Abstract
Background
Between January 24, 2020 and February 15, 2020, an outbreak of COVID-19 occurred among 335 passengers on a flight from Singapore to Hangzhou in China. This study aimed to investigate the source of the outbreak and assess the risk of transmission of COVID-19 during the flight.
Method
Using a standardized questionnaire, we collected information on the travelers’ demographic characteristics and illness before, during, and after the flight. We also collected data on factors potentially associated with COVID-19 transmission during the flight.
Results
A total of 16 COVID-19 patients were diagnosed among all passengers; the overall attack rate was 4.8%. The attack rate among passengers who had departed from Wuhan was significantly higher than that among those who had departed from other places. One passenger without an epidemiological history of exposure before boarding developed COVID-19. During the flight, he was seated near four infected passengers from Wuhan for approximately an hour and did not wear his facemask correctly during the flight.
Conclusions
COVID-19 transmission may have occurred during the flight. However, the majority of the cases in the flight-associated outbreak could not be attributed to transmission on the flight but were associated with exposure to the virus in Wuhan or to infected members in a single tour group.
Keywords: COVID-19, Air travel, Travel-associated infections, Outbreak investigation
Highlights
-
•
SARS-CoV-2 transmission, especially during flight, was of global concern.
-
•
An outbreak of COVID-19 among passengers on a flight was investigated.
-
•
There appears to have been limited transmission of COVID-19 to one person on board the flight.
1. Introduction
In December 2019, a cluster of acute respiratory illness, now known as coronavirus disease 2019 (COVID-19), occurred in Wuhan, Hubei Province in China [1,2]. By March 22, 2020, a total of 81,093 COVID-19 cases had been confirmed in China, of which 50,005 cases were from Wuhan City [3]. The condition rapidly spread globally, and on March 11, 2020 the World Health Organization declared a COVID-19 pandemic [4]. Epidemiological investigation has shown that COVID-19 is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which can be transmitted from human to human. The two primary transmission routes of SARS-CoV-2 are by contact (direct and indirect contact) or droplets, but the possibility of air-borne infection could not be totally excluded [5,6].
Air travel for leisure and business purposes has risen markedly in recent years due to economic growth and increased globalization [7,8]. Although infrequently reported and difficult to assess accurately, respiratory agents may be easily transmitted to passengers during air travel owing to limited ventilation, high occupant density and a long exposure time [9,10]. Multiple outbreaks of respiratory diseases, such as severe acute respiratory syndrome (SARS), measles, tuberculosis, and influenza, associated with air travel have been reported [[11], [12], [13], [14]]. Recent studies suggest that SARS-CoV-2 may be more transmissible than severe acute respiratory syndrome (SARS) coronavirus and Middle East respiratory syndrome (MERS) coronavirus [15]. However, there have not yet been any reports of probable transmission of SARS-CoV-2 during air travel.
On January 24, 2020, a flight originating from Singapore, and bound for Hangzhou, in China, was strictly managed after landing because approximately 100 passengers aboard the flight had visited Wuhan. Following a quarantine inspection in the airport, several passengers had already developed fever or upper respiratory infection symptoms. They were confirmed to have SARS-CoV-2 infections on the early morning of January 25. As in closed/semiclosed settings, on flight transmission of COVID-19 is facilitated by direct person-to person contact or contact with contaminated surfaces. Consequently, all passengers were required to spend at least 14 days under medical observation. By the end of the medical observation period on February 8, 2020, a total of 16 passengers had been confirmed with SARS-CoV-2 infection.
Here we describe the investigation of the outbreak of COVID-19 among passengers on this flight. The objectives of the investigation were to identify possible sources of exposure, and to evaluate whether transmission occurred during the flight. Because there are no published reports of transmission of SARS-CoV-2 during air travel, our investigation provides preliminary evidence of the risk of SARS-CoV-2 transmission on aircraft.
2. Methods
2.1. Flight
The flight left from Singapore Changi Airport on 24 January 2020, and landed at Hangzhou Xiaoshan Airport in China a few hours later. The aircraft was a Boeing 787-9. The total seat occupancy on the flight was 89% (335/375). The aircraft was equipped with air handling systems.
