Abstract
Objective:
To compare two kinds of metal markers for preoperative localization of ground glass nodules (GGNs).
Methods:
We retrospectively investigated data from 198 cases of GGN localization and compared the success rate and complications of both approaches.
Results:
In the hook wire and coil groups, the success rates of CT-guided localization for GGNs were 99.2 and 98.7%, respectively (p = 1.000). The success rates of video-assisted thoracoscopic surgery in both groups were 100% without transthoracic surgery. The post-localization complication rates in the hook wire group and coil group were 36.9 and 32.9% (p = 0.568), and the postoperative complication rates in the hook wire and coil groups were 13.9 and 11.8%, respectively (p = 0.672).
Conclusions:
Preoperative localization of GGNs with both hook wire and coil methods proved to be useful and effective. Both methods have acceptable preoperative and postoperative complication rates, but the localization and operation times were shorter for the hook wire group than the coil group.
Advances in knowledge:
Most of previous articles studied a single preoperative localization method. Few studies have compared the preoperative and postoperative methods for metal markers. This paper compared two preoperative localization methods for GGNs to provide clinical guidance.
Introduction
With the popularization of low-dose CT, solitary peripheral pulmonary nodules (nodule diameter <1 cm) are increasingly detected,1 especially ground glass nodules (GGNs). Because of the malignant probability of GGNs,2,3 the diagnosis and treatment of pulmonary nodules have become clinical focuses. Video-assisted thoracoscopic surgery (VATS) provides a new minimally invasive approach to diagnosis and treatment of pulmonary nodules.4 However, nodule localization before VATS is still limited because lung GGNs found on CT are usually invisible or imperceptible at surgery.5 To accurately locate small pulmonary nodules as soon as possible, maximize tumor removal, and protect lung function, preoperative nodular localization is considered a safe and reliable method and has a high success rate.6
Several preoperative localization methods for nodules have been reported, including hook wires,7 99mTechnetium,8 methylene blue,9 hydrogel plugs,10 and coils.11 Among these methods, hook wire which was first reported by Mack in 1992 is the most commonly used with 96% success rate in guiding CT localization.6,12 The coil is another localization method with a very high localization success rate.13 Postoperative complications include pneumothorax, pulmonary hemorrhage, and dislodgement or migration. Few articles have compared the two methods, and there is no consensus on which one is superior. The purpose of this study was to compare the safety and feasibility of the hook wire and coil methods by comparison of their success rates and complications rates.
Methods and materials
Participants
This was a retrospective study of data from 198 cases of preoperative localization and wedge resection under VATS from 2014 to 2018. The inclusion criteria were as follows: single GGN with suspected malignant signs (such as increased density and diameter of the GGN, the presence of lobulated or spiculated margin, and pleural indentation et al) resected after CT localization with hook wire or coil by VATS. The exclusion criteria were as follows: multiple nodules, attachment of bronchi or blood vessels to the nodule, distance from the pleura >40 mm or <5 mm, obvious multiple metastatic nodules, and more than two nodules located and/or operated on at the same time.
Variables
The main evaluation objectives were success rates of the positioning and operation. The secondary outcomes were localization complications, postoperative complications, positioning time, operating time, postoperative extubation time, and hospitalization time. Localization success was defined as CT-guided hook wire or coil location in the GGN or within 1 cm. The positioning success rate was the ratio of the number of successes (minus the number of dislodgements) to the total number of positionings in each group. Surgical success was defined by the complete removal of the nodule under VATS that did not require a thoracotomy. The time from entering to leaving the operating room was defined as the time of surgery. The surgical success rate was estimated as the ratio of VATS successes (minus those switched to thoracotomy) to the number of surgical procedures in each group. Extubation time was the time from pleural drainage tube insertion to removal. A major complication was defined as the need for a second thoracotomy, and minor complications were those did not require a second thoracotomy.
