Abstract
Introduction
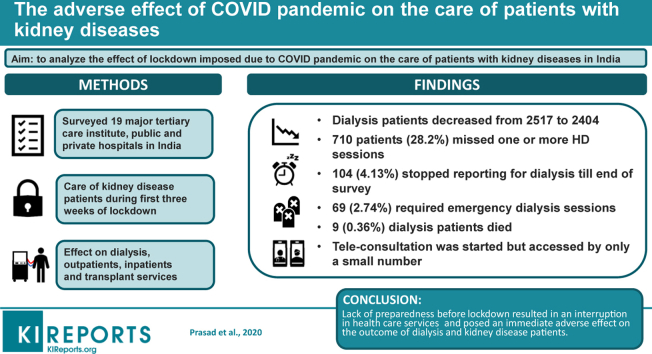
The coronavirus disease 2019 (COVID-19) pandemic has affected the care of patients with noncommunicable diseases, including those suffering from kidney-related ailments. Many parts of the world, including India, adopted lockdown to curb community transmission of disease. The lockdown affected transportation, access to health care facilities, and availability of medicines and consumables as well as outpatient and inpatient services. We aimed to analyze the effect of lockdown imposed due to the COVID-19 pandemic on the care of patients with kidney diseases in India.
Methods
We surveyed 19 major hospitals (8 in the public and 11 in the private sector) to determine the effect of lockdown on the care of patients with kidney disease, including those on dialysis after the first 3 weeks of lockdown.
Results
The total number of dialysis patients in these centers came down from 2517 to 2404. Approximately 710 (28.2%) patients missed 1 or more dialysis sessions, 69 (2.74%) required emergency dialysis sessions, 104 (4.13%) stopped reporting for dialysis, and 9 (0.36%) were confirmed to have died. Outpatient attendance in the surveyed hospital came down by 92.3%, and inpatient service reduced by 61%. Tele-consultation was started but was accessed by only a small number of patients.
Conclusion
Lack of preparedness before lockdown resulted in an interruption in health care services and posed an immediate adverse effect on the outcome of dialysis patients and patients with kidney disease in India. The long-term impact on the health of patients with less severe forms of kidney disease remains unknown.
Keywords: coronavirus disease, dialysis, lockdown, pandemic
Graphical abstract
The COVID-19 pandemic, caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has directly or indirectly affected everyone in the world.1,2 The 850 million people suffering from kidney-related ailments, including the 3.9 million on regular dialysis and recipients of kidney transplantation will not be spared its effects.3
To curb the disease transmission, many countries have adopted the policy of lockdown, an action for mass quarantine. The government of India ordered a nationwide lockdown for 3 weeks on March 24, 2020, which was subsequently extended and still remains in effect with some relaxations at the time of writing.4,5 The lockdown restricted the movement of 1.3 billion people at a time when the number of confirmed coronavirus cases in India was approximately 500. Although its impact on the prevention of spread remains unclear, the lockdown severely limited the ability of patients with chronic diseases to access medical care. The impact was felt almost immediately by patients on dialysis. Public and private transports were shut down, which prevented patients from reaching dialysis centers.6 Lockdown also affected the availability of consumables for hemodialysis and peritoneal dialysis and essential medicines. Regular outpatient services were suspended, and inpatient services severely curtailed. Interruptions in supply chains and increased demand led to shortages of personal protective equipment (PPE), placing health care workers, including dialysis staff, at undue risk. Many hospitals and dialysis centers were ordered to close, and all staff quarantined for 2 weeks after a SARS-CoV-2–positive patient was detected. To this was added social stigma associated with the care of COVID patients spread through social media and word of mouth. This caused fear among the staff, leading to absenteeism.
As with many national societies, the Indian Society of Nephrology issued guidance (adopted by the Indian Ministry of Health), and a hemodialysis preparedness checklist was developed for managing dialysis services during the pandemic.7, 8, 9 Despite these efforts, reports of dialysis patients suffering extreme adversity and even death were reported in the lay press. However, the exact magnitude of service disruption remains unknown.
We conducted a survey to ascertain the impact of COVID pandemic on the care of non-COVID patients with kidney disease during the first 3 weeks of the lockdown.
