Abstract
Background
Erector spinae plane block (ESPB) as a new trunk fascia block technique was proposed in 2016. ESPB has aroused the interest of many nerve block experts. However, there are few clinical studies on ESPB for lumbar surgery, and its effectiveness and safety are controversial. The goal of this review is to summarize the use of ESPB for lumbar spine surgery in order to better understand this technique.
Methods
PubMed, EMBASE, Cochrane library and ClinicalTrial.gov databases were searched up to July 30, 2019. According to the inclusion and exclusion criteria established in advance, “lumbar spine surgery” and “ESPB” related MesH terms and free-text words were used. Data on pain scores, analgesic consumptions and adverse effects were reported. All processes follow PRISMA statement guidelines.
Results
A total of 171 participants from 11 publications were identified, including two randomized controlled trials (RCTs), one retrospective cohort study, four case reports and four cases series. Block operation planes from T8 to L4. The main anesthetics used in the block are bupivacaine, ropivacaine and lidocaine. There was evidence for reducing postoperative pain scores and analgesic consumptions.
Conclusion
The effectiveness and safety of ESPB for lumbar spine surgery are still controversial. The current evidence is insufficient to support the widespread use of ESPB for lumbar spine surgery. High-quality RCTs are urgently needed.
Keywords: ESPB, lumbar spine surgery, postoperative analgesia
Introduction
Postoperative pain is often severe in patients undergoing lumbar surgery. Due to postoperative pain, patients are unwilling to get out of bed at an early stage, which affects their recovery.1,2 Patient-controlled analgesia or epidural injection analgesia is usually used in the clinic. However, patient-controlled analgesia is prone to opioid-related side effects. Epidural injection is associated with infections, hematomas and other adverse events.3,4 Furthermore, the analgesic effect of conventional postoperative analgesia is limited. If the postoperative pain of the lumbar spine could not be effectively relieved, it may develop into chronic pain, affecting the quality of life of the patients.5
Erector spinae plane block (ESPB) as a new trunk fascia block technique was proposed in 2016.6 ESPB has aroused the interest of many nerve block experts. The benefits of ESPB are not yet demonstrated. The specific mechanism is still controversial. Some believethat ESPB can block the posterior root of the spinal nerve and produce part of the paraspinal block effect with the diffusion of the drug solution.7,8 Many scholars have applied ESPB to postoperative analgesia in chest and abdomen. Furthermore, they found that ESPB may reduce perioperative muscle relaxation and analgesic drug use. Finneran and co-workers reported that ESPB can provide analgesia for breast surgery.9 A study reported that ESPB was effective for abdominal analgesia in weight loss surgery.10 Similarly, a report showed that ESPB relieved postoperative pain in patients with lumbosacral spine surgery, reducing the use of analgesic drugs.11 Some believed that the analgesic effect of ESPB may be better than that of epidural injection.12 Reducing the use of analgesic drugs in the perioperative period is beneficial to accelerate the recovery of patients and reduce the cost of hospitalization.
However, few clinical studies have focused on ESPB in lumbar surgery. What is more, there are differences in the mechanism and effect of block in different parts of the erector spinal muscle.13 Some scholars question the practicability of ESPB in lumbar surgery. Tseng and Xu believe that postoperative analgesia in patients with lumbar spine surgery using a thoracolumbar interfascial plane (TILP) block may be better than ESPB.14 Therefore, it is necessary to systematically summarize the use of ESPB in lumbar spine surgery so as to better understand and promote this technique and benefit patients undergoing lumbar surgery.
Methods
Literature Search
PubMed, EMBASE, Cochrane library,= and ClinicalTrial.gov databases were searched. MeSH terms and free-text words were used, including “lumbar spine surgery”, “decompression”, “lumbar spinal stenosis”, “spondylolisthesis”, “ESP block”, “erector spinae plane block”. The search time was from inception to July 30, 2019. References to relevant articles or reviews were screened to prevent missed inspection. Our retrieval method was developed together with experienced literature retrieval teachers. All the retrieval results were read independently by the two researchers (QY, ZTJ). According to the established inclusion and exclusion criteria, the title, abstract and full text were strictly evaluated, and the basic information included in the article was extracted. Disagreements were resolved by discussing or consulting with another author. All processes followed PRISMA statement guidelines.
