Abstract
Objectives
Reduced strength and girth in thigh muscles such as the quadriceps and the hamstrings have been observed in patients with knee osteoarthritis (OA). However, studies on the characteristics of calf muscles in these patients are lacking. This study aimed to evaluate the girth, strength, and flexibility of the calf muscle of patients with knee OA.
Methods
In this case–control study, we recruited 15 patients with knee OA and 15 healthy control participants. The girth, strength, and flexibility of the calf muscle were evaluated in one session using a flexible non-elastic tape measure (centimetre), a handheld dynamometer (Newton), and a standard goniometer (degree) to measure ankle dorsiflexion.
Results
Strength of the calf muscle strength was significantly lower in the patients with knee OA comapred with the control group (−42.03; 95% CI: −73.9, −10.1; p = .012). No significant differences in calf muscle girth (.27; 95% CI: −2.63, 3.16; p = .852) or flexibility (−1.93; 95% CI: −4.8, .93; p = .177) were found between the two groups.
Conclusion
In our study, patients with knee OA demonstrated reduced calf muscle strength. We recommend that the management of patients with knee OA include strengthening the calf muscles.
Keywords: Arthritis, Calf muscles, Muscle girth, Muscle strength, Musculoskeletal
Highlights
-
•
Patients with knee OA did not have reduced girth or flexibility in the calf muscle.
-
•
Patients with knee OA may demonstrate weakness in the calf muscle.
-
•
Calf muscle strength should be included in the management of patients with knee OA.
الملخص
أهداف البحث
خشونة الركبة (الفصال العظمي) أحد أمراض الجهاز العضلي الهيكلي الأكثر شيوعا. يعتبر الألم والقصور الوظيفي من أهم وأكثر الأعراض المصاحبة لهذا المرض. أثبتت الدراسات وجود ضعف وقصور في عضلات الفخذ الأمامية والخلفية في هذه الشريحة من المرضى. في المقابل، الدراسات على خصائص عضلة الساق لدى هؤلاء المرضى مازالت غير متوفرة. الهدف من هذا البحث هو قياس حجم ومرونة وقوة عضلة الساق عند مرضى خشونة الركبة ومقارنتهم بمجموعة من الأصحاء.
طرق البحث
تصميم الدراسة هو دراسة مقترنة لحالات ضابطة. شارك في هذه الدراسة ١٥ مريضـا بخشونة الركبة و١٥ من المتطوعين الأصحاء (المجموعة الضابطة). تم قياس قوة عضلة الساق، ومرونتها، وحجمها هي ما في هذه الدراسة. قياس حجم عضلة الساق كان باستخدام شريط غير مرن لقياس محيط العضلة، وقوة عضلة الساق باستخدام جهاز قياس قوة العضلات، ومرونة العضلة عن طريق قياس المدى الحركي لمفصل الكاحل.
النتائج
وُجد ضعف في قوة عضلة الساق لمرضى خشونة الركبة مقارنة بمجموعة الأصحاء. ولم يوجد فرق في مرونة عضلة الساق أو حجمها بين المجموعتين.
الاستنتاجات
تبين من هذه الدراسة وجود ضعف ملحوظ في قوة عضلة الساق لدى مرضى خشونة الركبة مقارنة بمجموعة الأصحاء، وبذلك نوصي بالأخذ في الاعتبار قوة عضلة الساق أثناء تقييم وعلاج مرضى خشونة الركبة.
