Abstract
Objective
Knowledge on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in liver transplant recipients is lacking, particularly in terms of severity of the disease. The aim of this study was to describe the demographic, baseline clinical characteristics and early outcomes of a European cohort of liver transplant recipients with SARS-CoV-2 infection.
Design
We conducted an international prospective study across Europe on liver transplant recipients with SARS-CoV-2 infection confirmed by microbiological assay during the first outbreak of COVID-19 pandemic. Baseline characteristics, clinical presentation, management of immunosuppressive therapy and outcomes were collected.
Results
57 patients were included (70% male, median (IQR) age at diagnosis 65 (57–70) years). 21 (37%), 32 (56%) and 21 (37%) patients had one cardiovascular disease, arterial hypertension and diabetes mellitus, respectively. The most common symptoms were fever (79%), cough (55%), dyspnoea (46%), fatigue or myalgia (56%) and GI symptoms (33%). Immunosuppression was reduced in 22 recipients (37%) and discontinued in 4 (7%). With this regard, no impact on outcome was observed. Forty-one (72%) subjects were hospitalised and 11 (19%) developed acute respiratory distress syndrome. Overall, we estimated a case fatality rate of 12% (95% CI 5% to 24%), which increased to 17% (95% CI 7% to 32%) among hospitalised patients. Five out of the seven patients who died had a history of cancer.
Conclusion
In this European multicentre prospective study of liver transplant recipients, COVID-19 was associated with an overall and in-hospital fatality rate of 12% (95% CI 5% to 24%) and 17% (95% CI 7% to 32%), respectively. A history of cancer was more frequent in patients with poorer outcome.
Keywords: orthotopic liver transplantation, chronic liver disease, infectious disease
Significance of this study.
What is already known on this subject?
Recipients of liver transplantation can be infected with SARS-CoV-2.
The outcome of COVID-19 of these immunosuppressed patients is not well known.
What are the new findings?
In our European cohort of liver transplant patients, overall and in-hospital fatality rates were 12% (95% CI 5% to 24%) and 17% (95% CI 7% to 32%), respectively. All deaths occurred in hospitalised patients.
Immunosuppressants were not discontinued in the vast majority of liver transplant recipients with COVID-19 infection.
How might it impact on clinical practice in the foreseeable future?
Patients infected in the first year after transplantation are presenting with less symptoms.
A history of cancer was more frequent in liver transplant recipient with poorer outcome, suggesting that higher attention should be paid in these patients.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a virus belonging to the Orthocoronavirinae subfamily, first identified in Wuhan, Hubei Province, China, in December 2019.1 Infection with SARS-CoV-2 is responsible for a clinical condition, named COVID-19, which ranges from mild respiratory and/or GI symptoms to interstitial pneumonia with acute respiratory distress syndrome (ARDS), diffuse thrombotic and thromboembolic disease,2 multiorgan failure (MOF) and even death with a case fatality rate ranging from 5.65%3 to 15%,4 5 with high geographical heterogeneity. The outbreak of SARS-CoV-2 infection, declared pandemic on 11 March 2020 by the WHO,6 has rapidly become a public health matter with several unmet issues. To date, firm knowledge on disease evolution, risk factors, clinical manifestations and optimal management are lacking, particularly in specific categories of patients. In the setting of solid organ transplantation, and particularly liver transplant recipients, information on natural history of COVID-19 are limited to expert statements,7 8 case reports9 and small case series.10 11 Concerns have been raised about immunosuppression therapy, and it is still unknown whether the latter actually represents an increased risk for more severe illness, including higher risk of bacterial coinfection,12 13 or not. In this view, previous experience with similar viruses, such as SARS-CoV in 200314 and MERS-CoV in 2015,15 suggests that solid organ recipients would be prone to have increased morbidity.16 However, in these cases, sample size and data quality did not allow definitive conclusion. Moreover, recent evidence has shown SARS-CoV-2 associated liver injury,17–19 which might per se impair the prognosis of liver transplant patients with COVID-19. Overall, liver transplant patients are a population with multiple potential risk factors for poorer outcome that need to be investigated in detail.
This study describes the demographics, baseline clinical characteristics and early outcomes of a European cohort of liver transplant recipients with SARS-CoV-2 confirmed infection during the first outbreak of COVID-19 pandemic.
Methods
Study design
We conducted a European multicentre prospective cohort study recruiting consecutive liver transplant recipients from 19 secondary and tertiary (with more than 100 patients in regular follow-up) liver transplant centres across Europe. The coordinating centre was the Inselspital, University Hospital of Berne (KEK Approval Project ID 2020-00682). Written informed consent was obtained from all the included patients. The recruitment was conducted from 10 March to 10 May 2020.
Study population
Consecutive adult (aged >18 years at the time of SARS-CoV-2 infection) liver transplant recipients with concomitant confirmed SARS-CoV-2 infection were included in the study. The definition of confirmed SARS-CoV-2 infection was made according to the WHO guidelines and based on the presence of a laboratory assay proving SARS-CoV-2 infection, irrespective of clinical signs and symptoms of the disease.20 Nucleic acid amplification test (NAAT) positive for SARS-CoV-2 in nasopharyngeal swab, sputum samples and bronchoalveolar lavage (BAL) was considered diagnostic. Typical radiological findings included bilateral, peripheral, consolidation and/or ground glass opacities, detected by using chest X-ray or thorax-CT scan.21
Patients were enrolled in the study at the time of diagnosis of COVID-19 and were followed up until death or 10 May 2020.
Baseline information regarding indication to liver transplantation, underlying liver disease and comorbidities, as well as anthropometric data were collected. At the time of COVID-19 diagnosis, clinical features and laboratory parameters were recorded. All laboratory and imaging investigations were performed as part of standard care of patients. Information on management of baseline immunosuppression, namely, its reduction or discontinuation, as well as specific pharmacological therapies and ventilation support, were obtained.
Patients were classified according to the severity of COVID-19 disease in outpatient care and hospitalisation, respectively.13 Time from liver transplantation was classified as very long term (more than 10 years from liver transplant)10 and very short term (1 year or less from liver transplant), whereas the terms long and short term were adopted if the patients had been transplanted for more or less than 5 years, respectively.22 Management of single immunosuppression therapy was classified as follows: no change, reduction or discontinuation. For patients on double immunosuppression, reduction was defined as reduction of at least one immunosuppressive drug and/or discontinuation of one medication, while discontinuation was defined as discontinuation of both drugs.
