Abstract
Identifying ways to increase public spending on health is critical for the achievement of universal health coverage. While policymakers and donors often look at available options for increasing public spending for health in the medium-term, examining trends and drivers of past growth can help countries elucidate important lessons and to anticipate changes in the future. This note analyzes trends in inflation-adjusted per capita public spending for health vis-à-vis economic growth within and across a sample of 150 countries over the 2000–2017 period. Since 2000, per capita public spending for health across low- and middle-income countries has more than doubled. Less than one-fifth of this increase, however, resulted from a higher priority for health in government budgets. The remainder was largely due to conducive macroeconomic conditions such as economic growth and increases in total public spending. Furthermore, across most countries, a single time trend does not adequately capture the evolution either of economic growth or of per capita public spending on health. Instability in growth rates is large for both indicators, revealing distinct episodic patterns.
Keywords: National government health expenditure, Public expenditure, Health care financing, Economic growth
Highlights
-
•
Public spending on health growth largely due to conducive macroeconomic conditions.
-
•
Reprioritization for increasing public spending for health has been marginal.
-
•
Counter-cyclical policies essential for public financing during economic downturns.
-
•
Single time trend not adequate to capture evolution of public spending on health.
1. Introduction
Public financing is essential for making progress towards universal health coverage (UHC), a United Nations Sustainable Development Goal (SDG) policy commitment which emphasizes that everyone should have access to quality health services they need and that the use of these services does not expose individuals to undue financial hardship (World Bank, 2017). The focus on both effective service coverage as well as financial risk protection under UHC implies that how countries finance their health systems matters (Kutzin, 2012). Financing for health in most low- and middle-income countries (LMICs) is dominated by high levels of out-of-pocket (OOP) spending, an inefficient and inequitable modality which contributes to foregone care among vulnerable populations and puts them at risk of impoverishment from illness-related catastrophic expenditures. Low levels of government revenue generation and low priority for health in government budgets are two key factors contributing to low levels of public spending for health, which, in turn, is one of the primary reasons behind high levels of OOP spending in LMICs (World Bank, 2019). Identifying ways to increase public spending on health is thus critical for the achievement of UHC. While policymakers and donors often look at available options for increasing public spending for health in the medium-term, examining trends and drivers of past growth can elucidate important lessons and help countries anticipate changes in the future.
We analyze trends in inflation-adjusted per capita public spending for health vis-à-vis economic growth within and across a sample of 150 countries over the 2000–2017 period using publicly available data from the World Health Organization's (WHO's) Global Health Expenditure Database (GHED). Since 2000, per capita public spending for health across LMICs has more than doubled. Globally, when high-income countries are included, levels of per capita public spending for health have increased by more than 60 percent (from US$431 in 2000 to US$708 in 2017) with an annual growth rate of 4.0 percent. This was higher than global economic growth of 2.5 percent, implying an income elasticity of per capita public spending on health of 1.6 (per capita GDP is used as proxy for income). This indicates that per capita public spending on health on average grew 60% faster than per capita GDP between 2000 and 2017.
To understand the growth dynamics of public spending for health and explain why the income elasticity of per capita public spending for health has been greater than 1, we decompose contributions from three macro-fiscal drivers -- economic growth, changes in total public spending, and reprioritization for health -- exploiting a macroeconomic accounting identity that captures the relationship between these factors. On average, global comparative data show that both total public spending as well as priority for health increased with economic growth. Across most countries, however, a single time trend does not adequately capture the evolution either of economic growth or of per capita public spending on health. Instability in growth rates is large for both indicators, revealing distinct episodic patterns.
2. Study data and methods
Per capita public spending on health was calculated by summing three major subaccounts of health expenditure from their revenue sources: transfers from government domestic revenue (labelled ‘FS.1’ under the new System of Health Accounts methodology; see OECD, Eurostat, and WHO, 2011), transfers distributed by government from foreign origins (‘FS.2’), and social health insurance (SHI) contributions (‘FS.3’). Countries were categorized as low-income (LIC), lower middle income (LMI), upper middle income (UMI), and high income (HIC) based on their World Bank (WB) income classification in 2017. HICs were further classified into those that were members of the Organization of Economic Cooperation and Development (OECD) and non-OECD countries. Data for LMICs were also disaggregated into six WB regions: Latin America and Caribbean (LAC), East Asia and Pacific (EAP), Middle East and North Africa (MNA), Europe and Central Asia (ECA), Sub-Saharan Africa (SSA), and South Asia (SAR). Finally, countries with population below 600,000 were excluded from the analysis to minimize outliers in the data. Public spending for health was converted to real per capita terms using population and inflation numbers derived from variables published in GHED. The total public spending share of GDP was also taken from GHED.