Inclusion and Exclusion Criteria
Inclusion Criteria
(1) Study: Case report, case series, retrospective cohort study, and randomized controlled trials (RCTs); (2) participants: lumbar spine surgery patients; (3) interventions: erector spinae plane block.
Exclusion Criteria
Review.
Data Collection
Type of publication, year of publication, journal name, authorship country of origin, type of block (single shot, continuous, intermittent bolus), anatomic location, patient age, multimodal analgesia use, opioid consumption, sensory and motor changes, reported single injection techniques, continuous catheters, additives, opioid-related and block-related side effects and adverse events, visual analogue scales (VAS) or numeric rating scales (NRS), patient satisfaction were collected.
Quality Evaluation
Risk of bias for RCTs were assessed by two researchers using a modified Cochrane risk of bias assessment tool. RCTs were evaluated in terms of random sequence generation; allocation concealment; blinding of patients, clinicians, data collectors, outcome assessors, and data analysts; incomplete outcome data; and selective outcome reporting; other biases. Each potential source of bias was graded as “low risk”, “unclear risk” or “high risk”. Bias risk map and bias risk summary diagram were generated by RevMan 5.3 (The Cochrane Collaboration, 2014).
Results
Search results
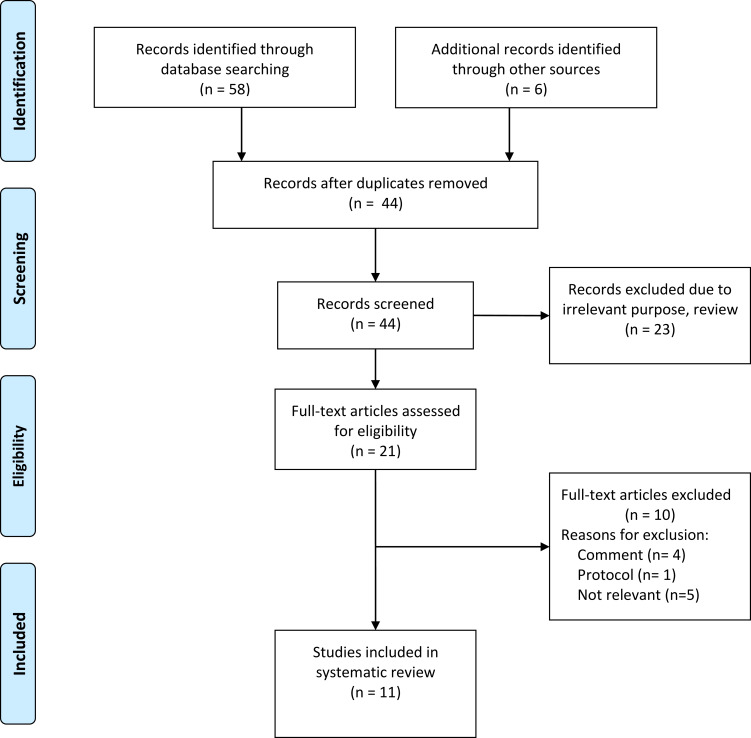
A total of 171 participants from 11 publications were identified, including two RCTs, one retrospective cohort study, four case reports and four caseseries.11,15-24 The main reasons for the exclusion of articles were non-lumbar surgery or unrelated to the purpose of the study (Figure 1).
Figure 1.
Flow chart showing the identification and selection of the articles for the systematic review.
