Abstract
Background
Humans are generally susceptible to SARS-CoV-2, which has caused a global pandemic of COVID-19. The screening of infected people in the population still mainly depends on clinical symptoms. However, there is limited research on the characteristics of clinical symptoms in different populations, especially in imported cases.
Methods
To retrospectively analyze the clinical data of 494 confirmed COVID-19 patients admitted to a designated hospital in Shanghai from January 20, 2020, to March 31, 2020, we compared the clinical manifestations in different populations and their influencing factors in COVID-19 patients.
Results
(1) Of the 494 patients, 453 (91.7%) had different symptoms at admission, and 39 (7.89%) patients were asymptomatic. (2) We compared the symptoms of patients according to different stratifications and found the following results: (a) The proportion of dyspnea was significantly higher in male patients than in female patients (P < .05). (b) The proportions of a stuffy nose, sore throat, and olfactory and gustatory dysfunction were significantly higher in children than in adult patients (P < .05). (c) The proportions of fever, chest tightness, shortness of breath, and fatigue were significantly higher in local cases than in imported cases. In comparison, the proportions of nasal congestion, stuffy nose, sore throat, headache, and olfactory and gustatory dysfunction were significantly lower in imported cases than in imported cases (P < .05). (d) The proportions of chest tightness, shortness of breath, and dyspnea were significantly higher in severely ill patients than in those with mild symptoms (P < .05). (3) Thirty-one asymptomatic patients were significantly younger than symptomatic patients, and they had a higher proportion of imported cases, white blood cell and lymphocyte count levels, and fewer abnormal CT cases than the group of symptomatic patients (P < .05). (4) The number of days since the onset of the disease needed for the symptoms to disappear was associated with the epidemiological history (imported cases), the number of days until the pharyngeal swab nucleic acid test turned negative, the days of hospitalization, the days of onset, and the white blood cell and lymphocyte count levels (P < .05).
Conclusions
The majority of COVID-19 patients (91.7%) had early symptoms, whereas 7.89% of COVID-19 patients were asymptomatic. Younger patients had fewer symptoms, mainly the upper respiratory symptoms, and the illness condition was milder, which was more common in imported cases. Elderly male patients had severe symptoms when admitted. The number of days needed for the patient's symptoms to disappear was closely related to the number of days necessary for the pharyngeal swab nucleic acid test to turn negative.
Key Words: SARS-CoV-2, Novel coronavirus pneumonia, Symptoms
Due to the highly contagious SARS-CoV-2 and the susceptibility of the population, the rapid spread of the COVID-19 epidemic has caused an ongoing global pandemic, and many countries declared a national emergency.1 Until May 6, the cumulative number of diagnoses was 3,638,437, and the cumulative number of deaths was 256,958.2 The mortality rate in several countries exceeded 10%, which brought substantial economic losses and life threats to people around the world. At present, the diagnosis of COVID-19 depends on nucleic acid testing.3 However, due to the rapid increase in the number of infections, the high cost of nucleic acid testing, and the shortage of medical supplies, nucleic acid testing cannot be entirely popularized. Many countries have taken measures to monitor the temperature to screen suspected patients for investigation and isolation. However, recent studies have found that the clinical manifestations of some patients with COVID-19 are not typical, and many asymptomatic infections have been reported.4, 5, 6 International studies have found that asymptomatic infections may account for about 60% of all infections, and there are robust viral replication in these patient's throat swab and the virus is highly infectious,4 which has brought challenges to the control of outbreaks worldwide. Therefore, it is urgent to fully understand the clinical symptoms of patients with COVID-19 in different populations and its influencing factors, but the relevant reports are scarce. By summarizing and comparing the symptoms characteristics and its influencing factors of COVID-19 patients in Shanghai, China, this study may provide a theoretical basis for first-line quarantine personnel and clinicians to screen suspected patients.
Methods
Study subjects
We conducted a retrospective study on patients with COVID-19 from January 20, 2020, to March 31, 2020, in the Shanghai Public Health Clinical Center. The patients were diagnosed according to the Chinese management guideline for COVID-19 guidance by the National Health Committee (version 7.0) (hereinafter referred to as “guideline”).7 All of the confirmed cases of COVID-19 were defined as a positive real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay result using pharyngeal swab specimens.8 Only laboratory-confirmed cases were included in the analysis.
