Abstract
Introduction
The COVID-19 pandemic has substantially impacted maternity care provision worldwide. Studies based on modelling estimated large indirect effects of the pandemic on services and health outcomes. The objective of this study was to prospectively document experiences of frontline maternal and newborn healthcare providers.
Methods
We conducted a global, cross-sectional study of maternal and newborn health professionals via an online survey disseminated through professional networks and social media in 12 languages. Information was collected between 24 March and 10 April 2020 on respondents’ background, preparedness for and response to COVID-19 and their experience during the pandemic. An optional module sought information on adaptations to 17 care processes. Descriptive statistics and qualitative thematic analysis were used to analyse responses, disaggregating by low-income and middle-income countries (LMICs) and high-income countries (HICs).
Results
We analysed responses from 714 maternal and newborn health professionals. Only one-third received training on COVID-19 from their health facility and nearly all searched for information themselves. Half of respondents in LMICs received updated guidelines for care provision compared with 82% in HICs. Overall, 47% of participants in LMICs and 69% in HICs felt mostly or completely knowledgeable in how to care for COVID-19 maternity patients. Facility-level responses to COVID-19 (signage, screening, testing and isolation rooms) were more common in HICs than LMICs. Globally, 90% of respondents reported somewhat or substantially higher levels of stress. There was a widespread perception of reduced use of routine maternity care services, and of modification in care processes, some of which were not evidence-based practices.
Conclusions
Substantial knowledge gaps exist in guidance on management of maternity cases with or without COVID-19. Formal information-sharing channels for providers must be established and mental health support provided. Surveys of maternity care providers can help track the situation, capture innovations and support rapid development of effective responses.
Keywords: maternal health, child health, health systems, health services research, cross-sectional survey
Key questions.
What is already known?
In addition to lack of healthcare worker protection, staffing shortages, heightened risk of nosocomial transmission and decreased healthcare use described in previous infectious disease outbreaks, maternal and newborn care during the COVID-19 pandemic has also been affected by large-scale lockdowns/curfews.
The two studies assessing the indirect effects of COVID-19 on maternal and child health have used models to estimate mortality impacts.
Experiences of frontline health professionals providing maternal and newborn care during the COVID-19 pandemic have not been empirically documented to date.
Key questions.
What are the new findings?
Respondents in high-income countries more commonly reported available/updated guidelines, access to COVID-19 testing and dedicated isolation rooms for confirmed/suspected COVID-19 maternity patients.
Levels of stress increased among health professionals globally, including due to changed working hours, difficulties in reaching health facilities and staff shortages.
Healthcare providers are worried about the impact of rapidly changing care practices on health outcomes: reduced access to antenatal care, fewer outpatient visits, shorter length of stay in facilities after birth, banning birth companions, separating newborns from COVID-19 positive mothers and postponing routine immunisations.
What do the new findings imply?
COVID-19 illustrates the susceptibility of maternity care services to emergencies, including by reversing hard-won gains in healthcare utilisation and use of evidence-based practices.
Maternity care differs from other services, inasmuch as healthy women are being brought into health facilities that are operating suboptimally, and potentially increasing risk of infection, from COVID-19 and other healthcare-associated infections.
These rapid findings can inform countries of the main issues emerging and help develop effective responses, but similar efforts are needed to understand women’s experiences.
Introduction
Coronavirus disease (COVID-19) has affected 5.5 million cases as of 28 May 2020 and caused more than 350 000 deaths globally,1 with an estimated case fatality rate of 2.3%.2 This highly infectious disease is transmitted through close contact with infected persons or via contaminated surfaces. Vertical transmission (antenatally or intrapartum) remains a possible concern,3 4 and COVID-19 effects during the first and second trimesters of pregnancy are unclear. Breastfeeding continues to be encouraged with appropriate hygiene measures, including wearing face masks.5 6 The limited available evidence suggests that pregnant women do not face higher risks of infection and disease severity.7–9 A meta-analysis of 41 pregnant women with COVID-19 showed higher risk of preterm birth, pre-eclampsia and caesarean section.10 Symptoms among newborns seem to be mild,11 though one study reported a higher perinatal death risk.10 More data and larger sample sizes must be collected to draw definitive conclusions.12 It is prudent to protect pregnant women from COVID-19 through both individual-level and population-level measures, considering the increased risk of infection with other respiratory viruses such as influenza, and the increased mortality linked with H1N1.10 However, recommendations to avoid infection remain similar for pregnant women and the general public.13 Some countries, such as the UK, categorised pregnant women as a vulnerable group and issued stricter measures for them.7
The pandemic’s indirect effects will likely surpass the direct infection effects on women and newborns. Previous outbreaks severely reduced health systems’ capacity to provide essential maternal and newborn health (MNH) care, with negative impacts on health outcomes.14–16 Ebola virus disease (EVD), severe acute respiratory syndrome and Middle East respiratory syndrome (MERS) outbreaks highlighted challenges in countries’ preparedness to face outbreaks, amplified by weak existing systems. These include lack of protection of healthcare workers leading to disruptions in staffing, heightened risk of nosocomial transmission and elevated stress among service providers.17 18 Other indirect consequences of outbreaks include limited capacity for public health surveillance and lower use of healthcare.19–21 During the COVID-19 pandemic, large disruptions to healthcare provision and utilisation also stem from unprecedented large-scale measures implemented by countries (eg, lockdowns, curfews and transport restrictions). Indirect influences of previous outbreaks persisted long after their containment,22 but much of the evidence available about MNH is modelled or uses secondary data such as population-based surveys and routine health information systems that are originally collected for purposes other than studying the effect of the outbreak on MNH and fail to prospectively document these impacts over time.19 23 24
To date, studies assessing potential indirect effects of the COVID-19 pandemic on sexual, reproductive, maternal and child health in low-income and middle-income countries (LMICs) have used modelling approaches. Roberton and colleagues25 modelled three scenarios projecting a decrease in the coverage of basic life-saving interventions. They estimated an increase in maternal deaths between 12 190 and 56 700, and 253 500–1 157 000 additional deaths of children under 5 years. Similar conclusions were drawn by Riley et al,26 who projected that a modest decline in the use of sexual and reproductive healthcare services in 132 LMICs will result, over a year, in 48 million additional women with unmet need for modern contraceptives, 15 million additional unwanted pregnancies and over 3 million additional unsafe abortions. It is therefore critical that the precise nature of both direct and indirect impacts of COVID-19, and the adaptations and innovations tested to reduce its impact are prospectively captured and described.27
Health professionals’ views and experiences when providing care to women and newborns during this pandemic have not been empirically documented to date, and there is a necessity for prospectively assessing the effects of the COVID-19 pandemic on MNH services. The objective of this paper is to synthesise key themes identified in the first round of a global online survey of health professionals working in MNH along four dimensions: preparedness for COVID-19, response to COVID-19, personal experience in the workplace and changes in care provision and processes. This online survey is part of a larger study seeking to: (1) understand how health professionals and health facilities prepare and respond to COVID-19 in regard to the care provided to women and their babies; and (2) document and analyse the effect of the COVID-19 pandemic on the services available to pregnant, labouring and postpartum women and their newborns, including as a result of increasing pressures on the healthcare system.
