Extracorporeal membrane oxygenation (ECMO) support is proposed as rescue therapy for severe acute respiratory distress syndrome (ARDS) related to coronavirus disease 2019 (COVID-19) [1]. Severe bleeding events were described in severe ARDS patients requiring ECMO in large cohorts [2]. Few studies reported their experiences in COVID-19 critically ill patients receiving ECMO [3]. However, Yang et al. [4] highlighted in their retrospective cohort a high mortality rate in these patients. We report a severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) necrotising pneumonia-induced fatal haemorrhagic complication with ECMO.
Short abstract
ECMO and curative anticoagulation may be associated with severe bleeding events in #COVID19 pneumonia. ECMO and high levels of anticoagulation must be considered with caution in the most severe patients with #SARS-CoV-2 necrotising pneumonia. https://bit.ly/3clhu31
To the Editor:
Extracorporeal membrane oxygenation (ECMO) support is proposed as rescue therapy for severe acute respiratory distress syndrome (ARDS) related to coronavirus disease 2019 (COVID-19) [1]. Severe bleeding events were described in severe ARDS patients requiring ECMO in large cohorts [2]. Few studies reported their experiences in COVID-19 critically ill patients receiving ECMO [3]. However, Yang et al. [4] highlighted in their retrospective cohort a high mortality rate in these patients. We report a severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) necrotising pneumonia-induced fatal haemorrhagic complication with ECMO.
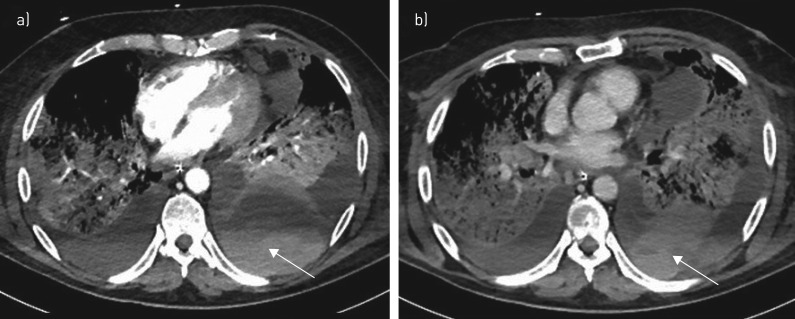
A 68-year-old patient without comorbidities was hospitalised in our French medical ICU on 20 March 2020, with positive reverse transcriptase-PCR for SARS-CoV-2 and severe ARDS according to the Berlin definition; i.e. arterial oxygen tension/inspired oxygen fraction ratio (PaO2/FIO2) at 80 mmHg under invasive mechanical ventilation with a positive end-expiratory pressure of 15 cmH2O and bilateral ground-glass opacities on chest images without heart failure [5]. The patient received an intravenously prophylactic dose of unfractionated heparin to prevent thromboembolic events. Four days later, ECMO was implemented for refractory respiratory failure despite protective ventilation: tidal volume 6 mL·Kg−1 and respiratory rate 30 breaths·min−1, driving pressure was 15 cmH2O, PaO2/FIO2 was 48 mmHg, the patient had respiratory acidosis (pH 7.24) and arterial carbon dioxide tension was 72 mmHg. After 72-h of ECMO, the patient developed haemorrhagic shock related to spontaneous left haemothorax. Injected computed tomography examination ruled out any macrovascular injuries or pulmonary embolism but showed a defect of segmental lung enhancement related to pulmonary necrosis (figure 1). Inflammatory parameters were high, including leukocyte count (28.6 g·L−1), CRP (135 mg·Kg−1) and fibrinogen (670 mg·dL−1). Prothrombin time and platelet count were in the normal range, and heparinisation was monitored with Anti-Xa (target: 0.2–0.5 UI Anti-Xa per mL) without any overdosing. An invasive microbiological sample was performed and neither bacterial nor fungal co-infection were found. Management consisted of thoracic drainage and massive blood component transfusion according to standard guidance for haemorrhagic shock. Despite these therapeutics and other specific organ supports, the patient died from vasoplegic refractory shock with multiple organ failure related to a major systemic inflammatory response syndrome.
FIGURE 1.
Computed tomography images of a 68-year-old patient with severe acute respiratory distress syndrome-coronavirus-2. Axial images in a) the arterial phase and b) after 80 s show major left circumferential haemothorax with fresh blood (arrows) without active bleeding, complicating lower lobar pulmonary necrosis.
