Abstract
Clusters of coronavirus disease 2019 (COVID-19) in long-term care facilities (LTCFs) have been widely reported in Korea and around the world. COVID-19 has a high mortality rate, and older patients and those with underlying diseases are at particularly high risk of being infected. Outbreaks in LTCFs, where many high-risk patients reside, result in the occupation of beds meant for severely ill patients and even death in many patients. Long-term care hospitals (LTCH) are major LTCFs in Korea. Therefore, it is very important to protect patients in LTCHs from COVID-19. The reality is that preparedness for COVID-19 in LTCHs is inadequate, and there are barriers to improvements in preparedness. Through institutional improvement and policy support, the government should help healthcare personnel and LTCHs improve installation and raise the level of knowledge of infection prevention and control. With these improvement, prevention, surveillance, and screening for COVID-19 should be done and a response system to the COVID-19 outbreak should be established. There are many challenges that must be overcome to meet the goals proposed in this article. This may be possible only with a spirit of solidarity and cooperation of government, public and private healthcare facilities.
Keywords: COVID-19, Long-term care facility, Preparedness
Introduction
Coronavirus disease 2019 (COVID-19) is an acute infectious respiratory disease caused by the severe acute respiratory syndrome coronavirus 2019 (SARS-CoV-2), which was first reported in Wuhan, China, on December 31, 2019 [1]. Since then, it was rapidly transmitted around the world. On March 11, 2020, the World Health Organiaztion declared a global pandemic. As of April 2020, 2,314,621 cases of COVID-19 were reported worldwide, resulting in 157,847 deaths [2]. It is estimated that the actual number of cases is higher than that reported [3].
COVID-19 causes severe pneumonia in about 15% of infected patients [4]. It has a particularly high fatality rate for older adults. In Korea, the fatality rate was 2.0% in those aged 50 years or older and 8.5% in those aged 80 or older, while it was less than 0.1% in those aged 50 or younger [5]. Higher fatality rates were also reported in patients with underlying diseases such as cardiovascular disease, compared to patients without such diseases [6]. In long-term care facilities (LTCFs), the residents were mainly older adults and those with underling diseases. Thus, individuals in LTCFs are at high risk of COVID-19. There are several news articles and reports of deaths associated with outbreaks in LTCFs around the world [7,8,9,10]. Long-term care hospitals (LTCHs), one of the LTCFs, play important role in long-term care service in Korea. Therefore, it is very important to protect individuals in LTCHs from COVID-19 and to ensure that patients, caregivers, and healthcare workers in LTCHs respond appropriately when infected by SARS-CoV-2. This article aims to review the current preparedness of LTCHs in the fight aginst COVID-19, and propose strategies to protect LTCHs during the COVID-19 pandemic.
Current status of long-term care hospitals in Korea
A LTCH is a LTCF aimed at providing medical services to patients who need long term care due to illness or disability. Since it is categorized as a medical institution, it is under the control of National Health Insurance Service and is required to have more than 30 beds for hospitalization, one doctor per 40 patients, and one nurse per 6 patients [11]. Unlike a LTCH, it is not mandatory to provide medical service in a nursing home that aims to support activities of daily living life in older adults. As of 2018, there were 1,363 LTCHs in Korea, of which 33.5% (457/1,363) were located in Seoul, Gyeonggi, and Incheon [12].
As shown in Table 1, patients in LTCHs are graded according to their need for medical services, behavior problems, and level of cognitive impairment. Of the patients hospitalized in LTCHs, 49.6% are included in the cognitive impairment or physical deterioration groups; those patients do not necessarily require medical services [12]. As shown in Table 2, 63.1% (861/1,363) of LTCHs were listed as facilities with 100 – 200 beds and 13.0% (178/1,363) had fewer than 100 beds. The Ministry of Health and Welfare evaluated the appropriateness of medical services of LTCHs according to criteria for medical personnel, necessary personnel, medical procedures, and medical results. Based on the above evaluation, LTCHs were classified into one of five grades. In the 2017 evaluation, only 18.2% (248/1,363) of LTCHs were classified in the first grade; most were classified in the second (37.2%) or third grade (23.7%) [12]. In particular, the proportion of first grade LTCHs with fewer than 200 beds, which accounts for 80% of LTCHs, was lower than that of LTCHs with more than 200 beds (14.4% [150/1,039] in LTCHs with <200 beds vs. 30.2% [98/325] in LTCHs with ≥200 beds; P <0.01). The median number of patients per physician was 31.8 (interquartile range [IQR] 29.4 to 33.6), and the median number of patients per nurse was 10.5 (IQR, 8.4 to 12.6). These results do not meet the Ministry of Health and Welfare’s requirment [12]. The National Health Insurance Service pays a LTCH a set amount for each patient according to the LTCHs grade [11].