Methods
Study design, population and sampling
This is a cross-sectional study of health professionals providing MNH care services. The target population was health professionals directly providing maternal (antenatal, intrapartum and/or postnatal) or newborn care, including midwives, nurses, obstetricians/gynaecologists, neonatologists, paediatricians, anaesthetists, general practitioners, medical officers, clinical officers, community health workers, lactation counsellors, paramedics, health technicians and health professionals in training. Due to the unavailability of a global sampling frame for this study population, sampling was non-random and not intended to generate generalisable nationally representative results of either health professionals or facilities. Rather, our intention was to collect and synthesise the voices and experiences of MNH professionals from various countries, contexts, services and facility types at the early stage of the COVID-19 pandemic. An invitation to complete the survey was distributed using personal networks of the multicountry research team members, maternal/newborn platforms and social media (eg, Facebook, Twitter and WhatsApp). Respondents were encouraged to share the survey with other colleagues in an attempt to snowball the sample population. Respondents provided informed consent online by checking a box affirming that they voluntarily agreed to participate in the survey.
Questionnaire
A questionnaire was developed in English by an international team of collaborators including health professionals, experts in health systems, infectious diseases, infection prevention and control, maternal health epidemiologists and public health researchers from various global settings. It was piloted by asking five MNH professionals from different settings to complete the questionnaire and provide feedback, which was used to assess face validity and refine the wording of questions and response options. The final version was translated into 11 languages that were made available consecutively (French and Arabic were available at launch; Italian, Portuguese, Spanish, Japanese, German and Dutch were available within 10 days; Chinese, Russian and Kiswahili were added after 3 weeks). We collected data on respondents’ background, preparedness for COVID-19, response to COVID-19 and own work experience during the pandemic. All respondents were invited to participate in an optional module that asked about adaptations to 17 care processes and respondents’ perceptions regarding changes in the uptake of care by women and newborns. The questionnaire is provided in online supplementary file 1.
bmjgh-2020-002967supp001.pdf (172.4KB, pdf)
Data processing and analysis
We use responses collected between 24 March and 10 April 2020. We cleaned 798 received responses by removing duplicate submissions (n=49), refusals to participate (n=14) and submissions made by those not directly providing maternal or newborn care (eg, lecturers and public health officials; n=10). Quantitative analysis involved descriptive statistics (frequencies and percentages) using Stata/SE V.14. Responses were stratified by country income levels according to World Bank classification.28 We conducted a qualitative thematic analysis of free-text answers to derive common themes of respondents’ experiences and changes in the work environment and care process by country income levels. When possible, we triangulated qualitative and quantitative results to validate emerging themes.
Missing data
From the 725 remaining responses, we dropped from the analysis 11 responses with missing answers on more than 90% of questions. The extent of missingness to close-ended questions ranged from 0.5% to 6.5% and that to open-ended questions from 16% to 28% of respondents. Missing answers to the ‘Country’ question were recoded based on the ‘Region’ answer for 93 responses; for example, a respondent with a missing response for country but region reported as Maharashtra was coded as from India.
Results
Respondents’ characteristics
The sample included 714 MNH care professionals, 59% of whom participated in the questionnaires’ optional module (n=397). Participants worked in 81 countries and 63% were from high-income countries (HICs; table 1). Online supplementary file 2 includes a map showing respondents’ geographic distribution and the total number of confirmed cases as of the midpoint of our data collection period (1 April 2020). Most were obstetricians/gynaecologists or midwives (38% and 35%, respectively), and around 60% worked in public sector facilities. Nearly half of respondents from HICs (49%) reported that their facilities had seen COVID-19 confirmed or suspected maternity patients, compared with 13% of respondents from LMICs.
Table 1.
Background characteristics of maternal and newborn healthcare providers who responded to the survey and optional module
| Survey n=714* (%) |
Optional module n=397* (%) |
|
| Country income level (World Bank classification) | ||
| Low-income and middle-income countries | 263 (37) | 136 (35) |
| High-income countries | 444 (63) | 256 (65) |
| Region | ||
| East Asia and Pacific | 82 (12) | 51 (13) |
| Europe and Central Asia | 249 (35) | 131 (33) |
| Latin America and Caribbean | 43 (6) | 30 (8) |
| Middle East and North Africa | 53 (7) | 29 (7) |
| North America | 87 (12) | 53 (14) |
| South Asia | 83 (12) | 37 (9) |
| Sub-Saharan Africa | 110 (16) | 61 (16) |
| Cadre | ||
| Midwife | 248 (35) | 135 (34) |
| Nurse-midwife | 83 (12) | 48 (12) |
| Nurse | 22 (3) | 14 (4) |
| Obstetrician/gynaecologist | 269 (38) | 148 (38) |
| Neonatologist | 6 (1) | 3 (1) |
| Paediatrician | 4 (1) | 4 (1) |
| General practitioner | 10 (1) | 5 (1) |
| Medical doctor (no specialisation) | 15 (2) | 10 (3) |
| Medical student/intern/resident | 13 (2) | 6 (2) |
| Community health worker/outreach worker | 12 (2) | 6 (2) |
| Other | 29 (4) | 16 (4) |
| Position | ||
| Head of facility | 60 (9) | 34 (9) |
| Head of department or ward | 71 (10) | 41 (11) |
| Head of team | 94 (13) | 54 (14) |
| Team member | 346 (50) | 195 (50) |
| Locum or interim member | 22 (3) | 10 (3) |
| Other† | 101 (15) | 53 (13) |
| Type of care provided (multiple responses allowed) | ||
| Outpatient ANC | 438 (61) | 244 (62) |
| Home-based childbirth care | 77 (11) | 47 (12) |
| Outpatient PNC | 316 (44) | 176 (45) |
| Outpatient breastfeeding support | 217 (30) | 121 (31) |
| Inpatient ANC | 374 (52) | 218 (56) |
| Inpatient childbirth care | 437 (61) | 249 (64) |
| Inpatient PNC | 350 (49) | 193 (50) |
| Surgical care | 213 (30) | 115 (29) |
| Neonatal care (small and sick newborns) | 85 (12) | 47 (12) |
| Home visits | 131 (18) | 78 (20) |
| Community outreach | 105 (15) | 69 (18) |
| Abortion care | 157 (22) | 86 (22) |
| Postabortion care | 179 (25) | 104 (27) |
| Other | 84 (12) | 42 (11) |
| Health facility level | ||
| Referral hospital | 250 (36) | 144 (37) |
| District/regional hospital | 154 (22) | 77 (20) |
| Health centre | 76 (11) | 46 (12) |
| Polyclinic | 6 (1) | 6 (2) |
| Clinic | 66 (10) | 36 (9) |
| Health post/unit or dispensary | 16 (2) | 9 (2) |
| Other‡ | 116 (17) | 68 (18) |
| Health facility sector | ||
| Public (national) | 183 (27) | 86 (22) |
| Public (university or teaching) | 138 (20) | 81 (21) |
| Public (district level or below) | 80 (12) | 61 (16) |
| Social security | 7 (1) | 3 (1) |
| Health insurance or HMO | 10 (2) | 7 (2) |
| Private university | 25 (4) | 10 (3) |
| Private for profit | 95 (14) | 57 (15) |
| Non-governmental | 61 (9) | 29 (8) |
| Faith-based or mission | 23 (3) | 15 (4) |
| Other | 56 (8) | 34 (9) |
| Type of area | ||
| Large city (more than 1 million inhabitants) | 273 (40) | 151 (39) |
| Small city (100 000 to 1 million inhabitants) | 220 (32) | 125 (32) |
| Town (fewer than 100 000 inhabitants) | 106 (16) | 61 (16) |
| Village/rural area | 64 (9) | 38 (10) |
| Refugee/displaced persons camp | 8 (1) | 2 (1) |
| Other | 9 (1) | 9 (2) |
| Facility characteristics | ||
| Caesarean section provision | 535 (81) | 301 (81) |
| Accept referrals from other facilities | 476 (71) | 269 (71) |
| ICU available | 429 (64) | 236 (62) |
| NICU available | 398 (59) | 226 (59) |
*Differential number of missing values across variables.