Included Literature
Outcome indicators included morphine consumption, pain scores, adverse reactions and patient satisfaction after lumbar spine surgery. The follow-up period was from 10 hours to 72 hours. Only one article reported that postoperative pain in the lumbar spine was relieved by ESPB and catheterization (placement of a continuous peripheral nerve catheter), and the other 10 articles were treated with bilateral single injection before operation. Block operation plane from T8 to L4. The main anesthetics used in the block are bupivacaine, ropivacaine and lidocaine. Most of the studies lack a comparator; the effectiveness and safety of ESPB for lumbar spine surgery are still controversial (Table 1).
Table 1.
Qualitative Evaluation of the Studies That Assessed the Postoperative Analgesia of ESPB on Lumbar Spine Surgery
| Author | Country | Study Design | Study Size | Surgical Operation | ESPB | Outcome | Side Effect | Follow-Up Time | Conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Canturk et al (2019)15 | Turkey | Case report | 1 | Lumbar spinal fusion | L1 vertebra level, both sides with 10 mL bupivacaine 0.25% and 10 mL prilocaine 1%, single-shot. | Opioid consumption, NRS pain scores. | None | 24 hours | ESPB provides a clear surgical field and long-lasting postoperative analgesia. |
| De et al (2019)16 | Spain | Case series | 8 | Lumbar spinal fusion | L4 vertebra level, both sides with 20 mL ropivacaine 0.2%, single-shot. | VAS pain scores, rescue analgesia consumption. | None | 48 hours | Lumbar ESP appears to contribute to pain control during the first 48 hours after lumbar spinal fusion. |
| Singh et al (2019)17 | India | Case series | 7 | Surgery for PLID or lumbar stenosis | T10 vertebra level, both sides with 20 mL bupivacaine 0.25%, single-shot. | NRS score, rescue analgesia. | None | 10 hours | The average length of analgesia provided by ESPB was between 6 and 8 hours. |
| Almeida et al (2019)18 | Portugal | Case report | 1 | L2–S1 spine fusion | Post-operative day 1, T8 vertebra level, both sides with 20mL ropivacaine 0.2%, ESP catheterizations and continuous infusion (5 mL/hour) of ropivacaine 0.2% per side was maintained for 48 hours. | NRS scores | None | 48 hours | Bilateral ESP catheterizations at T8 are safe and contribute to significant analgesic improvement. |
| Singh et al (2019)19 | India | RCT | 40 | Elective lumbar spine surgery | T10 vertebra level, both sides with 20 mL bupivacaine 0.5%, single-shot. | Opioid consumption, NRS scores, patient satisfaction. | Two patients in the control group developed severe nausea and vomiting. | 24 hours | US-guided ESP block reduces postoperative opioid requirement and improves patient satisfaction. |
| Ueshima et al (2019)20 | Japan | Retrospective study | 41 | Lumbar spinal surgery | Target vertebral level, both sides with 20 mL levobupivacaine 0.375%. | NRS scores, analgesia consumption, complications. | None | 24 hours | The ESP block provides effective postoperative analgesic effect for 24 hours. |
| Yayik et al (2019)21 | Turkey | RCT | 60 | Open lumbar decompression | L3 vertebra level, both sides with 20 mL bupivacaine 0.25%, single-shot. | VAS scores, opioid consumption, rescue analgesia, opioid-related side effects. | None | 24 hours | ESP block can be used in multimodal analgesia practice to reduce opioid consumption and relieve acute postoperative pain. |
| Brandao et al (2018)22 | Portugal | Clinical report | 1 | Lumbar spine surgery | L4 vertebra level, both sides with 15 mL ropivacaine 0.375%, single-shot. | Pain scores, analgesia consumption. | None | 48 hours | Performing the block preoperatively dismissed the need for extra intraoperative opioids other than those for intubation and provide a clear surgical field. |
| Calandese et al (2018)23 | Italy | Case report | 1 | Anterior thoracolumbar spine surgery | T10 vertebra level, a total of 40 mL of 0.25% levobupivacaine and 2 mL (8 mg) of dexamethasone was injected bilaterally. | NRS scores, analgesia consumption. | None | 24 hours | ESPB as part of a multimodal analgesia strategy can provide effective postoperative pain management after anterior thoracolumbar spine surgery. |
| Cesur et al (2018)24 | Turkey | Case series | 5 | Lumbar surgery | T12 vertebra level, both sides with 20 mL local anesthetic solution containing bupivacaine 0.25% and lidocaine 1%, single-shot. | NRS scores, analgesia consumption. | None | 24 hours | ESPB achieved effective analgesia and reduced opioid consumption in the single or multilevel lumbar spine surgeries. |
| Melvin et al (2018)11 | USA | Case series | 6 | Lumbosacral spine surgery | T10 (n= 2) and T12 (n= 4), which concluded 3 single-injection and 3 continuous ESPB. | NRS scores, analgesia use. | None | 72 hours | The ESP block contribute significantly to analgesia and enhance recovery. |
Abbreviations: ESPB, erector spinae plane block; ESP, erector spinae plane; NRS, numeric rating scales; VAS, visual analogue scales; PLID, prolapsed lumbar intervertebral disk; RCT, randomized controlled trial; US, ultrsound.