Table 1. Characteristics of patients in long-term care hospital in Koreaa .
| Level | Criteria | Cases (%) |
|---|---|---|
| Highest medical service | Critical patient level including comatose, mechanical ventilator, internal bleeding | 10,910 (1.5) |
| High medical service | Very low ADL, refractory neurological disease, or pressure sore | 180,167 (25.6) |
| Medium medical service | Patient hospitalized in general room, low ADL, or with refractory neurological disease | 145,666 (20.7) |
| Low medical service | Patient receiving professional rehabilitation services other than the above mentioned criteria | 12,722 (1.8) |
| Problematic behavior | Delirum, hallucination, anxiety, wandering etc. | 5,617 (0.8) |
| Cognitive dysfunction | Cognive dysfunction clearly identified | 279,630 (39.7) |
| Physical deterioration | Cases other than the abov ementioned criteria | 69,743 (9.9) |
| Total | 704,475 (100.0) |
aReport by the Health Insurance Review and Assessment Service on the seventh evaluation of adequacy of inpatient payment in long-term care hospitals in 2018.
ADL, activities of daily living.
Table 2. Number and proportion of long-term care hospitals in Korea by grade and number of bedsa .
| Number of beds | ≥500 (n [%]) | 400 – 500 (n [%]) | 300 – 400 (n [%]) | 200 – 300 (n [%]) | 100 – 200 (n [%]) | <100 (n [%]) |
|---|---|---|---|---|---|---|
| 1st grade | 5 (29.4) | 5 (17.2) | 19 (22.4) | 69 (35.6) | 137 (15.9) | 13 (7.3) |
| 2nd grade | 7 (41.2) | 18 (62.1) | 41 (48.1) | 74 (38.1) | 338 (39.3) | 30 (16.9) |
| 3rd grade | 4 (23.5) | 5 (17.2) | 19 (22.4) | 35 (18.1) | 221 (25.7) | 39 (21.9) |
| 4th grade | 1 (5.9) | 1 (3.5) | 5 (5.9) | 9 (4.6) | 93 (10.8) | 34 (19.1) |
| 5th grade | 0 (0.0) | 0 (0.0) | 1 (1.2) | 6 (3.1) | 46 (5.3) | 31 (17.4) |
| Not graded | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.5) | 26 (3.0) | 31 (17.4) |
| Total | 17 (100.0) | 29 (100.0) | 85 (100.0) | 194 (100.0) | 861 (100.0) | 178 (100.0) |
aReport by the Health Insurance Review and Assessment Service on the seventh evaluation of adequacy of inpatient payment in long-term care hospitals in 2018.
COVID-19 cluster outbreaks in long-term care hospitals in Korea
As shown in Table 3, several clusters of COVID-19 outbreaks occurred in LTCHs across Korea. In particular, 126 cases were reported at Daegu Hansarang Nursing Hospital, and 72 at Gyeongsan Seo Nursing Hospital. When an outbreak occurs in an LTCH, infected patients need to be assigned to a high-risk bed; eventually, it is likely that beds meant for patients with severe COVID-19 will be filled quickly. There are only 27 beds for patients with severe COVID-19 in Gyeonggi Province. Just one outbreak of a cluster of COVID-19 in this province is enough to occupy all the beds for severe COVID-19.
