Abstract
Vibrio vulnificus infection was first reported as a necrotizing skin disease of unknown cause in Korea in 1979. In the early days, this disease caused panic across the country due to dreadful wound and its high mortality. Since then, the nature of the disease has become better understood and the overwhelming public fear has dissipated. However, there are still a certain number of infected patients each year and the high mortality rate remains a major health and social problem. From this review on historical and clinical perspective, better understanding of V. vulnificus infection would provide valuable information for public health planning.
Keywords: Vibrio vulnificus, Necrotizing fasciitis, Sepsis, Gangrene
History and epidemiologic characteristics
Vibrio vulnificus infection is a fatal disease that results in high fever and hemorrhagic necrotic skin lesions, and 50% of infected patients die from septic shock [1]. V. vulnificus was first reported in 1976 by Hollis et al in the United States, where, unlike other species of the genus Vibrio, it caused extraintestinal infections in humans and had biochemical characteristics that were distinguishable from those of other species [2]. In 1979, it was reported that infection with V. vulnificus led to primary sepsis or wound infection [3], leading to the name of the pathogen (vulni = wound, ficus = to make) due to it causing a distinct type of skin lesions [4].
V. vulnificus seems to have existed before the 1970s, considering that it can be found wherever its survival conditions are met. The cases presumed to be V. vulnificus infection were also described in antiquity in the records of Hippocrates and in the book, “The principle of surgery,” published in 1801 [5,6]. This disease rarely occurs in clean sea areas without tidal flats or in areas with low water temperature. Even in areas with tidal flats, these bacteria proliferate in areas with high chemical oxygen demand (COD), an indicator that reflects the degree of pollution. This suggests that recent environmental changes have led to an increase in occurrence of infection, and the presence of the bacteria and the infection have become known [7].
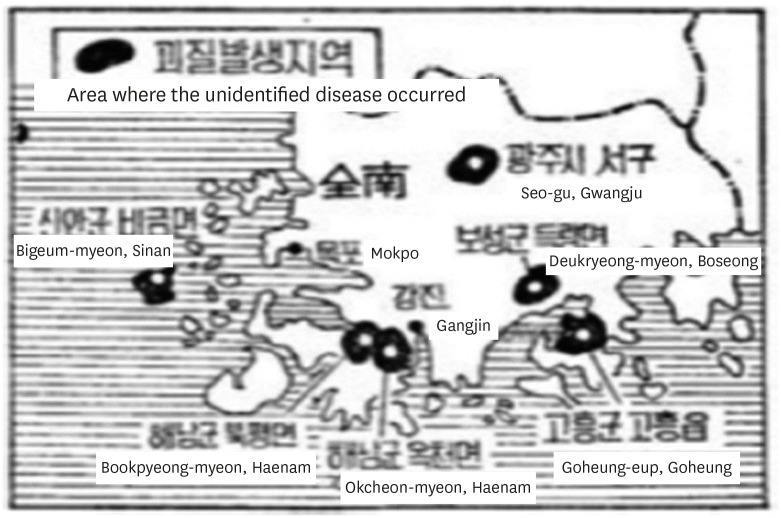
In Korea, V. vulnificus infection was first reported in Jeollanam-do in 1979. At the time, it was reported in the media that "from August to October, an unknown malignant skin disease occurred in rural areas of Jeollanam-do (Fig. 1), affecting 10 persons, seven of them died 3 - 4 days after symptoms began”. This led to significant social ramifications [8]. An epidemiological investigation team was dispatched. The Ministry of Health and Social Affairs at the time stated that the disease was "a non-infectious malignant necrotic dermatitis, most likely caused by a deteriorating wound from an insect bite from mosquito or leech" [9]. Subsequently, Dr. Jung-Soon Koo and Dr. Yoon-Sup Jeong each reported infection caused by V. vulnificus for the first time in 1982 [10,11]. The following year, in 1983, Dr. Yeong Pyo Kim and Dr. Seok Don Park revealed that the so-called “the unknown skin disease” reported in 1979 was also caused by V. vulnificus infection, confirming its domestic occurrence [12].
Figure 1. An unidentified epidemics in Jeollanam-do.
Source: Kyunghyang Shinmun, November 27, 1979.