According to the classification criteria referred in the “guideline,” 30 patients were clinically classified as severely and critically ill patients, and 464 patients were clinically classified as mild and ordinary patients.
Research methods
Two attending physicians reviewed the electronic medical records of all patients and collected relevant epidemiological investigation, demographic data, medical history, symptoms, laboratory examination results, and chest CT scan reports. Routine blood test results were collected, including white blood cell (WBC) and lymphocyte (LYM) counts.
The biological safety protection third-level laboratory of Shanghai Public Health Clinical Center was approved by the Chinese Center for Disease Control and Prevention. According to WHO guidelines on qRT-PCR, pharyngeal swab samples were collected and tested for SARS-CoV-2 RNA.
To exclude as far as possible the interference of the relevant treatment after admission, early clinical symptoms were defined as all of the clinical symptoms that occur within 3 days after the diagnosis of the pharyngeal swab nucleic acid test. For patients who were asymptomatic at admission, we observed symptoms during the entire hospitalization process. The observation time for olfactory and gustatory dysfunction was from the onset to discharge.
This study screened out asymptomatic infections from close clinical and community contacts and imported cases from outbreak areas. Asymptomatic cases with COVID-19 were defined as asymptomatic cases with a positive nucleic acid test.
Fever was defined as an axillary temperature of at least 37.3°C. Respiratory symptoms included cough, running nose, sore pharyngeal, sore pharyngeal, chest tightness, chest pain, shortness of breath, and dyspnea. Gastrointestinal symptoms included abdominal distension, diarrhea, anorexia, nausea, and vomiting, among others. Systemic symptoms were defined as fatigue, dizziness, headache, muscle aches, arthralgia, and other symptoms.
The days of onset were defined as the time interval from the onset of symptoms to admission to our hospital. The number of days needed for the pharyngeal swab nucleic acid test to turn negative was defined as the time interval from the first symptoms to the day the nucleic acid test first turned negative. The days needed for the pharyngeal swab nucleic acid test to become negative in the asymptomatic patients were defined as the time interval from the first positive nucleic acid test to the first negative nucleic acid test. The days until the patient's symptoms disappeared were defined as the time interval from the patient's first symptoms to their disappearance.
The discharged patient had to conform to the following conditions:6 (1) The patient' temperature returned to normal for more than 3 days; (2) respiratory symptoms improved significantly; lung imaging showed a significant improvement in acute exudative lesions; (3) the RT-PCR test of pharyngeal swab samples had 2 consecutive negative results (at least 24 hours apart), and we recorded the earliest date the nucleic acid test turned negative.
This study was approved by the Shanghai Public Health Clinical Center Ethics Committee, Fudan University. Written informed consent was waived in light of the urgent need to collect new infectious disease data.
Statistical analysis
For continuous variables, first, a distribution of data test was conducted. The normally distributed data were expressed as mean ± standard deviation (χ ± s). The t test was used for the comparison of differences between groups. The non-normally distributed continuous variables were expressed as medians (interquartile range), and differences between groups were compared by the Mann-Whitney test. Categorical variables were expressed in terms of frequency or rate, and the differences between groups were compared by the χ2 test or Fisher exact test. To explore the factors associated with the period during which the symptoms were observed, the Spearman correlation analysis was used. If the P value of the test result was <.05, the difference was considered to be statistically significant. All of the research data were described and analyzed using SPSS 25.0 statistical software (IBM, Seattle WA).
Results
Demographic characteristics and baseline data
Of the 494 patients with COVID-19, 266 were male (53.8%), the age range was 6-88 years old, and the median age was 40 years old. There were 30 critically ill patients with a critical illness rate of 6.07%, and 7 deaths with a mortality rate of 1.42%. They were 415 (84.01%) patients with abnormal CT findings, including 121 patients with no respiratory symptoms, 22 patients without fever and respiratory symptoms, and 15 patients with no symptoms (see Table 1 ).
Table 1.