The boarding time of the flight was 16:30 local time, and the time of departure and landing were 16:50 and 21:40, respectively. A total of 346 people took the flight, of whom 335 were passengers and 11 were crew members. All crew members were Singaporean. Based on the departure records, we divided the passengers into two groups: Group A comprised those who departed from Wuhan to Singapore on 19 January 2020; and Group B comprised those who did not depart from Wuhan and did not have a history of travel to Wuhan.
2.2. Epidemiological investigations
All passengers were interviewed face-to-face or by telephone using a standardized questionnaire. We collected information on traveler demographics, health conditions, and symptoms (including fever, dry cough, shivering, expectoration and headaches) before, during, and after the flight, mask-wearing status, seat location, and activity during the flight. All passengers were required to take their temperature before deplaning.
2.3. Case definition
Infected passengers were categorized as symptomatic and asymptomatic. According to the national guidelines, a confirmed case of symptomatic COVID-19 was defined as a passenger who had a SARS-CoV-2 infection confirmed by real-time reverse-transcription polymerase chain reaction (RT-PCR) testing of a throat swab sample, and had symptoms of typical upper respiratory tract infection (such as runny nose, sore throat and dry cough) [16]. Asymptomatic cases were diagnosed based on positive RT-PCR test results but without any COVID-19 symptoms. The date of the positive RT-PCR test result was used as the onset date for asymptomatic cases, which was in line with a national study [17].
2.4. Laboratory testing
Consistent with a previous national study, all samples were tested for SARS-CoV-2 by use of RT-PCR with the Chinese Centers for Disease Control and Prevention recommended kit in accordance with the protocol established by the World Health Organization [18]. The RT-PCR was conducted at the Zhejiang Provincial Center for Disease Control and Prevention.
2.5. Medical isolation and observation
Since there were a large number of passengers originating from Wuhan and two passengers presented with a fever and upper respiratory infection symptoms, all passengers were regarded as close contacts and required to follow medical isolation and observation protocols for at least 14 days after deplaning on January 24. On arrival of the flight in Hangzhou, after preliminary investigation, passengers in Group A were accommodated in Hotel A near the Hangzhou Xiaoshan international airport; and passengers in Group B were transferred to Hotel B in the center of Hangzhou City; passengers (regardless of their group) who already had symptoms after preliminary investigation were sent to the infectious hospital designated for treatment of COVID-19 in Hangzhou. Except for children staying with a parent, the other passengers lived singly for medical isolation and observation in Hotel A or Hotel B. During the medical isolation and observation period, all passengers were required to take their temperature twice daily and report their health condition if they developed symptoms of an upper respiratory tract infection. If passengers isolated in Hotel A or Hotel B developed illness, they were to be transferred to the designated hospital immediately.
All crew members were isolated in Hotel B. They returned to Singapore on January 26, 2020. According to a message from the diplomatic department of Zhejiang Province, none of these crew members were infected with SARS-CoV-2.
2.6. Ethical considerations
According to the law on public health response in China, formal ethical review and approval of this outbreak investigation was not required.
2.7. Statistical analysis
A descriptive analysis was performed using R (Version 3.6.2) statistical software. Categorical variables were presented as frequencies and percentages. Because our study focused on passengers, crew members were excluded when we calculated the attack rate or performed the analysis of risk infection. Characteristics associated with the risk of infection were compared and tested for statistical significance using the chi-square or Fisher's exact tests.
3. Results
A total of 16 infected passengers, including 10 symptomatic passengers and 6 asymptomatic passengers, were diagnosed between 24 January and 15 February 2020. The overall attack rate among the passengers was 4.8% (16/335).