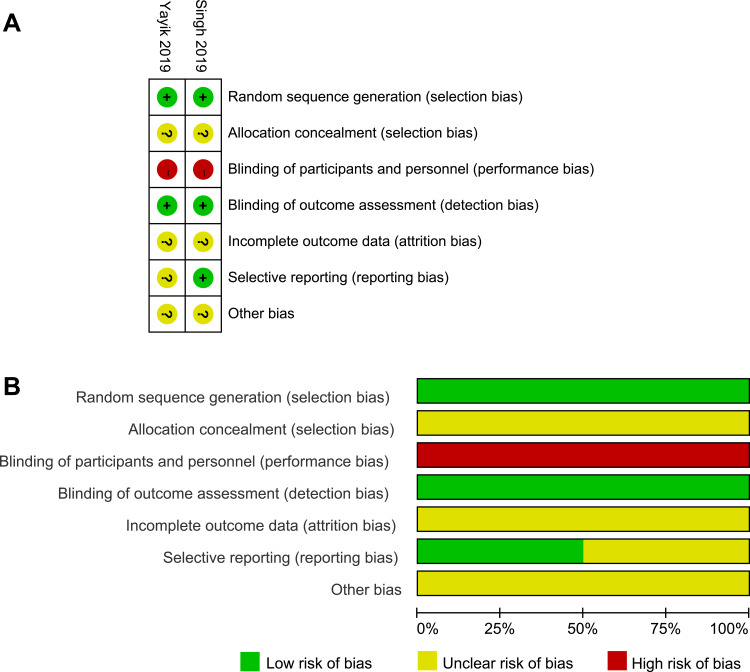
At the same time, a total of two RCTs were included, but the heterogeneity of outcome indicators could not be analyzed by meta-analysis. Both RCTs found that ESPB significantly reduced lumbar postoperative pain scores and analgesic drug consumption, and no operation-related adverse events occurred. However, the random blind method of the two studies did not do well. Furthermore, small RCTs may not be able to detect adverse effects of therapeutic procedures (Figure 2A and B).
Figure 2.
(A) Risk of bias summary: green circles with “+” sign indicate low risk, yellow circles with “?” sign indicate unclear risk, red circles with “–” sign indicate high risk. (B) Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies.