Demographic, laboratory, and CT findings of patients on admission (n = 494 cases)
| Index | n/median | %/IQR |
|---|---|---|
| Sex (male) | 266 | 53.80% |
| Age, years | 40 | 27-59 |
| <18 | 25 | 5.06% |
| ≥18, <65 | 393 | 79.55% |
| ≥65 | 76 | 15.38% |
| Severe illness/death cases | 30/7 | 6.07%/1.42% |
| Early asymptomatic infection | 39 | 7.89% |
| Imported cases | 167 | 33.81% |
| Days of illness onset* | 4 | 2-7 |
| Days of hospitalization⁎⁎ | 16 | 12-21 |
| Days needed for the pharyngeal swab nucleic acid turned negative⁎⁎⁎ | 13 | 8-18 |
| WBC (×109/L) | 5.00 | 4.03-6.28 |
| LYM (×109/L) | 1.29 | 0.91-1.74 |
| Patients with abnormal CT findings | 415 | 84.01% |
Days of onset = date of admission − date of early symptom, asymptomatic cases were not included.
Days of hospitalization = date of discharge − date of admission, deaths cases were not included.
Days needed for pharyngeal swab nucleic acid turned negative = first date of pharyngeal swab nucleic acid turned negative − first date of early symptom, and days needed for asymptomatic infected patient's nucleic acid turned negative = date of pharyngeal swab nucleic acid turned negative − date of diagnosis, death cases were not included.
Distribution of symptoms in COVID-19 patients
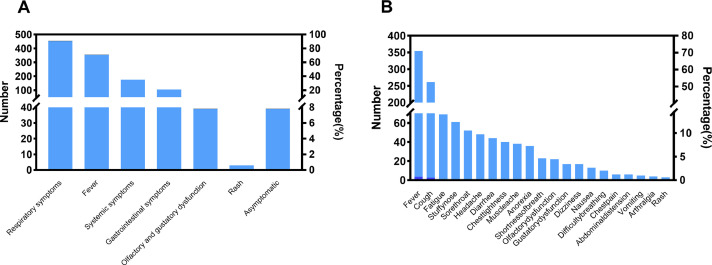
Of the 494 patients, 453 had symptoms (91.7%) at admission, and 39 (7.89%) patients had no symptoms at admission. Of these, 31 (6.28%) were asymptomatic throughout hospitalization and 8 (1.62%) patients were asymptomatic on admission, but with symptoms during hospitalization. Two hundred and three patients (44.81%) had 3 or more symptoms. All of the symptoms included respiratory symptoms, fever, gastrointestinal symptoms, olfactory and gustatory dysfunction, rashes, and systemic symptoms (see Fig 1 ).
Fig 1.
Distribution of symptoms in COVID-19 patients (n = 494). (A) Early symptom distribution of COVID-19 patients. (B) Details of early symptoms of COVID-19 patients.
Comparison of different stratification of symptomatic patients (n = 453)
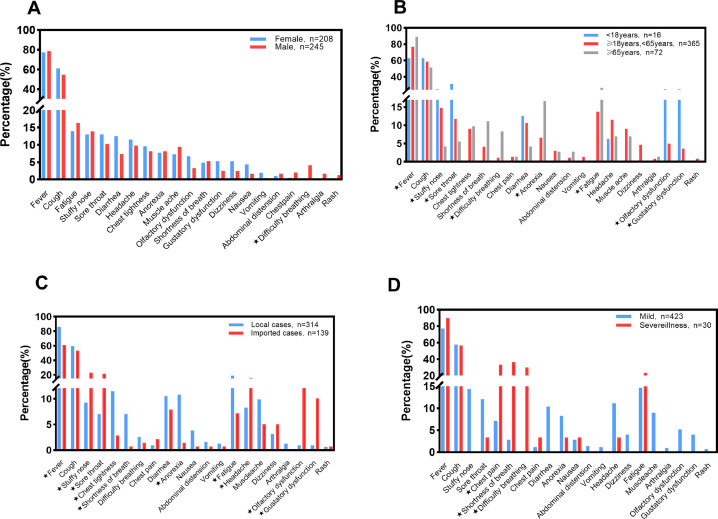
We compared the symptoms of patients between the groups according to different stratification and found the following results: the proportion of dyspnea was significantly higher in males than in females. The young-age group had the fewest number of symptoms and the lowest rate of fever. Still, the incidence of nasal congestion, sore pharyngeal, olfactory, and gustatory dysfunction in the young-age group was significantly higher than in elderly patients. Elderly patients had the highest proportion of symptoms, such as fever, dyspnea, fatigue, and anorexia, but no olfactory and gustatory dysfunction. Local cases had more fever, chest tightness, shortness of breath, and fatigue symptoms than imported cases. At the same time, the frequencies of nasal congestion, runny nose, sore pharyngeal, headache, and olfactory and gustatory dysfunction were significantly lower than those in imported cases, and the differences were statistically significant. The proportions of symptoms of chest tightness, shortness of breath, and dyspnea were significantly higher in the severely ill group than in the mild group, and the remaining symptoms were not statistically significant (see Fig 2 ).
