18) an increased stay in hospital. 10% (n=16) of PTNs had their treatment cancelled, while 8% (n=13) experienced adverse events or greater toxicity. Patient readmission due to treatment failure and increased monitoring presented in 6% (n=8) and 3% (n=5) were transferred to where the medicine could be provided. 2% of PTNs (n=4) answered that they knew of a death occurring due to a shortage. 11% (n=17) stated to not know of the impact the shortage had on their treatment.
Solutions and suggestions to more effectively manage shortages
65% of HPs (n=1205), 62% of PHYs (n=84), 65% of NRs (n=56) and 56% of OHCPs (n=86) opted to ‘better enforce the mandatory early notification of a medicine shortages’ deeming it as the best received proposal/strategy to mitigate them. The least preferred was ‘ensure appropriate staffing levels in order to lower the impact that medicines shortages currently have on the overall patient services’, with only 37% of HPs (n=674), 32% of PHYs (n=43), 37% of NRs (n=32) and 28% of OHCPs (n=41) ranking it as 5 (=very useful).
HPs made 235 proposals applicable to alleviating the problem of shortages, ranging from improvements within the supply chain towards adjustments inside the hospital proper. Some of the most common themes to this question included: improving communication (46 responses), applying prudent tendering/procurement mechanisms that ensure that there is more than one supplier per medicine/API in Europe (36 responses), mandating manufacturers to stop ‘just in time production’ and to increase stocks at national level, especially for those essential and/or regularly out of stock (29 responses), imposing/enforcing penalties for the non-communication of a medicine shortage (24 responses) and moving the production of APIs/medicines back to Europe (22 responses).
Discussion
The EAHP Medicine Shortage Survey indicated an increase of HPs sharing their input and concerns when facing medicine shortages along with their colleagues and PTNs which coincides with rising medicine shortages across Europe as reported by healthcare and patient organisations, as well as healthcare authorities.5 9 13 While 95% of HPs considered shortages to be a problem in 2019, it is lower among PHYs (71%) and NRS (62%). The fact that the HPs spend a significant amount of time daily to mitigate medicine shortages and adapt treatment protocols shows that HPs ensure only a limited amount of shortages reach PHYs, NRS and OHCPs.14
The four groups surveyed differ in their perception of the cause of shortages. Although they share similar opinions on origins (price, procurement/tendering procedures and legislative obstacles), HPs are noticeably more concerned with issues related to a medicine's manufacturing process and supply chain. The differing concerns might stem from everyday tasks and responsibilities that the healthcare professionals surveyed carry out, which shapes their views on shortages.2
According to HPs, PHYs and NRS, shortages largely affect antimicrobials, while OHCPs have the opinion that oncology medicines are most affected. Interestingly, though, the overall percentage that reported experiencing a shortage of antimicrobials in 2019, 63% is considerably lower compared with 2018, (77%). This drop then does not seem to reflect the rising shortages of antimicrobials jeopardising efforts made by antimicrobial stewardship teams and affecting bacterial resistance.11 15–17
When faced with a shortage, the survey finds that the authority to which it is reported is determined by the respective country of the healthcare professional. As reported, a majority of reports come from HPs, with 64% reporting to a medicine agency. 54% of PHYs and NRS do not know where to report a shortage. Regardless, as opposed to 2018 when 56% HPs found their reporting system to be useful, only 48% of HPs and 36% of PHYs did so in 2019. Such a lack of a functional reporting system may negatively affect mitigating shortages.4 Similarly, the healthcare professionals surveyed were not aware who is to report a shortage, with 60% of HPs stating that they did not know if manufacturers can report one, compared with 13% of PHYs and 28% of NRS.
This variance in the responses by group most likely stems from a significant portion of PHYs and NRS simply being unaware of their respective national public shortages-reporting system. The large divergence between the answers of PHYs and NRS and HPs might simply indicate that PHYs and NRS would be more likely aware of such systems if they were to have the ability to report them.