الكلمات المفتاحية: التهاب المفاصل, عضلات الساق, حجم العضلة, قوة العضلة, العضلي الهيكلي
Introduction
Osteoarthritis (OA) is the most common type of arthritis and is characterized by inflammation of and degenerative changes to joint tissues.1 As part of the Global Burden of Disease 2010 study, an extended report by Cross and colleagues2 estimated the burden of hip and knee OA worldwide. Hip and knee OA was ranked as the 11th highest contributor to disability worldwide and the 38th highest in disability-adjusted life years. Years lived with disability because of hip and knee OA increased from 10.5 million in 1990 to 17.1 million in 2010.2 Knee OA is more common than hip OA. The prevalence of symptomatic knee OA worldwide in 2010 was 3.8% and was higher in women than in men. In the same year, the prevalence was highest in the Asia Pacific region, followed by Oceania and North Africa/Middle East.2 In the USA, the prevalence of knee OA in adults was estimated to be 33.7% (12.4 million).3 The cross-sectional study of Al-Arfaj and Al-Boukai4 reported that 53.3% of men and 60.9% of women in KSA had radiographic knee OA.
Osteoarthritis not only affects physical health, but it may also negatively impact mental health, increase the risk for cardiovascular disease, cause the consumption of more resources, and incur higher costs.5 Several clinical practice guidelines recommend numerous surgical, pharmacological, and nonpharmacological interventions for patients with knee OA. These treatments include, but are not limited to, total knee arthroplasty,6 acetaminophen (paracetamol), nonsteroidal anti-inflammatory drugs, biomechanical interventions, corticosteroids, self-management, education, and muscle-strengthening training.7, 8, 9, 10
Muscle strength and flexibility can reduce pain and disability, improve and maintain the range of motion (ROM) and physical function of a joint, and enhance postural stability and balance.11 Studies have investigated the strength,12 flexibility,13, 14, 15 and girth16, 17, 18 of the muscles that act on the knee, namely, hip abductors and adductors, quadriceps, and hamstrings, in patients with knee OA. However, investigations of the characteristics of the calf muscle in patients with knee OA are scarce.
The calf muscle is an important group of muscles, consisting of the gastrocnemius, soleus, and plantaris muscles, in the knee joint. Anatomically, the calf muscle, particularly the gastrocnemius, and the quadriceps and hamstrings attach to the knee bone.19 Functionally, the calf muscle assists in knee flexion19 and is one of the most important muscles used in the activities of daily living like walking and running.19,20 Only a few studies have investigated the flexibility of the gastrocnemius muscle in patients with knee OA.13,21 Our literature review found that research on calf muscle strength and girth in patients with knee OA is lacking. Therefore, we asked the following question: Are the calf muscle girth, strength, and flexibility different between patients with knee OA and healthy controls? The null hypothesis was that there is no difference. The primary aim of our study was to evaluate calf muscle girth, strength, and flexibility in patients with knee OA and a secondary aim was to investigate any correlations between calf muscle girth, strength, and flexibility. Our study is the first of its kind and will provide greater insight into any deficits or impairments of the calf muscle.
Materials and Methods
This case–control study was conducted in the Department of Physical Therapy, King Fahad Central Hospital in Jazan, KSA.
Sample size calculation
The sample size for our study was calculated using open source software from the University of British Columbia (http://www.stat.ubc.ca/∼rollin/stats/ssize/n2.html). The calculations were based on data from a previous study that measured the strength of the quadriceps in patients with knee OA using a handheld dynamometer (HHD).22 The following data were used for our calculation: mean strength of 30.1 N in patients with knee OA and 39.7 N in control patients, standard deviation of 8.35, α (alpha) of .05, and power of .80. The calculation yielded a sample size of 24 participants, which was increased 20% to account for potential dropouts. Thus, the total number of participants was 30.
Participants
A convenience sample was used to recruit the participants. Patients were evaluated by an orthopaedic physician using the criteria for knee OA established by the American College of Rheumatology.23 These patients were enrolled if they were an adult, had unilateral knee OA (the more painful knee was studied if the patient had bilateral OA),24 and a Kellgren–Lawrence25 (K-L) grade ≥ 2. Patients were excluded if they had a pathology such as rheumatoid arthritis or neurological impairment24,26,27 or had had lower-limb surgery, arthroplasty,24 amputation,26 or rupture or trauma of the calf muscle. Healthy participants, who had no history of knee OA, were recruited to match patients with knee OA with respect to gender, age, and body mass index (BMI).26
Procedure
The procedure of the study was explained to the participants. The participants then attended a testing session and were asked to sign an informed consent form. Data were collected using a data collection sheet designed by the principal investigator. Height and weight were measured using a mechanical beam scale (402LB, Health O Meter, McCook, IL, USA) and the girth, strength, and flexibility of the calf muscle were assessed (see below). The affected leg of the patients with knee OA and the matching leg of the control participants were examined. If a patient had bilateral knee OA, the knee with more severe symptoms according to a numeric pain rating scale (NPRS) was examined. The entire session lasted for approximately 1 h.