CT-guided localization process
A radiologist was accompanied by a thoracic surgeon to locate a hook wire (20 g × 120 mm; Pajunk, Germany) or coil (imwce-35-5-5, diameter: 5 mm, 0.035 inch diameter, 5 cm; Cook Medical, USA) under preoperative CT guidance. The choice of metal marker for the guiding depends on the thoracic surgeon and patients. A 64-row multislice spiral CT (GE Healthcare, USA) was used for the guiding. For the coil localization, the appropriate localization position was determined from the images, and the localization path was selected to avoid blood vessels and bronchi to the greatest possible extent. After local anesthesia, the localization needle was inserted into or around the nodule within 1 cm along the shortest path. After confirming that the needle tip was in the lesion and measuring the distance between the guide tip and pleura and calculating the depth of coil, the spring coil was released through the introducer needle (Figure 1a), and the guide needle was removed. CT scanning was repeated to confirm the exact location of the coil (Figure 1b), and patients were observed for pneumothorax and bleeding. The procedures for hook wire localization were the same as those in the coil group. After the target nodule was confirmed, a reasonable puncture path was selected based on the intraoperative CT image (Figure 2a), then the hook wire needle was inserted around the lesion (Figure 2b). After successful positioning, the patient was placed in the mobile bed and sent to the operating room for VATS.
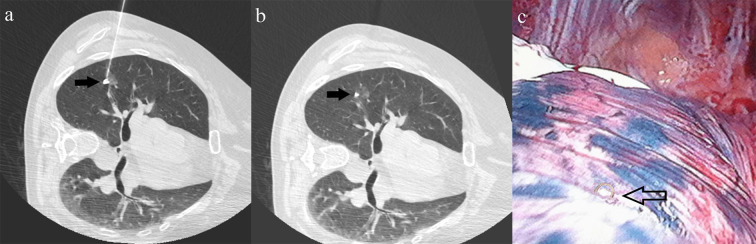
Figure 1.
A 51-year-old female with a GGN in the upper right lobe underwent VATS surgery. (a) The coil was released next to the nodule (black arrow). (b) The postoperative coil was localized in upper right lobe (black arrow). (c) The coil site (black hollow arrow) in the pleura was seen during VATS.
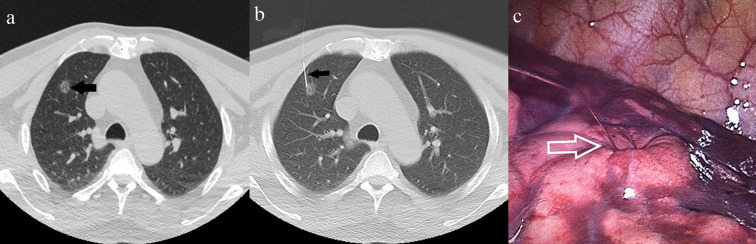
Figure 2.
A GGN was found in the upper right lobe of a 55-year-old female undergoing VATS. (a) The lesion (black arrow) was observed on an axial CT image. (b): A hook wire needle (black arrow) was inserted around the lesion. (c): The end of the hook wire (white hollow arrow) was visualized during VATS.
VATS
All patients underwent VATS within 30 min after localization. The patient was placed in a lateral position for dual-port thoracoscopic surgery under general anesthesia. VATS operation was performed under the guidance of nodule positioning by visualizing the microcoils outside the visceral pleura or the surface ends of the hook wire (Figures 1c and 2c). C-arm fluoroscopy-assisted wedge cutting was performed in the coil group. The resected specimens were submitted to the pathology department for rapid frozen examination to reconfirm that the lesion was completely removed and determine if it was benign or malignant. As lobectomy and lymph node resection are required if the nodule is malignant.
Statistical methods
SPSS software (v.25, IBM, USA) was used for statistical analyses. Continuous variables were analyzed by t-tests, and categorical variables were compared by chi-square, Pearson, and Fisher tests. Differences were considered significant at p < 0.05.