The main outcome was patient death, while secondary outcomes were ARDS diagnosis23 and hospitalisation. All the data were entered in an electronic dataset using a standardised case report form.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting or dissemination plans of our research.
Statistical analysis
Descriptive analysis of quantitative variables normally distributed were expressed as mean (number and %) and SD, whereas not-normally distributed variables were shown as median and IQR. Comparison of quantitative variables between two groups was performed using the t-test or non-parametric tests, according to the normality of the distribution. Comparison of proportions was performed using the Fisher’s exact test. Missed data were not imputed, and all the analysis was performed only on non-missing data. P value less than 0.05 was considered statistically significant. SPSS software (V.25; IBM) was used for statistical analysis.
Results
Demographics and general characteristics of study population
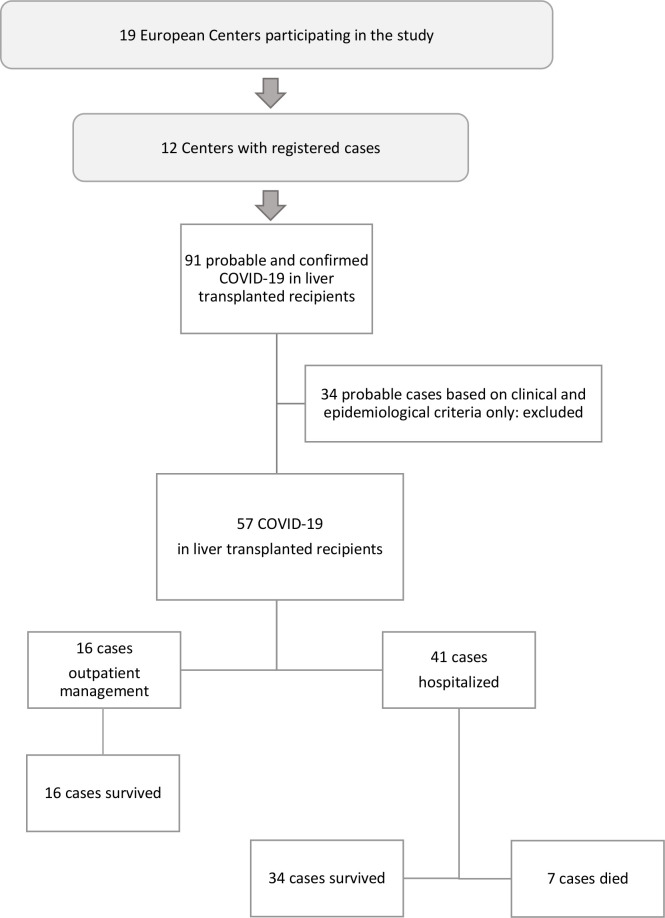
Among 19 centres from seven European countries involved in the study, 12 registered at least one case. Of the 11 790 liver transplant recipient in regular follow-up overall, 91 patients were reported, of whom 57 were classified as confirmed cases and considered for statistical analysis (figure 1). Overall, 40 recipients (70%) were male and median age (IQR) at diagnosis was 65 (57–70) years. Mean body mass index (BMI, kg/m2) was 26.0±4.6, with 23 (43%) and 8 (14%) patients being overweight and obese, respectively. Eleven (19%) and 21 (37%) subjects were defined as very short-term and very long-term transplant recipients, respectively. Additionally, median time (IQR) from transplant to COVID-19 diagnosis was 6 (2–13) years, and 32 (56%) patients had been transplanted more than 5 years before COVID-19 diagnosis. Characteristics related to indication for liver transplantation and underlying liver disease are summarised in table 1. With regard to comorbidities, 21 (37%) and 10 (18%) patients had one and more than one cardiovascular (CV) disease, respectively. In terms of CV risk factors, 32 (56%) recipients had arterial hypertension, and 21 (37%) diabetes mellitus, while 7 (12%) were active or former smokers. Sixteen (28%) patients had chronic kidney disease. Furthermore, 24 (42%) subjects had a clinical history of neoplasia (20 with hepatocellular carcinoma (HCC)), which was active in 5 (9%) patients. Concomitant respiratory diseases were found in 13 (23%) patients. Only one patient was HIV positive. Concerning pharmacological therapy for CV prevention, 13 (23%) recipients were on ACE inhibitors or sartans, while 9 (16%) were on low-dose aspirin.
Figure 1.
Flowchart of the study design.
Table 1.
Demographic characteristics of liver transplant recipient with SARS-CoV-2 infection
| Study population | Results |
| Patients, n | 57 |
| Sex, male, n (%) | 40 (70) |
| Ethnicity, Caucasian, n (%) | 53 (93) |
| Age, years, median (IQR) | 65 (57–70) |
| Age ≥65, n (%) | 29 (51) |
| Age <65, n (%) | 28 (49) |
| BMI, kg/m2, mean (SD) | 26.0±4.6 |
| BMI, classes, n (%) | |
| 18–24.9 | 23 (43) |
| 25–29.9 | 23 (43) |
| >30 | 8 (14) |
| Time from transplant to diagnosis, years, median (IQR) | 6 (2–13) |
| Very long-term transplant recipients, n (%) | 21 (37) |
| Very short-term transplant recipients, n (%) | 11 (19) |
| Long-term transplant recipients, n (%) | 32 (56) |
| Indication to LT, n (%) | |
| End-stage liver disease | 38 (68) |
| Liver tumour | 16 (29) |
| Acute liver failure | 4 (7) |
| Other | 9 (16) |
| Underlying liver disease, n (%) | |
| ALD | 15 (26) |
| Viral | 24 (42) |
| HCV | 11 (19) |
| HBV | 13 (23) |
| PSC | 3 (5) |
| PBC | 4 (7) |
| NAFLD/NASH | 2 (4) |
| Autoimmune | 1 (2) |
| Hemochromatosis | 1 (2) |
| Wilson’s disease | 1 (2) |
| Other | 10 (18) |
| HCC, yes, n (%) | 20 (35) |
| Comorbidities, n (%) | |
| Cardiovascular disease | 21 (37) |
| Coronary artery disease | 7 (12) |
| Heart failure | 9 (16) |
| Atrial fibrillation | 6 (11) |
| Stroke | 1 (2) |
| Other | 8 (14) |
| >1 cardiovascular disease | 10 (18) |
| Arterial hypertension | 32 (56) |
| Diabetes mellitus | 21 (37) |
| Active cancer | 5 (9) |
| Kidney insufficiency | 16 (28) |
| Respiratory disease | 13 (23) |
| COPD | 7 (12) |
| HIV | 1 (2) |
| Smoke history, yes, n (%) | 7 (12) |
| Symptoms at presentation, n (%) | |
| Fever | 44 (79) |
| Cough | 31 (55) |
| Dyspnoea | 26 (46) |
| Fatigue and myalgia | 32 (56) |
| GI symptoms | 18 (33) |
| Diarrhoea | 16 (28) |
| Abdominal pain | 1 (2) |
| Vomiting | 1 (2) |
| Anosmia or dysgeusia | 4 (7) |
| Other | 8 (14) |
| Concomitant bacterial infection, n (%) | 9 (16) |
| Suspected | 3 (6) |
| Confirmed | 6 (11) |
ALD, alcoholic liver disease; BMI, body mass index; COPD, chronic obstructive pulmonary disease; HCC, hepatocellular carcinoma; LT, liver transplantation; NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis; PBC, primary biliary cholangitis; PSC, primary sclerosing cholangitis.