All participants had the girth, strength, and flexibility of their calf muscle measured in that order. Calf muscle girth was measured using a 1.5-m non-elastic fiberglass cloth tape measure (TT-SR26, China Eastern Tape Measure Manufacturer Co., Ltd., Ningbo City, Zhejiang, China). This tape measure does not tear or stretch easily and is used mainly to measure length and girth. A tape measure is a valid and reliable tool for measuring muscle girth.28 Each participant was asked to sit on a chair and relax with both feet on the floor. The tape measure was placed around the calf at the point of greatest girth without compressing the subcutaneous tissue. The average of 3 girth measurements was used for analysis.29
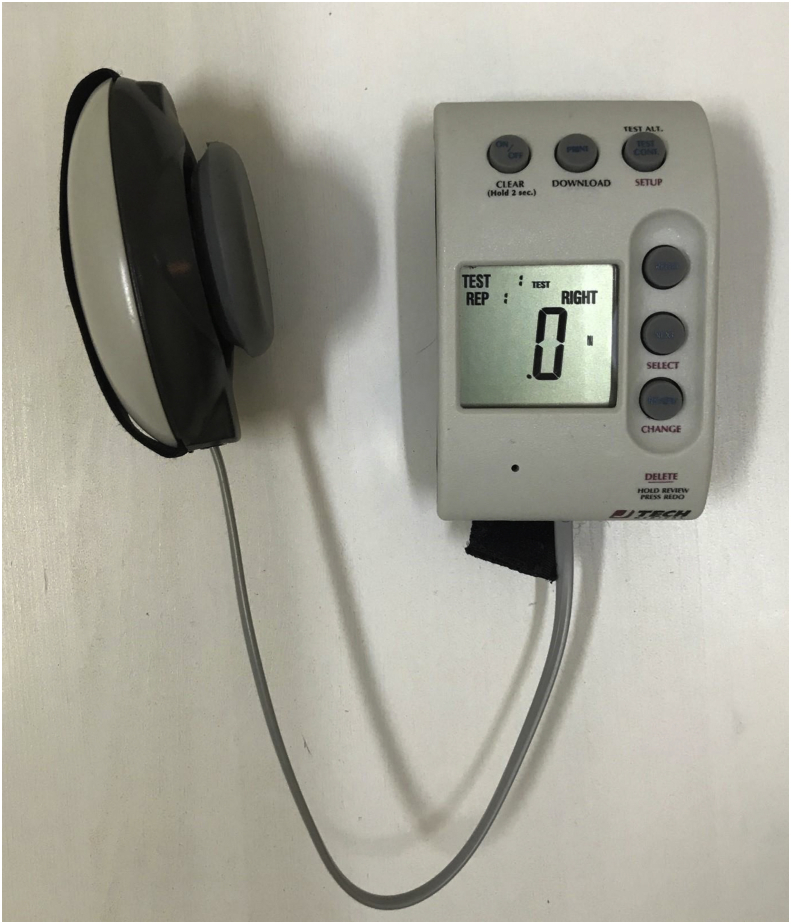
An HHD (JT-AA104, PowerTrack MMT; JTECH Medical Industries, Midvale, UT, USA) was used to measure the isometric strength of the calf muscle (Figure 1). An HHD is a highly reliable and valid instrument for assessing the isometric strength and power of the lower-limb muscle.30,31 Each participant was instructed to lie supine on a plinth with the hips and ankles in neutral positions and the knees extended. The HHD was placed on the metatarsal heads at the sole of the foot while the participant held the sides of the plinth for stability. The participant was instructed to maximally contract the calf muscle while the therapist resisted the movement (isometric contraction). The protocol of a previous study was followed.30 The average value from 3 tests was used for analysis.