Methods
An online questionnaire was distributed through e-mail to the director or the heads of the departments of 26 public sector tertiary care teaching institutes and private sector corporate hospitals to complete the survey at the end of the first lockdown period, which lasted for 3 weeks. The invited centers were distributed all over in northern, southern, western, and eastern regions of the country. The authors (NP, SKA, and MR) conceptualized and framed the questionnaire, and NP and MB received answers to the survey questionnaire. NP and VJ performed the data analysis and manuscript writing. The manuscript was circulated to all authors for their feedback, comments. and approval before submission for publication. The questionnaire, the list of the centers, and the region of India to which these centers belong are shown in Supplementary Table S1.
Data Extraction and Analysis
The data were extracted and entered into an Excel sheet and subsequently transferred to the SPSS file (IBM SPSS 20.0 version; IBM Corp, Armonk, NY) for analysis purposes. The data were analyzed to see the effect of lockdown in the public and private sector hospitals in terms of dialysis, and outpatient department and inpatient department related services by comparing data before and after the first lockdown period.
Results
A total of 19 centers responded to the survey, which includes 8 public and 11 private sector hospitals from all parts of India. Together, these centers had 523 dialysis stations for maintenance hemodialysis: the public sector hospitals had 209 stations catering to 972 (range, 18–400) patients, whereas the private sector hospitals had 314 stations, servicing 1545 (range, 40–250) patients on regular dialysis. Thus, a total of 2517 patients were on regular dialysis at these centers before the lockdown (Table 1).
Table 1.
Effect of lockdown on dialysis patients during the COVID-19 pandemic
| Characteristics | Hospitals |
||
|---|---|---|---|
| Government n = 972 | Private n = 1545 | Total n = 2517 | |
| No. of dialysis stations before lockdown | 209 | 314 | 523 |
| No. of dialysis stations after lockdown | 200 | 296 | 496 |
| No. of maintenance dialysis patients | |||
| Before lockdown | 972 | 1545 | 2517 |
| After lockdown | 928 | 1476 | 2404 |
| Patients missing 1 or more HD sessions due to lockdown, n (%) | 419 (47.25) | 291 (18.83) | 710 (28.20) |
| Missing HD with information to HD unit | 198 (20.37) | 133 (8.6) | 331 (13.15) |
| Missing HD without information to HD unit | 105 (10.8) | 84 (5.4) | 189 (7.51) |
| Patients for whom doctors decreased the frequency of HD | 47 (4.83) | 30 (1.94) | 77 (3.06) |
| Permanently missing HD until end of lockdown | 63 (6.48) | 41 (2.65) | 104 (4.13) |
| Death | 06 (0.62) | 03 (0.19) | 09 (0.36) |
| Patients requiring emergency dialysis, n (%) | 33 (3.39) | 36 (2.33) | 69 (2.74) |
| No. of centers facilitating patients’ arrival to HD unit | 4 | 5 | 9 |
| PD patients | |||
| No. of PD patients | 496 | 141 | 637 |
COVID-19, coronavirus disease 2019; HD, hemodialysis; PD, peritoneal dialysis.
After lockdown, the number of serving dialysis stations declined from 523 to 496, by 9 in the public hospitals and 18 in the private sector. The total number of patients on regular dialysis decreased from 2517 to 2404 (from 972 to 928 in public and from 1545 to 1476 in the private sector) (Table 1).
A total of 710 (28.2%) patients missed 1 or more sessions of dialysis during these 3 weeks of lockdown. Of them, 331 (198 in the public sector and 133 in the private sector) missed dialysis sessions after informing the dialysis center of their inability to report to the unit; and 189 patients (105 in the public sector and 84 in the private sector) missed dialysis sessions without any information to their respective dialysis centers. Another 77 patients (47 in public and 30 in public sectors) were advised by the treating nephrologists to reduce dialysis frequency because of accommodating potential dialysis required for the COVID-19–positive patients and curbs imposed by the hospitals (Table 1).
A total of 69 (2.74%) patients (33 in the public sector and 36 in the private sector) who missed dialysis landed in the emergency room for dialysis. A total of 104 (4.13%) patients (63 from public and 41 from private centers) had stopped reporting to the dialysis centers permanently during these 3 weeks, and 9 patients (6 from public and 3 from private) were known to have died. Of note, only 9 hospitals (4 public and 5 private) facilitated the travel of patients to the dialysis center.
COVID Testing and Maintenance Hemodialysis Providers
The Indian Ministry of Health and Family Welfare, Government of India, and Indian Council of Medical Research, New Delhi, issued guidance for testing SARS-CoV-2, which has undergone modification since the initial announcement.10,11 During the survey period, testing for COVID-19 was suggested only for patients with symptoms or history of travel from other countries or contact with SARS-CoV-2–infected individuals. However, the survey showed heterogeneity in this regard, with some hospitals adhering to the advisory, whereas others used their own protocols.