Variability in reporting systems across Europe does exist in terms of reporting shortages and accessing the repositories fed by updates on shortages.4 Among the four surveyed healthcare-professional groups, 40% of PHYs stated that they do get feedback from their designated national authority, compared with 16% of NRS and 21% of HPs. These numbers do not reflect the regulatory authorities’ recommendations, which emphasise that feedback on shortage duration, cause and possible substitutes having a tremendous impact on healthcare professionals when managing shortages.11 18–20
In order to mitigate shortages successfully, multi-stakeholder task-force groups are viewed as an effective way to increase information exchange and propose shortage management strategies either by hospital or on a national level.4 However, the survey showed that only a small percentage of professionals (8% of OHCPs/5% of HPs/1% of PHYs) are aware that such groups are organised regionally. Concerning information exchange in a healthcare setting, in line with the recommendation of using multiple communication channels when mitigating shortages is the use of emails and phone calls that are primarily to share data on substitutes and ongoing shortages among the healthcare professionals surveyed.11 Nevertheless, DTCs as bodies intended to address all issues regarding a medicine’s application are representative among the responses, with only 17% of PHYs, 14% of NRS, 8% of HPs and 2% of OHCPs citing them. This is in stark contrast with the American Association of Health System Pharmacists’ recommendation, according to which multidisciplinary teams may serve as an important step in prioritising patients and deciding on available treatments and substitutes in order to mitigate shortages.11
As indicated by a majority of survey respondents, when a medicine is supplied by a single pharmaceutical company, shortages are more frequent, thereby underlining, as recommended by healthcare experts, the necessity of ensuring a diverse set of suppliers in order to address shortages.2
Medicine shortages affect health outcomes by interfering with care management in patients’ lives.5 21 22 Shortages worsen the ability to provide safe, efficient treatment, risking delays in care, readmission and even death.23 Interestingly, while PHYs and NRS consider patient readmission a major impact from shortages, HPs paid it the least attention. This stark difference in opinion might stem from the differing roles and tasks carried out respective to their profession and how they interact with shortage impacts.8
Some healthcare professionals did report knowing of risk assessment procedures and reporting tools to mitigate shortages and their effects, such as Failure Mode and Effect Analysis, Datix, Brexit or standard procedures offered by respective national agencies (ie, NHS England; HPRA). Despite growing shortages, HPs across Europe did not report conducting risk assessments on shortages in a systematic manner among the 123 free text responses provided. This finding is in line with recent research conducted within the COST Action 15 105 network.24
Having patients involved in managing medicine shortages still remains a challenge, as it is difficult for them to be fully informed about a shortage and the challenges affecting their treatment. However, facing abrupt treatment interruption or less effective treatment accompanied by more adverse events following therapy substitution, PTNs expressed the need to know more on shortages. Although healthcare professionals do have concerns about the impact shortages may have on patient health, prescribing PHYs seldom inform patients on substitutes introduced to treatment. Therefore, patients might be unaware of the effect medicine shortages have.8 When offered with an alternative, the surveyed PTNs noted the information usually presented involves data on the substitute's dosing patterns, or, if no such substitute exists, the necessity to bring their home medication to a hospital.
The literature also confirms that being updated actively on shortages is vital in successful mitigation.4 13 25 As further confirmation, this paper also finds that healthcare professionals consider mandatory shortage notifications and improving communication as the most preferential method to mitigating shortages. However, it is necessary for data on the shortages received to be clear and provided in a timely manner, before HPs invest time and effort on it. Therefore, it is not singularly a matter of how many staff are available. As a result, although HPs do report spending significant time managing shortages,5 14 26 the participants here may have not considered increasing staffing to mitigate shortages.14 The PTNs surveyed did expressly state that hospital pharmacies should ensure reserve stocks to serve in the time of shortages. Buffer stocks are, indeed, one option available to better manage frequent shortages,27 but stockpiling medicine may cause additional shortages and may create strain on limited resources.11
Conclusion
Acknowledged by all groups (HPs, PHYs, NRS, OHCPs and PTNs), the 2019 EAHP Medicine Shortages Survey demonstrates that shortages are becoming more frequent and affect an increasing number of patients. As with surveys conducted in 2014 and 2018, oncology medicines, antibiotics and anaesthetics still represent the medicines most affected by shortages, leading to delays in care, poor health outcomes, medicine errors and adverse events. Hospital pharmacists face tremendous challenges to mitigate shortages but appear to lack a coordinated approach in managing them, especially in terms of data sharing and more prominent multi-stakeholder involvement. Since healthcare professionals are found to still mainly communicate on shortages via emails and phone calls, rather than through multidisciplinary committees, it may be concluded that shortage management requires better structuring, including procedures involving risk assessment to prevent threats to sustainable and continuous patient care posed by shortages.