Table 3. Current status of clusters of coronavirus disease 19 (COVID-19) in long-term care hospitals in Korea.
| Region | Name | Date of first patient diagnosis | Total number of patients per facility |
|---|---|---|---|
| Daegu | Gimshin Nursing Hospital | February 24, 2020 | 46 |
| Daegu | Shiji Elderly Nursing Hospital | March 6, 2020 | 16 |
| Daegu | Hansarang Nursing Hospital | March 17, 2020 | 126 |
| Daegu | Daesil Nursing Hospital | March 17, 2020 | 98 |
| Gyeongsan, Gyeongsanbuk-do | Seo Nursing Hospital | March 19, 2020 | 72 |
A case of COVID-19 who worked as an nursing assistant in a long-term care hospital
As a member of the Expert Committee of Gyeonggi COVID-19 Emergency Response Task Force, I had a chance to oversee an emergency response to a COVID-19 outbreak in a LTCH. Information on epidemiological investigation and emergency response is accessible at website of Bucheon COVID-19 status [13]. On March 9, 2020, a cluster outbreak was reported at a call center in a building in Guro, in Seoul. On March 8, 2020, an infected worker from the building had a service at a church located in Bucheon. After contact tracing, it was found that one of contact persons in this church were working as a nursing assistant at a LTCH; she tested as positive on March 12, 2020. She worked on March 10 and 11, 2020 at the LTCH and was then isolated from March 12, 2020. The infected nurse assistant did not complain of any symptoms and said that she had been wearing a mask and surgical gloves during patient care. This LTCH was spread over floors 2 through 5 in a five-story building that had a basement floor for parking. As of the confirmed date, there were 142 patients and 85 healthcare workers, including caregivers. Six to ten patients had been assigned to each room, and bed distance had been less than one meter apart. All patients and 22 healthcare workers were considered contact persons because the infected nurse assistant worked on all floors. The third and fourth floor were considered a highly contaminated zone, because the infected nurse assistant spent more time on those floors. The close contact patients who were in dischargeable condition and 16 healthcare workers were isolated at home. Of the patients who were hospitalized on the second toand fifth floor, 73 were transferred to public hospitals and nearby private acute care hospitals. The remaining patients were in the isolation cohort after the beds were repositioned to maintain a bed distance of 2 m or more. Caregivers were also in the isolation cohort in each room for patient care, and their in-hospital movement was restricted. Fourteen nurses and nurse assistants volunteered to be quarantined in the LTCH for patient care.
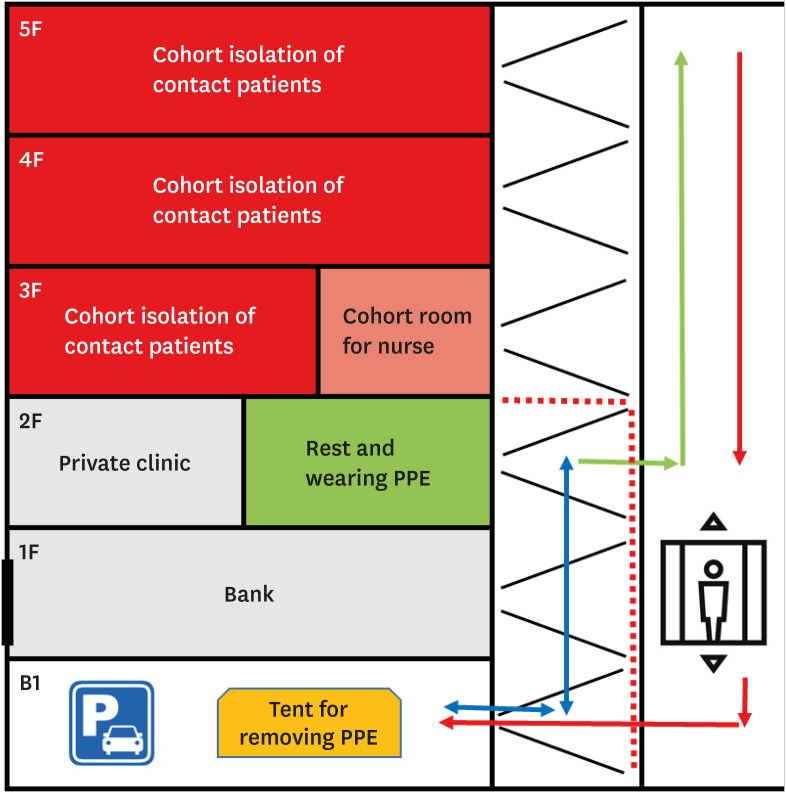
The layout of the space and movement flow are illustrated in Figure 1. Cohort nurses and nurse assistants stayed in the space on the third floor that was separated from the patients’ rooms. After disinfection, the second floor was used as a green zone for the movement of healthcare workers who had not been in contact with an infected person and who wore personal protective equipment (PPE). The parking lot on the first basement floor was temporarily used for removing PPEs. Visitors were prohibited from using the elevator, which was only used for medical personnel wearing PPE. Visitors were allowed to use the stairs to go to the bank and the private medical clinic located on the first and second floors., respectively. Meals for patients and employees were provided from outside. Fortunately, there were no more infected persons, and the quarantine was dismissed after all patients and employees tested negative 14 days from the start of quarantine.