The relative contributions to changes in public spending for health over time from a sub-set of factors were analyzed exploiting a key macroeconomic identity that, in any given year t, the following must hold true (Tandon et al., 2018):
where P is per capita public spending on health in constant local currency unit (LCUs), H is health's share of total public spending, E is the total public spending share of GDP, and Y is per capita GDP in LCUs. Taking the logarithmic difference in t+1 versus t (denoted by lowercase with ‘hat’) of P must mathematically equal the sum of the logarithmic growth rates in health's share of total public spending, of the total public spending share of GDP, and of per capita GDP:
Although mathematically this identity must hold exactly, empirically it will hold only approximately given data-related measurement errors. This implies that growth in per capita public spending on health () over a given time period must be accounted for by changes in per capita GDP (), changes in the total public spending share of GDP (), and by changes in health's share of total public spending (). Furthermore, dividing each component of the equation by yields the elasticity of each component with respect to the relative percentage change in national income:
This equation shows that the income elasticity of public spending on health () is 1 plus the sum of the income elasticities of both health's share () and of total public spending (). Hence, if income elasticity of public spending for health is estimated to be greater than 1, this can be due to an increase in prioritization for health and from an increase in the size of public spending in GDP either or both of which could themselves be a result of economic growth.
Following Pritchett (2000), shifts in per capita economic growth trends were estimated by finding the ‘breakpoint’ year (t*) that minimized the sum of squared errors over all t:
where I(.) is an indicator function (1 if the argument holds; 0 otherwise), t = [t 0, …,T] where t 0 is 2000, T is 2017, t* is the breakpoint year chosen subject to the constraint that each segment of the trend covers a minimum of three years (that is, t*-t 0 ≥ 3 and T-t* ≥ 3) and a and b are the intercept and time-trend slope, respectively, where the suffix 1 or 2 represents the estimates before and after the estimated breakpoint. The same method was also applied to capture changes in growth rates of P t across countries. Based on this, trend patterns were classified into 10 distinct types depending on the pace of growth before and after break points (Table 1 ).
Table 1.
Landscaping patterns of growth.
| Pattern | Growth rate |
Sample per capita growth | |
|---|---|---|---|
| Before break | After break | ||
| Steep Hill | ≥5 percent | ≥5 percent |  |
| Hill | ≥3 percent | ≥3 percent |  |
| Accelerator | 0 percent ≥ & < 3 percent | ≥3 percent |  |
| Valley | <0 percent | 0 percent ≥ & < 3 percent |  |
| Steep Valley | <0 percent | ≥5 percent |  |
| Plateau | ≥3 percent | 0 percent ≥ & < 3 percent |  |
| Plain | 0 percent ≥ & < 3 percent | 0 percent ≥ & < 3 percent |  |
| Mountain | ≥3 percent | <0 percent |  |
| Cliff | 0 percent ≥ & < 3 percent | <0 percent |  |
| Slippery Slope | <0 percent | <0 percent |  |
Source/Notes: SOURCE: Authors' classifications based on Pritchett (2000). NOTE: Index refers to constant per capita public spending on health using first year as the base year.
Given the relatively short time period over which cross-country data are available, the method allows for only a single break point. The choice of a minimum of three years is arbitrary and for illustrative purposes only. In country-specific applications of this analysis, where longer time series data may be available, additional break points could be considered.
3. Study results
Applying the decomposition methodology reveals that, globally, more than half of the increase in per capita public spending on health has been the result of economic growth. This finding is broadly consistent with others in the literature, such as those reported by the Global Burden of Disease Health Financing Collaborator Network (2019) and Saxenian et al. (2019). For the remainder, increases in total public spending contributed more than reprioritization across LMICs, whereas the reverse was true in HICs by a very large margin (Table 2 ). Some of the largest increases in per capita public spending for health occurred among LMICs in the ECA and EAP regions, including in countries such as Armenia, Azerbaijan, China, Georgia, Indonesia, and Vietnam. Reprioritization accounted for less than one-fifth of the change in public spending for health in LMICs, less than half of its contribution among HICs.