Few data are available regarding alveolar damage related to SARS-CoV-2, and necrotising pneumonia has never been described. Some characteristics of COVID-19 pulmonary injuries must be pointed out. First, necrotising pneumonia is known to be associated with fungal or bacterial co-infection, especially Staphylococcus aureus, which is one of the major causes of death following virus influenza infection [6]. Despite invasive aspergillosis being reported in immunocompetent severe COVID-19 patients [7], other pathogen profiles are not yet established, and descriptive clinico-microbiological studies are still warranted. Secondly, severe SARS-CoV-2 is characterised by an overexuberant inflammatory response [8], which could also be exacerbated by implementation of ECMO [9], contributing to worse lung damage. Interestingly, pathological findings in post mortem lung biopsies have been recently described after SARS-CoV-2 infection-induced ARDS. Abnormalities were predominantly pulmonary oedema and hyaline membrane formation [10], or the presence of acute fibrinous and organising pneumonia [11]. Those abnormalities might be a target for anti-inflammatory drugs. Moreover, exudative diffuse alveolar damage with massive capillary congestion, often accompanied by microthrombi, were recently reported in a case series of autopsies [12]. In this later study, the authors also described other lung injuries related to pulmonary embolisms, alveolar haemorrhage and vasculitis. These findings provide an important insight into the complexity of COVID-19 pathophysiology, but pulmonary capillarostasis and the presence of microthrombi in the lungs suggest a key role in impaired microcirculation, that might explain the necrotising pneumonia seen in our case, then the occurrence of haemothorax under curative anticoagulation due to ECMO. Thirdly, significant abnormalities in coagulation parameters have been reported in critically ill patients with COVID-19 that are associated with mortality [13]. This procoagulant state may increase the risk for thromboembolic events, especially disseminated intravascular coagulopathy and pulmonary embolism [14]. Of note, biomarkers showed hyperinflammation without argument for associated disseminated intravascular coagulopathy in our case report. To date, few bleeding manifestations have been reported in the literature focusing on COVID-19. In this context, some authors suggest, without an evidence-based approach, a potential benefit of preventive anticoagulation for thromboembolic disease at higher than usual doses in intensive care unit patients with ARDS and without contraindications [14, 15].
In conclusion, SARS-CoV-2 patients seems to be more prone to disseminated intravascular coagulopathy development and thromboembolic complications related to a particular hyperinflammatory status, and consequently good candidates for early thromboembolic prophylaxis. Our experience and the weakness of strong evidence about COVID-19 pathophysiological and disease courses support the fact that ECMO and escalated doses of anticoagulation for thromboembolic event prophylaxis in severe COVID-19 patients must be considered with caution.
Acknowledgements
The authors declare they have obtained the patient's next of kin consent for the publication.
Footnotes
Conflict of interest: S. Goursaud has nothing to disclose.
Conflict of interest: M. Mombrun has nothing to disclose.
Conflict of interest: D. du Cheyron has nothing to disclose.
References
- 1.World Health Organization. 27 May 2020. Clinical management of COVID-19. Interim guidance. WHO/2019-nCoV/clinical/2020.5.
- 2.Combes A, Hajage D, Capellier G, et al. . Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med 2018; 378: 1965–1975. doi: 10.1056/NEJMoa1800385 [DOI] [PubMed] [Google Scholar]
- 3.Ñamendys-Silva S. ECMO for ARDS due to COVID-19. Heart Lung 2020; 49: 348–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang X, Yu Y, Xu J, et al. . Clinical course and outcomes of critically ill patients with a SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020; 4: 475–481. doi: 10.1016/S2213-2600(20)30079-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, et al. . Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012; 307: 2526–2533. [DOI] [PubMed] [Google Scholar]
- 6.Morris DE, Cleary DW, Clarke SC. Secondary bacterial infections associated with influenza pandemics. Front Microbiol 2017; 8: 1041. doi: 10.3389/fmicb.2017.01041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koehler P, Cornely OA, Böttiger BW, et al. . COVID-19 associated pulmonary aspergillosis. Mycoses 2020; 63: 528–534. doi: 10.1111/myc.13096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehta P, McAuley DF, Brown M, et al. . COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020; 395: 1033–1034. doi: 10.1016/S0140-6736(20)30628-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henry B. COVID-19, ECMO, and lymphopenia: a word of caution. Lancet Respir Med 2020; 8: e24. doi: 10.1016/S2213-2600(20)30119-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu Z, Shi L, Wang Y, et al. . Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020; 8: 420–422. doi: 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Copin MC, Parmentier E, Duburcq T, et al. . Time to consider histologic pattern of lung injury to treat critically ill patients with COVID-19 infection. Intensive Care Med 2020; 46: 1124–1126. doi: 10.1007/s00134-020-06057-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menter T, Haslbauer JD, Nienhold R, et al. . Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction. Histopathology 2020; in press [ 10.1111/his.14134]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang N, Li D, Wang X, et al. . Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020; 18: 844–847. doi: 10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Helms J, Tacquard C, Severac F, et al. . High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020; 46: 1089–1098. doi: 10.1007/s00134-020-06062-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood 2020; 135: 2033–2040. doi: 10.1182/blood.2020006000 [DOI] [PMC free article] [PubMed] [Google Scholar]