When we considered very-long term recipients in terms of comorbidities, CV disease (57% vs 25%, respectively; p=0.023) and arterial hypertension (76% vs 44%; p=0.028) were significantly more frequent.
Presentation of COVID-19 in liver transplant patients
At the time of diagnosis, the most commonly self-reported symptoms were fever (44 patients, 79%), cough (31 patients, 55%), dyspnoea (26 patients, 46%), fatigue or myalgia (32 patients, 56%), anosmia or dysgeusia (4 patients, 7%), as well as GI symptoms (18 patients, 33%). Patients who experienced the latter often had more than one GI symptom, diarrhoea being the most frequently reported (16 patients). Other unspecific symptoms included loss of appetite (four patients), headache (one patients) and sore throat (one patient), while confusion and delirium were reported in two hospitalised patients.
When long-term and short-term recipients were compared in terms of symptoms at presentation, fever (91% vs 63%, respectively; p=0.019) and dyspnoea (59% vs 29%; p=0.032) were significantly more frequent among long-term recipients.
When very short-term recipients were considered, fever (50% vs 85%, respectively; p=0.045) and cough (27% vs 62%, p=0.048) were significantly less prevalent (table 2).
Table 2.
Differential distribution of symptoms between long-term and short-term liver transplant patients
| Symptoms, n (%) |
Overall | Long-term transplant recipient | P value | Very-short term transplant recipient | P value | ||
| No | Yes | Yes | No | ||||
| Sex, male | 40 (70) | 19 (48) | 21 (53) | 0.561 | 10 (25%) | 30 (75%) | 0.146 |
| Age, years, median (IQR) | 65 (57–70) | 59 (53–65) | 68 (61–76) | <0.001 | 55 (52–70) | 65 (59–72) | 0.058 |
| BMI, kg/m2, mean (SD) | 26.0±4.6 | 26.1±4.6 | 25.7±5.1 | 0.563 | 26.8±5.7 | 25.3±3.6 | 0.043 |
| Fever | 44 (79) | 15 (63) | 29 (91) | 0.005 | 6 (55) | 38 (84) | 0.045 |
| Cough | 31 (55) | 11 (46) | 20 (63) | 0.280 | 3 (27) | 28 (62) | 0.048 |
| Dyspnoea | 26 (46) | 7 (29) | 19 (59) | 0.032 | 3 (27) | 23 (51) | 0.192 |
| Fatigue | 32 (56) | 11 (44) | 21 (66) | 0.117 | 4 (36) | 28 (61) | 0.184 |
| Conjunctivitis | 0 | – | – | – | – | – | – |
| Anosmia/dysgeusia | 4 (7) | 0 | 4 (13) | 0.131 | 0 | 4 (9) | 0.573 |
| GI | 18 (33) | 6 (25) | 12 (38) | 0.394 | 1 (9) | 17 (38) | 0.084 |
| Other | 8 (14) | 3 (13) | 5 (16) | 1.000 | 1 (9) | 7 (16) | 1.000 |
In the entire population, the diagnosis of SARS-CoV-2 infection was confirmed by NAAT positivity in nasopharyngeal swab, while one additional patients received BAL. Concerning radiological findings, CT scan and pulmonary radiography showed typical features of the disease in 24 (43%) and 23 (40%) cases, respectively.
The main laboratory findings are summarised in table 3. Four patients (8%) displayed relevant increase in liver enzymes (AST and/or ALT>2 × ULN). Conversely, median (IQR) leucocytes, lymphocytes and thrombocytes were 4.5 (3.3–6.0)×1000/µL, 0.79 (0.40–1.10)×1000/µL and 160 (91–268)×1000/μL, respectively.
Table 3.
Initial laboratory data of liver transplant recipient with SARS-CoV-2 infection
| Patients tested, n (%) | Results | Patients with value, n | |
| Deviation from reference (%) | |||
| Blood counts, median (IQR) | |||
| Leucocytes (×1000/μL) | 51 (90) | 4.50 (3.33–6.00) | 17 (33)* |
| Platelets (×1000/μL) | 49 (86) | 160 (91–268) | 17 (35)* |
| Lymphocytes (×1000/μL) | 49 (86) | 0.79 (0.40–1.10) | 37 (76)* |
| Biochemical and liver-related test, median (IQR) | |||
| AST (U/L) | 49 (86) | 38 (25–53) | 13 (26)† |
| ALT (U/L) | 49 (86) | 30 (20–42) | 10 (20)† |
| GGT (U/L) | 45 (79) | 66 (39–161) | 29 (64)† |
| ALP (U/L) | 37 (65) | 97 (74–171) | 9 (24)† |
| Total bilirubin (mg/dL) | 43 (75) | 0.70 (0.48–1.09) | 10 (23)† |
| INR (ratio) | 42 (74) | 1.10 (1.03–1.28) | 14 (33)† |
| Albumin (g/L) | 19 (33) | 32 (29.5–36.5) | 8 (42)* |
| Creatinine (mg/dL) | 50 (88) | 1.16 (0.93–1.55) | 20 (40)† |
| Glucose (mg/dL) | 36 (63.2) | 127.5 (92.5–163.0) | 24 (67)† |
| Inflammatory-related markers, median (IQR) | |||
| D-Dimer (ng/mL) | 17 (29.8) | 871 (380–1739) | 10 (59)† |
| LDH (U/L) | 31 (54.4) | 273 (192–384) | 20 (65)† |
| IL-6 (pg/L) | 9 (15.8) | 93 (59–288) | – |
| Ferritin (ng/mL) | 13 (22.8) | 567 (171–1194) | 9 (69)† |
*Below reference.