Table 2.
Accounting for changes in public spending for health, 2000–2017.
| N | Annual growth in per capita GDP (%) | Per capita public spending on health |
||||||
|---|---|---|---|---|---|---|---|---|
| 2000 (constant 2017 US$) | Annual growth (%) | 2017 (constant 2017 US$) | Decomposition, share from: |
|||||
| Economic growth (%) | Change in total public spending (%) | Reprioritization for health (%) | ||||||
| LMICs | 106 | 2.9 | 59 | 4.3 | 119 | 67 | 18 | 15 |
| LIC | 27 | 2.0 | 8 | 4.0 | 14 | 51 | 41 | 8 |
| LMI | 39 | 3.3 | 29 | 4.5 | 59 | 72 | 16 | 12 |
| UMI | 40 | 3.1 | 123 | 4.4 | 248 | 71 | 6 | 23 |
| SSA | 42 | 2.0 | 27 | 3.8 | 50 | 53 | 26 | 21 |
| SAR | 6 | 4.2 | 20 | 3.5 | 33 | 69 | 10 | −21 |
| MNA | 8 | 1.9 | 89 | 3.9 | 154 | 48 | 14 | 38 |
| EAP | 13 | 4.3 | 40 | 6.0 | 93 | 72 | 20 | 8 |
| ECA | 19 | 4.8 | 79 | 6.1 | 184 | 78 | 6 | 15 |
| LAC | 18 | 2.0 | 127 | 2.9 | 242 | 67 | 19 | 14 |
| HICs | 44 | 1.6 | 1327 | 3.2 | 2129 | 49 | 10 | 40 |
| Non-OECD | 15 | 1.6 | 494 | 3.5 | 858 | 45 | 23 | 31 |
| OECD | 29 | 1.6 | 1758 | 3.1 | 2786 | 52 | 3 | 46 |
| All | 150 | 2.5 | 431 | 4.0 | 708 | 63 | 16 | 21 |
Source/Notes: SOURCE: Authors' calculations using data from the WHO Global Health Expenditure Database. NOTE: All US$ numbers are in constant 2017 terms; Shares may not add up to 100% due to rounding.
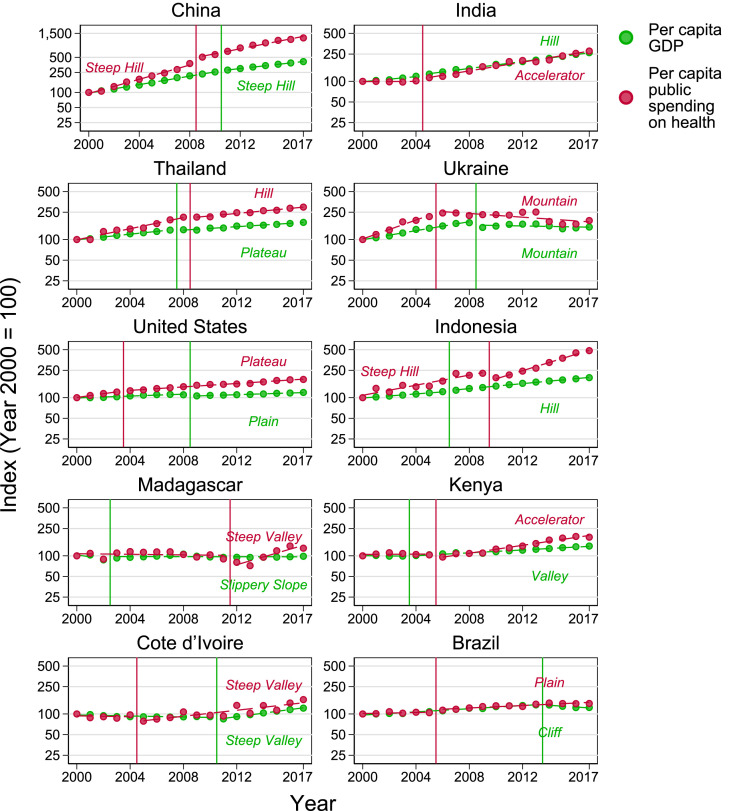
Although some countries experienced consistently steady linear growth in both per capita GDP and per capita public spending for health, most showed large shifts in trends often with statistically-identifiable break points that occurred primarily in 2008, the year of the global financial crisis, following which average growth rates declined significantly (Table 3 ). Fig. 1 shows some country examples.