A total of 12 centers (63%), 6 each in public and private, had created cohorting solutions for dialysing SARS-CoV-2–positive or COVID-suspect patients, whereas 7 centers did not have any mechanism to segregate or isolate COVID patients. Of the 12 hospitals, 8 (66.66%) adopted isolation rooms with dedicated machines for dialysis, and 3 (25%) had dedicated machines without isolation, and 1 (8.33%) had dedicated shifts. In the private sector hospitals, 4 have isolated rooms with dedicated machines, and 2 centers had dedicated machines without isolating the patient for suspect or positive patients. Of the 6 public sector hospitals, 3 had isolated rooms with dedicated machines, 2 centers had dedicated machines without isolation, and 1 center pooled all such patients of day to dialyse in a single shift.
Effect on Peritoneal Dialysis
The surveyed centers were managing a total of 637 (range, 0–130) patients on peritoneal dialysis (PD), the public sector had a total of 496 PD (range, 4–130) patients, whereas 141 (range, 0–60) were being managed in private hospitals (Table 1). Overall, 6 centers (3 public and 3 private) had their patients reporting difficulties in the supply of bags during the survey period. None of the patients developed any complication.
Kidney Transplantation
The number of renal transplants in the surveyed centers decreased from 132 (range, 0–25) in the month before the pandemic declaration to 33 (range, 0–15) in the month after pandemic declaration. In public sector hospitals, the number decreased from 69 (range, 0–18) to 16 (range, 0–15), whereas the corresponding numbers were from 63 (range, 0–25) to 17 (range, 0–4) in private sector hospitals. After the imposition of lockdown, only 2 kidney transplants (0 in the public sector and 2 in private sector hospital) were conducted in the surveyed hospitals. A total of 18 SARS-CoV-2–infected kidney transplant recipients were seen during lockdown (16 in public hospitals and 2 in private hospitals).
Effect of Lockdown on Outpatient and Inpatient Services
Data on the impact of lockdown on outpatient department services during the pandemic are presented in Table 2. The total daily attendance in the outpatient departments in the surveyed centers decreased from a total of 1241 (range, 6–250) on the day just before the lockdown, to 95 (range, 0–40) on the day of the survey, representing a decline of 92.3%. During this time, the government allowed telemedicine consultations, which were used by all the 8 public hospitals and 9 private hospitals. The platforms used included phone calls, WhatsApp, e-mail, skype, zoom, and other services.
Table 2.
Effect of lockdown on OPD and IPD services during the COVID-19 pandemic
| Characteristics | Hospitals |
||
|---|---|---|---|
| Government | Private | Total | |
| New patients in OPD per day before | 920 | 321 | 1241 |
| New patients in OPD per day after | 75 | 20 | 95 |
| Advise patients using telemedicine | 8 | 9 | 17 |
| IPD services | |||
| No. of admitted patients before lockdown | 359 | 395 | 754 |
| No. of patients in IPD services on the day of reporting | 159 | 135 | 294 |
COVID-19, coronavirus disease 2019; IPD, inpatient department; OPD, outpatient department.
Seven of the 8 public hospitals and 10 of the 11 private sector hospitals reported data on inpatient department services. The number of patients admitted to renal wards in the 17 hospitals decreased from 754 (range, 8–100) to 294 (range, 0–50). In the public sector, the number of inpatient department patients decreased from 359 (range, 8–80) to 159 (range, 8–40), whereas in the private sector, this number decreased from 395 (range, 10–100) to 135 (range, 0–50).
Effect on Human Resources
The total number of nephrologists in all the centers was 221 (134 in public and 87 in the private sector), and the nonphysician workforce comprised 531 people (260 in public and 271 in the private sector). A total of 15 (10 in public and 5 in private) kidney doctors had been quarantined in all the centers due to incidental contact exposure to patients with COVID during the lockdown period.
Of the 8 public sector hospitals, 6 had the policy of testing themselves if they had flu-like symptoms, and 2 had adopted the policy of self-isolating. Of the 11 private sectors, 9 had a policy of testing if they develop flu-like symptoms, and 2 had self-isolation as per the survey report.
Discussion
This survey clearly demonstrates the impact of the COVID-19 pandemic and lockdown on the care of patients with kidney diseases in India, a low- to middle-income country. We found a reduction in capacity to deliver lifesaving in-center hemodialysis, leading to a reduction in dialysis frequency and dropouts directly attributable to these measures. Although not captured fully, this is likely to have resulted in patient deaths. Further, there was a large reduction in the number of kidney transplant surgeries and patients with kidney diseases that accessed regular outpatient and inpatient care.