†Above reference.
ALP, alanine alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; GGT, gamma-glutamyltransferase; IL-6, interleukin-6; INR, international normalised ratio; LDH, lactate dehydrogenase.
Concomitant bacterial infection was described in nine patients (16%). Three (6%) of them were defined suspected, since no confirmatory positive cultures were available, although clinical and laboratory findings were suggestive (symptomatic urinary infection, cholangitis and pulmonary coinfection) and six (11%) cases were defined as confirmed (positive blood culture). Gram-positive concomitant infection was found in three patients, while one patient resulted to be infected by Gram-negative strains and two subjects by both Gram-positive and Gram-negative strains. The most common Gram-negative strains belonged to Enterobacteriaceae (two Escherichia coli, one Enterobacter cloacae), whereas between Gram-positive strains enterococci were the most reported.
Management of immunosuppression therapy and COVID-19 therapy
Baseline immunosuppression therapy and its management are described in table 4. Overall, reduction was observed in 22 (39%) patients, and complete discontinuation was reported in 4 cases (7%). Considering individual therapies, antimetabolites were the most frequently discontinued drugs (18%), whereas calcineurin inhibitors (CNIs) were the most frequently reduced ones (16%).
Table 4.
Baseline immunosuppression characteristics and modification during the infection
| Baseline immunosuppression therapy | Overall, n (%) | No modification, n (%) | Reduction, n (%) | Discontinuation, n (%) |
| Single agent | ||||
| CNIs | 16 (28) | 12 (75) | 2 (12.5) | 2 (12.5) |
| Cyclosporine | 3 (5) | 2 (67) | 0 | 1 (33) |
| Tacrolimus | 13 (29) | 10 (77) | 2 (15) | 1 (8) |
| mTORi | 2 (4) | 1 (50) | 0 | 1 (50) |
| Everolimus | 1 (2) | 1 (100) | 0 | 0 |
| Sirolimus | 1 (2) | 0 | 0 | 1 (100) |
| MMF | 2 (3) | 0 | 0 | 1 (100) |
| Steroid | 1 (2) | 1 (100) | 0 | 0 |
| Two or more agents | ||||
| CNIs+MMF | 21 (37) | 7 (33) | 6 (29) | 8 (38) |
| CNIs | – | – | 5 | 1 |
| MMF | – | – | 1 | 7 |
| CNIs+mTORi | 3 (5) | 1 (33.3) | 1 (33.3) | 1 (33.3) |
| CNIs | – | – | 1 | 0 |
| mTORi | – | – | 0 | 1 |
| CNIs+steroids | 9 (16) | 1 (11.2) | 4 (44.4) | 4 (44.4) |
| CNIs | – | – | 4 | 4 |
| Steroids | – | – | 0 | 0 |
| CNIs+AZA | 1 (2) | 1 (100) | 0 | 0 |
| mTORi +MMF | 2 (3) | 1 (50) | 0 | 1 (50) |
| mTOR | – | – | 0 | 1 |
| MMF | – | – | 0 | 0 |
AZA, azathioprine; CNIs, calcineurin inihibitors, including cyclosporine and tacrolimus; MMF, mycophenolate mofetil; mTORi, mammalian target of rapamycin inhibitor, including sirolimus and everolimus.
Concerning specific therapy for COVID-19, 19 (35%) patients received steroids, 22 (44%) hydroxychloroquine and 5 (9%) antivirals, including lopinavir/ritonavir (3 patients), darunavir/cobicistat and remdesivir. Only one patient was treated with tocilizumab, while two more patients were on immunomodulatory therapies because of concomitant comorbities (one on rituximab for active lymphoma and the other one on ruxolitinib for a graft vs host disease). Overall, 35 (63%) and 16 (29%) subjects received at least one and more than one antibiotic drug, respectively. Of those, 15 (27%) were treated with azithromycin as part of the standard care of COVID-19 therapy in some centres.24
As for respiratory support, oxygen therapy was required in more than half of the patients (30, 54%). Of those, the majority required only oxygen therapy through nasal cannula (18 patients, 32%), whereas 8 (14%) subjects received high-flow oxygen. Four (7%) patients required intubation and invasive mechanical ventilation (table 5).
Table 5.
Therapeutic strategies for COVID-19 and outcomes
| Study population | Results |
| Patients, n | 57 |
| Medications, n (%) | |
| Steroids (for COVID-19) | 19 (35) |
| Antibiotics | 35 (63) |
| Azitromycin | 15 (27) |
| >1 antibiotic | 16 (29) |
| Antivirals | 5 (9) |
| Lopinavir/ritonavir | 3 (5) |
| Darunavir/cobicistat | 1 (2) |
| Remdesivir | 1 (2) |
| Immunomodulator | 3 (5) |
| Tocilizumab | 1 (2) |
| Rituximab | 1 (2) |
| Ruxolitinib | 1 (2) |
| Hydroxychloroquine | 24 (44) |
| Oxygen therapy (higher intensity), n (%) | |
| Overall | 30 (54) |
| Nasal cannula | 18 (32) |
| Non-invasive ventilation | 8 (14) |
| Invasive mechanical ventilation | 4 (7) |
| Outcomes, n (%) | |
| Death | 7 (12) |
| ARDS | 11 (19) |
| ICU admission | 4 (7) |
| Hospitalisation (no ICU) | 37 (65) |
| Need for rehabilitation | 7 (17) |
| Duration of hospitalisation, median (IQR) | |
| Hospital stay | 10 (7–22) |
| ICU stay | 16 (10–19) |
| Rehab stay | 14 (11–15) |
ARDS, acute respiratory distress syndrome; ICU, intensive care unit.