After it was found that the cause of the unidentified disease was V. vulnificus, the infection cases were reported all over the country. In 1984 and 1985, the media reported serious symptoms of infections, such as gangrene and hemorrhagic bullae, resulting in a "gangrene wave" that caused panic throughout the whole country. When the route of infection was identified as contaminated seafood, socio-economic panic was created where "fisherman and fish farmers were struggling because the seafood they produced were not being sold, and the seafood restaurants fell into recession due to a drastic decrease in the number of customers" [13].
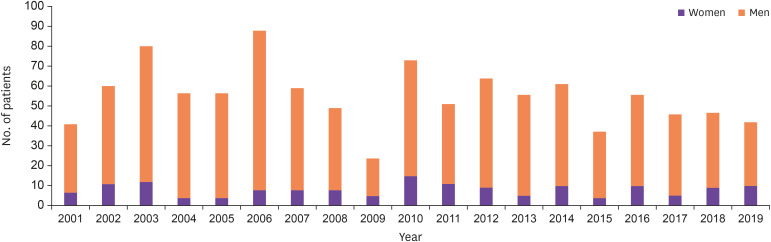
Since then, the epidemiology of the disease has become better understood and the overwhelming public fear has dissipated; however, there are still a certain number of infected patients each year and the high mortality rate remains a major health and social problem. In Korea, based on the laboratory-based pathogen surveillance system, which had started in 1994, eight patients in 1994, 16 patients in 1995, 11 patients in 1996, 13 patients in 1997, and 44 patients in 1998 were bacteriologically confirmed [14]. In 2000, it was designated as a group III National Notifiable Infectious Diseases; since then, the number of patients reported is 24 – 88 per year (Fig. 2) [15] and the incidence rate is approximately 0.05 – 0.18 per 100,000 people. Given the passive reporting system and number of cases where patients were treated or died without diagnosis, the actual number of cases could be much higher than this.
Figure 2. Number of patients with Vibrio vulnificus infection by year (2001 – 2019). Source: Korean Centers for Disease Prevention and Control.
The occurrence of V. vulnificus infection is highly related to changes in the natural environment. In Korea, it mainly occurs from May to November every year because V. vulnificus multiply more when the temperature of the seawater rises above 18 – 20°C; consequently, the number of bacteria in the seawater and seafood increases at this time [16]. According to the results from surveillance cultures of domestic seawater, bacteria multiply mainly in the seawater and tidal flats of the southern and western coastal areas and is also isolated in the seawater from Ganghwa island, Gimpo, Gangneung, Ulsan, Busan, and Jeju island.
Before 2011, the first patients were generally reported between June and July. Since then, the first patients became reported earlier by year: in May in 2012-2014 and in April in 2017-2018. This phenomenon seems to be related to an increase in the average temperature of seawater. There was also an increase in the incidence of patients after an increase in precipitation or after heavy rain [17,18]. This may be because, although V. vulnificus is halophilic, it grows well at a relatively low salinity (10 – 18 ‰). If the amount of freshwater flowing into the coast due to heavy rain increases, the salinity of the seawater is lowered, leading to a proliferation of V. vulnificus.
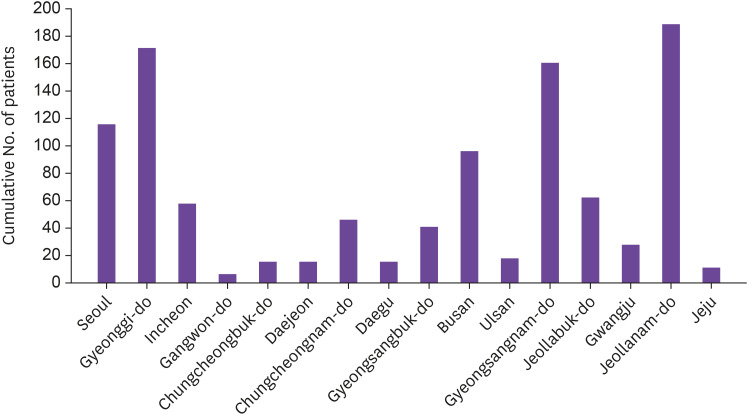
Looking at the number of patients by region, even though there are more cases in the southern and western coastal regions such as Jeollanam-do, Gyeongsangnam-do, and Gyeonggi-do, cases occur throughout the whole country, including inland regions (Fig. 3) [15]. This seems to stem from the geographical characteristics of Korea, which is bordered by sea on three sides, and the culture of enjoying raw seafood.