Ever since the onset of the pandemic, the ability of countries to address the medical needs of patients with COVID-19 has been under a scanner.10,12 The discussion, however, has been around the adequacy of testing capabilities, availability of hospital beds, ventilators, and PPE.10,13
In recent weeks, concerns have been raised around the impact of such a drastic redesign of the health care system on the care of patients with chronic diseases.13,14 Using the lens of kidney disease, we provide for the first-time objective evidence of such a disruption in India. According to the Global Burden of Disease Study, chronic kidney disease was responsible for 234,345 disability-adjusted life years in 2016 in India.15,16 At the best of times, the Indian health care system is unable to provide care to all the patients with this condition.10,12,17 A large number of patients with end-stage kidney disease are unable to get dialysis and die.17,18 A recent estimate put the number of patients on dialysis at 174,478, which gives a prevalence of approximately 150 per million population, a figure that puts India among the bottom of the countries listed in the Annual Report of the US Renal Data System.19
We show direct evidence of adverse impact on the care of dialysis patients: 28.2% were forced to miss 1 or more dialysis sessions, in many cases requiring emergency dialysis. The reasons were both involuntary because of the patient's inability to reach the dialysis units because of lack of transport, and on medical advice because of reduction in capacity secondary to curtailment in the number of available dialysis stations to meet with the pandemic norms. These patients on regular dialysis do not normally absent themselves wilfully. It is theoretically possible that these patients could have gone to another dialysis unit. However, it is well-known that the number of dialysis units in India is low, and they are mostly located in urban areas. A recent study showed low population coverage of dialysis facilities in India. Almost 60% lived more than 50 km away from a health facility providing dialysis, and nearly a quarter lived more than 100 km away from the facility.18 Interestingly, we noticed a relatively low impact of lockdown on PD, a home-based therapy. Unfortunately, the penetration of PD in India is relatively low; however, a few patients may face problems with supplies for accessories used for the PD.
We also note that patients in the public sector hospitals were more likely to miss dialysis or drop out completely. Most of the Indian population, especially those belonging to low-middle socioeconomic groups, depend on the public sector for usual care, including renal care. These people are more disadvantaged in terms of access to services during the lockdown. A large number of public hospitals were converted into COVID care centers. In some instances, dialysis units were shut down, and patients forced to seek care in other facilities, which in most cases were already full.20,21 In many private hospitals, services were affected due to lockdown restrictions, lack of internal protocols to handle the pandemic, fear of infection to medical staff, and an unwillingness to risk the business from non-COVID patients.22 In an attempt to prevent the inadvertent entry of SARS-CoV-2–infected patients, some hospitals adopted testing policies at variance from that issued by the governments, even requiring that all new patients first undergo testing for the infection irrespective of whether they met the recommended eligibility criteria for testing. Because these patients did not meet the eligibility criteria set down by the government, they were put in an impossible situation, desperately seeking care in multiple hospitals, and needing emergency dialysis.
Until recently, anecdotal reports of interruptions in care leading to death of dialysis patients had been reported in the lay press,20,21 but we provide objective evidence for the same. Deaths could be confirmed in approximately 0.4%, whereas the outcome of the remainder remains unknown at the time of writing. The next most extreme impact was complete dropout, noted in approximately 4.13% of patients. Whereas the outcomes of these patients were not known, it is unlikely that patients on maintenance hemodialysis could survive without dialysis beyond a few days. Some of these deaths could have been prevented with adequate preparedness of dialysis units. Because the lockdown was sudden, units had no time to set up screening areas, isolation rooms, testing facilities for COVID, and arrangement of accessories, like N-95 masks and PPE kits. It was only after reports of death and refusal of dialysis by many hospitals made it to the media,20,21,22 that the attention of the government was drawn, leading to the development of guidance specifically prohibiting denial of dialysis on the grounds of fear of COVID.8,9
Kidney transplant services were suspended throughout the country as part of the suspension of all nonessential surgeries, as was done in other countries.23,24 For some patients, early living donor transplantation is critical for long-term survival because high-quality dialysis cannot be ensured, and delaying transplant can lead to an adverse outcome.25 Although this aspect was not explored, transplant recipients are particularly vulnerable to interruptions in the availability of medications or laboratory monitoring.