†Mainly self-practising midwives.
‡Mainly birth centres and private practice.
ANC, antenatal care; HMO, Health maintenance organisation; ICU, intensive care unit; NICU, neonatal intensive care unit; PNC, postnatal care.
bmjgh-2020-002967supp002.pdf (187.9KB, pdf)
Knowledge on providing MNH care and COVID-19
Most respondents (90%) received information on COVID-19, including on transmission, treatment, prevention, screening and updated policies, and only one-third attended trainings/drills on the response to COVID-19 (table 2). Several perceived that trainings would make them ‘feel better prepared’ to respond to women’s needs during the outbreak.
Table 2.
Preparedness for COVID-19 among maternal and newborn health professionals, by country income category
| LMIC n=263 (%) |
HIC n=444 (%) |
Total* n=714 (%) |
|
| Institution provided information on how to prepare for COVID-19 | 217 (86) | 403 (93) | 620 (90) |
| Institution provided training on COVID-19 | 94 (37) | 143 (34) | 237 (35) |
| Received updated guidelines for MNH care provision because of COVID-19 | 118 (47) | 347 (82) | 465 (69) |
| Personally searched for guidance and information to prepare for COVID-19 | 242 (95) | 387 (90) | 629 (92) |
| Received information related to COVID-19 informally through colleagues | 230 (91) | 386 (89) | 616 (90) |
| Facility published materials covering COVID-19 targeted towards pregnant, labouring or postnatal women | 98 (38) | 194 (46) | 292 (43) |
| Perception that patients’ questions were adequately answered at facility | 145 (57) | 267 (64) | 412 (61) |
| Level of knowing how to provide care for a woman with COVID-19 | |||
| Not at all clear | 16 (6) | 6 (1) | 22 (3) |
| Some points clear but not confident in what to do | 59 (24) | 43 (10) | 102 (15) |
| Somewhat clear but major issues remain | 56 (23) | 84 (20) | 140 (21) |
| Mostly clear but some areas of concern remain | 80 (32) | 203 (48) | 283 (42) |
| Very clear | 38 (15) | 90 (21) | 128 (19) |
*Differential number of missing values across variables.
HICs, high-income countries; LMICs, low-income and middle-income countries; MNH, maternal and newborn health.
Half of LMIC-based respondents received updated guidelines reflecting measures for the outbreak when providing MNH care, compared with 82% of those from HICs (table 2). This was a source of concern for some respondents from Tanzania, Rwanda, Uganda and India, as remarked by an obstetrician/gynaecologist from Uganda: ‘I am worried that no national guidelines [are] rolled out yet regarding care for pregnant women and newborns’. Some midwives in HICs requested clearer guidelines on home-based midwifery care. Nearly all respondents searched personally for information on COVID-19 (92%) and received informal guidance from colleagues (90%, table 2). Some LMIC-based participants worried about lack of access to/availability of evidence on COVID-19 effects during pregnancy and possible transmission to fetus and/or newborn. Only 19% of participants perceived that they were completely knowledgeable of providing care to COVID-19 maternity patients (table 2).
Personal experiences
Facilities adopted several measures in response to COVID-19. Most HIC-based respondents noted that their facilities set up a sign-posted entrance and screening area (75%) and reserved isolation rooms for COVID-19 suspected cases (83%), compared with 37% and 57% of LMIC-based respondents, respectively (table 3). Most facilities (62%) reportedly designated a COVID-19 liaison person/team. Screening for COVID-19 symptoms among maternity patients was more commonly reported by respondents from HICs (76%). For example, antenatal care (ANC) outpatients and inpatients were screened either in person or over the phone before appointments/admission. The ability to test maternity patients for COVID-19 was limited in LMICs (23%), rural areas (9% in LMICs; 28% in HICs) and completely unavailable in refugee and/or displaced persons camps (n=6, data not shown).
Table 3.
Response to COVID-19 among maternal and newborn health professionals and their workplaces, by country income category
| LMIC n=263 (%) |
HIC n=444 (%) |
Total* n=714 (%) |
|
| Sign-posted area for screening of COVID-19 suspected cases in facility | |||
| No | 38 (15) | 32 (8) | 70 (11) |
| Some measures taken | 106 (42) | 65 (16) | 171 (26) |
| Yes | 95 (37) | 298 (72) | 393 (59) |
| Reserved isolation rooms for suspected cases | 143 (57) | 341 (83) | 484 (73) |
| Screening for COVID-19 symptoms among maternity patients | 117 (47) | 320 (76) | 437 (75) |
| Possible to order a test for COVID-19 for maternity patients | 58 (23) | 258 (61) | 316 (47) |
| Sufficient PPE items | |||
| Gloves | 174 (70) | 399 (92) | 578 (84) |
| Masks | 117 (47) | 224 (52) | 345 (50) |
| Aprons | 88 (36) | 260 (61) | 352 (52) |
| All three types | 79 (32) | 188 (44) | 267 (40) |
| Respondents’ work affected by COVID-19 | 177 (71) | 372 (86) | 549 (81) |
| Respondents’ stress levels | |||
| Same as usual | 21 (8) | 47 (11) | 68 (10) |
| Somewhat higher than usual | 136 (54) | 215 (50) | 351 (52) |
| Substantially higher than usual | 93 (37) | 167 (39) | 260 (38) |
*Differential number of missing values by variables.
HICs, high-income countries; LMICs, low-income and middle-income countries; PPE, personal protective equipment.
Healthcare workers reported various concerns regarding care provision during the outbreak. Respondents perceived the lack of COVID-19 symptom screening and testing as threats to staff and patient safety. A midwife from Canada wrote, ‘I'm worried about being infected by someone who is asymptomatic, and then being a vector to others’. Personal protective equipment (PPE) deficiencies also compromised patients’ and healthcare providers’ safety across all settings but more prominently in LMICs (table 3). A midwife from the UK pleaded, ‘let midwives who are in close contact with women wear masks. Please let us use masks for all’. Respondents advocated for clear and unified protocols regarding PPE use. A nurse-midwife from the USA wrote, ‘we are not allowed to wear masks and goggles unless delivering a patient, we’re told to « take the mask off or go home », that we’re scaring the patients’. Despite the need to feel protected, respondents described wearing additional PPE as time-consuming and worried about delays in providing emergency care because of donning and doffing PPE. There were additional concerns that PPE disrupts clear communication with patients; a midwife from Denmark remarked that ‘[i]t can be hard to connect with people through masks and [goggles], facial expressions are harder to read’.