Fig 2.
Comparison of different stratification of symptomatic patients (n = 453). *: P < .05. (A) Comparing female with male group, there was no difference in age, onset days, epidemiological history (local or imported) between the 2 groups, while male patients had a higher critical illness rate. (B) Comparing the 3 groups of different age patients, there was no statistically significant difference in gender and the days of onset in the 3 groups, while the differences in disease classification and epidemiological characteristics (local, imported) were statistically significant. (C) Comparing local with imported group, there was no statistically significant. (D) Comparing mild with severe illness group, the differences in the days of onset was not statistically significant, while the differences in gender, age, and epidemiological history (local, imported) were statistically significant.
Comparison of COVID-19 patients with symptomatic and asymptomatic infection
Asymptomatic infections were significantly more frequent in younger patients than in elderly patients. The proportion of imported cases and both WBC and LYM count levels in the symptomatic patients were higher than in the symptomatic patients. The abnormal CT cases in the asymptomatic infections were fewer than those in symptomatic infections. The differences were statistically significant. However, there was no statistically significant difference in gender, the days needed for the pharyngeal swab nucleic acid test to turn negative after admission, and the days of hospitalization.
Eight patients were asymptomatic in the early stage, but cough and fever symptoms appeared after admission. Among them, 4 patients had symptoms after the nucleic acid test turned negative, 3 patients had symptoms before the nucleic acid test turned negative, and 1 patient had symptoms on the day when the nucleic acid test turned negative (see Tables 2 and 3 ).
Table 2.
Comparison of COVID-19 patients with symptomatic and asymptomatic infection
| Symptomatic n = 453 cases |
Asymptomatic n = 31 cases |
P | |
|---|---|---|---|
| Sex (male) | 245 (54.08%) | 15 (48.39%) | .538 |
| Age, years | 40 (29-59) | 26 (18-55) | .009 |
| <18 | 16 (3.53%) | 8 (25.81%) | .000 |
| ≥18, <65 | 365 (80.57%) | 19 (61.29%) | .010 |
| ≥65 | 72 (15.89%) | 4 (12.90%) | .851 |
| Severe illness/death cases | 30/7 | 0/0 | .274/1.000 |
| Imported cases | 139 (30.68%) | 21 (67.74%) | .000 |
| Days needed for pharyngeal swab nucleic acid turned negative after admission | 7 (3-13) | 7 (3-12) | .810 |
| Days of hospitalization | 16 (12-21) | 15 (12-20) | .232 |
| WBC (×109/L) | 5.00 (4.03-6.28) | 5.11 (4.15-6.41) | .002 |
| LYM (×109/L) | 1.29 (0.91-1.73) | 1.33 (0.96-1.78) | .000 |
| Patients with abnormal CT findings | 393 (86.75%) | 15 (48.39%) | .000 |
Table 3.