What does this paper add?
What is already known on this subject
Medicine shortages were reported across Europe in the 2014 and 2018 surveys.
Causes of shortages are complex and multifactorial.
Shortages have been shown to affect patient safety and health outcomes.
What does this study add
The medicines most affected by shortages in 2019 are antibiotics, oncology medicines and anaesthetics.
Healthcare professionals use different risk-assessment and standard operating procedures to mitigate shortages.
A distinct lack of multi-stakeholder engagement still remains a challenge to managing shortages more efficiently.
Patients are often not well informed about how their treatment may be affected by shortages and how it will be mitigated.
Footnotes
Contributors: AB, NM, PH, PP and SK designed and carried out the survey. NM and SK performed data analysis and interpretation needed for the manuscript. AB, NM, PH, PP and SK contributed to critical analysis and interpretation of data as well as revising the manuscript. NM compiled the first draft and the subsequent iterations of the manuscript. All authors read, commented on and contributed to the manuscript for the accuracy of the content. All authors finally approved the version to be published and agreed to be accountable for all aspects of the work in terms of its accuracy and integrity. NM is the corresponding author.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data availability statement: Data are available upon reasonable request. The data that support the findings of this study are available from the EAHP, upon reasonable request.
References
- 1. Fox ER, Sweet BV, Jensen V. Drug shortages: a complex health care crisis. Mayo Clin Proc 2014;89:361–73. 10.1016/j.mayocp.2013.11.014 [DOI] [PubMed] [Google Scholar]
- 2. The Economist Intelligence Unit Addressing medicine shortages in Europe taking a concerted approach to drive action on economic, manufacturing and regulatory factors, 2017. Available: http://graphics.eiu.com/upload/topic-pages/medicine-shortages/Addressing-medicine-shortages-in-Europe-EIU.pdf [Accessed 24 Apr 2020].
- 3. World Health Organization Medication without Harm – WHO global patient safety challenge, 2017. Available: https://www.who.int/PTNafety/medication-safety/medication-without-harm-brochure/en/ [Accessed 24 Apr 2020].
- 4. Bochenek T, Abilova V, Alkan A, et al. . Systemic measures and legislative and organizational frameworks aimed at preventing or mitigating drug shortages in 28 European and Western Asian countries. Front Pharmacol 2017;8:942. 10.3389/fphar.2017.00942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Miljković N, Gibbons N, Batista A, et al. . Results of EAHP’s 2018 Survey on Medicines Shortages. Eur J Hosp Pharm 2019;26:60–5. 10.1136/ejhpharm-2018-001835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Institute for Safe Medication Practices Drug shortages threaten patient safety, 2010. Available: www.ismp.org/resources/drug-shortagesthreaten-patient-safety [Accessed 24 Apr 2020].
- 7. The Society of Hospital Pharmacists of Australia Medicine shortages in Australia a snapshot of shortages in Australian hospitals, 2017. Available: https://www.shpa.org.au/sites/default/files/uploaded-content/website-content/shpa_medicines_shortages_in_australia_report_june_2017.pdf [Accessed 24 Apr 2020].
- 8. US Food and Drug Administration Drug shortages: root causes and potential solutions, 2019. Available: https://www.fda.gov/media/131130/download [Accessed 24 Apr 2020].
- 9. Pharmaceutical Group of the European Union PGEU survey on medicine shortages 2019, 2020. Available: https://www.pgeu.eu/wp-content/uploads/2019/03/PGEU-Medicine-Shortages-Survey-Results-2019.pdf [Accessed 24 Apr 2020].
- 10. European Association of Hospital Pharmacists EAHP's 2014 medicines shortages report, 2014. Available: https://www.eahp.eu/sites/default/files/shortages_report05online.pdf [Accessed 24 Apr 2020].