Figure 1. Schema of isolation cohort of contact patients and staff members in a case of coronavirus disease 2019 (COVID-19) working as a nurse assistant in a long-term care hospital.
The green arrow represents the movement flow for healthcare workers wearing personal protective equipment (PPE) and the red arrow represents the movement flow after patient care. Nurse and nurse assistant cohorts stayed in a space that was separated from the patients’ rooms on the third floor. After disinfection, the second floor was used as a green zone for wearing PPE and working place for health care workers who had not had contact with a nursing assisstnat with COVID-19. The parking lot on the first basement floor was temporarily used for removing PPE. Visitors were forbidden to use the elevator, which was reserved for medical personnel wearing PPE. Visitors were allowed to use the stairs to go to the bank and the private medical clinic, which were located on the first and second floors (The blue arrow).
Obstacles to preventing outbreaks in long-term care hospitals in Korea
It would be very difficult to protect LTCHs from COVID-19 and rapidly respond to such an outbreak of COVID-19 in LTCHs owing to many systematical reasons. There are many patients in each room in beds that are close to each other; this seems to be a favorable condition for patient-to-patient transmission. There is insufficient space for isolation, quarantine, and grouping into cohorts in a LTCH. A previous survey done in 2018 reported that there were isolation rooms and negative pressure rooms in 58.5% (121/207) and 0.5% (1/208) in nursing hospitals in Korea [14]. Transfers of patients who have come in contact with infected persons are not easily accepted by other hospitals, owing to inadequate facilities for quarantine combined with the great fear of contamination. Knowledge among employess regarding infection control and prevention (IPC) in the LTCHs seems to be poor. Previous studies showed that infection control managers in LTCHs needed education on IPC [14,15]. The IPC team in my hospital should have educated nurses about the basics, such as disinfection, as well as putting on and takin off PPE. Additionally, caregivers who had closely cared for patients in the nursing hospital had no knowledge of the basics of IPC. In the event of an outbreak of COVID-19 in a LTCH, it is unclear who will communicate with the epidemiological investigator team and make decisions for rapid response. A building that is not built to provide medical service is not equipped with air ventilation; opening windows is the only the way to ventilate a room. Additionally, the movement of visitors and employees is hard to control, because a LTCH is also home to other private facilities. The COVID-19 test is not available at all LTCFs, because there is no safe installation or personnel trained in specimen collection, and no system for delivering specimens [16]. In the case, a regional public health community center have managed all the steps for testing for COVID-19 instead of a LTCH.
Suggestions for protecting individuals in long-term care hospitals from COVID-19
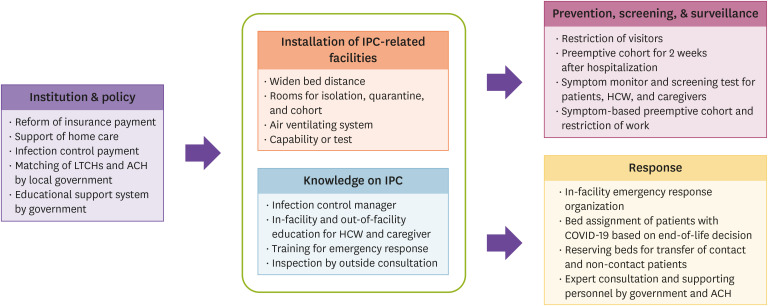
In Figure 2, suggestions for protecting individuals in LTCHs from COVID-19 are summarized. Improvement of installation and knowledge of IPC, which should be guided by institutional improvement and policy support, will strengthen the various aspects of preparedness, such as prevention, screening, surveillance, and rapid response action against COVID-19.