Characteristics of early asymptomatic patients (n = 8 cases)
| Sex | Age, years | Mild | Date of the first positive nucleic acid test | Date of onset | symptom | Date of the first negative nucleic acid test | CT finding | Antibody of COVID-19 | |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | F | 25 | Yes | 2020/2/4 | 2020/2/13 | Cough | 2020/2/11 | Yes | * |
| Case 2 | F | 51 | Yes | 2020/2/14 | 2020/2/18 | Cough | 2020/2/17 | No | * |
| Case 3 | M | 30 | Yes | 2020/2/16 | 2020/2/20 | Cough | 2020/2/20 | Yes | * |
| Case 4 | M | 43 | Yes | 2020/3/25 | 2020/3/29 | Fever | 2020/3/30 | Yes | Positive |
| Case 5 | M | 52 | Yes | 2020/3/25 | 2020/3/28 | Cough | 2020/4/1 | Yes | Negative |
| Case 6 | M | 6 | Yes | 2020/3/26 | 2020/4/2 | Fever | 2020/4/4 | No | Positive |
| Case 7 | F | 32 | Yes | 2020/3/28 | 2020/4/5 | Cough | 2020/3/30 | Yes | Positive |
| Case 8 | M | 53 | Yes | 2020/3/31 | 2020/4/8 | Cough | 2020/4/2 | Yes | Positive |
F refers to female; M refers to female; * means not detected.
Comparison of nucleic acid positive and nucleic acid negative patients after symptoms disappeared
Among the patients with COVID-19, there were 168 (34%) patients with positive nucleic acid test after the symptoms disappeared, and it took more days for the pharyngeal swab nucleic acid test to turn negative in these patients than in those with a negative nucleic acid test after the symptoms disappeared (see Table 4 ).
Table 4.
Comparison of nucleic acid positive and nucleic acid negative patients after symptoms disappeared
| Nucleic acid negative cases after symptoms disappeared n = 250 |
Nucleic acid positive cases after symptoms disappeared n = 168 |
P | |
|---|---|---|---|
| Sex (male) | 123 (49.20%) | 94 (56.00%) | .176 |
| Age, years | 38 (28-57) | 40 (28-59) | |
| <18 | 9 (3.60%) | 7 (4.17%) | .767 |
| ≥18, <65 | 211 (84.40%) | 136 (80.95%) | .357 |
| ≥65 | 30 (12.00%) | 25 (14.88%) | .393 |
| Imported cases | 76 (30.40%) | 54 (32.14%) | .706 |
| Days of illness onset | 3 (5-8) | 4 (2-6) | .107 |
| Days needed for the pharyngeal swab nucleic acid turned negative | 11 (8-15) | 14 (12-18) | .000 |
| WBC (×109/L) | 4.96 (4.1-6.10) | 5.07 (4.03-6.41) | .477 |
| LYM (×109/L) | 1.31 (0.96-1.79) | 1.34 (0.93-1.73) | .075 |
| Patients with abnormal CT findings | 210 (84.00%) | 149 (88.69%) | .177 |
Factors associated with the number of days necessary for the symptoms to disappear in patients with COVID-19
The days until the symptoms disappeared in patients with COVID-19 were positively correlated with the history of epidemiology (imported cases), the days needed for the pharyngeal swab nucleic acid test to turn negative, and the days of hospitalization. It was negatively correlated with days of onset, WBC count level, and LYM count level (see Table 5 ).
Table 5.
Factors associated with the number of days until the symptoms disappeared
| Correlation coefficient | P | |
|---|---|---|
| Sex (male) | 0.063 | .199 |
| Age, years | 0.021 | .662 |
| Imported cases | 0.120 | .014 |
| Days needed for the pharyngeal swab nucleic acid turned negative | 0.259 | .000 |
| Days of illness onset | −0.134 | .006 |
| Days of hospitalization | 0.290 | .000 |
| WBC (×109/L) | −0.119 | .015 |
| LYM (×109/L) | −0.123 | .012 |
Discussion
We analyzed the clinical characteristics of 494 patients with COVID-19 in Shanghai and found that COVID-19 patients were mostly adults, up to 94.94%, and children and adolescent cases were rare (5.06%). Similar to previous research results,9 , 10 children did not seem to be susceptible, or their symptoms were relatively mild, and they cannot easily catch the infection. However, there was no significant difference in the sex ratio.
