Abstract
The number of cases of coronavirus disease 2019 (COVID-19) has been exponentially increasing everyday. It is important to recognize the comorbidities and risk factors associated with this highly contagious and serious disease that has caused thousands of deaths worldwide. Patients with certain conditions like diabetes, hypertension, cardiovascular disease and chronic lung diseases have been reported to develop serious complications from COVID-19. Idiopathic pulmonary fibrosis (IPF) is a disease that is more prevalent in the elderly population, the same group that are more susceptible to serious complications from COVID-19. Our literature search did not reveal any review about COVID-19 in IPF patients. We report a patient with IPF who was exposed to COVID-19 from her spouse and died from its complications. This case would help to raise the awareness among IPF patients to follow the necessary precautions to reduce the risk of contracting the disease.
Keywords: covid-19, corona virus, ipf, idiopathic pulmonary fibrosis, acute hypoxemic respiratory failure
Introduction
Coronavirus disease 2019 (COVID-19) is a rapidly spreading infectious disease caused by novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) [1]. This pandemic has already led to thousands of deaths worldwide, and the number of infected cases continues to rise everyday. Although this virus could infect anyone, it has been found that patients who are older and those with certain pre-existing comorbidities suffer from serious complications due to this disease. Idiopathic pulmonary fibrosis (IPF) is a chronic progressive interstitial lung disease of unknown etiology and its prevalence is higher in the elderly population. Chronic lung disease has been recognized as a risk factor for serious COVID-19 disease, and we report a case of fatal COVID-19 viral pneumonia in a patient with IPF [1-3].
Case presentation
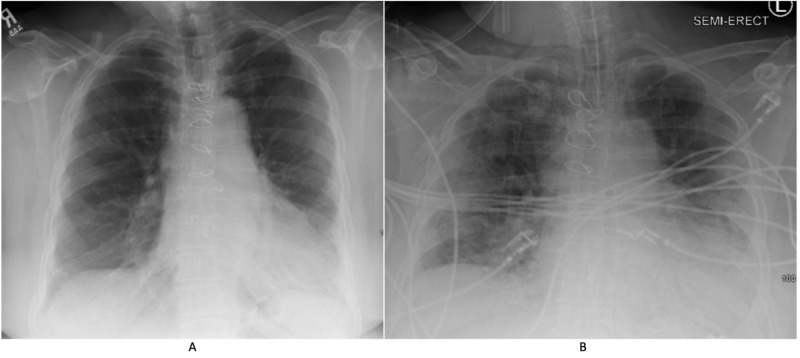
On April 2, 2020, a 79-year-old female with a history of hypertension and IPF presented with cough, worsening dyspnea, increased oxygen requirements, fever and diarrhea. Her vital signs include a temperature of 100.4°F, a heart rate of 98 bpm, an oxygen saturation of 85% on room air and a blood pressure of 102/56 mmHg. She is usually on oxygen two liters per minute at home for chronic hypoxic respiratory failure from IPF. She was on nintedanib 100 mg twice daily for her IPF and metoprolol 12.5 mg daily for her hypertension. Her pulmonary function test done two years ago showed moderate restrictive lung disease with a forced vital capacity of two liters (77% predicted), total lung capacity of three liters (63% predicted) and diffusion capacity of 58% predicted. Her physical exam was unremarkable. She was placed on isolation precautions because of her clinical presentation and her test for SARS-CoV-2 came back positive (Roche’s Cobas nucleic acid amplification test). She was exposed to her husband who was recently diagnosed with COVID-19. She required three liters of supplemental oxygen for her hypoxemia. Chest radiology showed multifocal consolidations in both lungs (Figure 1).
Figure 1. Chest X-ray.
(A) Chest X-ray done three months prior to presentation shows bilateral interstitial infiltrates predominantly in the lung bases. (B) Chest X-ray done on day 4 of COVID-19 shows worsening bilateral multifocal infiltrates superimposed on chronic changes.