Clinical outcome in liver transplant patients with COVID-19
Overall, 16 (28%, 95% CI 17% to 42%) patients received outpatient care for COVID-19, while 41 (72%, 95% CI 59% to 83%) subjects were hospitalised, with a median (IQR) hospital stay duration of 10 days (7–22). Among hospitalised recipients, 4 (10%, 95% CI 3% to 23%) were admitted to the ICU and required invasive mechanical ventilation, while 11 (19%, 95% CI 10% to 32%) developed ARDS. Death was registered in seven cases (12%, median time from transplant to death was 6 years, IQR 3–13), all of whom were hospitalised with ARDS. Overall, case fatality rate was 12% (95% CI 5% to 24%) in our population, which increased to 17% (95% CI 7% to 32%) among hospitalised patients. General characteristics of patients who did not survive, of those with ARDS and of those who were hospitalised are summarised in tables 6 and 7. Five out of the seven patients who died had a history of cancer, of whom three had an active cancer at moment of the diagnosis of COVID-19. Moreover, 9 out of 11 patients with ARDS had a clinical history for cancer. Median (IQR) lymphocyte and platelet counts (×1000/μL) were significantly lower (0.49 (0.30–0.60) vs 0.80 (0.52–1.18), p=0.030; 93 (79-110) vs 170 (104–273), p=0.044, respectively) in the group of patients who did not survive.
Table 6.
Characteristics of liver transplant recipients died because of COVID-19
| Case | Sex (M/F) | Age, years | Ethnicity | BMI, kg/m2 | Comorbidity | Symptoms at presentation | Immunosuppression management | Respiratory support | ICU admission |
| 1 | M | 67 | Caucasian | 27.8 | History of renal tumour | Fever, cough, dyspnoea | CNIs alone | NIMV | No |
| No change | |||||||||
| 2 | M | 78 | Caucasian | 23.1 | History of PTLD | Fever, cough, dyspnoea | CNIs alone | NIMV | No |
| CV disease | No change | ||||||||
| Diabetes | |||||||||
| CKD | |||||||||
| 3 | M | 75 | Caucasian | 25.1 | Active tumour: HCC recurrence | Dyspnoea, | CNIs alone | NIMV | No |
| CV disease | Fatigue/myalgia | No change | |||||||
| Arterial hypertension | |||||||||
| 4 | M | 55 | Caucasian | 21.6 | – | Fever, dyspnoea | CNIs+steroids | NIMV | No |
| Only CNIs discontinuation | |||||||||
| 5 | M | 70 | Caucasian | 28.5 | Active tumour: HCC recurrence | Fever, dyspnoea | CNIs+steroids | IMV | Yes |
| Arterial hypertension | Only CNIs discontinuation | ||||||||
| 6 | M | 66 | Caucasian | 23.8 | Active tumour: PTLD | Fever, cough, fatigue/myalgia, GI symptoms | Steroids | IMV | Yes |
| Arterial hypertension | No change | ||||||||
| 7 | F | 79 | Caucasian | 21.3 | CV disease | Fever, dyspnoea, fatigue/myalgia | MMF alone | NC | No |
| Diabetes | |||||||||
| Arterial hypertension | |||||||||
| CKD |
CKD, chronic kidney disease; CNIs, calcineurin inhibitors; CV, cardiovascular; F, female; IMV, invasive mechanical ventilation; M, male; MMF, mycophenolate mofetil; NC, nasal cannula; NIMV, non-invasive mechanical ventilation; PTLD, post-transplant lymphoproliferative disorder.
Table 7.
General characteristics of patients who did not survive, of those with ARDS and of those who were hospitalised
| Outcome | Overall | Death (n=7) | P value | ARDS (n=11) | P value | Hospitalisation (n=41) | P value | |||
| Yes | No | Yes | No | Yes | No | |||||
| Sex, male | 40 (70) | 6 (86) | 34 (68) | 0.662 | 10 (91) | 30 (65) | 0.146 | 29 (71) | 11 (69) | 0.883 |
| Age, years, median (IQR) | 65 (57–70) | 70 (67–77) | 62 (57–70) | 0.088 | 68 (63–73) | 62 (55–70) | 0.052 | 65 (57–71) | 60 (54–68) | 0.162 |
| BMI, kg/m2, mean (SD) | 26.0 (21.4–30.6) | 24.5 (21.7–27.3) | 26.3 (21.4–31.2) | 0.185 | 25.5 (21.6–28.2) | 26.2 (21.3–31.1) | 0.625 | 25.5 (29.7–21.4) | 27.4 (21.6–33.2) | 0.258 |
| HCC as indication to LT | 20 (35) | 5 (71) | 15 (30) | 0.084 | 8 (73) | 12 (26) | 0.011 | 15 (37) | 5 (31) | 0.703 |
| Very long-term LT | 21 (37) | 3 (43) | 18 (36) | 0.701 | 4 (36) | 17 (37) | 1.000 | 16 (39) | 5 (31) | 0.582 |
| Very short-term LT | 11 (19) | 2 (29) | 9 (18) | 0.610 | 3 (27) | 8 (17) | 0.429 | 9 (22) | 2 (13) | 0.710 |
| Smoke history | 7 (14) | 1 (17) | 6 (14) | 1.000 | 1 (10) | 7 (15) | 1.000 | 5 (14) | 2 (14) | 1.000 |
| Cardiovascular disease | 21 (37) | 3 (43) | 18 (36) | 0.700 | 5 (46) | 16 (35) | 0.511 | 14 (34) | 7 (44) | 0.502 |
| Arterial hypertension | 32 (56) | 4 (57) | 28 (56) | 1.000 | 6 (55) | 27 (57) | 1.000 | 22 (54) | 10 (63) | 0.544 |
| Diabetes mellitus | 21 (37) | 2 (29) | 19 (38) | 1.000 | 4 (36) | 17 (36) | 1.000 | 14 (34) | 7 (44) | 0.502 |
| History of cancer | 24 (42) | 5 (71) | 19 (38) | 0.119 | 9 (82) | 15 (33) | 0.005 | 18 (44) | 6 (38) | 0.659 |
| Active cancer | 5 (9) | 3 (43) | 2 (4) | 0.011 | 4 (36) | 1 (2) | 0.004 | 5 (12) | 0 (0) | 0.308 |
| Dyspnoea at presentation | 26 (46) | 6 (86) | 20 (41) | 0.041 | 9 (82) | 17 (39) | 0.016 | 22 (54) | 4 (27) | 0.129 |
| Leucocytes, ×1000/μL, median (IQR) | 4.51 (3.33–6.00) | 2.95 (1.77–4.51) | 4.70 (3.65–6.00) | 0.113 | 3.70 (1.93–5.52) | 4.70 (3.65–6.00) | 0.297 | 4.61 (3.39–6.85) | 3.85 (3.27–5.13) | 0.170 |