Figure 3. Regional cumulative number of patients with Vibrio vulnificus infection (2001 - 2019).
Source: Korea Centers for Disease Prevention and Control.
Disease characteristics in Korea
1. Microbiologic characteristics
V. vulnificus is a Gram-negative rod bacterium. It is found along the coast where the water temperature is 9 – 31°C and is widely detected in Korea's coastal waters, seawater in estuaries, sea sediments, tidal flats, and various types of fish, seaweed, and plankton. Shellfish, such as oysters, clams, mussels, and scallops, are filtration feeders and V. vulnificus, which is ingested with seawater, is concentrated in their tissue, leading to shellfish becoming a major source of infection.
The temperature and salinity of seawater greatly affect the proliferation of V. vulnificus. It multiplies well when the water temperature is above 18 – 20°C. At lower temperatures, the bacteria are detected but have a slower growth rate and the population decreases when the temperature rises above 30°C. In terms of salinity, about 10 – 18‰ is the most optimal concentration for growth. When salinity is lower than 2 – 2.5‰ or higher than 35‰ like in the deep sea, the bacteria are barely detected [16].
2. Clinical characteristics
V. vulnificus infection usually manifests as a primary sepsis or wound infection. It can also occur as a form of gastroenteritis. Cases of pneumonia, meningitis, spontaneous bacterial peritonitis, endometritis, osteomyelitis, septic arthritis, endophthalmitis, and keratitis have been rarely reported.
Primary sepsis occurs mainly as a bacteremia with no clear entry site of infection in people with risk factors or underlying diseases. Symptoms appear on average 2 – 2.5 days after consuming contaminated seafood, as early as within 3 hours of exposure, mostly within 7 days, and as late as 14 days after exposure. Patients suddenly develop fever and chills; sometimes, gastrointestinal symptoms, such as vomiting, nausea, stomach pain, and diarrhea, appear first. When symptoms of sepsis begin, the blood pressure drops in 60 – 70% of patients. Skin lesions developing as a metastatic infection are observed in more than 90% of patients, more frequently in the limbs, especially the legs. Skin lesion proceeds from erythema to ecchymosis, bullae, large hemorrhagic bullae, and ulcers, which later progress into necrotizing fasciitis and myonecrosis (Fig. 4). More than half of the patients arrived at the hospital with low blood pressure, decreased consciousness, and oliguria, which meant that in many cases, patients visit hospital late after sepsis has progressed to severe condition [19,20].
Figure 4. Skin lesions of a patient with Vibrio vulnificus sepsis.
Provided by Chonnam National University Hospital
The wound infection type shows limited lesion along area where the bacteria infect through damaged skin. It can occur in people without underlying diseases. Symptoms appear 12 – 72 hours after exposure and usually develop within 7 days, but the incubation period may last until 12 days after exposure. Depending on their immune status, mild disease may recover, but in more than half of patients it progresses to severe disease, such as necrotizing fasciitis with hemorrhagic bullae and necrotizing vasculitis, within 24 hours of symptoms developing.
3. Routes of infections
V. vulnificus sepsis is caused by eating raw or undercooked seafood contaminated with V. vulnificus. Vegetables and cooking utensils, if washed with contaminated seawater, can be the source of infection as well. In the United States, oysters are considered the main source of infection [16]. In Korea, various seafood such as trout, mudskippers, small octopus, crab, shrimp, and shellfish are involved as an infection source [20]. V. vulnificus is frequently identified in seawater, tidal flats, shellfish caught from the coast of Korean peninsula and water in aquariums when the seawater temperature rises above 18–20°C. Nevertheless, the incidence of V. vulnificus infection is not that high even in this season. This is because the development of the V. vulnificus infection is largely affected by host immunity. Of all affected patients, 90 – 95% have underlying diseases, especially chronic liver disease such as chronic hepatitis B, C or alcoholic cirrhosis. Among patients who reported they had no underlying disease prior to V. vulnificus infection, it has been found that many of them already had chronic liver diseases due to long-term drinking. Wound infections, which occur rarely, caused by open wounds exposed to contaminated seawater, tools trimming seafood, fishing needles or fishery products.