Results
A total of 122 patients in the hook wire group underwent preoperative localization, compared with 76 in the coil group. The maximum nodule diameters in the hook wire and coil groups were 8.28 ± 3.19 mm and 9.58 ± 4.16 mm (p = 0.014), respectively. The shortest distances from the nodules to the pleura were 19.82 ± 8.86 mm and 21.84 ± 10.06 mm, respectively (p = 0.140). There were no significant differences for age, sex, smoking history, or nodule distribution between the two groups. Baseline data for both groups of patients and nodules are presented in Table 1. The success rates of preoperative positioning in the hook wire group and coil group were 99.2 and 98.7% (p = 1.000), respectively. There was no significant difference in the individual or total localization complication rates between the two groups (p > 0.05, see Table 2). There was one case of dislodgement in each group. Pneumothorax complications occurred in 25 patients in the hook wire group and in 11 cases in the coil group (20.5% vs 14.5%). Mild hemorrhage affected 18 and 10 patients in the hook wire and coil groups, respectively (14.8% vs 13.2%). The complications of all cases were resolved without further treatment. The total postlocalization complication rates were 36.9 and 32.9% (hook wire vs coil, p = 0.568). Details of the positioning data can be found in Table 2. All procedures were completed successfully with VATS. The operation time of the coil group was longer than that of the hook wire group (101.84 ± 42.11 vs 87.74±45.36 min, p = 0.030). The chest drain extubation times in the coil and hook wire groups were 5.93 ± 3.32 and 5.69 ± 3.39 days (p = 0.618), respectively, and the durations of hospital stay were 10.34 ± 5.30 and 9.67 ± 4.6 days (p = 0.366). In the hook wire group, 13.9% of patients had postoperative complications (14 cases of air leak, one case of hemothorax, and two cases of chylothorax), compared to 11.8% in the coil group (eight cases of air leak and one case of chylothorax). There was a case of hemothorax who had the second thoracotomy performed in the hook wire group. The cause of the hemothorax was confirmed by the result of the second operation is that the resected nodule was relatively deep, and blood vessels ligated during VATS had ruptured after surgery. The postoperative results are shown in Table 3.
Table 1.
Characteristics of patients and nodules
| Hook wire group (n = 122) |
Coil group (n = 76) |
P value | |
|---|---|---|---|
| Age (years) | 57.47 ± 10.28 | 56.79 ± 10.68 | 0.657 |
| Sex (male/female) | 59/63 | 38/38 | 0.822 |
| Smoke (yes/no) | 27/95 | 12/64 | 0.275 |
| Diameter (mm) | 8.28 ± 3.19 | 9.58 ± 4.16 | 0.014 |
| Distance (mm) | 19.82 ± 8.86 | 21.84 ± 10.06 | 0.140 |
| Location | |||
| Right upper lobe | 48 (39.3%) | 20 (26.3%) | 0.060 |
| Right middle lobe | 7 (5.7%) | 6 (7.9%) | 0.567 |
| Right lower lobe | 28 (23.0%) | 17 (2.4%) | 0.924 |
| Left upper lobe | 23 (18.9%) | 19 (25.0%) | 0.303 |
| Left lower lobe | 16 (13.1%) | 14 (18.4%) | 0.311 |
Table 2.
Results of CT-guided localization by group
| Hook wire group (n = 122) n (%) |
Coil group (n = 76) n (%) |
P value | |
|---|---|---|---|
| Procedure success | 121 (99.2%) | 75 (98.7%) | 1.000 |
| Complications | 45 (36.9%) | 25 (32.9%) | 0.568 |
| Pneumothorax | 25 (20.5%) | 11 (14.5%) | 0.310 |
| Pulmonary hemorrhage | 18 (14.8%) | 10 (13.2%) | 0.685 |
| Both hemorrhage and pneumothorax | 1 (0.8%) | 3 (3.9%) | 0.159 |
| Dislodgement or migration | 1 (0.8%) | 1 (1.3%) | 0.771 |
| Localization position | |||
| Supine | 36 (29.5%) | 25 (32.9%) | 0.616 |
| Prone | 52 (42.6%) | 39 (51.3%) | 0.233 |
| Lateral | 34 (27.9%) | 12 (15.8%) | 0.491 |
| Localization time (min) | 20.45 ± 11.73 | 23.53 ± 6.28 | 0.017 |
Table 3.
Surgical variables after VATS by group
| Hook wire group (n = 122) |
Coil group (n = 77) |
P value | |
|---|---|---|---|
| Successful VATS | 122 (100%) | 77 (100%) | 1.000 |
| Operation time (min) | 87.74 ± 45.36 | 101.84 ± 42.11 | 0.030 |
| Tube removal time (days) | 5.69 ± 3.39 | 5.93 ± 3.32 | 0.618 |
| Duration of hospital stay (days) | 9.67 ± 4.65 | 10.34 ± 5.30 | 0.366 |
| Surgical bleeding (ml) | 36.98 ± 6.93 | 43.95 ± 5.13 | 0.472 |
| Postoperative complications | 17 (13.9%) | 9 (11.8%) | 0.672 |
| Hemothorax | 1 | 0 | |
| Air leak | 14 | 8 | |
| Chylothorax | 2 | 1 |
VATS, video-assisted thoracoscopic surgery.