Most respondents noted that COVID-19 affected their work (81%) and that their stress levels were higher than usual (90%, table 3). An obstetrician from Mozambique described, ‘My stress level is immeasurable. Every time a pregnant woman with flu-like symptoms [visits the health facility], I feel almost completely lost. I need to be equally protected and I don't feel any protection from whoever [is responsible of protecting me]’. Challenges included shortage of qualified staff, either because of symptoms, self-isolation after potential exposure, or inability to reach their workplace, as a midwife in Uganda described: ‘[t]ransport to work is a big challenge due to lockdown; many staff live far away from the hospital. Staff who manage to come to work hurry to leave early to observe the curfew time of 7.00 p.m.’. This shortage led to an increase in workload and frequent changes in schedules. Certain healthcare facilities increasingly relied on locum workers and students to fill staffing shortages. Some respondents requested more support from management as exhaustion increased. A department head in Uganda reported, ‘[t]here are no more clear work schedules as I get to attend many unscheduled/emergency meetings. Staff are very anxious and panicky and need talking to all the time, which is exhausting’. Some participants from LMICs such as India, Bangladesh, Bolivia and Syria expressed concerns regarding ‘patients and relatives not following instructions given by staff members’, such as social/physical distancing and hygiene. A nurse from Syria attributed this to a ‘lack of awareness and knowledge, and indifference among beneficiaries’.
Changes to care provided to women and newborns
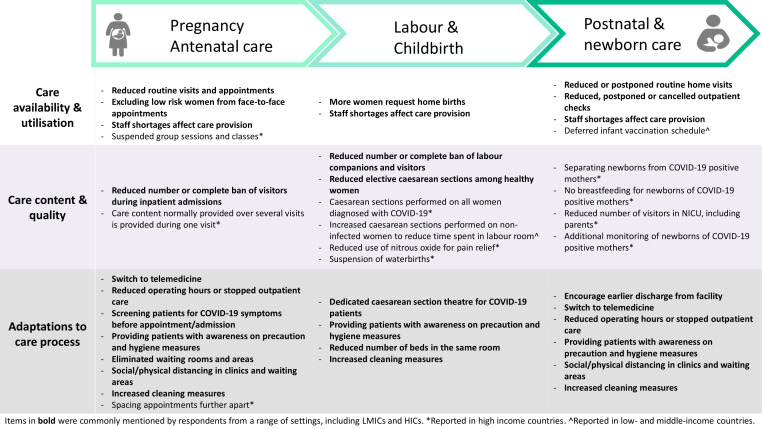
Figure 1 displays major reported changes in service provision and utilisation, care content and quality, and care processes across the continuum of care. In all settings and across the continuum of care, participants saw fewer patients at facilities, due to transportation restrictions or fear of nosocomial transmission. A nurse-midwife from Kenya wrote, ‘[a]ccessing inpatient antenatal care [is] minimal. Women fear [getting] infected with COVID-19 if [they are] in hospitals. Most of them keep off from hospital even when they are sick’. Most respondents noted shorter visiting hours and fewer allowed visitors, while others reported screening visitors for symptoms or banning visits altogether. The number of labour companions was limited to one person (also allowed to accompany the mother after birth), or none at all. An obstetrician from the Czech Republic remarked that: ‘[the] Gynaecological and Obstetrical Society recommended to ban partners and doulas from accompanying a woman at birth - outrageous!!!’.
Figure 1.
Reported changes to service provision across the continuum of maternal and newborn care. HICs, high-income countries; LMICs, low-income and middle-income countries; NICU, neonatal intensive care unit.
Among the reported changes, some facilities implemented social/physical distancing in waiting areas and in hospital rooms by reducing the number of beds. However, this was difficult to achieve in small facilities; an obstetrician/gynaecologist from India noted: ‘[It is] not practically possible [to place each patient in a separate birthing room] in our set up’. Non-essential services including elective gynaecological procedures and infertility treatments were postponed or cancelled. Several facilities restricted routine ANC to the management of high-risk patients. A respondent from New York reported a ‘significant decrease in number of ANC visits’, whereby new policies recommended reducing face-to-face visits during pregnancy ‘from 10 to 12 [visits], to four [visits]’. Other changes include eliminating waiting areas, spacing appointments to reduce contact between patients and cancelling group activities such as health education sessions.
The pandemic entailed adaptations to care process and content, subsequently affecting quality. ANC and postnatal care (PNC) provision and breastfeeding counselling shifted to telemedicine. Participants in LMICs acknowledged that women’s inadequate access to communication infrastructure prevents equitable healthcare provision. Respondents were concerned over uncertain impacts of reduced contacts on the quality of care. A midwife from the UK wrote: ‘[w]hilst I completely see the need to restrict face-to-face care to protect staff and patients, my heart just breaks for women and families who we won't be able to offer the full range of midwifery support to… that is, breastfeeding support, daily visits, and just generally our time’. Across all settings, the demand for home births increased and new practices aimed to reduce labour inductions. In certain HICs, induction of labour was discouraged before 41 weeks of gestation, using nitrous oxide for pain relief diminished to reduce risk of transmission through aerosols, and waterbirths were suspended. Caesarean sections were commonly performed among women diagnosed with COVID-19 and some facilities dedicated theatres specifically for this purpose. Elective caesarean sections decreased among ‘healthy’ maternity patients. However, some facilities aimed to reduce labour duration and time spent in the labour room by augmentation. Respondents speculated about a potential rise in caesarean section rates in their facilities, as noted by an obstetrician/gynaecologist from India: ‘We will not allow as much time in second stage [of labour], this is likely to push up our caesarean rate’.
Respondents frequently mentioned shortened length of stay in facilities after childbirth; for example, a reduction ‘to 6–8 from 24 or more [hours]’ (midwife from Canada). A midwife from the UK wrote, ‘[the] lack of time and staff will lead to mothers and babies going home with very little feeding support or knowledge which will have a short and long term impact on their health and ability to deal with infections’. Routine postnatal checks were postponed or substituted with telemedicine in some cases as reported by a nurse-midwife from the USA, ‘[w]e are postponing the routine postpartum visit until 12 weeks postpartum, and are prescribing most contraceptives over the phone and breastfeeding support is all done virtually’. Changes to newborn PNC were infrequent and included monitoring and isolating babies of mothers with COVID-19. Three respondents from India noted that vaccination schedules were disrupted or postponed. MNH professionals feared that changes in standards of care would lead to poor health outcomes among women and newborns and subsequently to the loss of achieved progress. ‘I am worried about the implications of policies that call for separating newborns from COVID-19 positive mothers immediately after birth, without allowing for skin-to-skin or delayed cord clamping’, wrote a nurse-midwife from the USA.