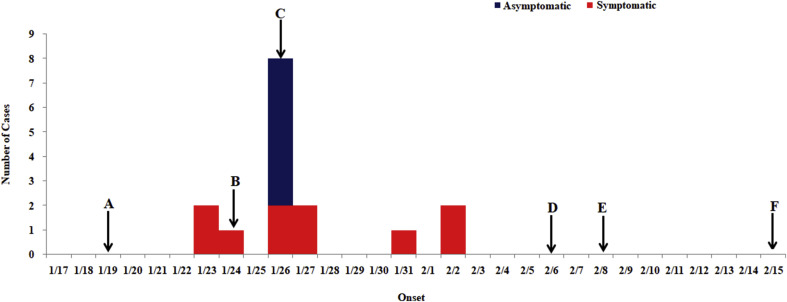
3.1. Temporal distribution
All infected passengers left for Singapore on January 19, 2020 (Fig. 1 ). Of the 10 symptomatic passengers, 2 (Cases 1 and 7) had developed symptoms before boarding and one (Case 2) developed symptoms on 24 January after the flight had landed in Hangzhou (Table 1 ). During the medical isolation and observation period, two passengers (Cases 5 and 6) developed symptoms on January 26 and 27 respectively. Six asymptomatic cases (Case 3 and Cases 11–15) were diagnosed on January 26 when all passengers were sampled and tested for the first time. On February 2, one week after the landing of flight, another two passengers (Cases 10 and 16) developed fever. On 6 February, we sampled and tested all passengers for the second time. However, no additional new cases were discovered during the second screening of all passengers. Moreover, no further cases were reported after 2 February. Passengers who had not departed from Wuhan ended their medical isolation and observation on February 8, and later, passengers who had departed from Wuhan ended their medical isolation and observation one week later, on 15 February (Fig. 1).
Fig. 1.
Epidemic curve indicating the date of onset of COVID-19 cases among passengers on the flight, January to February 2020. (A): The case passengers flew from China to Singapore on 19 January (One passenger departed from Hangzhou; and the remaining 15 case passengers departed from Wuhan.). (B): The flight departed from Singapore to Hangzhou on 24 January and the passengers were placed in medical isolation and under observation on arrival in Hangzhou. (C): All passengers had samples collected for testing on 26 January. (D): All passengers had a second set of samples collected on 6 February. (E): The passengers from places other than Wuhan ended their medical isolation on 8 February. (F): Those who departed from Wuhan ended their medical isolation one week later on 15 February.
Table 1.
Summary of the details of individual cases in a flight-associated outbreak of SARS-CoV-2 infection in January–February 2020.
| Case | Age (years) | Sex | Typea | Onsetb | Residential city | Tour Group | Departure | Seat | Relationship |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 26 | F | Symptomatic | January 23 | Wuhan | A | Wuhan | 11D | Leader of Tour Group A |
| 2 | 45 | M | Symptomatic | January 24 | Wuhan | A | Wuhan | 12D | Husband of Case 3 |
| 3 | 44 | F | Asymptomatic | January 26 | Wuhan | A | Wuhan | 12E | Wife of Case 2 |
| 4 | 29 | F | Symptomatic | January 26 | Wuhan | A | Wuhan | 12A | Daughter of Case 6; niece of Case 5 |
| 5 | 52 | F | Symptomatic | January 27 | Wuhan | A | Wuhan | 44A | Aunt of Case 4; older sister of Case 6 |
| 6 | 45 | F | Symptomatic | January 26 | Wuhan | A | Wuhan | 18A | Mother of Case 4; younger sister of Case 5 |
| 7 | 33 | F | Symptomatic | January 23 | Wuhan | A | Wuhan | 31K | Wife of Case 8 |
| 8 | 36 | M | Symptomatic | January 27 | Wuhan | A | Wuhan | 31J | Husband of Case 7 |
| 9 | 33 | F | Symptomatic | January 31 | Qinghuang Dao | A | Wuhan | 11H | Wife of Case 10 |
| 10 | 32 | M | Symptomatic | February 2 | Qinghuang Dao | A | Wuhan | 11J | Husband of Case 9 |
| 11 | 43 | F | Asymptomatic | January 26 | Wuhan | A | Wuhan | 30D | None |
| 12 | 44 | M | Asymptomatic | January 26 | Wuhan | A | Wuhan | 30E | None |
| 13 | 26 | F | Asymptomatic | January 26 | Wuhan | B | Wuhan | 6H | None |
| 14 | 28 | M | Asymptomatic | January 26 | Wuhan | C | Wuhan | 16E | None |
| 15 | 27 | F | Asymptomatic | January 26 | Wuhan | C | Wuhan | 16F | None |
| 16 | 44 | M | Symptomatic | February 2 | Hangzhou | D | Hangzhou | 29B | None |
F, female; M, male.