Postoperative outcomes were as follows: carcinoma in situ (n = 18), microinvasive adenocarcinoma (n = 80), invasive adenocarcinoma (n = 51), dysplasia (n = 14), inflammation (n = 17), hyperplasia (n = 4), hamartoma (n = 1), carbon deposition (n = 2), metastasis (n = 1), squamous cell carcinoma (n = 2), granuloma (n = 1), tuberculosis (n = 5), and aspergillus (n = 1).
Discussion
The purpose of this investigation was to compare two metal materials that are conducive to preoperative GGN localization. Previous studies concluded that both approaches are safe and effective. Here we compared the localization, operation, and complication rates for both methods. The localization success rates of the hook wire and coil groups were 99.2 and 98.7%, respectively, which are similar to previous literature reports of 96 and 97% success rates.6 VATS resection was 100% effective for both groups. There was no statistical difference between groups for localization or total postoperative complications.
The hook wire and coil are the two most commonly used metal makers in preoperative CT localization. Pneumothorax and hemorrhage are the primary localization complications, and migration and dislodgement are the main causes of localization failure. The reported incidence of dislodgement in the literature is 7.5%.6 In this study, one dislodgement occurred in each group, but the lesions were successfully removed based on the hematoma location on the lung tissue surface. In the hook wire group, pneumothorax was the main cause of dislodgement. If pneumothorax formed and progressed, the guide wire in the lung would be pulled by the guide wire fixed on the chest wall, which would easily lead to dislodgement and result in localization failure.14 When the lung was deflated, the wire was more likely to shift relative to the position of the target nodule.15 In the hook wire group, slight pneumothorax occurred during the localization period, and dislodgement was detected when the patient was brought to the operating room. The reported incidence of hook wire dislodgement was 3–20% during patient transportation to the operating room or intraoperatively. In the coil group, coil displacement was also found in the pleura before VATS. The presumed reason was that the distance from the pleura was relatively small due to large respiratory movement after pneumothorax. The lung parenchyma gradually shrank, which increased the possibility that the coil located in the superficial lung parenchyma moved toward the lung surface with less resistance. Patients should therefore be transferred to the operating room for surgery as soon as possible after localization to avoid the risk of dislodgement due to pneumothorax.
Because the coil does not have a hook-like structure for better fixation, operators were inclined to choose a slightly deeper nodule to position the coil to avoid dislodgement. This maybe the reason why the nodule-to-pleural distance was slightly longer in coil group. However, there was no statistical difference between the two methods with regard to nodule size. Although the total complication rates for the two localization methods were not statistically different, it was slightly higher in the hook wire group. Because the wire is hook-shaped and fixed on the chest wall. The tip can damage the surrounding tissue and cause hemorrhage, and the wire fixed on the chest wall was easily affected by respiratory movement causing pneumothorax. This explains why the hook wire group had a high proportion of pneumothorax compared to the coil group, as the coil is not fixed to the chest wall.15,16 The spring coil itself has the structural characteristic of a thrombus fiber coating,11 This can explain why the incidence rates of pneumothorax and hemorrhage in the coil group were lower than those of the hook wire group in our study. However, the localization time was significantly longer for the coil group because the process requires measuring the distance between the guide tip and pleura and calculating the length of coil released. Because the released coil was located within 1 cm around the nodule, damage to the lesion is avoided and does not affect wedge resection, which is usually within 2 cm of the lesion. There are also reports in the literature that coil use does not affect the pathological diagnosis or cause needle tract dissemination.14,17
The main postoperative complications in this study were postoperative air leakage and chylothorax. We speculate that the possible cause of chylothorax was due to damage to the thoracic duct during VATS surgery. This was not related to localization, which does not damage the lymphatic vessels. One major complication occurred in the hook wire group (postoperative hemothorax), and a thoracotomy was performed the next day. There was no statistical difference in the time of drainage tube removal or the amount of surgical bleeding between the two groups. However, operation time was significantly longer for the coil group because it was necessary to use a fluoroscopy device to intraoperatively confirm the coil’s position. This increases the operation time, and the use of fluoroscopy equipment also adds radiation risk to both the patient and doctors.