Table 3.
Statistics on instability of growth rates, 2000–2017.
| Summary from ‘best break’ analysis |
|||||
|---|---|---|---|---|---|
| Mean break year | Percentage point shift | Growth rate before break | Growth rate after break | R2 of trend | |
| LMICs | |||||
| Per capita GDP | 2008 (3) | −1.1 (4.6) | 3.4 (4.0) | 2.3 (2.9) | 0.81 (0.29) |
| Per capita public spending for health | 2009 (3) | −4.3 (14.9) | 5.4 (8.0) | 1.1 (13.3) | 0.65 (0.31) |
| HICs | |||||
| Per capita GDP | 2008 (2) | −0.5 (3.2) | 1.9 (2.8) | 1.4 (1.8) | 0.69 (0.28) |
| Per capita public spending for health | 2008 (2) | −1.2 (5.8) | 3.9 (4.6) | 2.7 (3.0) | 0.73 (0.31) |
Source/Notes: SOURCE: Authors' calculations using data from WHO Global Health Expenditure Database. NOTE: Standard deviation in parenthesis.
Fig. 1.
Caption: Per capita GDP and public spending on health, by patterns of growth, 2000–2017, Source/Notes: SOURCE: Authors' analysis using data from WHO Global Health Expenditure Database. NOTE: Y-axes are expressed in logarithmic scale.
4. Discussion
A few countries such as Ukraine, Cote d’Ivoire, and China showed the same trend patterns for both per capita GDP and public spending on health (Fig. 1). However, many countries including Madagascar, Brazil, Kenya, India, Indonesia, Thailand, and the United States, among others, changed trend patterns, sometimes significantly. For example, economic growth was negative in Brazil following 2014, with a per capita GDP landscape that can be characterized as a ‘cliff’. During the period, the country also experienced a decline in the total public revenue share of GDP. However, reprioritization efforts combined with a deficit-fueled rise in total public spending protected levels of per capita public spending for health from declining thus leading to a ‘plateau’ landscape.
Indonesia was an ‘accelerator’ for per capita GDP but a ‘steep hill’ for per capita public spending for health, primarily because priority for health increased in recent years especially after 2014 when a new administration took office. The trend in Madagascar changed from being a ‘slippery slope’ for economic growth to a ‘steep valley’ for per capita public spending on health: economic growth was relatively stagnant from 2000 to 2017 leading to an almost flat landscape for per capita GDP. Volatility in public spending for health prior to the break in trend was primarily a result of changes in priority; and a steady increase in health’s share of total public spending is the reason for the ‘steep valley’ landscape for the latter post-2011.