Discussion
There is an increase in the number of patients with lumbar diseases, and a large number of them need lumbar surgery.25 As there is obvious pain after lumbar surgery, postoperative analgesia is often needed. However, patient-controlled intravenous analgesia and epidural analgesia, which are commonly used in the clinic, have their own shortcomings.4,25 Side effects such as nausea and vomiting caused by postoperative opioid use result in poor postoperative experience, reduce patient satisfaction, and are not conducive to rapid recovery.26 In fact, neuraxial techniques may be complicated with headache, backache, unintended dural punctures, and puncture site hemorrhage. Neuraxial ultrasound may help improve the safety. Epidural hematoma, epidural abscess and intracord injections are rare but serious complications that need more attention.27 In addition, neuraxial techniques have disadvantages such as hypotension, urinary retention and being limited to the patient who has spine fracture or spine surgery. Paraneuraxial nerve blocks such as Erector spinae plane (ESP) block may have an advantage in success rate and analgesic efficacy.28 In recent years, many researchers have used ESPB for postoperative analgesia and found that local anesthetic spread well, volume-dependent, and extended into the neural foramina and epidural space normally. At the same time, local anesthetic may show significantly more epidural spread when the lamina and ligaments are compromised, which need more attention.10,29 The local anesthetics injected during ESPB spread widely and could produce the effect of a paraspinal block; therefore, the block range was wide and could last until a period of time after operation.14,30,31 However, there are few studies on ESPB for postoperative analgesia of lumbar spinae surgery patients.32 Therefore, it is necessary to summarize the relevant clinical studies. Eleven studies of ESPB for lumbar surgery were included, and data from 171 patients were extracted and analyzed. Interestingly, two RCTs showed that ESPB may reduce postoperative opioid consumption and pain scores in patients undergoing lumbar surgery. One study showed that ESPB may improve patient satisfaction. However, most of the studies lack a comparator. The effectiveness and safety of ESPB for lumbar spine surgery are still controversial. High-quality RCTs are urgently needed.
It has been reported that pain is obvious at 4 hours after lumbar surgery and relieved after 72 hours. What is more, regional anesthesia can help patients reduce pain and other discomfort.18,33 Interestingly, Singh found that when 0.25% 20 mL bupivacaine was injected on both sides of the T10 plane, the 6th hour NRS score was low; however, the 8th hour NRS score was high after lumbar surgery, which suggested that the ESPB could last for 6– 8 h after operation.34 The duration of ESPB block was related to the type and dose of local anesthetics. In addition, local will be washout during the surgery, if ESPB was performed before incision.13 However, safety and dosing were not evaluated in any of the included studies. Duration was not assessed as a primary endpoint in the included research. The safe doses of different local anesthetics were different. For example, the unilateral injection volume of ropivacaine was 20 to 40 mL, the concentration was 0.25% to 0.5%, and the total safe dose was 150 mg. It is recommended that each side of bilateral block should be given 0.375% ropivacaine 20 mL in adults.15,35 Therefore, the dose or concentration can be increased appropriately to prolong the analgesia time and help the patients to get through the most painful stage after operation. At the same time, adding other meds to prolong the duration could be helpful. Related high-quality research is necessary and urgently needed.
The puncture plane was from T8 to L4, and the follow-up time was from 10 to 72 h. However, in different studies, different anesthetic techniques were used. Some researchers pay attention to the use of rescue painkillers, while some studies focus on the total amount of postoperative analgesia drugs.14,36 Furthermore, different basic analgesia regimens may cause differences in pain scores. As a result, there is great heterogeneity among different studies, and the results cannot be quantitatively synthesized and analyzed. At the same time, it is suggested that we should pay more attention to the primary outcome indicators in the design of clinical trials in the future. The recently reported protocol of ESPB for postoperative analgesia of lumbar surgery is worthy of reference.14 At the same time, it is important to note that little attention has been paid to the effects of ESPB on the use of intraoperative analgesic drugs and muscle relaxants. Only one case report mentioned that ESPB could effectively reduce the use of analgesia and muscle relaxant drugs during the perioperative period of spondylolisthesis correction surgery, and appropriate hypotension was beneficial to surgical visual field exposure and operation.37 Reducing the use of perioperative anesthetics cannot only reduce the cost of hospitalization, but also reduce the possible side effects of extensive use of anesthetics. At present, some scholars believe that perioperative use of opioids can affect the immune function of patients, and may be associated with the poor prognosis of tumor patients. At the same time, reducing the use of perioperative opioids may reduce the risk of tumor recurrence.38,39 From this point of view, it seems that the effect of ESPB on intraoperative opioid dosage is also worthy of attention. On the other hand, the included studies did not seem to pay particular attention to the effect of ESPB on early out-of-bed activity and postoperative hospital stay in patients with lumbar spine surgery. Early out-of-bed activity and early discharge from hospital comply with ERAS, which is also the reason for the promotion of ESPB in patients undergoing lumbar surgery. At the same time, no adverse events related to ESPB were found in the 11 studies. We believe that the clinical research quality of ESPB for lumbar surgery should be improved, and the mechanism of ESPB for postoperative analgesia and perioperative protection of lumbar spine should be further explored.