Asymptomatic patients tested positive for SARS-CoV-2 using RT-PCR but did not have symptoms of COVID-19; Symptomatic cases tested positive for SARS-CoV-2 on RT-PCR and had symptoms of COVID-19 such as fever and dry cough.
In the asymptomatic patients, the diagnosis date was used as the onset date.
3.2. Seating
Fig. 2 shows seating locations on the airplane for all passengers. Two seating areas had a relatively high concentration of cases: six of the case passengers sat in Rows 11 and 12 and five case passengers sat in Rows 29 to 31. The remaining case passengers were scattered in the Row 6, Row 16, Row 18 and Row 44 (Fig. 2).
Fig. 2.
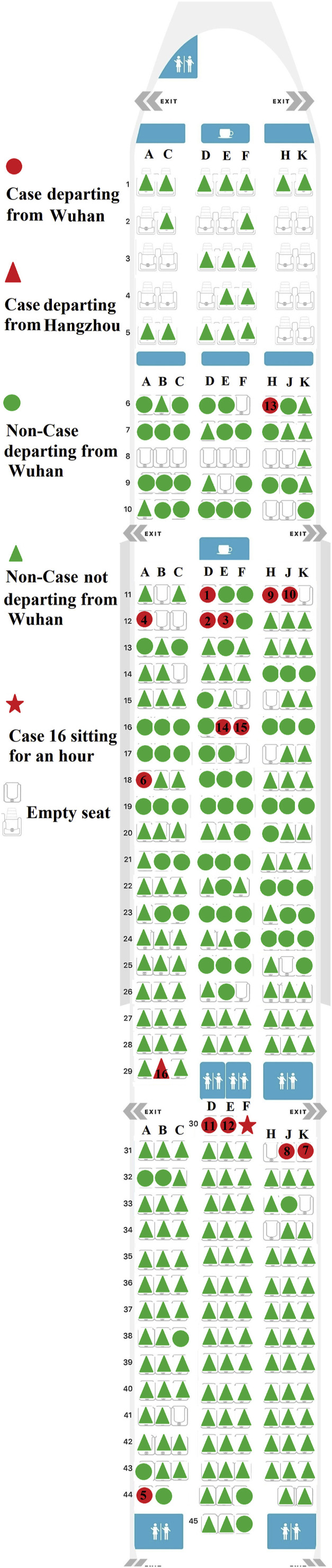
Aircraft configuration and the location of the seats where the 16 case passengers sat during the flight. The numbers in the red background correspond to the Case number shown in Table 1. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Case 16 originally sat in Seat 29B. There were no infected passengers in the first three rows close to Seat 29B; only one passenger who had departed from Wuhan was sitting in the aforementioned location. There was a wide aisle behind Seat 29B, where the toilet was located. However, during flight, Case 16 moved to Seat 30F and sat there for an hour. In the seats around Seat 30F, there were four infected passengers, with Case 11 and Case 12 sitting on the left side of him, and Case 7 and Case 8 sitting behind him on the right (Fig. 2).
3.3. Characteristics of the case passengers
Among the 16 cases, the median age was 37 years (range: 26–52 years). Six cases were female. The 16 cases belonged to four tour groups, with 12 cases in Tour Group A (TGA); one case in Tour Group B (TGB); two cases in Tour Group C (TGC); and one case in tour group D (TGD). Some cases were among passengers who were in a relationship with another case, e.g. Cases 2 and 3 were a couple (Table 1).
There were 15 tour members in TGA, of whom 12 were confirmed SARS-CoV-2 infection, an attack rate of 80%. All the cases in TGA, TGB and TGC departed from Wuhan. In contrast, Case 16, who was a member of TGD, lived in Hangzhou, and departed from Hangzhou. The detailed information of all cases is listed in Table 1.
Table 2 summarizes the attack rates according to city of departure, age, and sex. The attack rate of passengers who departed from Wuhan was 13.8%, compared to 0.4% in passengers who did not depart from Wuhan (p < 0.001). The attack rate did not differ significantly by sex but was significantly higher among passengers aged 20–29 years, and 40–59 years, than in those aged<20 years and ≥60 years.
Table 2.