Figure 1.
Digital handheld dynamometer used to measure calf muscle strength.
A standard goniometer (EZ Read Jamar Goniometer, Model 7541; Patterson Medical, Warrenville, IL, USA) was used to measure the range of motion (ROM) of ankle dorsiflexion as an indicator of the flexibility of the gastrocnemius muscle. The method has demonstrated good validity and reliability.32 Each participant was asked to lean on the wall with both feet 60 cm away from the wall. Then, the test leg was moved backward to be about a foot behind the other leg. The participant then maximally dorsiflexed the ankle while keeping the knee extended and the heel on the floor. The axis of the goniometer was placed posterior to the distal fibula, with the stationary arm parallel to the lateral aspect of the foot and the moving arm pointed to the proximal head of the fibula.32 Repeated dorsiflexion could affect perception of the end point of the gastrocnemius stretch, which could lead to increased ankle dorsiflexion and consequently affect the overall result. Therefore, only one dorsiflexion was performed and its measurement used for analysis.33
Statistical analysis
The data were analysed using SPSS Statistics for Windows ver. 20.0 (IBM, Armonk, NY, USA). Quantitative variables were described via the mean and standard deviation (SD) calculated using descriptive statistics. The Kolmogorov–Simonov test was used to evaluate the normality of the data distribution (p > .05). Independent t tests were used to investigate the differences between the demographic data of the groups at baseline and the differences in the outcome measures, namely, calf muscle girth, strength, and flexibility. The effect sizes were calculated using Cohen's d equation and the data from the independent t tests of the outcome measures. The ranges of the effect size were .20–.49 (small), .50–.79 (moderate), and ≥.80 (large).34 The categorical data were analysed using χ2 tests. The correlation between the outcome measures was determined using intraclass correlation coefficients (ICCs) with two-way mixed effects, consistency, and multiple raters or measurements. The criterion for statistical significance was set at p < .05 with a 95% confidence interval (CI).
Results
No significant differences between patients with knee OA and control participants with respect to all baseline demographic data were noted, which may indicate that the groups were homogenous (Table 1).
Table 1.
Characteristics of the participants in both groups at baseline.
| Variable | Knee OA group (n = 15) | Control group (n = 15) | Significance |
|---|---|---|---|
| Male/Female | 9/6 | 9/6 | χ2 = .000; p = 1.00 |
| Age (years) | 58 ± 11 | 58 ± 11 | t = .000; p = 1.00 |
| BMI (kg/cm2) | 32.1 ± 4.2 | 32.0 ± 4.2 | t = .047; p = .963 |
| Duration of symptoms (months) | 6.0 ± 6.9 | – | |
| NPRS | 7.2 ± 2.0 | – | |
| Affected knee side (right/left) | 6/9 | – | |
| K&L OA grade (2/3/4) | 6/1/8 | – |
BMI: body mass index; NPRS: Numeric Pain Rating Scale; K&L: Kellgren and Lawrence grading system; OA: osteoarthritis.
Values are expressed as mean ± SD (standard deviation), except where otherwise indicated.
Interestingly, an independent t test revealed a significant difference in calf muscle strength between the knee OA group and the control group (−42.0; 95% CI: −74.7, −9.4; p = .014). On the other hand, no significant differences were found in calf muscle girth or flexibility between the groups (p > .05) (Table 2).
Table 2.