Most of the patients with COVID-19 in Shanghai area visited the hospital earlier, and the median period of onset was only 4 days. The critical illness rate was 6.07%, which also confirmed that the early intervention of COVID-19 was essential for reducing critical illness and mortality rates in many epidemic areas. Our study also showed that the median periods until the pharyngeal swab nucleic acid test turned negative and to end hospitalization were about 2 weeks, which indirectly confirmed that 14 days of observation in isolation for suspected patients is necessary; even asymptomatic patients could clean the virus within 2 weeks. The longest period required for the pharyngeal swab nucleic acid test to turn negative was 18 days in asymptomatic patients, and only 12.9% (4/31) cases were over 14 days. The median of the WBC count level and the LYM count were within the normal reference range, and no obvious bacterial infection was seen. Eighty-four percent of patients (415/494) had abnormal CT manifestations. Still, some of these patients had no symptoms, which seems to suggest that patients with abnormal CT manifestations also need to be tested for the SARS-CoV-2 infection, even if the patient has no fever or respiratory symptoms. Although COVID-19 is a respiratory infection disease, the early symptoms of patients were not limited to respiratory symptoms and fever. In fact, 21.05% of patients could show gastrointestinal symptoms in the early stage, some patients had viremia-related symptoms, such as headache, dizziness, muscle aches, arthralgia, and fatigue, and 7.89% of patients had olfactory and gustatory dysfunctions. Unlike the findings of a multicenter European study,11 85.6% and 88.0% of patients had olfactory and gustatory dysfunctions, respectively, and this difference may be related to genetic background of the populations tested. In addition, it was interesting to observe that 3 patients (0.61%) had rashes in the early stage of the disease. It is well known that people with viral infections, such as measles and chickenpox, usually present with fever and rashes, but there have been no reports of COVID-19 patients with rashes in the early stage. However, we cannot rule out the effects of early medication on these patients with rashes, and further observation is needed in the future.
The proportion of severely ill patients was higher in males, and male patients had a higher proportion of symptoms of dyspnea. Our data also reflected to a certain extent that children with COVID-19 often presented with upper respiratory tract symptoms, and the illness condition was often mild. The proportion of elderly people with dyspnea was higher, which is related to the fact that advanced age was likely to cause severe disease. Imported cases in Shanghai, which is an international city, had increased significantly since March, and their age was significantly lower than that of local patients, the time of confirmed disease was earlier, and the condition was milder. These patients had mainly upper respiratory tract symptoms such as nasal congestion, sore pharyngeal, headache, and abnormal olfactory and gustatory functions.
Except for most symptomatic infected patients, the proportion of asymptomatic infections was not high, almost 7.9%, and they were younger and mostly imported cases. We also found that the levels of WBC count and LYM count in the asymptomatic infections were significantly higher than in the symptomatic patients, which confirmed that the LYM count was important to clear the virus. But it also meant that these patients often did not go to the clinic; it was difficult to identify them in the crowd, and they may cause infection in the surrounding population. Eight patients developed cough and fever after admission. Interestingly, 4 patients had symptoms after the nucleic acid test turned negative. We are still not sure whether the symptoms of these 4 patients were related to COVID-19.
In our study, we identified the special case of the “asymptomatic COVID-19 infected person.” In one-third of patients with COVID-19, the pharyngeal swab nucleic acid test was still positive after the symptoms disappeared. For these patients, the period necessary for the pharyngeal swab nucleic acid test to turn negative was significantly longer than for those whose pharyngeal swab nucleic acid test turned negative after the symptoms disappeared. Strangely, in patients with a positive pharyngeal swab nucleic acid test, after these symptoms disappeared, their chest CT showed complete disappearance of lung lesions. Still, head magnetic resonance found inflammation of the maxillary sinus or paranasal sinuses, which seems to indicate the presence of viruses in the upper respiratory tract for a long time after these patients improved. There have been many reports showing pharyngeal swab virus nucleic acid test turning positive again in the patients with COVID-19 who were discharged from the hospital,12 , 13 but whether these patients' pharyngeal swab nucleic acid test turned positive again is also related to upper respiratory tract inflammation. Their infectivity to the surrounding population is not yet clear, and further research is needed in the future.