Limitation
Although we have strictly formulated the scheme of literature retrieval and data extraction, there are few research reports that can be included. Only two RCT articles were included, and the outcome could not be analyzed. The sample size of the two articles is small, and the random, blind method and research quality need to be improved. Furthermore, most of the studies lack a comparator.
Conclusions
The effectiveness and safety of ESPB for lumbar spine surgery are still controversial. The current evidence is insufficient to support the widespread use of ESPB for lumbar spine surgery. High-quality RCTs are urgently needed.
Acknowledgments
We are thankful to Ling-bing Meng and Meng-lei Hao for their assistance and suggestions during the submitting process.
Funding Statement
Not applicable.
Abbreviations
ESPB, erector spinae plane block; TILP, thoracolumbar interfascial plane; RCTs, randomized controlled trials.
Data Sharing Statement
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Saleh A, Thirukumaran C, Mesfin A, Molinari RW. Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2320 patients. Spine J. 2017;17(8):1106–1112. doi: 10.1016/j.spinee.2017.03.019 [DOI] [PubMed] [Google Scholar]
- 2.Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79–86. [DOI] [PubMed] [Google Scholar]
- 3.Naik BI, Nemergut EC, Kazemi A, et al. The effect of dexmedetomidine on postoperative opioid consumption and pain after major spine surgery. Anesth Analg. 2016;122(5):1646–1653. doi: 10.1213/ANE.0000000000001226 [DOI] [PubMed] [Google Scholar]
- 4.Gessler F, Mutlak H, Tizi K, et al. Postoperative patient-controlled epidural analgesia in patients with spondylodiscitis and posterior spinal fusion surgery. J Neurosurg Spine. 2016;24(6):965–970. doi: 10.3171/2015.8.SPINE15415 [DOI] [PubMed] [Google Scholar]
- 5.Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118(3):474–475. doi: 10.1093/bja/aex013 [DOI] [PubMed] [Google Scholar]
- 6.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–627. doi: 10.1097/AAP.0000000000000451 [DOI] [PubMed] [Google Scholar]
- 7.Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: back to basics. Reg Anesth Pain Med. 2018;43(4):341–346. doi: 10.1097/AAP.0000000000000750 [DOI] [PubMed] [Google Scholar]
- 8.Hamilton DL, Manickam BP. Is the erector spinae plane (ESP) block a sheath block. Anaesthesia. 2017;72(7):915–916. doi: 10.1111/anae.13912 [DOI] [PubMed] [Google Scholar]
- 9.Finneran JJ 4th, Gabriel RA, Khatibi B. Erector spinae plane blocks provide analgesia for breast and axillary surgery: a series of 3 cases. Reg Anesth Pain Med. 2018;43(1):101–102. doi: 10.1097/AAP.0000000000000695 [DOI] [PubMed] [Google Scholar]
- 10.Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. Reg Anesth Pain Med. 2017;42(3):372–376. doi: 10.1097/AAP.0000000000000581 [DOI] [PubMed] [Google Scholar]
- 11.Melvin JP, Schrot RJ, Chu GM, Chin KJ. Low thoracic erector spinae plane block for perioperative analgesia in lumbosacral spine surgery: a case series. Can J Anaesth. 2018;65(9):1057–1065. [DOI] [PubMed] [Google Scholar]
- 12.Celik M, Tulgar S, Ahiskalioglu A, Alper F. Is high volume lumbar erector spinae plane block an alternative to transforaminal epidural injection? Evaluation with MRI. Reg Anesth Pain Med. 2019;44(9):906–907. doi: 10.1136/rapm-2019-100514 [DOI] [PubMed] [Google Scholar]