Measurements of calf muscle girth, strength, and flexibility in both groups.
| Outcomes | Knee OA group (n = 15) | Control group (n = 15) | Levene's test | Between-group differences |
|||
|---|---|---|---|---|---|---|---|
| Mean difference (95% CI) | Cohen's d | t test | p value | ||||
| Girth (cm) | 39.6 ± 4.2 | 39.3 ± 3.5 | F1,28 = .008, p = .931 | .3 (−2.6, 3.2) | .04 | .189 | .852 |
| Strength (N) | 123.4 ± 23.4 | 165.4 ± 55.6 | F1,19 = 4.2, p = .05 | −42.0 (−73.9, −10.1) | −.44 | −2.697 | ∗.014 |
| Flexibility (ankle DF [°]) | 13.2 ± 3.8 | 15.1 ± 3.9 | F1,28 = .093, p = .762 | −1.9 (−4.8, 1.0) | −.24 | −1.383 | .177 |
CI: confidence interval, DF: dorsiflexion.
∗ indicates significant difference.
Values are expressed as mean ± SD.
The ICCs demonstrated no correlation between any of the outcome measures (calf muscle girth, strength, and flexibility) (Table 3).
Table 3.
Correlation between calf muscle girth, strength, and flexibility for the knee OA group (n = 15) and the control group (n = 15).
| Group/Outcome | ICC(3,2) | 95% CI | p value |
|---|---|---|---|
| Knee OA group: | |||
| Strength vs girth | −.242 | −2.698, .583 | .654 |
| Strength vs flexibility | .159 | −1.506, .718 | .376 |
| Girth vs flexibility | .168 | −1.477, .721 | .367 |
| Control group: | |||
| Strength vs girth | .006 | −1.960, .666 | .495 |
| Strength vs flexibility | −.048 | −2.121, .648 | .534 |
| Girth vs flexibility | −.254 | −2.736, .579 | .661 |
ICC: intraclass correlation coefficient, CI: confidence interval.
Discussion
Our study found that calf muscle strength was significantly reduced in the patients with knee OA compared with that in the healthy control participants. However, no statistically significant difference was detected in calf muscle girth and flexibility between the two groups.
No studies have evaluated calf muscle strength and girth in patients with knee OA. Instead, other muscles were investigated and demonstrated weakness. In a systematic review, Alnahdi et al.12 found that the strength of the hip muscles, hamstrings, and quadriceps was significantly reduced in patients with knee OA. Calf muscle strength was quantified for musculoskeletal conditions other than knee OA. For instance, Bell et al.35 observed a significant reduction in calf muscle strength as measured by an HHD in patients with “medial knee displacement”. Moreover, Carroll et al.36 investigated and compared the strength of the foot and ankle muscles in patients with rheumatoid arthritis with that of matched controls and observed a significant reduction in plantar flexion strength in the patients.
Our study did not investigate the cause–effect relationship. Thus, the observed calf muscle weakness could be a causative factor or a complication of knee OA. Calf muscle weakness in patients with knee OA may be partly explained by the anatomical and functional relationships between the calf muscle and the knee joint. In our study, plantar flexion strength was tested with the knee fully extended, which greatly involves the gastrocnemius muscle. Lloyd and colleagues37 reported that the gastrocnemius muscle dynamically stabilizes the knee because it originates in the femoral condyles. A recent review reported that the gastrocnemius muscle has a key role in the anterior-posterior stability of the knee joint.38
Our results demonstrated that there was no significant difference in the flexibility of the calf muscle between the two groups. This agrees with the finding of a previous study13 but is inconsistent with that of another study21 that investigated the flexibility of the gastrocnemius muscle in addition to other muscles. The normal ROM of ankle dorsiflexion is approximately 20°.39 In our study, ankle dorsiflexion was 13° in the patients with knee OA and 15° in the controls. These values are similar to those in Shiraz et al.13 (patients: ∼8.5°, controls: ∼10.5°) and lower than those in Jyoti et al.21 (patients: ∼20.0°, controls: ∼29.0°). The high age and BMI of our participants may have contributed to the low ROM of ankle dorsiflexion.15 The flexibility of the quadriceps and hamstrings in patients with knee OA was also affected.13,14 Knee OA causes patients to limit their activity level, resulting in an overall reduction in flexibility. Further studies are needed to better understand the effect of reduced ROM of ankle dorsiflexion in patients with knee OA.