4. Diagnosis and treatment
If patients with risk factors present with typical symptoms, presumptive diagnosis is possible. The history of consuming raw or undercooked shellfish, contact with seawater, or injury during fishing or cleaning seafood helps the diagnosis. The diagnosis is confirmed when V. vulnificus is isolated from cultures of blood or skin lesions. For the best prognosis, rapid diagnosis, rapid antibiotic administration, and proper surgical treatment are important. According to recent data in Korea, the mortality rate is still very high, on average of 53% [19].
Prevention and control policies in Korea
As V. vulnificus is ubiquitous worldwide in the environment as commensal, eradication is impossible; therefore, activities to prevent human infection are mainly focused on environmental monitoring and public education. In 1992, the National Institutes of Health (currently the Korea Centers for Disease Control and Prevention, KCDC) started a monthly laboratory surveillance project that all Vibrio isolates from the samples collected by the local governments were investigated for species identification and antimicrobial susceptibility tests. Since 1994, occurrence of V. vulnificus infection has been monitored as part of a laboratory-based pathogen surveillance system. In the revised law on the prevention of infectious diseases that took effect on August 1, 2000, V. vulnificus infection was designated as a group III national notifiable infectious disease. In 2006, the KCDC started the “Pathogenic Vibrio Lab Monitoring project” [21]. This project surveys whether pathogenic Vibrio bacteria (V. cholerae, V. vulnificus, V. parahaemolyticus, etc.) are detected in seawater, aquarium water, and distributed fisheries on the domestic coast. Eleven National Quarantine Stations (Busan, Incheon, Gunsan, Mokpo, Yeosu, Masan, Tongyeong, Ulsan, Pohang, East Sea, and Jeju) participate in this surveillance project. The Institute of Health and Environment (Incheon and Jeonnam) also joined to this surveillance since 2008. In 2017, the Ministry of Food and Drug Safety and KCDC launched “V. vulnificus monitoring and prediction system”. This system predicts the likelihood of V. vulnificus infection outbreak by monitoring the marine environment, such as water temperature and salinity, in real-time in 41 base areas including major ports, fish farms, and beaches. And it provides the risk levels of V. vulnificus infection in real time to the public, which are divided into four levels of attention, caution, warning and danger. This system intended to prevent V. vulnificus infection by predicting and warning of its occurrence. It also provides public education and promotion programs for prevention of V. vulnificus infection.
Everyone, especially those with underlying diseases, should follow good practices for preventing infection. Fish and shellfish should be thoroughly cooked (It is important to cook for an adequate amount of time to achieve sterilization; after the shell is opened, they need to be heated for an additional 5 to 9 minutes). Those with open skin injuries should not enter the seawater. Cooking utensils, such as cutting boards or knives, used for cooking raw fish or shellfish should not have contact with other foods. Gloves should be worn when handling seafood. In particular, patients with chronic diseases, such as liver diseases or diabetes, gastrointestinal tract diseases, or reduced immunity, should be more cautious because they have a higher morbidity and fatality. Many people living on the coast do not know whether they have chronic liver disease until V. vulnificus infection occurs, so more preventive training is necessary for residents on the coast. Heavy drinkers should be careful not to consume raw seafood during the summer.
Footnotes
Conflict of Interest: No conflicts of interest.
- Conceptualization: SIJ, KRP.
- Data curation: SJK.
- Writing - original draft: SJK, SIJ.
- Writing - review & editing: KRP.
This secondary publication is based on ‘Korean Society of Infectious Diseases (KSID). Korean History of Infectious Diseases II. Seoul: Koonja; 2018. (ISBN 979-11-5955-379-0)’.