Figure 2. Schematic diagram of suggestions for preparedness for and response to coronavirus disease 2019 (COVID-19) in long-term care hospitals in Korea.
LTCH, long-term care hospitals; ACH, acute care hospitals; IPC, infection prevention and control; HCW, healthcare workers.
Currently, IPC is limited in LTCHs. This is inevitable given the increase in the population of older adults [17]. In addition, it is also due to institutional problems that can be ameliorated. First, many patients are forced to live in LTCHs, because family members are unable to take care of patients at home by themselves. The number of healthcare facilities providing hospital-based home care service are decreasing [18]. This is the major reason for overcrowding in LTCHs. A support policy could be implemented including home care staff members and visiting caregivers, and the government should guide patients to choose home care service rather than LTCHs [19]. Second, a payment system by which a LTCH receives a set amount of money per patient per day, forces it to hospitalize as many patients as they possibly can. Under the current payment system, managers of LTCHs place as many beds as possible in a room; as such, they cannot invest in installation and personnel for IPC [20,21]. The current payment system ought to, therefore, undergo reform to encourage preparedness for COVID-19 outbreaks. A special payment for IPC should be charged and LTCHs should be monitored to ensure proper use of the resources. Third, local governments should systematically match a LTCH with a regional acute care hospital that has an IPC expert because most LTCHs are unable to educate and train employees themselves [17]. The government should also provide an educational system for healthcare workers in LTCHs [17].
A higher installation rate of hygiene-related facilities are more likely to have better healthcare quality [22]. Infection control managers consider lack of isolation rooms as major obstacle for IPC in LTCHs [21]. The distance between beds should be widened to reduce contact and transmission of infections. Separate rooms for isolation and specimen collection should be established, and assigning rooms for newly hospitalized patients or patients with fever and respiratory symptoms are recommended to help reduce the possibility of transmission [23]. If possible, air ventilating systems are recommended to be installed for safe. Additionally, LTCHs should have their own testing units.
Regarding the knowledge of IPC, each LTCH should have its own infection control manager. The infection control manager should complete a course in IPC education provided by an academic institution, an acute care hospital, or the government. The content of education should reflect the reality of LTCHs [21]. The duties of infection control managers should be as follows: (1) to provide knowledge on IPC to employees, (2) to monitor and report suspected symptoms in patients and staff, (3) to plan emergency response actions and conduct training, and (4) to communicate with an epidemiologic investigator in case of a COVID-19 outbreak in their LTCH. The IPC team from the acute care hospital that is matched with LTCHs should regularly inspect the LTCHs and provide consultation on IPC.
The important means of preventing COVID-19 in LTCHs are preemptive isolation, screening, and testing; similar to that in a community setting. Patients should be screened for symptoms and signs of infection when they are hospitalized. Where possible, nursing hospitals should consider preemptive cohort rooms for monitoring of patients who were newly hospitalized during a possible incubation period [23]. If a patient has suspected symptoms and signs, this patient should be preemptively placed in an isolating room and be tested for COVID-19. Employees should report their symptoms and signs to an infection control manager before and during work [23,24]. At least twice a day, caregivers should also notify an infection control manager of symptoms they do or do not have [23,24]. Employees or caregivers with symptoms and signs should be isolated and allowed to come back to work only after a negative test result is confirmed. The government should find ways to financially support those staff members who are isolated and restricted from working. We can expect screening of patients, employees, and caregivers in LTCHs to be a surveillance system.