Our findings revealed no significant difference in calf muscle girth between the two groups. We chose to study calf muscle girth because it is a likely clinical indicator of muscle atrophy. Our literature search found no studies on calf muscle girth in patients with knee OA. Therefore, our findings may be discussed along with the findings of calf muscle girth in conditions other than knee OA28 and with the results of studies on thigh muscles.16, 17, 18 Ross et al.28 found a significant reduction in calf muscle girth in patients who required knee arthroscopic surgery after a unilateral knee injury. On the other hand, other studies examined thigh girth in patients with knee OA and observed no significant difference between patients and control participants.17,18 The difference between the findings of the calf muscle study and the thigh muscle studies may be partly attributed to the differences between the characteristics of the participants, the designs and methodologies used, and the characteristics of the muscles. Gur and Cakin17 concluded that loss of muscle strength after development of knee OA was not explained by quantitative changes in muscle mass. This may partly explain why we did not observe a reduction in calf muscle girth with the reduction in strength.
One limitation of our study is that the investigators were not blinded to which group the participants were assigned. This may have caused unintentional bias when performing the outcome measurements. However, this bias would have been limited with respect to the measurement of calf muscle strength because the investigators were blinded to the HHD values from the maximal voluntary contraction performed during the test. Another limitation was that the investigator had to hold the HHD to resist the force generated by the participant.31 Inadequate force and stabilization by the investigator could have affected the results. Even if the investigator braced against a wall, the assessment of the ankle plantar flexors of strong participants may not have been accurate. However, this protocol is the gold standard for measuring ankle plantar flexion strength.30,31 Despite these limitations, this study provides important information about the girth and strength of the calf muscle, which will be useful for subsequent studies on the characteristics of the calf muscle in patients with knee OA.
Conclusions
Our study found that calf muscle strength was lower in patients with knee OA compared with that in healthy control participants. There were no significant differences in calf muscle girth or flexibility between the two groups. No correlations were found between calf muscle girth, strength, and flexibility.
Recommendations
Upon our literature review, we conclude that ours is the only study that examined calf muscle girth and strength in patients with knee OA. Therefore, further research is needed to confirm or refute our results. In addition, future studies should investigate the effect of calf muscle strengthening exercises on pain and function in patients with knee OA. Clinicians should consider calf muscle strength during the management of this group of patients.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Ethical approval was obtained from the Institute Review Board of Imam Abdulrahman Bin Faisal University, Dammam, KSA (IRB-PGS-2017-03-178, 1 October 2017). The study was performed with the consideration of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Authors contributions
HAA and AMA conceptualized and designed the study, analysed and interpreted the data, and accounted for all aspects of the research. HAA provided the research materials, collected and organized the data, wrote the initial draft of the manuscript, and provided logistic support. HAA and AMA critically reviewed and approved the final draft of the manuscript. HAA and AMA agreed to be accountable for the accuracy or integrity of all parts of the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgment
The authors thank all those who volunteered their time to participate in this study. The authors also thank Mrs. Leena Hakami for her assistance with data collection and data entry.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Loeser R.F., Goldring S.R., Scanzello C.R., Goldring M.B. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64(6):1697–1707. doi: 10.1002/art.34453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cross M., Smith E., Hoy D., Nolte S., Ackerman I., Fransen M. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence R.C., Felson D.T., Helmick C.G., Arnold L.M., Choi H., Deyo R.A. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Arfaj A., Al-Boukai A.A. Prevalence of radiographic knee osteoarthritis in Saudi Arabia. Clin Rheumatol. 2002;21(2):142–145. doi: 10.1007/s10067-002-8273-8. [DOI] [PubMed] [Google Scholar]
- 5.Vina E.R., Kwoh C.K. Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol. 2018;30(2):160–167. doi: 10.1097/BOR.0000000000000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGrory B.J., Weber K.L., Jevsevar D.S., Sevarino K. Surgical management of osteoarthritis of the knee: evidence-based guideline. J Am Acad Orthop Surg. 2016;24(8):e87–e93. doi: 10.5435/JAAOS-D-16-00159. [DOI] [PubMed] [Google Scholar]
- 7.McAlindon T.E., Bannuru R.R., Sullivan M.C., Arden N.K., Berenbaum F., Bierma-Zeinstra S.M. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(3):363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Jevsevar D.S. Treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg. 2013;21(9):571–576. doi: 10.5435/JAAOS-21-09-571. [DOI] [PubMed] [Google Scholar]
- 9.Fernandes L., Hagen K.B., Bijlsma J.W.J., Andreassen O., Christensen P., Conaghan P.G. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125–1135. doi: 10.1136/annrheumdis-2012-202745. [DOI] [PubMed] [Google Scholar]
- 10.RACGP . 2nd ed. The Royal Australian College of General Practitioners; East Melbourne: 2018. Guideline for the management of knee and hip osteoarthritis. [Google Scholar]
- 11.Garber C.E., Blissmer B., Deschenes M.R., Franklin B.A., Lamonte M.J., Lee I.M. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 12.Alnahdi A.H., Zeni J.A., Snyder-Mackler L. Muscle impairments in patients with knee osteoarthritis. Sport Health. 2012;4(4):284–292. doi: 10.1177/1941738112445726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shirazi S.A., Nezhad F.G., Ebrahimian M., Nouraddini E., Mansoorian A., Emami F. Flexibility of knee Joint muscles in women with knee osteoarthritis and healthy controls. J Rehab Sci Res. 2015;2(3):47–52. [Google Scholar]
- 14.Onigbinde A.T., Akindoyi O., Faremi F.A., Okonji A., Shuaib O., Lanre O.O. An assessment of hamstring flexibility of subjects with knee osteoarthritis and their age matched control. Clin Med Res. 2013;2(6):121–125. [Google Scholar]
- 15.Messier S.P., Loeser R.F., Hoover J.L., Semble E.L., Wise C.M. Osteoarthritis of the knee: effects on gait, strength, and flexibility. Arch Phys Med Rehabil. 1992;73(1):29–36. [PubMed] [Google Scholar]
- 16.Diracoglu D., Baskent A., Yagci I., Ozcakar L., Aydin R. Isokinetic strength measurements in early knee osteoarthritis. Acta Reumatol Port. 2009;34(1):72–77. [PubMed] [Google Scholar]
- 17.Gur H., Cakin N. Muscle mass, isokinetic torque, and functional capacity in women with osteoarthritis of the knee. Arch Phys Med Rehabil. 2003;84(10):1534–1541. doi: 10.1016/s0003-9993(03)00288-0. [DOI] [PubMed] [Google Scholar]
- 18.Emrani A., Bagheri H., Hadian M.R., Jabal-Ameli M., Olyaei G.R., Talebian S. Isokinetic strength and functional status in knee osteoarthritis. J Phys Ther Sci. 2006;18(2):107–114. [Google Scholar]
- 19.Jarmey C. 2nd ed. North Atlantic Books; Berkeley: 2008. The concise book of muscles. [Google Scholar]
- 20.Farr J.N., Going S.B., McKnight P.E., Kasle S., Cussler E.C., Cornett M. Progressive resistance training improves overall physical activity levels in patients with early osteoarthritis of the knee: a randomized controlled trial. Phys Ther. 2010;90(3):356–366. doi: 10.2522/ptj.20090041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jyoti, Joshi S., Yadav V.S. Knee joint muscle flexibility in knee osteoarthritis patients and healthy individuals. Int J Health Sci Res. 2019;9(6):156–163. [Google Scholar]