She received azithromycin and hydroxychloroquine as per the protocol. However, her condition deteriorated requiring 10 liters of supplemental oxygen and on day 3 she was transferred to intensive care unit and intubated for worsening hypoxic respiratory failure. She required 100% fractional concentration of oxygen in inspired gas (FiO2) and 10 cm H2O positive end-expiratory pressure (PEEP) on the ventilator. A limited bedside echocardiogram revealed normal left and right ventricular function. Her inflammatory markers continued to worsen. Ferritin which was 600 ng/mL at the time of her presentation, worsened to 50,480 ng/mL. Her white blood cell (WBC) count was 15,000/mm3 with an absolute lymphocyte count of 800/mm3, procalcitonin was 0.14 ng/mL, D-dimer was 3.3 µg/mL and lactate dehydrogenase (LDH) was 628 IU/L. She received a single intravenous dose of tocilizumab 600 mg. On day 4, she developed severe septic shock and multiorgan dysfunction (worsening renal function, liver function, circulatory collapse and respiratory failure) requiring norepinephrine, vasopressin, phenylephrine and angiotensin II. She was started on intravenous hydrocortisone 100 mg three times daily, but despite all the aggressive measures she died on day 5. We would like to mention that at the time of this patient's presentation, other treatments like convalescent plasma and remdesivir were not readily available.
Discussion
Chronic lung disease has been reported as a potential risk factor for COVID-19 caused by SARS-CoV-2. In a study that looked at the clinical characteristics and comorbidities in more than 44,000 patients infected with SARS-CoV-2 in China, chronic lung disease had been listed as a comorbidity in only 2.4% of them [1]. On April 8 2020, Centers for Disease Control (CDC) released an early report on the characteristics of hospitalized patients with COVID-19 in the United States, and chronic lung disease was reported as a risk factor in 34.6% of the 159 hospitalized COVID-19 patients [2]. It was also reported that 80% of these patients had obstructive lung disease. On April 29 2020, in the data released by CDC, out of 305 COVID-19 patients in Georgia, chronic respiratory disease was reported as a comorbidity in 20.3% and out of whom 77% had obstructive airway diseases [3]. The prevalence of COVID-19 in IPF has not been reported. IPF is the most common type of idiopathic interstitial pneumonia, characterized by progressive fibrosis with a high fatality rate. The incidence and prevalence of the disease increase with age. IPF is characterized by inflammation and lung injury, and the role of cytokines in its pathogenesis has been well established [4]. There is accumulating evidence that a subgroup of patients with COVID-19 develop cytokine storm syndrome leading to increased mortality from the virus-induced hyperinflammation [5]. It is possible that co-existence of these two fatal disease conditions may significantly affect patient outcomes. On the other hand, survivors of COVID 19 have been reported to develop pulmonary fibrosis as a consequence of dysregulated immune response [6].
Conclusions
Patients living with IPF may not be at increased risk for contracting COVID-19, but probably are at high risk for developing severe fatal complications from the disease. Hence, it is vital to recognize IPF as a potential serious risk factor for COVID-19 complications and IPF patients take the necessary extra precautions advised by CDC to protect themselves and minimize the risk of contracting COVID-19.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Huang C, Wang Y, Li X, et al. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention: COVID-19 Response Team. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 States, March 1-30. [May;2020 ];https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6915e3-H.pdf . 2020 doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed]
- 3.Centers for Disease Control and Prevention: COVID-19 Response Team. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 - Georgia. [May;2020 ];https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6918e1-H.pdf March. 2020
- 4.The role of inflammation in the pathogenesis of idiopathic pulmonary fibrosis. Bringardner BD, Baran CP, Eubank TD, Marsh CB. Antioxid Redox Signal. 2008;10:287–302. doi: 10.1089/ars.2007.1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.COVID- 19: consider cytokine storm syndromes and immunosuppression. Mehta P, McAuley DF, Brown M, et al. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Advances in the research of mechanism of pulmonary fibrosis induced by Corona Virus Disease 2019 and the corresponding therapeutic measures. [Article in Chinese] Wang J, Wang BJ, Yang JC, et al. Zhonghua Shao Shang Za Zhi. 2020;36:0. doi: 10.3760/cma.j.cn501120-20200307-00132. [DOI] [PubMed] [Google Scholar]