| Platelets, ×1000/μL, median (IQR) | 160 (91–268) | 93 (79–110) | 170 (104–273) | 0.044 | 102 (88–134) | 183 (104–280) | 0.064 | 164 (91–270) | 149 (96–202) | 0.745 |
| Lymphocytes, ×1000/μL, median (IQR) | 0.79 (0.40–1.10) | 0.49 (0.30–0.60) | 0.80 (0.52–1.18) | 0.030 | 0.49 (0.40–0.76) | 0.81 (0.58–1.18) | 0.064 | 0.73 (0.45–1.00) | 1.02 (0.74–1.22) | 0.126 |
| AST, U/L, median (IQR) | 38 (25–53) | 48 (36–80) | 35 (24–52) | 0.134 | 38 (27–57) | 38 (23–53) | 0.358 | 45 (27–57) | 21 (17–29) | <0.001 |
| ALT, U/L, median (IQR) | 30 (20–42) | 21 (16–74) | 31 (21–42) | 0.602 | 22 (16–30) | 32 (22–44) | 0.142 | 33 (23–57) | 21 (18–30) | 0.026 |
| Overall immunosuppression reduction | 22 (39) | 2 (29) | 20 (40) | 0.695 | 4 (36) | 18 (39) | 1.000 | 18 (44) | 4 (25) | 0.236 |
| Overall immunosuppression discontinuation | 4 (7) | 1 (14) | 3 (6) | 0.417 | 1 (9) | 3 (7) | 1.000 | 4 (10) | 0 (0) | 0.568 |
| ACE inhibitors or sartans | 13 (24) | 3 (50) | 10 (20) | 0.136 | 3 (30) | 10 (22) | 0.685 | 10 (25) | 3 (20) | 1.000 |
| Oxygen therapy | 30 (54) | 7 (100) | 23 (47) | 0.012 | 11 (100) | 19 (42) | <0.001 | 29 (71) | 1 (7) | <0.001 |
| Steroids (for COVID-19) | 19 (35) | 4 (67) | 15 (31) | 0.167 | 6 (60) | 13 (29) | 0.077 | 18 (45) | 1 (7) | 0.010 |
| Antibiotics | 35 (63) | 7 (100) | 28 (57) | 0.038 | 10 (91) | 25 (57) | 0.039 | 30 (73) | 5 (33) | 0.012 |
| >1 antibiotic | 16 (29) | 4 (67) | 12 (24) | 0.049 | 6 (60) | 10 (22) | 0.024 | 15 (38) | 1 (6) | 0.023 |
| Antiviral | 5 (9) | 1 (14) | 4 (8) | 0.501 | 1 (9) | 4 (9) | 1.000 | 5 (12) | 0 (0) | 0.309 |
| Hydroxychloroquine | 24 (44) | 3 (50) | 21 (43) | 1.000 | 5 (50) | 19 (42) | 0.655 | 22 (55) | 2 (13) | 0.006 |
ALT, alanine aminotransferase; ARDS, acute respiratory distress syndrome; AST, aspartate aminotransferase; BMI, body mass index; HCC, hepatocellular carcinoma; LT, liver transplantation; MMF, mycophenolate mofetil,.
Discussion
In this observational prospective multicentre study, we report the characteristics, early outcome and management of the COVID-19 outbreak on the largest European cohort of liver transplant patients with confirmed SARS-CoV-2 infection up to date. Case fatality rate of the overall study population was 12% (95% CI 5% to 24%), whereas that of the hospitalised patients was 17% (95% CI 7% to 32%). This latter is in line with that of the general population, as reported by most of the largest studies, where the in-hospital case fatality rate ranges from 15% to 22%.1 25 26 All the patients who died, except one, were men. CV disease, obesity, arterial hypertension, diabetes mellitus and chronic kidney disease, although well represented in our population, were not over-represented in the group with adverse outcomes. A clinical history of neoplasia, especially an active cancer at the moment of the diagnosis, was frequently found in the group with a worse prognosis. Recently transplanted patients presented with less fever and respiratory-related symptoms than patients who were transplanted for more than 1 and 5 years, respectively. Among laboratory data, lymphocytopenia and thrombocytopenia were more frequent in patients who died. Alteration in liver enzymes was mild and rarely observed, although mostly found in hospitalised patients. Whether the immunosuppression was decreased or left unchanged had no impact on outcome.
Our study suggests that, despite well-described risk factors for poor outcome of COVID-19 infection are highly represented in our cohort, COVID-19 liver transplant patients show a clinical course not necessarily more severe to that observed in non-liver transplant patients affected by COVID-19.25–27 Publications pooling patients with different organ transplanted reported worse outcomes (in-hospital case fatality rate 24%–27%).11 13 Another publication merging surveys from European and American centres with a smaller sample than our prospective study reported 9 deaths among 39 liver transplant patients.28 Like others, we find that male patients are more prone to develop ARDS29 and have a more severe outcome.25 Although highly frequent in our cohort, CV and metabolic comorbidities were not over-represented in patients with poor outcomes.25 26 History of previous or active cancer, such as being transplanted for HCC or having cancer at the moment of the COVID-19 diagnosis, was associated with a poor outcome. This is in agreement with a national Chinese report on over 2000 confirmed COVID-19 cases with a history of cancer, showing them having higher risk to contract COVID-19 and poorer outcome than individuals without cancer.30 31
Concerning clinical presentation, patients transplanted for less than 5 years exhibited less frequently fever and dyspnoea. This may suggest higher immunosuppression attenuates COVID-19 typical clinical symptoms. GI manifestations were common (33%) in our series, which is in line with the 29% reported in solid organ transplant recipients in Spain.11
Lymphopenia has been reported to be predictive of poor outcome in non-transplanted COVID-19 patients.29 32 A similar trend was found also in our cohort of liver transplant patients.