- 22.Lewek M.D., Rudolph K.S., Snyder-Mackler L. Quadriceps femoris muscle weakness and activation failure in patients with symptomatic knee osteoarthritis. J Orthop Res. 2004;22(1):110–115. doi: 10.1016/S0736-0266(03)00154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Altman R.D. The classification of osteoarthritis. J Rheumatol Suppl. 1995;43:42–43. [PubMed] [Google Scholar]
- 24.Berger M.J., McKenzie C.A., Chess D.G., Goela A., Doherty T.J. Sex differences in quadriceps strength in OA. Int J Sports Med. 2012;33(11):926–933. doi: 10.1055/s-0032-1311587. [DOI] [PubMed] [Google Scholar]
- 25.Kohn M.D., Sassoon A.A., Fernando N.D. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886–1893. doi: 10.1007/s11999-016-4732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Costa R.A., Oliveira L.M., Watanabe S.H., Jones A., Natour J. Isokinetic assessment of the hip muscles in patients with osteoarthritis of the knee. Clinics (Sao Paulo, Brazil) 2010;65(12):1253–1259. doi: 10.1590/S1807-59322010001200006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu Q., Li J., Fang M., Gong L., Sun W., Zhou N. Effect of Chinese massage (Tui Na) on isokinetic muscle strength in patients with knee osteoarthritis. J Tradit Chin Med. 2016;36(3):314–320. doi: 10.1016/s0254-6272(16)30043-7. [DOI] [PubMed] [Google Scholar]
- 28.Ross M., Worrell T.W. Thigh and calf girth following knee injury and surgery. J Orthop Sports Phys Ther. 1998;27(1):9–15. doi: 10.2519/jospt.1998.27.1.9. [DOI] [PubMed] [Google Scholar]
- 29.Perez-Zepeda M.U., Gutierrez-Robledo L.M. Calf circumference predicts mobility disability: a secondary analysis of the Mexican health and ageing study. Eur Geriatr Med. 2016;7(3):262–266. doi: 10.1016/j.eurger.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mentiplay B.F., Perraton L.G., Bower K.J., Adair B., Pua Y.H., Williams G.P. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: a reliability and validity study. PloS One. 2015;10(10) doi: 10.1371/journal.pone.0140822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spink M.J., Fotoohabadi M.R., Menz H.B. Foot and ankle strength assessment using hand-held dynamometry: reliability and age-related differences. Gerontology. 2010;56(6):525–532. doi: 10.1159/000264655. [DOI] [PubMed] [Google Scholar]
- 32.Witvrouw E., Danneels L., Asselman P., D'Have T., Cambier D. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players. A prospective study. Am J Sports Med. 2003;31(1):41–46. doi: 10.1177/03635465030310011801. [DOI] [PubMed] [Google Scholar]
- 33.McKechnie G.J., Young W.B., Behm D.G. Acute effects of two massage techniques on ankle joint flexibility and power of the plantar flexors. J Sports Sci Med. 2007;6(4):498–504. [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen J. 2nd ed. Routledge; Hillsdale: 1988. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 35.Bell D.R., Padua D.A., Clark M.A. Muscle strength and flexibility characteristics of people displaying excessive medial knee displacement. Arch Phys Med Rehabil. 2008;89(7):1323–1328. doi: 10.1016/j.apmr.2007.11.048. [DOI] [PubMed] [Google Scholar]
- 36.Carroll M., Joyce W., Brenton-Rule A., Dalbeth N., Rome K. Assessment of foot and ankle muscle strength using hand held dynamometry in patients with established rheumatoid arthritis. J Foot Ankle Res. 2013;6(1):10. doi: 10.1186/1757-1146-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lloyd D.G., Buchanan T.S. Strategies of muscular support of varus and valgus isometric loads at the human knee. J Biomech. 2001;34(10):1257–1267. doi: 10.1016/s0021-9290(01)00095-1. [DOI] [PubMed] [Google Scholar]
- 38.Abulhasan J., Grey M. Anatomy and physiology of knee stability. J Funct Morphol Kinesiol. 2017;2(4):34. [Google Scholar]
- 39.Magee D.J. 6th ed. Saunders; St. Louis: 2014. Orthopedic physical assessment. [Google Scholar]