Attack rate according to characteristics of passengers involved in a flight-associated outbreak of COVID-19 in January–February 2020.
| Characteristics | Total N = 335 | Number of cases N = 16 | Attack rate (%) | P |
|---|---|---|---|---|
| Departure city | <0.001 | |||
| Wuhan | 109 | 15 | 13.76 | |
| Not Wuhan | 226 | 1 | 0.44 | |
| Sex | 0.565 | |||
| Male | 149 | 6 | 4.03 | |
| Female | 186 | 10 | 5.38 | |
| Age (years) | 0.010 | |||
| <20 | 69 | 0 | 0.00 | |
| 20–39 | 182 | 9 | 4.95 | |
| 40–59 | 71 | 7 | 9.86 | |
| ≥60 | 13 | 0 | 0.00 |
3.4. Exposure
According to the travel schedule, although TGA, TGB, and TGC all traveled to Singapore, there was no contact between the different groups before boarding the returning flight. All cases wore masks most of time and none of the cases visited a hospital or had contact with suspected or confirmed COVID-19 case during their travel.
Case 16 departed from Hangzhou to Singapore on 19 January 2020. None of the travelers in his tour group had visited Wuhan. Case 16 reported that he had not visited a hospital and had no contact with individuals suspected of having or confirmed with having COVID-19 before boarding the plane. Moreover, he stated he wore a mask while traveling in Singapore.
During air travel, all 16 case passengers wore masks. However, they removed their masks when they ate dinner or drank water provided during the flight. During the flight, Case 16 sat in Seat 30F for about an hour and talked to his wife and son in Seats 31E and 31F, respectively. While he talked, he reported that he did not wear his mask tightly, and his nose was outside of mask.
4. Discussion
We have described an outbreak of COVID-19 that affected 16 passengers who traveled on the same flight. The primary objective of our investigation was to determine possible sources of the outbreak and whether the transmission was occurred in the aircraft. We identified only one case (Case 16) who appears to have become infected during flight. The sources of infection in the remaining 15 passengers were complex and the passengers could have acquired their infections in Wuhan before their tour, or during the group tour before boarding.
Two cases (Cases 1 and 7) were infected before taking the flight because they were symptomatic before taking the flight. Previous research had suggested the SARS-CoV-2 is transmissible during the incubation period [19]. The high attack rate among the members of TGA indicates that SARS-CoV-2 infections occurred within TGA, which was the result of close exposure during their tour. Moreover, although TGA members drop off the mask during meals on the flight, they had donned a mask in most of other time. Considering that the median incubation period was 4 days (interquartile range: 2–7 days) [18], we hypothesize that the remaining 10 cases in TGA were probably infected before taking the flight, rather than of during the flight. However, it was not possible to determine whether they had become infected in Wuhan, or during travel.
Case 13 in TGB and Cases 14 and 15 in TGC were asymptomatic and were diagnosed in the January 26 when we collected samples from passengers and tested them for the first time. Although they had left Wuhan on January 19, 2020, other studies have shown that transmission of SARS-CoV-2 in Wuhan on that day became widespread prior to their departure [17,20]. They also wore masks during air travel. Therefore, we believe they are most likely to have been infected in Wuhan, and not during flight.
With regard to Case 16, he did not have a history of exposure to Wuhan, or any suspected or confirmed cases of COVID-19 before boarding the flight in Singapore, and he wore a mask while traveling in Singapore. After boarding, he moved from seat 29B to 30F which was in the close proximity to the seats of Cases 7, 8, 11, and 12. Moreover, he talked to his wife (31E) and son (31F) with his mask loosened. After landing, he was immediately isolated and could not have any other source of exposure. The time from the flight landing to the onset of his symptoms fell within the accepted 1-to-14-day COVID-19 incubation period [16]. Therefore, he probably acquired SARS-CoV-2 infection during the flight. Our investigation further corroborated the probable transmission of SARS-CoV-2 on the flight recently reported by Eldin et al. [21].