One of the key questions in the management of liver transplant patients affected with COVID-19 concerns the management of the immunosuppression.33 In our cohort, the immunosuppression was reduced in 39% of the patients and discontinued in 7%. Mycophenolate mofetil was the most discontinued therapy. The majority of the patients with COVID-19 who did not need a hospitalisation were kept on their usual immunosuppressive regimen. Although some reports want to suggest a potential positive role of tacrolimus as antiviral in the treatment of human coronaviruses,34 since 88% of our patients were treated with CNIs, it was not possible to assess any specific effect of this therapy.
Our study has limitations. All the participating centres are European. It will be important to have similar prospective studies from other continents. We limited our analysis to the patients with a positive reverse transcription PCR for SARS-CoV-2. We did not include patients with typical presentation but without a microbiological confirmation due to lack of testing capacity. On the other hand, the NAAT assay as the recommended confirmatory test has a sensitivity in the order of 71%,35 and this could be lower in immunosuppressed population.13 Moreover, although liver transplant patients were generally well instructed to contact their transplant centre as far as COVID-like symptoms appeared, we cannot exclude a global underestimation of the total number of COVID-19 infections in this population.
Our study has strengths. It is, at the time of writing, the largest prospective study of liver recipient patients affected by COVID-19. It is by design not a survey but a prospective acquisition of data approved by local ethics committees.
In conclusion, in this European multicentre prospective study of liver transplant recipients, COVID-19 is associated with an overall and in-hospital case fatality rate of 12% (95% CI 5% to 24%) and 17% (95% CI 7% to 32%), respectively. Patients infected early after liver transplantation did not have a worse outcome and tend to have less symptoms. A history of cancer was more frequent in patients with poorer outcome.
Acknowledgments
We thank all the liver transplant patients who participated in the study, Annetta Redmann from Bern CTU for logistical and technical support, and Professor Annalisa Berzigotti and Dr Giacomo Buso for statistical support and intellectual contribution.
Footnotes
Twitter: @mario.romero@salud.madrid.org, @dufour_jf
Correction notice: This article has been corrected since it published Online First. The first affiliation has been amended.
Collaborators: COVID-LT group: Michele Colledan (Department of Surgery, General Surgery and Abdominal Transplant Unit, "Papa Giovanni XXIII" Hospital, Bergamo, Italy), Stefano Fagiuoli (Gastroenterology and Transplant Hepatology, “Papa Giovanni XXIII” Hospital, Bergamo, Italy), Stefania Camagni (Gastroenterology and Transplant Hepatology, “Papa Giovanni XXIII” Hospital, Bergamo, Italy), Jean Delwaide (Division of Hepato-Gastroenterology and Digestive Oncology, University Hospital of Liege, Liege, Belgium), Giovanni Vitale (Department of Organ Failures and Transplantation, University Hospital of Bologna, Policlinico S. Orsola-Malpighi, Bologna, Italy), Darius Moradpour (Division of Gastroenterology and Hepatology, Centre Hospitalier Universitaire Vaudois, University of Lausanne, Lausanne, Switzerland), Manuel Pascual (Transplantation Center, Centre Hospitalier Universitaire Vaudois, University of Lausanne, Lausanne, Switzerland), Gloria Allegrini (Department of Gastroenterology, University Hospital Ancona, Polytechnic University of Marche, Ancona, Italy), Fabio Tarsetti (Department of Gastroenterology, University Hospital Ancona, Polytechnic University of Marche, Ancona, Italy), Ugo Giustizieri (Department of Surgery, General Surgery and Abdominal Transplant Unit, "Papa Giovanni XXIII" Hospital, Bergamo, Italy), Loredana Rota (Gastroenterology and Transplant Hepatology, “Papa Giovanni XXIII” Hospital, Bergamo, Italy), Florent Artru (Division of Gastroenterology and Hepatology, Centre Hospitalier Universitaire Vaudois, University of Lausanne, Lausanne, Switzerland), Anne-Catherine Saouli (Transplantation Center, Centre Hospitalier Universitaire Vaudois, University of Lausanne, Lausanne, Switzerland), Patrizia Burra (Multivisceral Transplant Unit, Department of Surgery, Oncology, Gastroenterology, Padua University Hospital, Padua, Italy), Martina Gambato (Multivisceral Transplant Unit, Department of Surgery, Oncology, Gastroenterology, Padua University Hospital, Padua, Italy), Irene Scalera (Department of Hepato-Biliary Surgery and Liver Transplantation, “Cardarelli” Hospital of Naples, Naples, Italy), Ioannis Petridis (Department for the Treatment and Study of Abdominal Diseases and Abdominal Transplantation, IRCCS-ISMETT (Istituto di Ricovero e Cura a Carattere Scientifico - Istituto Mediterraneo per i Trapianti e Terapie ad alta specializzazione), UPMC (University of Pittsburgh Medical Center) Italy, Palermo, Italy), Hugo Pinto Marques (Hepato-Biliary-Pancreatic and Transplantation Center, Curry Cabral Hospital, Lisbon's Central Hospitals and University Center, NOVA Medical School, Lisboa, Portugal), Martin-Walter Welker(Department of Internal Medicine 1, University Hospital Frankfurt, Goethe University, Frankfurt, Germany).
Contributors: CB: study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, statistical analysis, administrative, technical and material support. MFZ, LP, MFD, FI, OD, GD, OC, MCM, MF, GS-B, HvV, MJC, MCR, AdG, PT: acquisition of data, critical revision of the manuscript regarding important intellectual content. LDP, CA: acquisition of data. DS, JP, FN: study concept and design, acquisition and interpretation of data, technical and material support, critical revision of the manuscript regarding important intellectual content. J-FD: study concept and design, interpretation of data, drafting of the manuscript, critical revision of the manuscript regarding important intellectual content, funding recipient, technical and material support, study supervision.
Funding: This study was funded by Stiftung für die Leberkrankheiten (Switzerland).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: The ethical committee of each participating centre approved the study, which was carried in accordance with the Helsinki Declaration.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.