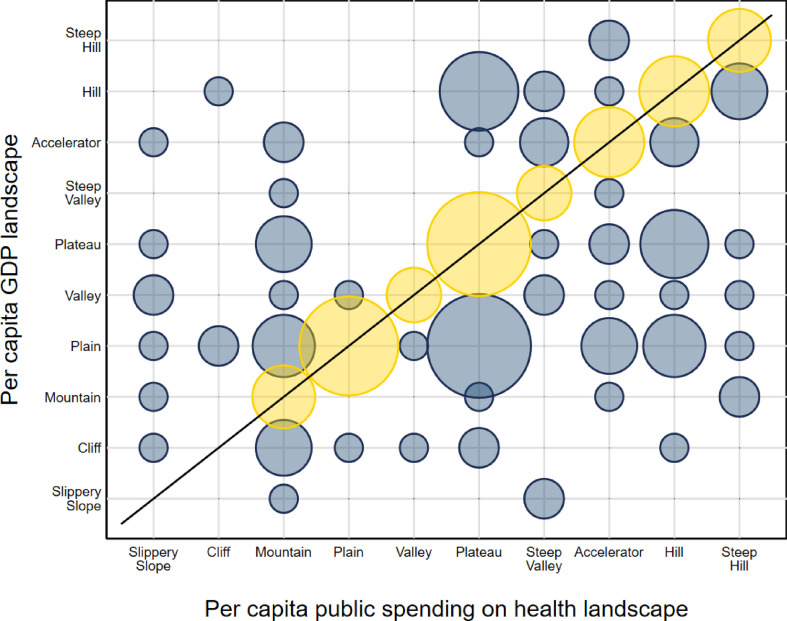
Overall, close to 70 percent of all countries in the sample (105 out of 150) showed different trend patterns for per capita public spending on health vis-à-vis economic growth. These differences were due to the intermediating effect of changes in total public spending and prioritization for health. In some cases, the adverse impact of a decline or volatility in per capita GDP was offset by corrective action by both a rise in total public spending and a higher priority for health; in other countries, the impact of changes in income on per capita public spending on health were magnified due to same-direction movements in prioritization and total public spending on health. In general, if the landscapes are ordered by decreasing growth rates following break points as in Fig. 2 , countries tend to be more likely to lie below the diagonal suggesting some evidence of counter-cyclicity for protecting public spending on health. Of the 105 countries with differing landscape patterns, close to two-thirds (70) fall below the diagonal.
Fig. 2.
Caption: Landscape distribution of countries, 2000–2017, Source/Notes: SOURCE: Authors' analysis using data from WHO Global Health Expenditure Database. NOTE: Chart shows concentration of countries per combination of per capita GDP landscape and per capita public spending on health landscape. Larger circles indicate higher number of countries. Yellow circles indicate countries with the same landscape for both per capita GDP and per capita public spending on health. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
5. Conclusions
Taking a retrospective data-driven decomposition approach can help countries better understand where realizations in per capita public spending for health have come from -- to assess both the potentially additive and ‘cancelling out’ effects of changes in income, prioritization, and total public spending -- and to inform how future trends might be impacted. The decomposition results show that economic growth was the main driver of changes in public spending on health. While the tendency is for changes in per capita public spending on health to go in the same direction as changes in per capita GDP, intermediating effects of changes in total public spending and prioritization for health led to different landscapes between per capita public spending on health and per capita GDP for majority of the countries. Such corrective action by both a rise in total public spending and a higher priority for health help mitigate the adverse impacts of a decline or volatility in per capita GDP. Thus while country context matters, the importance of economic growth for public spending on health underscores the critical need to situate, integrate, leverage, and proactively manage health financing reforms within a country's overall macro-fiscal context and to emphasize the need for counter-cyclical policies to support per capita public spending for health during economic downturns. On the flip side, the relatively marginal role of changes in priority for increasing public spending for health is notable, especially given how much effort and advocacy has focused on this aspect (African Union, 2001; Tandon et al., 2014). These lessons are now even more critical given the current global COVID-19 pandemic. Based on projections by the IMF (2020), the current crisis is expected to result in greater declines in economic growth than the 2008–2009 global financial crisis. The impact on public spending on health will depend on the extent to which expansionary fiscal policies and health reprioritization occurs. It is during these periods that it is particularly important to ensure levels of public financing are protected and increased to maintain effective service coverage and financial risk protection towards UHC.
Another key point is the diversity of growth trajectories across countries and, especially, the volatility in trends over time. The implications are clear: capturing economic growth or per capita public spending for health with a single growth rate is not the best metric to characterize country experiences. Changes in patterns are often in of themselves of interest to highlight reasons behind underlying breaks in dynamics of growth and in assessing potential impact on health systems and sustainability of reforms. Further analysis is needed to determine the extent to which the breaks and different landscapes are associated with changes in service delivery and health systems outcomes, including OOP spending for health.
Credit author statement
Ajay Tandon: Conceptualization, Methodology, Supervision, Writing-Original Draft. Jewelwayne Cain: Software, Validation, Data Curation, Visualization, Writing-Original Draft. Christoph Kurowski: Conceptualization, Supervision. Adrien Dozol: Validation, Writing-Review & Editing. Iryna Postolovska: Validation, Writing-Review & Editing.