Previous studies suggest that the basic reproductive number of COVID-19 ranges between 1.5 and 6.5. COVID-19 seems to be more transmissible than SARS and MERS [15]. However, in the present flight outbreak of COVID-19, the relative low number of the secondary cases that occurred due to transmission during the flight may be attributed to the wearing of masks, which have been shown to be effective in blocking the transmission of respiratory diseases at mass gatherings [22]. The low rate of transmission during the flight may also be attributed to the design of and equipment in the aircraft. The air recirculation system, with the highly efficient particulate filter equipment and laminar nature of airflow, may have effectively prevented or restricted the transmission of the virus [7,9]. In addition, after landing, all passengers were sent to designated places for medical isolation and observation. The strict management of all passengers further contributed to avoiding a larger travel-associated outbreak of COVID-19.
The atypical symptom onset of COVID-19 and the transmissibility of SARS-CoV-2 during incubation period make the prevention of SARS-CoV-2 transmission on aircraft challenging. Passengers are in close contact with one another in a confined space for hours during air travel. Numerous high-contact surfaces, such as armrests, tray tables, and seat controls, may serve as potential SARS-CoV-2 fomites [23]. Given these potential risks and those demonstrated by our investigation, development of appropriate prevention and control measures must take this into consideration. We suggest the key stakeholders should standardize aircraft disinfection protocols, train cabin crew for public health emergencies, implement technological solutions to reduce passenger contact with potentially contaminated surfaces, educate the general public to wear their masks closely and to wash their hands frequently. Fast reliable testing methods for detection of SARS-CoV-2 also need to be developed, to enable early diagnosis and to prevent infected passengers from boarding.
Our investigation had several limitations. Firstly, we collected exposure information by interview and telephone, and recall bias cannot be excluded. Moreover, we were unable to get a detailed and accurate trajectory of each case before boarding. Therefore, we cannot rule out the possibility that inapparent transmission between Case 16 and the other cases occurred in the shops, toilets, or airport lounge before boarding. Secondly, we did not perform virus isolation and genome sequencing of the virus, which could have provided evidence of whether viral transmission occurred during the flight. Thirdly, we did not perform surface swabs or take air samples in the aircraft cabin, and so do not have direct evidence of transmission occurring during the flight.
In conclusion, a flight-related outbreak of COVID-19 was investigated. The temporal, spatial, and exposure evidence suggests that SARS-CoV-2 transmission may have occurred during the flight. However, the majority of 16 cases in the outbreak were not attributed to transmission on the flight. Exposure to the virus in Wuhan or by infected members within the same tour group account for most cases in the outbreak. Our investigation suggests that it is important to take measures such as wearing a mask, temperature screening, and quarantine of close contacts to reduce the transmission of SARS-CoV-2 before, during, and after flights.
Funding
This work was financially supported by grants from Zhejiang province (Zhejiang Scientific and Technological Major Project) under the 2020 Emergency (Grant No. 2020C03124), Zhejiang University special scientific research fund for COVID-19 prevention and control (Grant No. 2020XGZX047) and Technology Project of Hangzhou Municipality (Grant No. 20202013A02).
CRediT authorship contribution statement
Junfang Chen: Writing - original draft, Investigation. Hanqing He: Writing - original draft, Investigation, Writing - original draft, Writing - review & editing. Wei Cheng: Writing - original draft, Writing - review & editing. Yan Liu: Writing - original draft, Investigation. Zhou Sun: Investigation, Writing - original draft, Writing - review & editing. Chengliang Chai: Writing - original draft, Investigation. Qingxin Kong: Writing - original draft, Investigation. Wanwan Sun: Writing - original draft. Jiaqi Zhang: Writing - original draft. Song Guo: Writing - original draft. Xuguang Shi: Writing - original draft. Jinna Wang: Writing - original draft. Enfu Chen: Writing - original draft. Zhiping Chen: Investigation, Writing - original draft.
Declaration of competing interest
For all authors none were declared.
Acknowledgments
We would like to thank public health physicians and staff from Xiaoshan District Center for Disease Control and Prevention for their invaluable assistance with field and telephone investigation, contacts management and data reporting.
References
- 1.Kucharski A.J., Russell T.W., Diamond C. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect Dis. 2020;S1473–3099(20) doi: 10.1016/S1473-3099(20)30144-4. https://doi:10.1016/S1473-3099(20)30144-4 30144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected Pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. https://doi:10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Health Commission of the People's Republic of China Update on COVID-19 epidemic at 24:00 on March 22. http://www.nhc.gov.cn/xcs/yqfkdt/202003/fbd8871d80574991a4913cd180f83402.shtml
- 4.World Health Organization Coronavirus disease 2019 (COVID-19) Situation report – 51. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 accessed.