- 13.Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanism of action of erector spinae blockade. Reg Anesth Pain Med. 2018;43(6):567–571. doi: 10.1097/AAP.0000000000000789 [DOI] [PubMed] [Google Scholar]
- 14.Tseng V, Xu JL. Erector spinae plane block for postoperative analgesia in lumbar spine surgery: is there a better option. J Neurosurg Anesthesiol. 2019. doi: 10.1097/ANA.0000000000000631 [DOI] [PubMed] [Google Scholar]
- 15.Canturk M. Ultrasound-guided bilateral lumbar erector spinae plane block for postoperative analgesia after spondylolisthesis correction surgery. J Clin Anesth. 2019;57:77–78. doi: 10.1016/j.jclinane.2019.03.015 [DOI] [PubMed] [Google Scholar]
- 16.De Lara Gonzalez S, Basora MM, Tio M, Martinez-Camacho A, Fuster S, Sala-Blanch X. L4 erector spinal plane block after lumbar spine arthrodesi: a case-series. Rev Esp Anestesiol Reanim. 2019;66(10):537–542. [DOI] [PubMed] [Google Scholar]
- 17.Singh S, Chaudhary NK. Bilateral ultasound guided erector spinae plane block for postoperative pain management in lumbar spine surgery: a case series. J Neurosurg Anesthesiol. 2019;31(3):354. doi: 10.1097/ANA.0000000000000518 [DOI] [PubMed] [Google Scholar]
- 18.Almeida CR, Oliveira AR, Cunha P. Continuous bilateral erector of spine plane block at T8 for extensive lumbar spine fusion surgery: case report. Pain Pract. 2019;19(5):536–540. doi: 10.1111/papr.12774 [DOI] [PubMed] [Google Scholar]
- 19.Singh S, Choudhary NK, Lalin D, Verma VK. Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: a randomized control trial. J Neurosurg Anesthesiol. 2019. [DOI] [PubMed] [Google Scholar]
- 20.Ueshima H, Inagaki M, Toyone T, Otake H. Efficacy of the erector spinae plane block for lumbar spinal surgery: a retrospective study. Asian Spine J. 2019;13(2):254–257. doi: 10.31616/asj.2018.0114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yayik AM, Cesur S, Ozturk F, et al. Postoperative analgesic efficacy of the ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal decompression surgery: a randomized controlled study. World Neurosurg. 2019;126:e779–e785. doi: 10.1016/j.wneu.2019.02.149 [DOI] [PubMed] [Google Scholar]
- 22.Brandao J, Graca R, Sa M, Cardoso JM, Caramelo S, Correia C. Lumbar erector spinae plane block: successful control of acute pain after lumbar spine surgery - a clinical report. Rev Esp Anestesiol Reanim. 2019;66(3):167–171. doi: 10.1016/j.redar.2018.10.005 [DOI] [PubMed] [Google Scholar]
- 23.Calandese F, Adduci A. Erector spinae plane block for acute postoperative pain management after anterior thoracolumbar spine surgery. J Clin Anesth. 2019;52:55–56. doi: 10.1016/j.jclinane.2018.08.014 [DOI] [PubMed] [Google Scholar]
- 24.Cesur S, Yayik AM, Ozturk F, Ahiskalioglu A. Ultrasound-guided low thoracic erector spinae plane block for effective postoperative analgesia after lumbar surgery: report of five cases. Cureus. 2018;10(11):e3603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waldrop R, Cheng J, Devin C, McGirt M, Fehlings M, Berven S. The burden of spinal disorders in the elderly. Neurosurgery. 2015;77(Suppl 4):S46–S50. doi: 10.1227/NEU.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 26.Graffigna G, Barello S. Patient Health Engagement (PHE) model in enhanced recovery after surgery (ERAS): monitoring patients’ engagement and psychological resilience in minimally invasive thoracic surgery. J Thorac Dis. 2018;10(Suppl 4):S517–S528. doi: 10.21037/jtd.2017.12.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Cassai A, Bonvicini D, Correale C, Sandei L, Tulgar S, Tonetti T. Erector spinae plane block: a systematic qualitative review. Minerva Anestesiol. 2019;85(3):308–319. doi: 10.23736/S0375-9393.18.13341-4 [DOI] [PubMed] [Google Scholar]