There are many other methods for nodular localization before VATS. Although useful, problems remain. For example, liquid contrast agent injection can cause an allergic reaction and may affect the accuracy of pathological results. There was a description of hydrogel localization,10 but this can cause an irritating cough and induce pneumothorax. Electromagnetic navigation and positioning technology have been developed in recent years, but there are no in-depth studies on their use.18 Radioisotopes can also be used to locate nodules, but the equipment has special requirements and radiation hazards, so their clinical use is limited.19 There are also early intraoperative localization modes or the simultaneous use of two methods.9,20 Dual marker localization is an alternative localization method. Although the positioning time is longer than that of the single method, dual positioning achieves a higher success rate and lowers the risk of failure.
Our results should be considered in the context of several shortcomings. It was a retrospective, single-centre study, and large multicentre, randomized controlled trials are required to support and validate the present findings. We also did not compare long-term postoperative survival or recurrence rates for the two localization methods.
In summary, both preoperative localization methods were effective and safe, and had high preoperative positioning rates. The positioning procedure was simpler for the hook wire compared to the coil, although there was no significant difference between the two groups regarding the postoperative complication rate, it was slightly higher in hook wire group than in coil group.
Footnotes
Acknowledgment: Liqing Kang and Junzhong Liu contributed to concept and design of the study. Xinhua Wang, Yongming Wang, Changsheng Liang and Minfeng Sun were involved in collection and assembly of data. Junzhong Liu was responsible of data analysis. All authors participated in manuscript writing.
Contributor Information
Junzhong Liu, Email: ljunzhong@sina.com.
Xinhua Wang, Email: xinhuawang6@sohu.com.
Yongming wang, Email: yingmingwang123@126.com.
Minfeng Sun, Email: wfhxbyyfsk@sina.com.
Changsheng Liang, Email: 1144320775@qq.com.
Liqing Kang, Email: 13333367921@163.com.
REFERENCES
- 1.Aberle DR, Abtin F, Brown K. Computed tomography screening for lung cancer: has it finally arrived? implications of the National lung screening trial. J Clin Oncol 2013; 31: 1002–8. doi: 10.1200/JCO.2012.43.3110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gao F, Sun Y, Zhang G, Zheng X, Li M, Hua Y. Ct characterization of different pathological types of subcentimeter pulmonary ground-glass nodular lesions. Br J Radiol 2019; 92: 20180204. doi: 10.1259/bjr.20180204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kitano K, Sato M. Latest update about virtual-assisted lung mapping in thoracic surgery. Ann Transl Med 2019; 7: 36. doi: 10.21037/atm.2018.12.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Congregado M, Merchan RJ, Gallardo G, Ayarra J, Loscertales J. Video-Assisted thoracic surgery (VATS) lobectomy: 13 years' experience. Surg Endosc 2008; 22: 1852–7. doi: 10.1007/s00464-007-9720-z [DOI] [PubMed] [Google Scholar]
- 5.Nakashima S, Watanabe A, Obama T, Yamada G, Takahashi H, Higami T. Need for preoperative computed tomography-guided localization in video-assisted thoracoscopic surgery pulmonary resections of metastatic pulmonary nodules. Ann Thorac Surg 2010; 89: 212–8. doi: 10.1016/j.athoracsur.2009.09.075 [DOI] [PubMed] [Google Scholar]
- 6.Park CH, Han K, Hur J, Lee SM, Lee JW, Hwang SH, et al. . Comparative effectiveness and safety of preoperative lung localization for pulmonary nodules: a systematic review and meta-analysis. Chest 2017; 151: 316–28. doi: 10.1016/j.chest.2016.09.017 [DOI] [PubMed] [Google Scholar]