To minimize damage to a LTCH in case of a COVID-19 outbreak, response action must be rapid and appropriate. For this, the LTCH must prepare itself for emergency response action in which the role of every member is clearly assigned in advance. The decision should be made quickly under the direction of an epidemiology investigator who classifies those who are infected, those who have come in contact with infected persons, and those who have had no contact with infected persons. In a previous report, 63% (48/76) of residents in a nursing facility found asymptomatic in point-prevalence test [25]. This suggests that screening test for all patients should be considered in the case of COVID-19 in a LTCF [26]. If a nursing hospital lacks testing capability, it must be supported by the public health center. Patients with COVID-19 should be transferred in accordance with the bed allocation principle. If a patient’s intention to refuse life-saving treatment such as a mechanical ventilator is confirmed before hospitalization, the demand for beds for severe COVID-19 will be reduced. With the cooperation of acute care hospitals in the region, the government should secure beds for contact and non-contact patients who need to be transferred from a nursing hospital where an outbreak of COVID-19 has occurred. To prevent patient-to-patient transmission inside the LTCH, the transfer should be done promptly and according to the emergency response action plan. In addition, the local government should establish plans to deploy infection control experts and substitute personnel to support a LTCH where an outbreak of COVID-19 has occurred.
Conclusion
It seems impossible to prevent cluster outbreaks in LTCHs without installation of well-equipped facilities and trained staff members. There is a concern that cluster outbreaks in LTCHs result in many deaths and rapid occupation of beds meant for patients with severe COVID-19. Taking this situation seriously, the government should provide institutional and policy support to ensure that LTCHs are prepared for COVID-19 outbreaks. This may be possible only with a spirit of solidarity and cooperation of government, public and private healthcare facilities.
Acknowledgments
This review article is based on a presentation at the third Gyeonggi COVID-19 webinar as well as in-depth discussions in the Policy Committee on Emerging Infectious Diseases of the Korean Society of Infectious Diseases (KSID) and the Expert Committee of the Gyeonggi COVID-19 Emergency Response Task Force. This review article does not reflect an official opinion of either committee. I am grateful to the Infection Control and Prevention Team at Soonchunhyang University Bucheon Hospitals for aiding the management of COVID-19 a case in a LTCF.
Footnotes
Conflict of Interest: No conflicts of interest.
SUPPLEMENTARY MATERIAL
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) Coronavirus disease 2019 (COVID-19) situation report-91. [Accessed 23 April 2020]. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200420-sitrep-91-covid-19.pdf?sfvrsn=fcf0670b_10.
- 3.Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, Shaman J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science. 2020;368:489–493. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention. Coronavirus disease-19: The first 7,755 cases in the Republic of Korea. Osong Public Health Res Perspect. 2020;11:85–90. doi: 10.24171/j.phrp.2020.11.2.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korean Society of Infectious Diseases and Korea Centers for Disease Control and Prevention. Analysis on 54 mortality cases of coronavirus disease 2019 in the Republic of Korea from January 19 to March 10, 2020. J Korean Med Sci. 2020;35:e132. doi: 10.3346/jkms.2020.35.e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, Lewis J, Baer A, Kawakami V, Lukoff MD, Ferro J, Brostrom-Smith C, Rea TD, Sayre MR, Riedo FX, Russell D, Hiatt B, Montgomery P, Rao AK, Chow EJ, Tobolowsky F, Hughes MJ, Bardossy AC, Oakley LP, Jacobs JR, Stone ND, Reddy SC, Jernigan JA, Honein MA, Clark TA, Duchin JS. Epidemiology of Covid-19 in a long-term care facility in King county, Washington. N Engl J Med. 2020 doi: 10.1056/NEJMoa2005412. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bensadoun E. Nearly half of Canada's COVID-19 deaths linked to long-term care facilities: Tam. Global News. 13 April 2020. [Accessed 23 April 2020]. Available at: https://globalnews.ca/news/6811726/coronavirus-long-term-care-deaths-canada/
- 9.Georgia Department of Community Health. Long-term care facility COVID-19 report. [Accessed 23 April 2020]. Available at: https://dch.georgia.gov/announcement/2020-04-28/long-term-care-facility-covid-19-report.
- 10.Chidambaram P. State reporting of cases and deaths due to COVID-19 in long-term care facilities. [Accessed 23 April 2020]. Available at: https://www.kff.org/medicaid/issue-brief/state-reporting-of-cases-and-deaths-due-to-covid-19-in-long-term-care-facilities/
- 11.Ministry of Health and Welfare. Detailed matters concerning the application criteria and methods of National Health Insurance payment, Notice No. 2019-183. [Accessed 23 April 2020]. Available at http://www.mohw.go.kr/react/jb/sjb0406vw.jsp?PAR_MENU_ID=03&MENU_ID=030406&page=1&CONT_SEQ=350579.