References
- 1.Horseman MA, Surani S. A comprehensive review of Vibrio vulnificus: an important cause of severe sepsis and skin and soft-tissue infection. Int J Infect Dis. 2011;15:e157–66. doi: 10.1016/j.ijid.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 2.Hollis DG, Weaver RE, Baker CN, Thornsberry C. Halophilic Vibrio species isolated from blood cultures. J Clin Microbiol. 1976;3:425–431. doi: 10.1128/jcm.3.4.425-431.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blake PA, Merson MH, Weaver RE, Hollis DG, Heublein PC. Disease caused by a marine Vibrio. Clinical characteristics and epidemiology. N Engl J Med. 1979;300:1–5. doi: 10.1056/NEJM197901043000101. [DOI] [PubMed] [Google Scholar]
- 4.Farmer JJ., 3rd Vibrio (“Beneckea”) vulnificus, the bacterium associated with sepsis, septicaemia, and the sea. Lancet. 1979;2:903. doi: 10.1016/s0140-6736(79)92715-6. [DOI] [PubMed] [Google Scholar]
- 5.Baethge BA, West BC. Vibrio vulnificus: did Hippocrates describe a fatal case? Rev Infect Dis. 1988;10:614–615. doi: 10.1093/clinids/10.3.614. [DOI] [PubMed] [Google Scholar]
- 6.Hassing RJ, de Groot YJ, Kompanje EJ. A description and illustration of a necrotizing fasciitis by John Bell in 1801, hypothetically caused by Vibrio vulnificus . Int J Infect Dis. 2010;14(Suppl 3):e341–3. doi: 10.1016/j.ijid.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Lee JH, Choi HI. Korea Health Industry Development Institute. R&D Trend. [Accessed 14 May 2020]. Available at: https://www.khidi.or.kr/board/view?linkId=178943&menuId=MENU01435.
- 8.The Kunghyang Shinmun. An unknown malignant skin disease occurred in rural areas of Jeollanam-do. 1979. Nov 27, [Google Scholar]
- 9.The Dong-a Ilbo. The unknown malignant skin disease in Jeollanam-do: non-infectious. 1979. Dec 03, [Google Scholar]
- 10.Goo JS, Kim DW, Han KS, Suk JS, Park MH, Kim SI. Lactose-fermenting Vibrio (Vibrio vulnificus) Sepsis 5 cases. Korean J Pathol. 1982;16:463–469. [Google Scholar]
- 11.Chong Y, Park MY, Lee SY, Kim KS, Lee SI. Vibrio vulnificus septicemia in a patient with liver cirrhosis. Yonsei Med J. 1982;23:146–152. doi: 10.3349/ymj.1982.23.2.146. [DOI] [PubMed] [Google Scholar]
- 12.Kim YP, Jeon IG, Na HC, Park SD. Four cases of the unknown skin disease, fulminating gangrenous dermatitis syndrome, due to Vibrio; Korean Society of Dermatology. 35th Spring Conference; 1983. p. Abstract 19. [Google Scholar]
- 13.The Kyunghyang Shinmun. Deep distress for septic shock. 1985. Jul 19, [Google Scholar]
- 14.Shin YH, Lee JK, Oh KS, Yoo JS, Lee SW, Lee GY, Chung DJ, Kim KS. National Surveillance of Vibrio vulnificus Infections in 1998. Korean J Infect Dis. 1999;31:232–236. [Google Scholar]
- 15.Korean Center for Disease Control and Prevention (KCDC) Infectious disease portal. [Accessed 14 May 2020]. https://www.cdc.go.kr/npt/biz/npp/ist/bass/bassDissStatsMain.do.
- 16.Oliver JD. The biology of Vibrio vulnificus. Microbiol Spectr. 2015;3:VE-0001–2014. doi: 10.1128/microbiolspec.VE-0001-2014. [DOI] [PubMed] [Google Scholar]
- 17.Kim SH, Jang JY. Correlations between climate change-related infectious diseases and meteorological factors in Korea. J Prev Med Public Health. 2010;43:436–444. doi: 10.3961/jpmph.2010.43.5.436. [DOI] [PubMed] [Google Scholar]
- 18.Na W, Lee KE, Myung HN, Jo SN, Jang JY. Incidences of waterborne and foodborne diseases after meteorological disasters in South Korea. Ann Glob Health. 2016;82:848–857. doi: 10.1016/j.aogh.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 19.Kim DM, Hong SJ. Vibrio vulnificus sepsis. Korean J Med. 2012;82:671–679. [Google Scholar]
- 20.Jung YS, Jung SI, Kang SJ, Jun CH, Park KH, Shin JH, Chung EK. Clinical manifestations and prognostic factors in Vibrio vulnificus septicemia. Korean J Med. 2008;74:288–295. [Google Scholar]
- 21.Korean Center for Disease Control and Prevention (KCDC) Infectious diseases portal. Pathogenic vibrio lab monitoring project 2020. [Accessed 14 May 2020]. Available at: http://www.cdc.go.kr/npt/biz/npp/portal/nppVbStatsMain.do.