Discussion
This paper uses a rapid collection of data from health professionals providing care to women and newborns globally during initial stages of the COVID-19 pandemic. We describe preparedness for COVID-19, response to COVID-19, personal experience in the workplace and changes in care provision and processes.
Preparedness
Healthcare providers commonly resort to personal searches and informal networks to fulfil information needs.29 Accessing unreliable information related to COVID-19 is likely, particularly on social media.30 31 Facility-specific creation and distribution of guidelines for managing maternity patients is somewhat lagging behind despite frequent updates by Ministries of Health and professional associations.32–38 Information sharing channels must be established to secure providers’ timely access to accurate information.39–41 Midwives supporting pregnant and labouring women during the pandemic,42 43 particularly independent practitioners, need clear guidelines for providing home-based care.44
Response
Sharp discrepancies in facility-level responses to COVID-19 between HICs and LMICs could stem from the differential progression of the outbreak (online supplementary file 2) or be partly attributed to limited health system capacities and resources in some countries.45 An attenuated outbreak is speculated in Africa, yet it is equally possible that trends similar to those witnessed in Europe will occur.46 47 This indicates an urgent need to mobilise resources, improve testing capacities and upgrade responses, with the needs and complexities of MNH care provision in mind. Absence of testing in refugee and/or displaced persons camps raises concerns. Overcrowding and inadequate water and sanitation in underserved settlements are barriers to basic infection prevention measures.47–50 Displaced women’s and newborns’ access to MNH services is suboptimal, and they experienced poor outcomes before the pandemic-induced disruptions of essential care.51–54 Efforts should ensure that displaced populations are protected, with adequate access to testing, treatment and quality MNH care to halt anticipated exacerbations of negative health outcomes.26 49
Personal experiences
MNH care workers during the pandemic experience increased stress and anxiety, consistently with experiences from previous outbreaks.18 41 Stress levels in LMICs were comparable with those in HICs, although countries were battling different outbreak stages (online supplementary file 2). This might be due to uniformly reported shortages in skilled workforce leading to higher workloads and staff burnout.45 55 Wilson et al41 suggest measures to prevent burnout among maternity care providers along prioritising adequate emotional, social and mental health support, including from managers.18 56 As our findings show, this adds burdens to management staff, a group that deserves special focus during this outbreak.41 Reliance on students increases their vulnerability to stressors considering their lack of experience, and senior colleagues should actively advocate for their well-being.41 Future research should explore the availability and effectiveness of mental and social support to MNH care providers during the pandemic.57
Insufficient PPE intensifies the fear of nosocomial transmission. In some facilities, PPE supplies are prioritised for departments treating COVID-19 cases and do not reach maternity wards. MNH care workers and patients could experience uneven risks of nosocomial infection during outbreaks.58 59 In some countries, obstetricians/gynaecologists commonly work in multiple facilities, and their risk of exposure might be exacerbated by the higher number of contacts they experience in this dual practice.60 Although PPE are essential, their rational use is recommended by the WHO given universal shortage.61 These guidelines must be clearly communicated to MNH care providers and patients.41 Health workers caring for women around the time of birth might be used to wearing some PPE; yet, it can make them feel dehumanised, and the donning and doffing of PPE might delay emergency service provision.18 62
Changes in care provision and processes
Care practices are rapidly changing and their consequences on health outcomes are uncertain. Our findings support narratives told by healthcare providers,63 and align with disruptions witnessed during previous outbreaks,55 64–66 which have increased maternal and neonatal mortality.19 67 Currently, there are signs of similar trends in two maternity hospitals in Uganda.68 Our knowledge of the impact of these changes is restricted to predictions resulting from modelling, which strongly suggest a threat to achieved improvements in LMICs.25 26 The actual impact is yet to be quantified,25 and the effect in HICs remains unclear. Prioritising measures depending on contextual needs can mitigate the pandemic’s indirect consequences.25 27
Previous outbreaks of infectious diseases such as EVD in West Africa and MERS in South Korea have imposed barriers to healthcare access and utilisation, including fear of nosocomial transmission, healthcare facilities’ closure and loss of trust in the healthcare workforce.55 66 69 Our findings show that in the case of COVID-19, fear of disease spread was perceived to reduce healthcare use, and unprecedented societal measures such as lockdowns, curfews and transport restrictions emerge as new challenges to healthcare provision and utilisation.
Although some changes to care content and process matched updated guidelines37 70 71 other modifications diverge from available evidence. These include eliminating birth companions,72 73 banning visitors, performing caesarean section on all COVID-19 positive women,73 74 augmenting labour or performing unindicated caesarean sections to control timing of deliveries, separating newborns from COVID-19 positive mothers, not allowing breast feeding75 and reducing length of stay with fewer home-based follow-ups.44 Such practices deny women’s access to quality care and jeopardise their well-being and that of their babies.76 Unlike curative services, maternity care provides holistic support to women going through a normal physiological process; both overintervention and underintervention can result in a massive preventable burden. Additionally, and although only reported in India in our survey, alarming disruptions or delays in routine immunisation are also implemented in other LMICs.77 During EVD outbreak, vaccination activities were similarly disrupted for safety purposes, leading to substantial declines in immunisation coverage.55 Catch-up campaigns should be prioritised following the relaxation of preventive measures.77 78 Introducing new models of care such as telehealth guidance26 70 was described as a ‘virtually perfect solution’ to continuing care provision.79 However, this model is not compatible with all healthcare services and providers dread its impact on care quality.44
Patient and community resistance to outbreak control measures and mutual incomprehension between patients and providers could shape the impact of COVID-19 on MNH care. Health-seeking behaviours rely on provider–patient relationships and common cultural, economic and social understanding of health and hygiene.80–83 Hierarchical issues may affect MNH care quality as shown in West African urban areas and Malagasy hospitals.80 81 84 Understanding social and cultural responses to epidemics is essential to mitigate disasters85 and avoid a top-down management of outbreak guidelines that may miss the mark of pre-existing factors.86
Limitations
The lack of representativeness and related sample bias are limitations of this sampling approach. Our sample might over-represent higher qualified cadres of health professionals in settings with limited use of technology among lower cadres of staff, and under-represent overstretched staff, or those with limited or no access to internet connection, as we received few responses from professionals working in lower level facilities, particularly in LMICs. Some cadres were less represented (eg, neonatologists and paediatricians). The sample’s representativeness is affected by the availability of the survey in three languages (English, French and Arabic) for a longer time than the remaining nine languages. The questionnaire asks about facilities where respondents work, which is not relevant to independently practising professionals, especially midwives; this might have discouraged some of them from completing the survey. Finally, data were collected across countries going through different stages of the outbreak; in some countries, responding to such surveys is discouraged or forbidden by authorities (eg, China).
Conclusion
This is the first study describing the preparedness for, response to, and effect of the COVID-19 pandemic on MNH care provision. The multicountry survey creates an innovative platform for lessons to be documented and shared. Our findings, ideally combined with an understanding of women’s perspectives, hold enormous potential for establishing a timely, evidence-based decision-making platform. Continued collection, rapid synthesis and timely dissemination of health workers’ voices to planners, programmers and policymakers is crucial to guide the development and implementation of contextually relevant guidance.