- 5.Van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim Y.I., Kim S.G., Kim S.M. Infection and rapid transmission of SARS-CoV-2 in Ferrets. Cell Host Microbe. 2020;S1931–3128(20) doi: 10.1016/j.chom.2020.03.023. https://doi:10.1016/j.chom.2020.03.023 30187-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korves T.M., Piceno Y.M., Tom L.M. Bacterial communities in commercial aircraft high-efficiency particulate air (HEPA) filters assessed by PhyloChip analysis. Indoor Air. 2013;23(1):50–61. doi: 10.1111/j.1600-0668.2012.00787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rebolledo J., Garvey P., Ryan A. International outbreak investigation of Salmonella Heidelberg associated with in-flight catering. Epidemiol Infect. 2014;142(4):833–842. doi: 10.1017/S0950268813001714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leder K., Newman D. Respiratory infections during air travel. Intern Med J. 2005;35(1):50–55. doi: 10.1111/j.1445-5994.2004.00696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta J.K., Lin C.H., Chen Q. Risk assessment of airborne infectious diseases in aircraft cabins. Indoor Air. 2012;22(5):388–395. doi: 10.1111/j.1600-0668.2012.00773.x. [DOI] [PubMed] [Google Scholar]
- 11.Lei H., Tang J.W., Li Y. Transmission routes of influenza A(H1N1)pdm09: analyses of inflight outbreaks. Epidemiol Infect. 2018;146(13):1731–1739. doi: 10.1017/S0950268818001772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edelson P.J. Patterns of measles transmission among airplane travelers. Trav Med Infect Dis. 2012;10(5–6):230–235. doi: 10.1016/j.tmaid.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 13.Olsen S.J., Chang H.L., Cheung T.Y. Transmission of the severe acute respiratory syndrome on aircraft. N Engl J Med. 2003;349(25):2416–2422. doi: 10.1056/NEJMoa031349. [DOI] [PubMed] [Google Scholar]
- 14.An der Heiden M., Hauer B., Fiebig L. Contact investigation after a fatal case of extensively drug-resistant tuberculosis (XDR-TB) in an aircraft, Germany. Euro Surveill. 2017;22(12) doi: 10.2807/1560-7917.ES.2017.22.12.30493. https://doi:10.2807/1560-7917 July 2013. ES. 2017.22.12.30493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y., Gayle A.A., Wilder-Smith A., Rocklov J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Trav Med. 2020;27(2) doi: 10.1093/jtm/taaa021. https://doi:10.1093/jtm/taaa021 taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Health Commission of the People's Republic of China COVID-19 prevention and control program. http://www.nhc.gov.cn/jkj/s3577/202003/4856d5b0458141fa9f376853224d41d7/files/4132bf035bc242478a6eaf157eb0d979.pdf 7 March 2020. sixth ed., [in Chinese] [DOI] [PMC free article] [PubMed]
- 17.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liuxingbingxue Zazhi. 2020;41(2):145–151. [Google Scholar]
- 18.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. http://doi:10.1056/NEJMoa2002032 NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tong Z.D., Tang A., Li K.F. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang province, China, 2020. Emerg Infect Dis. 2020;26(5):1052–1054. doi: 10.3201/eid2605.200198. http://doi:10.3201/eid2605.200198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.2648. http://doi:10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 21.Eldin C., Lagier J.C., Mailhe M., Gautret P. Probable aircraft transmission of Covid-19 in-flight from the Central African Republic to France. Trav Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101643. http://doi:10.1016/j.tmaid.2020.101643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barasheed O., Alfelali M., Mushta S. Uptake and effectiveness of facemask against respiratory infections at mass gatherings: a systematic review. Int J Infect Dis. 2016;47:105–111. doi: 10.1016/j.ijid.2016.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirking H.L., Cortes J., Burrer S. Likely transmission of norovirus on an airplane. Clin Infect Dis. 2010;50(9):1216–1221. doi: 10.1086/651597. October 2008. [DOI] [PubMed] [Google Scholar]