- 28.Perlas A, Chaparro LE, Chin KJ. Lumbar neuraxial ultrasound for spinal and epidural anesthesia: a systematic review and meta-analysis. Reg Anesth Pain Med. 2016;41(2):251–260. doi: 10.1097/AAP.0000000000000184 [DOI] [PubMed] [Google Scholar]
- 29.Xu JL. Paraneuraxial nerve blocks: a well-defined novel terminology that is clinically essential for regional anesthesia. J Clin Anesth. 2017;43:14. doi: 10.1016/j.jclinane.2017.09.002 [DOI] [PubMed] [Google Scholar]
- 30.Tseng V, Tara A, Hou J, Xu JL. Erector spinae plane block unbound: limits to safety in a patient with laminectomy. Saudi J Anaesth. 2019;13(3):253–254. doi: 10.4103/sja.SJA_186_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gurkan Y, Aksu C, Kus A, Yorukoglu UH. Erector spinae plane block and thoracic paravertebral block for breast surgery compared to IV-morphine: a randomized controlled trial. J Clin Anesth. 2019;59:84–88. doi: 10.1016/j.jclinane.2019.06.036 [DOI] [PubMed] [Google Scholar]
- 32.Tsui BC, Fonseca A, Munshey F, McFadyen G, Caruso TJ. The erector spinae plane (ESP) block: a pooled review of 242 cases. J Clin Anesth. 2019;53:29–34. doi: 10.1016/j.jclinane.2018.09.036 [DOI] [PubMed] [Google Scholar]
- 33.Bianconi M, Ferraro L, Ricci R, et al. The pharmacokinetics and efficacy of ropivacaine continuous wound instillation after spine fusion surgery. Anesth Analg. 2004;98(1):166–172. doi: 10.1213/01.ANE.0000093310.47375.44 [DOI] [PubMed] [Google Scholar]
- 34.Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a cochrane systematic review and meta-analysis. Br J Anaesth. 2013;111(5):711–720. doi: 10.1093/bja/aet213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tulgar S, Yildirim A, Karaoglan A, Ozer Z. Erector spinae plane block as the main anesthetic method for peri-paravertebral area surgical procedure. J Clin Anesth. 2019;54:157. doi: 10.1016/j.jclinane.2018.12.011 [DOI] [PubMed] [Google Scholar]
- 36.Fiorelli S, Leopizzi G, Saltelli G, et al. Bilateral ultrasound-guided erector spinae plane block for postoperative pain management in surgical repair of pectus excavatum via Ravitch technique. J Clin Anesth. 2019;56:28–29. doi: 10.1016/j.jclinane.2019.01.026 [DOI] [PubMed] [Google Scholar]
- 37.Breebaart MB, Van Aken D, De Fré O, et al. A prospective randomized double-blind trial of the efficacy of a bilateral lumbar erector spinae block on the 24h morphine consumption after posterior lumbar inter-body fusion surgery. Trials. 2019;20(1):441. doi: 10.1186/s13063-019-3541-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eisenstein TK. Opioids and the immune system: what is their mechanism of action. Br J Pharmacol. 2011;164(7):1826–1828. doi: 10.1111/j.1476-5381.2011.01513.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cronin-Fenton DP, Heide-Jorgensen U, Ahern TP, et al. Opioids and breast cancer recurrence: a Danish population-based cohort study. Cancer. 2015;121(19):3507–3514. doi: 10.1002/cncr.29532 [DOI] [PMC free article] [PubMed] [Google Scholar]