The COVID-19 pandemic illustrates a susceptibility to emergencies, which is not restricted to healthcare systems in LMICs. This crisis is challenging health systems and providers and disrupting access to basic services worldwide. Health system preparedness might have been equally inadequate in LMICs and HICs in some aspects, such as shortage in skilled staff, training provision and PPE sufficiency. However, it is likely that HICs were able to respond more effectively due to better health system resilience such as existing coordination systems to develop and implement changes to protocols.87 Findings from this study will be useful in supporting the development of effective responses to main identified issues, during various stages of the COVID-19 pandemic and more broadly during future health system shocks.
Acknowledgments
We would like to thank the study participants who took time to respond to this survey despite the difficult circumstances and increased workload. We acknowledge the Institutional Review Committee at the Institute of Tropical Medicine for providing helpful suggestions on this study protocol and for the expedited review of this study. We would like to thank all study collaborators and colleagues who distributed the invitation for this survey and provided suggestions on the questionnaire, including the coauthors of this paper, Dr Susannah Woodd and Dr Jean-Paul Dossou. We are immensely grateful to all those who volunteered to translate the survey, including Dr Francesca L Cavallaro, Dr Bouchra Assarag, Dr Karima Khalil, Dr Jose Penalvo, Dr Sonia Menon, Dr Claudia Nieto Sanchez, Virginia Castellano Pleguezelo, Dr Werner Soors, Verónica Blanco Gutiérrez, Dr Raffaella Ravinetto, Dr Manuela Straneo, Francesca Palestra, Dr Stacy Saha, Dr Shirajum Munira, Dr Mitsuaki Matsui, Wnurinham Silva, Dr Leonardo Chavane, Dr Enny S. Paixao, Min Dai, Dr Li Na, Dr Marc Snel, Dr Anna Larionova, Dr Vladimir Gordeev, Dr Christiane Schwarz, Evelyn Lesta, Elibariki Mkumbo, Dr Amani Kikula, Dr Elly Mertens and Hilde Cortier.
Footnotes
Handling editor: Seye Abimbola
Twitter: @abankethomas, @profwendygraham, @lenkabenova
Contributors: LB conceptualised the study and obtained funding. All authors contributed to the design of the study and development of the survey tool. AS analysed the data. CA, LB, EH and AS wrote the original draft of the manuscript. All authors contributed to the development of the manuscript and read and approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. AS is the guarantor.
Funding: This study was funded by the Institute of Tropical Medicine’s COVID-19 Pump Priming fund supported by the Flemish Government, Science & Innovation. LB is funded in part by the Research Foundation – Flanders (FWO) as part of her Senior Postdoctoral Fellowship.
Disclaimer: The funder had no role in the study design, data collection, analysis and interpretation of data or in writing the manuscript. Researchers are independent from funders, and all authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data, and the accuracy of the data analysis is also required.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the Institutional Review Committee at the Institute of Tropical Medicine (Antwerp, Belgium) on 20 March 2020 (approval reference 1372/20).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Anonymised data analysed in the current study will be made available from the corresponding author on reasonable request.
References
- 1.World Health Organization Coronavirus disease (COVID-19) situation Report-129, 2020. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200528-covid-19-sitrep-129.pdf?sfvrsn=5b154880_2 [Accessed 29 May 2020].
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 2020. [Epub ahead of print: 24 Feb 2020]. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 3.Zeng H, Xu C, Fan J, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA 2020. 10.1001/jama.2020.4861. [Epub ahead of print: 26 Mar 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amoroux A, Attie-Bitach T, Martinovic J. Evidence for and against vertical transmission for SARS-CoV-2 (COVID-19). Am J Obstet Gynecol. 10.1016/j.ajog.2020.04.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization FAQ breastfeeding and COVID-19. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-on-covid-19-and-breastfeeding
- 6.Salvatori G, De Rose DU, Concato C, et al. Managing COVID-19-Positive Maternal–Infant dyads: an Italian experience. Breastfeed Med 2020;15:347–8. 10.1089/bfm.2020.0095 [DOI] [PubMed] [Google Scholar]
- 7.Royal College of Obstetricians & Gynaecologists Coronavirus (COVID-19) infection in pregnancy; 2020. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/covid-19-virus-infection-and-pregnancy/
- 8.Breslin N, Baptiste C, Gyamfi-Bannerman C, et al. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM 2020;100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu N, Li W, Kang Q, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis 2020;20:559–64. 10.1016/S1473-3099(20)30176-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Mascio D, Khalil A, Saccone G, et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: a systematic review and meta-analysis. Am J Obstet Gynecol MFM 2020;100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeng L, Xia S, Yuan W, et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr 2020;23:2–4. 10.1001/jamapediatrics.2020.0878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buekens P, Alger J, Bréart G, et al. A call for action for COVID-19 surveillance and research during pregnancy. Lancet Glob Health 2020:S2214-109X 10.1016/S2214-109X(20)30206-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization Q&A on COVID-19, pregnancy and childbirth, 2020. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-on-covid-19-pregnancy-and-childbirth
- 14.Leno NN, Delamou A, Koita Y, et al. Ebola virus disease outbreak in guinea: what effects on prevention of mother-to-child transmission of HIV services? Reprod Health 2018;15:60. 10.1186/s12978-018-0502-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organisation Operational guidance for maintaining essential health services during an outbreak, 2020. Available: https://apps.who.int/iris/bitstream/handle/10665/331561/WHO-2019-nCoV-essential_health_services-2020.1-eng.pdf?sequence=1&isAllowed=y
- 16.Delamou A, Ayadi AME, Sidibe S, et al. Effect of Ebola virus disease on maternal and child health services in Guinea: a retrospective observational cohort study. Lancet Glob Health 2017;5:e448–57. 10.1016/S2214-109X(17)30078-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cipriano PF. 100 years on: the Spanish flu, pandemics and keeping nurses safe. Int Nurs Rev 2018;65:305–6. 10.1111/inr.12483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McMahon SA, Ho LS, Brown H, et al. Healthcare providers on the frontlines: a qualitative investigation of the social and emotional impact of delivering health services during Sierra Leone's Ebola epidemic. Health Policy Plan 2016;31:1232–9. 10.1093/heapol/czw055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sochas L, Channon AA, Nam S. Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy Plan 2017;32:iii32–9. 10.1093/heapol/czx108 [DOI] [PubMed] [Google Scholar]
- 20.Nuzzo JB, Meyer D, Snyder M, et al. What makes health systems resilient against infectious disease outbreaks and natural hazards? results from a scoping review. BMC Public Health 2019;19:1–9. 10.1186/s12889-019-7707-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oppenheim B, Gallivan M, Madhav NK, et al. Assessing global preparedness for the next pandemic: development and application of an epidemic preparedness index. BMJ Glob Health 2019;4:1–9. 10.1136/bmjgh-2018-001157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Camara BS, Delamou A, Diro E, et al. Effect of the 2014/2015 Ebola outbreak on reproductive health services in a rural district of Guinea: an ecological study. Trans R Soc Trop Med Hyg 2017;111:22–9. 10.1093/trstmh/trx009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bietsch K, Williamson J, Reeves M. Family planning during and after the West African Ebola crisis. Stud Fam Plann 2020;51:71–86. 10.1111/sifp.12110 [DOI] [PubMed] [Google Scholar]