- 12.Health Insurance Review & Assessment Service. The 7th report on the appropriateness of inpatient payment in long-term care hospitals in 2018. [Accessed 23 April 2020]. Available at: http://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020049000100&brdScnBltNo=4&brdBltNo=32.
- 13.Bucheon city. COVID-19 situation report. [Accessed 23 April 2020]. Available at: https://www.bucheon.go.kr/site/main/corona.
- 14.Kim OS, Jeong SY, Kim JY, So YR. Status of infection control and educational needs of nurses in long term care facilities in Korea. Korean J Rehabil Nurs. 2018;21:1–11. [Google Scholar]
- 15.Jung HY, Jung YK. Recognition and performance level of hospital infection control in nurses of long-term care hospital. Korean J Health Service Management. 2013;7:131–141. [Google Scholar]
- 16.European Center for Disease Preventiona and Control (ECDC) Infection prevention and control and preparedness for COVID-19 in healthcare settings-second update. [Accessed 23 April 2020]. Available at: https://www.ecdc.europa.eu/sites/default/files/documents/Infection-prevention-control-for-the-care-of-patients-with-2019-nCoV-healthcare-settings_update-31-March-2020.pdf.
- 17.Statistics Korea. 2017 population and housing survey. [Accessed 23 April 2020]. Available at: https://kostat.go.kr/portal/korea/kor_nw/1/2/2/index.board.
- 18.Song CR, Lee MK, Hwang MS, Yoon YM. The Current State of Hospital-based Home Care Services in Korea: Analysis of Data on Insurance Claims for Home Care from 2007 to 2012. J Korean Acad Soc Home Care Nurs. 2014;21:127–138. [Google Scholar]
- 19.Landers S, Madigan E, Leff B, Rosati RJ, McCann BA, Hornbake R, MacMillan R, Jones K, Bowles K, Dowding D, Lee T, Moorhead T, Rodriguez S, Breese E. The future of home health care: a strategic framework for optimizing value. Home Health Care Manage Pract. 2016;28:262–278. doi: 10.1177/1084822316666368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JH, Lee GE. Perception and practice of hospital infection control of nursing staff depending on the supplementation of nurses in long-term care hospitals. Korean J Occup Health Nurs. 2012;21:308–316. [Google Scholar]
- 21.Jeong SY, Kim OS, Choi JH, Lee SJ. Infection control tasks, difficulties, and educational needs of infection control practitioners in long term care facilities in Korea. Health Social Welfare Rev. 2018;38:331–362. [Google Scholar]
- 22.Sohn M, Choi M. Factors related to healthcare service quality in long-term care hospitals in South Korea: a mixed-methods study. Osong Public Health Res Perspect. 2017;8:332–341. doi: 10.24171/j.phrp.2017.8.5.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Korean Convalescent Hospital Association. Response manual against coronavirus disease 2019 (COVID-19) in convalescent hospitals. Ver 2.0. [Accessed 8 May 2020]. Available at: http://www.kagh.co.kr/NewsSite/View/Covid19/16675.nm.
- 24.National Health Insurance Service. Infection control report system. [Accessed 30 April 2020]. Available at https://medicare.nhis.or.kr/portal/index.do.
- 25.Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, Taylor J, Spicer K, Bardossy AC, Oakley LP, Tanwar S, Dyal JW, Harney J, Chisty Z, Bell JM, Methner M, Paul P, Carlson CM, McLaughlin HP, Thornburg N, Tong S, Tamin A, Tao Y, Uehara A, Harcourt J, Clark S, Brostrom-Smith C, Page LC, Kay M, Lewis J, Montgomery P, Stone ND, Clark TA, Honein MA, Duchin JS, Jernigan JA Public Health–Seattle and King County and CDC COVID-19 Investigation Team. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gandhi M, Yokoe DS, Havlir DV. Asymptomatic transmission, the Achilles' heel of current strategies to control Covid-19. N Engl J Med. 2020;382:2158–2160. doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.