Contributor Information
COVID-LT group:
Michele Colledan, Stefano Fagiuoli, Stefania Camagni, Jean Delwaide, Giovanni Vitale, Darius Moradpour, Manuel Pascual, Gloria Allegrini, Fabio Tarsetti, Ugo Giustizieri, Loredana Rota, Florent Artru, Anne-Catherine Saouli, Patrizia Burra, Martina Gambato, Irene Scalera, Ioannis Petridis, Hugo Pinto Marques, and Martin-Walter Welker
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Spiezia L, Boscolo A, Poletto F, et al. COVID-19-Related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost 2020;120:998–1000. 10.1055/s-0040-1710018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Deng X, Yang J, Wang W, et al. Case fatality risk of the first pandemic wave of novel coronavirus disease 2019 (COVID-19) in China. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa578. [Epub ahead of print: 15 May 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. COVID-19 coronavirus pandemic. Available: https://www.worldometers.info/coronavirus/
- 5. COVID-19 Dashboard by the center for systems science and engineering (CSSE) at Johns Hopkins University (JHU). Available: https://coronavirus.jhu.edu/map.html
- 6. WHO Coronavirus disease (COVID-19) pandemic. Available: https://www.who.int
- 7. Fix OK, Hameed B, Fontana RJ, et al. Clinical best practice advice for hepatology and liver transplant providers during the COVID-19 pandemic: AASLD expert panel consensus statement. Hepatology 2020. doi: 10.1002/hep.31281. [Epub ahead of print: 16 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Boettler T, Newsome PN, Mondelli MU, et al. Care of patients with liver disease during the COVID-19 pandemic: EASL-ESCMID position paper. JHEP Rep 2020;2:100113. 10.1016/j.jhepr.2020.100113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhu L, Xu X, Ma K, et al. Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am J Transplant 2020. doi: 10.1111/ajt.15869. [Epub ahead of print: 17 Mar 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bhoori S, Rossi RE, Citterio D, et al. COVID-19 in long-term liver transplant patients: preliminary experience from an Italian transplant centre in Lombardy. Lancet Gastroenterol Hepatol 2020;5:532–3. 10.1016/S2468-1253(20)30116-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fernández-Ruiz M, Andrés A, Loinaz C, et al. COVID-19 in solid organ transplant recipients: a single-center case series from Spain. Am J Transplant 2020. doi: 10.1111/ajt.15929. [Epub ahead of print: 16 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fishman JA. Infection in solid-organ transplant recipients. N Engl J Med 2007;357:2601–14. 10.1056/NEJMra064928 [DOI] [PubMed] [Google Scholar]
- 13. Pereira MR, Mohan S, Cohen DJ, et al. COVID-19 in solid organ transplant recipients: initial report from the US EpiCenter. Am J Transplant 2020. doi: 10.1111/ajt.15941. [Epub ahead of print: 24 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kumar D, Tellier R, Draker R, et al. Severe acute respiratory syndrome (SARS) in a liver transplant recipient and guidelines for donor SARS screening. Am J Transplant 2003;3:977–81. 10.1034/j.1600-6143.2003.00197.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. AlGhamdi M, Mushtaq F, Awn N, et al. Mers CoV infection in two renal transplant recipients: case report. Am J Transplant 2015;15:1101–4. 10.1111/ajt.13085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fishman JA, Grossi PA. Novel Coronavirus-19 (COVID-19) in the immunocompromised transplant recipient: #Flatteningthecurve. Am J Transplant 2020;382 10.1111/ajt.15890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhang C, Shi L, Wang F-S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol 2020;5:428–30. 10.1016/S2468-1253(20)30057-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Xu L, Liu J, Lu M, et al. Liver injury during highly pathogenic human coronavirus infections. Liver Int 2020;40:998–1004. 10.1111/liv.14435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fan Z, Chen L, Li J, et al. Clinical features of COVID-19-Related liver functional abnormality. Clin Gastroenterol Hepatol 2020;18:1561–6. 10.1016/j.cgh.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Global surveillance for COVID-19 caused by human infection with COVID-19 virus: interim guidance, 2020. Available: https://www.who.int/publications-detail/global-surveillance-for-covid-19-caused-by-human-infection-with-covid-19-virus-interim-guidance
- 21. Wong HYF, Lam HYS, Fong AH-T, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology 2019;201160:201160. 10.1148/radiol.2020201160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rabkin JM, de La Melena V, Orloff SL, et al. Late mortality after orthotopic liver transplantation. Am J Surg 2001;181:475–9. 10.1016/S0002-9610(01)00595-5 [DOI] [PubMed] [Google Scholar]
- 23. ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA 2012;307:2526–33. 10.1001/jama.2012.5669 [DOI] [PubMed] [Google Scholar]
- 24. Gautret P, Lagier J-C, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020;105949:105949. 10.1016/j.ijantimicag.2020.105949 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020. doi: 10.1001/jamainternmed.2020.0994. [Epub ahead of print: 13 Mar 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA 2020. doi: 10.1001/jama.2020.6775. [Epub ahead of print: 22 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect 2020. 10.1016/j.jinf.2020.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Webb GJ, Moon AM, Barnes E, et al. Determining risk factors for mortality in liver transplant patients with COVID-19. Lancet Gastroenterol Hepatol 2020. doi: 10.1016/S2468-1253(20)30125-4. [Epub ahead of print: 24 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhang J, Yu M, Tong S, et al. Predictive factors for disease progression in hospitalized patients with coronavirus disease 2019 in Wuhan, China. J Clin Virol 2020;127:104392. 10.1016/j.jcv.2020.104392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 2020;21:335–7. 10.1016/S1470-2045(20)30096-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Desai A, Sachdeva S, Parekh T, et al. COVID-19 and cancer: lessons from a pooled meta-analysis. JCO Glob Oncol 2020;6:557–9. 10.1200/GO.20.00097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tan L, Wang Q, Zhang D, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther 2020;5:33. 10.1038/s41392-020-0148-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. American Association for the Study of Liver Diseases Clinical insights for hepatology and liver transplant providers during the COVID-19 pandemic, 2020. Available: https://www.aasld.org/sites/
- 34. Russell B, Moss C, George G, et al. Associations between immune-suppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence. Ecancermedicalscience 2020;14:1022. 10.3332/ecancer.2020.1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology 2020;200432:200432 10.1148/radiol.2020200432 [DOI] [PMC free article] [PubMed] [Google Scholar]