- 11. Fox ER, McLaughlin MM. ASHP guidelines on managing drug product shortages. Am J Health Syst Pharm 2018;75:1742–50. 10.2146/ajhp180441 [DOI] [PubMed] [Google Scholar]
- 12. Griffith MM, Patel JA, Sutton SH, et al. . Prospective approach to managing antimicrobial drug shortages. Infect Control Hosp Epidemiol 2012;33:745–52. 10.1086/666332 [DOI] [PubMed] [Google Scholar]
- 13. France Assos Santé Pénuries de médicaments et de vaccins, 2018. Available: https://www.france-assos-sante.org/communique_presse/penurie-de-vaccins-et-medicaments-inquietudes-de-france-assos/ [Accessed 24 Apr 2020].
- 14. De Weerdt E, De Rijdt T, Simoens S, et al. . Time spent by Belgian hospital pharmacists on supply disruptions and drug shortages: an exploratory study. PLoS One 2017;12:e0174556. 10.1371/journal.pone.0174556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Griffith MM, Pentoney Z, Scheetz MH. Antimicrobial drug shortages: a crisis amidst the epidemic and the need for antimicrobial stewardship efforts to lessen the effects. Pharmacotherapy 2012;32:665–7. 10.1002/j.1875-9114.2012.01158.x [DOI] [PubMed] [Google Scholar]
- 16. Gross AE, Johannes RS, Gupta V, et al. . The effect of a piperacillin/tazobactam shortage on antimicrobial prescribing and clostridium difficile risk in 88 US medical centers. Clin Infect Dis 2017;65:613–8. 10.1093/cid/cix379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gundlapalli AV, Beekmann SE, Graham DR, et al. . Antimicrobial agent shortages: the new norm for infectious diseases physicians. Open Forum Infect Dis 2018;5:ofy068–ofy. 10.1093/ofid/ofy068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. European Medicines Agency Good practice guidance for communication to the public on medicines’ availability issues. Recommendations for EU national competent authorities and EMA to ensure adequate public information, 2019. Available: https://www.ema.europa.eu/en/documents/regulatory-procedural-guideline/good-practice-guidance-communication-public-medicines-availability-issues_en.pdf [Accessed 24 Apr 2020].
- 19. Australian Government Department of Health, Therapeutic Goods Administration . Management and communication of medicine shortages and discontinuations in Australia – Steps: report, manage and communicate, 2020. Available: https://www.tga.gov.au/book-page/steps-report-manage-and-communicate [Accessed 24 Apr 2020].
- 20. Australian Government Department of Health, Therapeutic Goods Administration . Medicine shortages information initiative, critical medicine shortages and other information, 2020. Available: https://apps.tga.gov.au/prod/MSI/search [Accessed 24 Apr 2020].
- 21. Institute for Safe Medication Practices Drug shortages: national survey reveals high level of frustration, low level of safety. 15 Horsham: ISMP Medication Safety Alert, 2010: 1–4. https://www.ismp.org/resources/special-issue-drug-shortages-national-survey-reveals-high-level-frustration-low-level [Google Scholar]
- 22. Institute for Safe Medication Practices ISMP survey on drug shortages for hospital pharmacy directors or their designees only. 22 Horsham: ISMP Medication Safety Alert, 2017: 5–6. https://www.ismp.org/resources/drug-shortages-continue-compromise-patient-care [Google Scholar]
- 23. Phuong JM, Penm J, Chaar B, et al. . The impacts of medication shortages on patient outcomes: a scoping review. PLoS One 2019;14:e0215837. 10.1371/journal.pone.0215837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Miljković N, Godman B, Kovačević M, et al. . Prospective risk assessment of medicine shortages in Europe and Israel: findings and implications. Front Pharmacol 2020;11:357. 10.3389/fphar.2020.00357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Acosta A, Vanegas EP, Rovira J, et al. . Medicine shortages: gaps between countries and global perspectives. Front Pharmacol 2019;10:763. 10.3389/fphar.2019.00763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kaakeh R, Sweet BV, Reilly C, et al. . Impact of drug shortages on U.S. health systems. Am J Health Syst Pharm 2011;68:1811–9. 10.2146/ajhp110210 [DOI] [PubMed] [Google Scholar]
- 27. Caulder CR, Mehta B, Bookstaver PB, et al. . Impact of drug shortages on health system pharmacies in the southeastern United States. Hosp Pharm 2015;50:279–86. 10.1310/hpj5004-279 [DOI] [PMC free article] [PubMed] [Google Scholar]