The regular outpatient and inpatient services were also affected. All outpatient department services were suspended, and admitted patients were discharged due to a combination of factors, such as lockdown restrictions and lack of internal protocols to handle the pandemic. The outpatient attendance declined by 92.3%, and the number of patients admitted in the renal wards dropped drastically. The long-term impact on the interruption in care cannot be estimated at this time. Even though the survey covered the first 3-week period, the lockdown has already gone on for 9 weeks, and outpatient services have still not resumed in many locations. Private hospitals are resuming service because this has a bearing on the hospital revenue. However, it is expected that the impact of COVID on how services are run will last for several months. It will be a challenge to ensure compliance with practices needed to limit the spread of coronavirus, like social distancing in heavily crowded public hospitals. Many public sector hospitals were converted to COVID hospitals, limiting regular services. Lack of preparedness, anxiety about COVID-19, and preferential shifting of services from non-COVID to COVID care are reasons for nonresumption of services in the public sector hospitals.
The pandemic saw the emergence of telemedicine services in India. New rules were formed and endorsed rapidly by the government and adopted quickly by hospitals.26 Teleconsultations were provided using the existing videoconferencing tools rather than specialized telemedicine platforms. In addition, medical care, howsoever limited, continued to be provided through e-mails, phone calls, and messaging services like WhatsApp. The impact of these services on the adequacy of care provided to the small number of patients who accessed it has not been evaluated
We provide the first data on the impact of COVID on the care of patients with chronic diseases in India. Noncommunicable diseases are responsible for more than half of all premature deaths in India. Even though we present data on renal care, patients with other chronic diseases are likely to have been similarly impacted. There is already evidence that care of patients being managed under the National Tuberculosis Control Program has been affected.27 Similar evidence about the care of patients with cancer has emerged from developed28,29 and developing countries, including India.30 The overall toll of the collateral damage in the form of impact on people with non-COVID conditions will take a long time to evaluate.
Our survey covers the range of health care facilities in all parts of India, both in the private and public sectors. These are large facilities located in major cities with greater resilience compared with smaller hospitals and standalone dialysis units, which are likely to have been even more affected. We observed that many doctors were quarantined because incidental exposure; however, the nonphysician staff, such as technicians and nurses, were more likely to abstain due to a combination of ignorance, fear, and practical difficulties with transport due to lockdown.
This study has a number of limitations. This survey was limited to 19 hospitals and did not cover small facilities in remote locations. It is likely that services were even more badly hit in those areas. Data collected in surveys are likely to be affected by recall bias. However, this survey collected actual data rather than respondents' opinions, which are unlikely to be affected.
To conclude, the COVID pandemic affected the non-COVID patients in India, as shown by the bystander effect on patients with kidney diseases.
Disclosure
VJ has received personal fees from Baxter Health Care, Nephro Plus, and Astra Zeneca, and a grant from Biocon Ltd. All the other authors declared no competing interests.
Acknowledgments
We acknowledge Dr. Aniket Kamble, Lancelot Kidney Centre, Dr. Manas Ranjan Behera, SGPGIMS, Lucknow, and Abhijit Konnur, MPUH, Nadiad for making the data from their center.
Footnotes
Table S1. A list of hospitals participated in the survey from different parts of India and a brief sample of survey questionnaire.
Supplementary Material
References
- 1.World Health Organization Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at:
- 2.Lai C.C., Shih T.P., Ko W.C. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jager K.J., Kovesdy C., Langham R. A single number for advocacy and communication-worldwide more than 850 million individuals have kidney diseases. Kidney Int. 2019;96:1048–1050. doi: 10.1016/j.kint.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 4.COVID-19 pandemic lockdown in India. https://en.wikipedia.org/wiki/COVID19_pandemic_lockdown_in_India Available at:
- 5.UN News COVID-19: lockdown across India, in line with WHO guidance. https://news.un.org/en/story/2020/03/1060132 Available at:
- 6.Ramachandran R., Jha V. Adding insult to injury: kidney replacement therapy during COVID-19 in India. Kidney Int. 2020;98:238–239. doi: 10.1016/j.kint.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Indian Society of Nephrology COVID-19 Working Group Guidelines. http://isn-india.org/UserFiles/Image/COVID 19%20working%20group%20of%20ISN%20India.pdf Available at:
- 8.The George Institute for Global Health Hemodialysis unit preparedness during and after COVID-19 pandemic. COVID-19 Kidney Health Action Group. https://www.georgeinstitute.org.in/media-releases/haemodialysis-unit-preparedness-checklist-developed-to-deliver-safe-dialysis-during Available at:
- 9.Government of India Ministry of Health and Family Welfare. Revised guidelines for dialysis. https://www.mohfw.gov.in/pdf/GuidelinesforDialysisofCovid19Patients.pdf Available at: Accessed May 10, 2020.