- 24.Stein D, Ward K, Cantelmo C. Estimating the potential impact of COVID-19 on mothers and newborns in low- and middle-income countries. Heal Policy Plus 2020. [Google Scholar]
- 25.Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health 2020;0. 10.1016/S2214-109X(20)30229-1. [Epub ahead of print: 12 May 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Riley T, Sully E, Ahmed Z, et al. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low- and middle-income countries. Int Perspect Sex Reprod Health 2020;46:73–6. 10.1363/46e9020 [DOI] [PubMed] [Google Scholar]
- 27.Graham WJ, Afolabi B, Benova L, et al. Protecting hard-won gains for mothers and newborns in low-income and middle-income countries in the face of COVID-19: call for a service safety net. BMJ Glob Health 2020;5:e002754 10.1136/bmjgh-2020-002754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The World Bank World bank country and lending groups, 2020. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- 29.Liverman CT, Ingalls CE, Fulco CE, et al. Understanding the information needs of health professionals : Toxicology and environmental health information resources: the role of the National library of medicine. US: National Academies Press, 1997. [PubMed] [Google Scholar]
- 30.Li HO-Y, Bailey A, Huynh D, et al. Youtube as a source of information on COVID-19: a pandemic of misinformation? BMJ Glob Health 2020;5:e002604. 10.1136/bmjgh-2020-002604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cinelli M, Quattrociocchi W, Galeazzi A, et al. The COVID-19 social media Infodemic. Available: http://arxiv.org/abs/2003.05004 [Accessed 6 May 2020]. [DOI] [PMC free article] [PubMed]
- 32.Ministry of Health - Kenya A Kenya practical guide for continuity of reproductive, maternal, newborn and family planning care and services in the background of COVID-19 pandemic, 2020. Available: https://www.health.go.ke/wp-content/uploads/2020/04/KENYA-COVID19-RMNH.pdf.pdf.pdf
- 33.The National Health Service Clinical guide for the temporary reorganisation of intrapartum maternity care during the coronavirus pandemic, 2020. Available: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0241-specialty-guide-intrapartum-maternity-care-9-april-2020.pdf
- 34.Chawla D, Chirla D, Dalwai S, et al. Perinatal-Neonatal Management of COVID-19 Infection - Guidelines of the Federation of Obstetric and Gynecological Societies of India (FOGSI), National Neonatology Forum of India (NNF), and Indian Academy of Pediatrics (IAP). Indian Pediatr 2020. [Epub ahead of print: 01 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Federal Ministry of Health - Nigeria, Nigeria Centre for Disease Control COVID-19 Guidelines for Pregnant Women and Nursing Mothers - Nigeria, 2020. Available: https://reliefweb.int/report/nigeria/covid-19-guidelines-pregnant-women-and-nursing-mothers [Accessed 6 May 2020].
- 36.New York State Department of Health Health Advisory: COVID-19 guidance for hospital operators regarding visitation updated guidance regarding obstetrical and pediatric settings, 2020. Available: https://opwdd.ny.gov/system/files/documents/2020/04/doh_covid19_hospitalvisitation_4.10.20.pdf
- 37.Royal College of Obstetricians & Gynaecologists, The Royal College of Midwives Guidance for provision of midwife-led settings and home birth in the evolving coronavirus (COVID-19) pandemic, 2020. Available: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-04-09-guidance-for-provision-of-midwife-led-settings-and-home-birth-in-the-evolving-coronavirus-covid-19-pandemic.pdf
- 38.Royal College of Obstetricians & Gynaecologists Guidance for deployment of obstetrics and gynaecology staff during the COVID-19 pandemic, 2020. Available: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-05-01-guidance-for-deployment-of-obstetrics-and-gynaecology-staff-during-the-covid-19-pandemic.pdf
- 39.World Health Organization Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health, 2020. Available: https://www.who.int/publications-detail/coronavirus-disease-(covid-19)-outbreak-rights-roles-and-responsibilities-of-health-workers-including-key-considerations-for-occupational-safety-and-health
- 40.Tran NT, Tappis H, Spilotros N, et al. Not a luxury: a call to maintain sexual and reproductive health in humanitarian and fragile settings during the COVID-19 pandemic. Lancet Glob Heal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilson AN, Ravaldi C, Scoullar MJL, et al. Caring for the carers: ensuring the provision of quality maternity care during a global pandemic. Women Birth 2020. 10.1016/j.wombi.2020.03.011. [Epub ahead of print: 08 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brussels U. Midwives step up to support pregnant women during pandemic, 2020. Available: https://www.un.org/en/pregnant-women-are-worried-about-giving-birth-during-pandemic
- 43.Ossola A. The challenges of supporting pregnant women during Covid-19, from a midwife, 2020. Available: https://qz.com/1847930/covid-19-is-transforming-the-role-of-midwives-during-childbirth/
- 44.Audet C. Giving birth amid a pandemic in Belgium: the challenges faced by mothers and midwives. BMJ Glob Heal blog 2020. [Google Scholar]
- 45.Hussein J. COVID-19: what implications for sexual and reproductive health and rights globally? Sex Reprod Health Matters 2020;28:1746065. 10.1080/26410397.2020.1746065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Martinez-Alvarez M, Jarde A, Usuf E, et al. COVID-19 pandemic in West Africa. Lancet Glob Health 2020;8:e631–2. 10.1016/S2214-109X(20)30123-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hopman J, Allegranzi B, Mehtar S. Managing COVID-19 in low- and middle-income countries. JAMA 2020. 10.1001/jama.2020.4169. [Epub ahead of print: 16 Mar 2020]. [DOI] [PubMed] [Google Scholar]
- 48.Gharibah M, Mehchy Z. COVID-19 pandemic: Syria’s response and healthcare capacity; 2020.
- 49.Lau LS, Samari G, Moresky RT, et al. COVID-19 in humanitarian settings and lessons learned from past epidemics. Nat Med 2020;26:647–8. 10.1038/s41591-020-0851-2 [DOI] [PubMed] [Google Scholar]
- 50.Vince G. The world's largest refugee camp prepares for COVID-19. BMJ 2020;368:m1205. 10.1136/bmj.m1205 [DOI] [PubMed] [Google Scholar]
- 51.DeJong J, Ghattas H, Bashour H, et al. Reproductive, maternal, neonatal and child health in conflict: a case study on Syria using countdown indicators. BMJ Glob Health 2017;2:e000302. 10.1136/bmjgh-2017-000302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Islam MM, Nuzhath T. Health risks of Rohingya refugee population in Bangladesh: a call for global attention. J Glob Health 2018;8 10.7189/jogh.08.020309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hynes M, Sakani O, Spiegel P, et al. A study of refugee maternal mortality in 10 countries, 2008-2010. Int Perspect Sex Reprod Health 2012;38:205–13. 10.1363/3820512 [DOI] [PubMed] [Google Scholar]
- 54.Gibson-Helm M, Boyle J, Cheng I-H, et al. Maternal health and pregnancy outcomes among women of refugee background from Asian countries. Int J Gynaecol Obstet 2015;129:146–51. 10.1016/j.ijgo.2014.10.036 [DOI] [PubMed] [Google Scholar]
- 55.Elston JWT, Moosa AJ, Moses F, et al. Impact of the Ebola outbreak on health systems and population health in Sierra Leone. J Public Health 10.1093/pubmed/fdv158 [DOI] [PubMed] [Google Scholar]
- 56.World Health Organization Mental health and psychosocial considerations during the COVID-19 outbreak. Available: https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2 [Accessed 4 May 2020].