Finally, we found that the faster the patient's pharyngeal swab nucleic acid test turned negative, the sooner the symptoms disappeared, and the shorter was the hospital stay. The symptoms of patients with high WBC and LYM counts disappeared faster. And the imported cases' symptoms disappeared more quickly. On the one hand, this may be related to the younger age of the imported cases and the earlier medical treatment. On the other hand, it could be considered that the virus may mutate during the transmission of the population and becomes adapted to the human body, the pathogenic ability was weakened, and the infection capacity became stronger, as many public health and virologists predict, the novel coronavirus infection may become the norm in the future, coexisting with humans for a long time, like an influenza virus.
This research had some limitations. First, our study was only a retrospective analysis of a single center in Shanghai. A small proportion of symptoms may be subjective to the patient, and second, asymptomatic infections were mostly imported cases and, due to the pandemic in the world, its epidemiological history outside the country was not clear, and it was impossible to determine the real time of infection.
Conclusions
In summary, from the analysis of this group of patients with COVID-19 in Shanghai, we conclude that young patients have more common upper respiratory symptoms after infection, and the prognosis is good. Furthermore, the proportion of early asymptomatic patients is not high (not more than 10%), and it is more common in young patients and imported cases. The days until the symptoms disappeared in patients with COVID-19 were positively correlated with the days needed for the pharyngeal swab nucleic acid test turned negative, but negatively correlated with the WBC count and LYM. The symptoms of the imported cases disappeared faster, and the illness condition was milder. For young people and entry-exit personnel, nucleic acid detection is required as a measure to exclude infected patients. During the outbreak of the epidemic, we consider that 14 days of isolated observation may be necessary for people with a history of epidemiology.
Acknowledgments
We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Footnotes
Funding/support: This study was supported by Top University and First-Class Discipline Construction Project of Fudan University (Project No: IDF162005); Scientific research project for novel coronavirus “2019-nCoV” of ZQ (Project No: 2020YJKY01).
Conflicts of interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Author contributions: All of the authors participated in the research design. LH, QZ, and YZ had the idea for this study, designed it, and had full access to all of the data. MX, ZY, and ZH performed the data management and statistical analyses after discussion with all authors. All of the authors participated in data interpretation and in writing the manuscript. All of the authors took responsibility for the decision to submit for publication.
References
- 1.Ding S, Liang TJ. Is SARS-CoV-2 also an enteric pathogen with potential fecal-oral transmission: a COVID-19 virological and clinical review. Gastroenterology. 2020;159:53–61. doi: 10.1053/j.gastro.2020.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available at: https://covid19.who.int. Accessed May 6, 2020.
- 3.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jane Q. Covert coronavirus infections could be seeding new outbreaks [e-pub ahead of print] Nature. 2020 doi: 10.1038/d41586-020-00822-x. Accessed August 11, 2020. [DOI] [PubMed] [Google Scholar]
- 5.Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. Accessed August 8, 2020. [DOI] [PubMed] [Google Scholar]
- 6.Hu ZL, Song C, Xu CJ, et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020;63:706–711. doi: 10.1007/s11427-020-1661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Health Commission of the People's Republic of China. Chinese management guideline for COVID-19 (version 7.0). 2020. Available at:http://www.nhc.gov.cn/yzygj/s7652m/202003/a31191442e29474b98bfed5579d5af95.shtml.pdf. Accessed March 4, 2020 [in Chinese].
- 8.Kui L, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei province. Chin Med J (Engl) 2020;133:1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin J Epidemiol. 2020;41:145–151. [PMC free article] [PubMed] [Google Scholar]
- 10.Yang Y, Lu QB, Liu MJ, et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China [e-pub ahead of print] Med Rxiv. 2020 doi: 10.1101/2020.02.10.20021675. Accessed August 11, 2020. [DOI] [Google Scholar]
- 11.Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020;277:2251–2261. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lan L, Xu D, Ye G, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323:1502–1503. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen C, Gao GJ, Xu YL, et al. SARS-CoV-2–Positive Sputum and Feces After Conversion of Pharyngeal Samples in Patients With COVID-19. Ann Intern Med. 2020;172:832–834. doi: 10.7326/M20-0991. [DOI] [PMC free article] [PubMed] [Google Scholar]