- 7.Li C, Liu B, Jia H, Dong Z, Meng H. Computed tomography-guided hook wire localization facilitates video-assisted thoracoscopic surgery of pulmonary ground-glass nodules. Thorac Cancer 2018; 9: 1145–50. doi: 10.1111/1759-7714.12801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nardini M, Bilancia R, Paul I, Jayakumar S, Papoulidis P, ElSaegh M, et al. . 99mTechnetium and methylene blue guided pulmonary nodules resections: preliminary British experience. J Thorac Dis 2018; 10: 1015–21. doi: 10.21037/jtd.2018.01.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin C-W, Ko H-J, Yang S-M, Chen Y-C, Ko W-C, Huang H-C, et al. . Computed tomography-guided dual localization with microcoil and patent blue vital dye for deep-seated pulmonary nodules in thoracoscopic surgery. J Formos Med Assoc 2019; 118: 979–85. doi: 10.1016/j.jfma.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 10.Imperatori A, Fontana F, Dominioni L, Piacentino F, Macchi E, Castiglioni M, et al. . Video-Assisted thoracoscopic resection of lung nodules localized with a hydrogel plug. Interact Cardiovasc Thorac Surg 2019; 29: 137–43. doi: 10.1093/icvts/ivz030 [DOI] [PubMed] [Google Scholar]
- 11.Su T-H, Fan Y-F, Jin L, He W, Hu L-B. Ct-Guided localization of small pulmonary nodules using adjacent microcoil implantation prior to video-assisted thoracoscopic surgical resection. Eur Radiol 2015; 25: 2627–33. doi: 10.1007/s00330-015-3676-5 [DOI] [PubMed] [Google Scholar]
- 12.Huang HZ, Wang GZ, LC X, GD L, Wang Y, Wang YH, et al. . Ct-Guided Hookwire localization before video-assisted thoracoscopic surgery for solitary ground-glass opacity. Oncotarget 2017; 8: 108118–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu L, Zhang LJ, Chen B, Cao JM, Lu GM, Yuan L, et al. . Novel CT-guided coil localization of peripheral pulmonary nodules prior to video-assisted thoracoscopic surgery: a pilot study. Acta Radiol 2014; 55: 699–706. doi: 10.1177/0284185113506136 [DOI] [PubMed] [Google Scholar]
- 14.Hu L, Gao J, Chen C, Zhi X, Liu H, Hong N. Comparison between the application of microcoil and hookwire for localizing pulmonary nodules. Eur Radiol 2019; 29: 4036–43. doi: 10.1007/s00330-018-5939-4 [DOI] [PubMed] [Google Scholar]
- 15.Hwang S, Kim TG, Song YG. Comparison of hook wire versus coil localization for video-assisted thoracoscopic surgery. Thorac Cancer 2018; 9: 384–9. doi: 10.1111/1759-7714.12589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bommart S, Bourdin A, Marin G, Berthet JP, Pujol JL, Serre I, et al. . Impact of preoperative marking coils on surgical and pathologic management of impalpable lung nodules. Ann Thorac Surg 2014; 97: 414–8. doi: 10.1016/j.athoracsur.2013.09.041 [DOI] [PubMed] [Google Scholar]
- 17.Mayo JR, Clifton JC, Powell TI, English JC, Evans KG, Yee J, et al. . Lung nodules: CT-guided placement of microcoils to direct video-assisted thoracoscopic surgical resection. Radiology 2009; 250: 576–85. doi: 10.1148/radiol.2502080442 [DOI] [PubMed] [Google Scholar]
- 18.Yu PSY, Man Chu C, Lau RWH, Wan IYP, Underwood MJ, Yu SCH, et al. . Video-Assisted thoracic surgery for tiny pulmonary nodules with real-time image guidance in the hybrid theatre: the initial experience. J Thorac Dis 2018; 10: 2933–9. doi: 10.21037/jtd.2018.05.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dailey WA, Frey GT, McKinney JM, Paz-Fumagalli R, Sella DM, Toskich BB, et al. . Percutaneous computed Tomography-Guided Radiotracer-Assisted localization of difficult pulmonary nodules in Uniportal video-assisted thoracic surgery. J Laparoendosc Adv Surg Tech A 2018; 28: 1451–7. doi: 10.1089/lap.2018.0248 [DOI] [PubMed] [Google Scholar]
- 20.Chao Y-K, Leow OQY, Wen C-T, Fang H-Y. Image-Guided thoracoscopic lung resection using a dual-marker localization technique in a hybrid operating room. Surg Endosc 2019; 33: 3858–63. doi: 10.1007/s00464-019-06883-y [DOI] [PubMed] [Google Scholar]