- 57.Kisely S, Warren N, McMahon L, et al. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 2020;369:m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Strong AE. Causes and effects of occupational risk for healthcare workers on the maternity ward of a Tanzanian Hospital. Hum Organ 2018;77:273–86. 10.17730/0018-7259.77.3.273 [DOI] [Google Scholar]
- 59.Dunn AC, Walker TA, Redd J, et al. Nosocomial transmission of Ebola virus disease on pediatric and maternity wards: Bombali and Tonkolili, Sierra Leone, 2014. Am J Infect Control 2016;44:269–72. 10.1016/j.ajic.2015.09.016 [DOI] [PubMed] [Google Scholar]
- 60.Moghri J, Rashidian A, Arab M, et al. Implications of dual practice among health workers: a systematic review. Iran J Public Health 2017;46:153–64. [PMC free article] [PubMed] [Google Scholar]
- 61.World Health Organization Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19), 2020. Available: https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf
- 62.Liu Q, Yang J, Liu Q, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Heal 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Penn-Kekana L. COVID-19 and MNCH: beyond the models, what are we hearing from countries? 2020. Available: https://www.harpnet.org/blog/covid-19-and-mch-beyond-the-models-what-are-we-hearing-from-countries/
- 64.Elston JWT, Cartwright C, Ndumbi P, et al. The health impact of the 2014-15 Ebola outbreak. Public Health 2017;143:60–70. 10.1016/j.puhe.2016.10.020 [DOI] [PubMed] [Google Scholar]
- 65.Brolin Ribacke KJ, Saulnier DD, Eriksson A, et al. Effects of the West Africa Ebola virus disease on health-care utilization – a systematic review. Front Public Health 2016;4:222 10.3389/fpubh.2016.00222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McQuilkin PA, Udhayashankar K, Niescierenko M, et al. Health-Care access during the Ebola virus epidemic in Liberia. Am J Trop Med Hyg 2017;97:931–6. 10.4269/ajtmh.16-0702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jones SA, Gopalakrishnan S, Ameh CA, et al. ‘Women and babies are dying but not of Ebola’: the effect of the Ebola virus epidemic on the availability, uptake and outcomes of maternal and newborn health services in Sierra Leone. BMJ Glob Heal 2016;1:e000065 10.1136/bmjgh-2016-000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wanduru P, Tetui M, Waiswa P. COVID-19 response in Uganda: notes and reflections. BMJ Glob Heal blogs 2020. [Google Scholar]
- 69.Lee H, Park JH. Changes in health care utilization during the MERS epidemic. Int J Infect Dis 2018;73:187 10.1016/j.ijid.2018.04.3838 [DOI] [Google Scholar]
- 70.UNFPA COVID-19 technical brief for maternity services, 2020. Available: https://www.unfpa.org/resources/covid-19-technical-brief-maternity-services
- 71.International Confederation of Midwives Women’s Rights in Childbirth Must be Upheld During the Coronavirus Pandemic, 2020. Available: https://www.internationalmidwives.org/icm-news/women%E2%80%99s-rights-in-childbirth-must-be-upheld-during-the-coronavirus-pandemic.html
- 72.Bobrow E. A chaotic week for pregnant women in New York City, 2020. Available: https://www.newyorker.com/science/medical-dispatch/a-chaotic-week-for-pregnant-women-in-new-york-city
- 73.Lowe NK. Reflections on COVID-19. J Obstet Gynecol Neonatal Nurs 2020;49:223–4. 10.1016/j.jogn.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ferrazzi E, Frigerio L, Savasi V, et al. Vaginal delivery in SARS-CoV-2-infected pregnant women in northern Italy: a retrospective analysis. BJOG 2020. 10.1111/1471-0528.16278. [Epub ahead of print: 27 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Petit G, Huet N. Coronavirus: baby blues as some mothers in France separated from newborn amid COVID-19 fears, 2020. Available: https://www.euronews.com/2020/03/31/coronavirus-baby-blues-as-some-mothers-in-france-separated-from-newborn-amid-covid-19-fear [Accessed 6 May 2020].
- 76.Campbell OMR, Calvert C, Testa A, et al. The scale, scope, coverage, and capability of childbirth care. Lancet 2016;388:2193–208. 10.1016/S0140-6736(16)31528-8 [DOI] [PubMed] [Google Scholar]
- 77.Nelson R. COVID-19 disrupts vaccine delivery. Lancet Infect Dis 2020;20:546. 10.1016/S1473-3099(20)30304-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.World Health Organization Guiding principles for immunization activities during the COVID-19 pandemic, 2020. Available: https://apps.who.int/iris/handle/10665/331590
- 79.Hollander JE, Carr BG. Virtually perfect? telemedicine for Covid-19. N Engl J Med 2020;382:1679–81. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 80.Jaffré Y, Olivier de Sardan J-P. Les difficiles relations entere soignants et soigne dans cinq capitales d’Afrique de l’Ouest. Bull Amades 2003:1–466. [Google Scholar]
- 81.Pourette D. Femmes, enfants et santé Madagascar – Approches anthropologiques comparées. Paris: Éditions L’Harmattan, 2018. [Google Scholar]
- 82.Nganga SW, Otieno NA, Adero M, et al. Patient and provider perspectives on how trust influences maternal vaccine acceptance among pregnant women in Kenya. BMC Health Serv Res 2019;19:1–13. 10.1186/s12913-019-4537-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gilson L. Trust in health care: theoretical perspectives and research needs. J Health Organ Manag 2006;20:359–75. 10.1108/14777260610701768 [DOI] [PubMed] [Google Scholar]
- 84.Mestre C. Maladies et violences ordinaires dans un hôpital malgache, 2014. [Google Scholar]
- 85.Fairhead J. Understanding social resistance to the Ebola response in the forest region of the Republic of guinea: an anthropological perspective. Afr Stud Rev 2016;59:7–31. 10.1017/asr.2016.87 [DOI] [Google Scholar]
- 86.Ronse M. Biology and culture are inseparable – considerations for the “exit strategy” expert group from the field of medical anthropology, 2020. Available: https://07323a85-0336-4ddc-87e4-29e3b506f20c.filesusr.com/ugd/3cbdf6_f9ef1e533ce54fd4844a76a805aa084e.pdf
- 87.Kruk ME, Myers M, Varpilah ST, et al. What is a resilient health system? lessons from Ebola. The Lancet 2015;385:1910–2. 10.1016/S0140-6736(15)60755-3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-002967supp001.pdf (172.4KB, pdf)
bmjgh-2020-002967supp002.pdf (187.9KB, pdf)