Details of funding source
This work was conducted under the auspices of the World Bank's Multi-Donor Trust Fund for Integrating Externally-Financed Health Programs supported by Australia's Department of Foreign Affairs and Trade.
Acknowledgements
The authors are grateful for comments and feedback received from Aneesa Arur, Volkan Cetinkaya, Adrien Dozol, Carol Dayo, Zelalem Debebe, Patrick Eozenou, Reem Hafez, Susan Ivatts, Laurence Lannes, Emiko Masaki, Nicolas Rosemberg, Andre Medici, Maude Ruest, George Schieber, Owen Smith, Shakil Ahmed, Ellen Van De Poel, Hideki Higashi, Hui Sin Tao, and Toomas Palu. We also acknowledge the insights received from the facilitators and participants of the Domestic Resource Mobilization collaborative of the Joint Learning Network (JLN) including Somil Nagpal, Maria Eugenia Bonilla-Chacin, Triin Habicht, Aditi Nigam, Valerie Ulep, and senior policymakers from 17 countries who participated and contributed to discussions. The findings, interpretations and conclusions expressed in the paper are entirely those of the authors, and do not represent the views of the World Bank, its Executive Directors, or the countries they represent.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2020.113171.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- African Union . 2001. pp. 24–27.http://www.un.org/ga/aids/pdf/abuja_declaration.pdf (Abuja Declaration on HIV/AIDS, Tuberculosis, and Other Related Infectious Diseases, African Summit on HIV/AIDS, Tuberculosis, and Other Related Infectious Diseases). April: Abuja, Nigeria. [Google Scholar]
- Global Burden of Disease Health Financing Collaborator Network Past, present, and future of global health financing: a review of development assistance, government, out- of-pocket, and other private spending on health for 195 countries, 1995–2050. Lancet. 2019 doi: 10.1016/S0140-6736(19)30841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Monetary Fund . 2020. World Economic Outlook, April 2020: the Great Lockdown.https://www.imf.org/en/Publications/WEO/Issues/2020/04/14/weo-april-2020 [Google Scholar]
- Kutzin J. Anything goes on the path to universal health coverage? No. Bull. World Health Organization, Nov 1. 2012;90(11):867–868. doi: 10.2471/BLT.12.113654. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3506412/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development, Eurostat, & World Health Organization . 2011. A System of Health Accounts.https://www.who.int/health-accounts/methodology/sha2011.pdf [Google Scholar]
- Pritchett L. Understanding patterns of economic growth: searching for hills among plateaus, mountains, and plains. World Bank Econ. Rev. 2000;14(2):221–250. [Google Scholar]
- Saxenian H., Bharali I., Ogbuoji O., Yamey G. A quantitative analysis of sources of changes in government expenditures on health, 2000 to 2015: what can we learn from experience to date? Gates Open Res. 2019;3:5. doi: 10.12688/gatesopenres.12900.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon A., Fleisher L., Rong L., Yap W.A. Reprioritizing government spending on health: pushing an elephant up the stairs? WHO South East Asia. J. Publ. Health. 2014;3(3):206–212. doi: 10.4103/2224-3151.206742. [DOI] [PubMed] [Google Scholar]
- Tandon A., Cain J., Kurowski C., Postolovska I. World Bank Group; Washington, D.C.: 2018. Intertemporal Dynamics of Public Spending for Universal Health Coverage: Accounting for Fiscal Space across Countries. HNP Discussion Paper.http://documents.worldbank.org/curated/en/639541545281356938/Intertemporal- Dynamics-of-Public-Financing-for-Universal-Health-Coverage-Accounting-for-Fiscal- Space-Across-Countries [Google Scholar]
- World Bank . World Bank Group; Washington, D.C.: 2017. Tracking Universal Health Coverage: 2017 Global Monitoring Report.http://documents.worldbank.org/curated/en/640121513095868125/Tracking-universal- health-coverage-2017-global-monitoring-report [Google Scholar]
- World Bank . World Bank Group; Washington, D.C: 2019. High-Performance Health Financing for Universal Health Coverage: Driving Sustainable, Inclusive Growth in the 21st Century.http://documents.worldbank.org/curated/en/641451561043585615/Driving-Sustainable- Inclusive-Growth-in-the-21st-Century [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.