- 10.Berendes S., Heywood P., Oliver S., Garner P. Quality of private and public ambulatory health care in low and middle income countries: systematic review of comparative studies. PLoS Med. 2011;8:e1000433. doi: 10.1371/journal.pmed.1000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rajagopalan S., Choutagunta A. Pandemic policy in developing countries: recommendations for India. https://www.mercatus.org/publications/covid-19-policy-brief-series/pandemic-policy-developing-countries-recommendations-india Available at:
- 12.Basu S., Andrews J., Kishore S. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Med. 2012;9:e1001244. doi: 10.1371/journal.pmed.1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bauchner H., Fontanarosa P.B., Livingston E.H. Conserving supply of personal protective equipment—a call for ideas. JAMA. 2020;323:1911. doi: 10.1001/jama.2020.4770. [DOI] [PubMed] [Google Scholar]
- 14.Luyckx V.A., Tonelli M., Stanifer J.W. The global burden of kidney disease and the sustainable development goals. Bull World Health Organ. 2018;96:414-422D. doi: 10.2471/BLT.17.206441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jha V., Ur-Rashid H., Agarwal S.K. The state of nephrology in South Asia. Kidney Int. 2019;95:31–37. doi: 10.1016/j.kint.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Prasad N., Jha V. Hemodialysis in Asia. Kidney Dis (Basel) 2015;1:165-177. doi: 10.1159/000441816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jha V. Current status of end-stage renal disease care in India and Pakistan. Kidney Int. 2013;3:157–160. [Google Scholar]
- 18.Dare A.J., Fu S.H., Patra J. Renal failure deaths and their risk factors in India 2001–13: nationally representative estimates from the Million Death Study. Lancet Glob Health. 2017;5:e89–e95. doi: 10.1016/S2214-109X(16)30308-4. [DOI] [PubMed] [Google Scholar]
- 19.Saran R., Robinson B., Abbott K.C. US Renal Data System 2018 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2019;73(suppl 1):Svii–Sxxii. doi: 10.1053/j.ajkd.2019.01.001. S1–S772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mampatta S.P. How coronavirus crisis is holding India's kidney patients to ransom. https://www.business-standard.com/article/health/how-coronavirus-crisis-is-holding-india-s-kidney-patients-to-ransom-120041100374_1.html Available at:
- 21.Dutt A. How Covid-19 is affecting dialysis patients. https://www.hindustantimes.com/delhi-news/how-covid-19-is-affecting-dialysis-patients/story-zKXDsVd50rrKoY4HrXKLVN.html Available at:
- 22.Simon T., Balasubramanian R. Healthcare during a pandemic: private versus public. https://www.deccanherald.com/opinion/panorama/healthcare-during-a-pandemic-private-versus-public-826224.html Available at: Accessed May 10, 2020.
- 23.Ahn C, Amer H, Anglicheau D, et al. Global Transplantation COVID Report March 2020 [e-pub ahead of print]. Transplantation.https://doi.org/10.1097/TP.0000000000003258. Accessed May 10, 2020. [DOI] [PMC free article] [PubMed]
- 24.Sahay M., Kute V., Prasad N. Corona, COVID and kidney transplantation. Indian J Transplant. 2020;14:1–4. [Google Scholar]
- 25.Aufhauser D.D., Jr., Peng A.W., Murken D.R. Impact of prolonged dialysis prior to renal transplantation. Clin Transplant. 2018;32 doi: 10.1111/ctr.13260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Telemedicine Practice Guidelines. https://www.mohfw.gov.in/pdf/Telemedicine.pdf Available at:
- 27.CIDRAP Experts warn COVID-19 lockdowns could have dire impact on TB. https://www.cidrap.umn.edu/news-perspective/2020/05/experts-warn-covid-19-lockdowns-could-have-dire-impact-tb Available at:
- 28.Bardelli A. Coronavirus lockdown: What I learnt when I shut my cancer lab in 48 hours [e-pub ahead of print]. Nature.https://doi.org/10.1038/d41586-020-00826-7. Accessed May 10, 2020. [DOI] [PubMed]
- 29.Moujaess E., Kourie H.R., Ghosn M. Cancer patients and research during COVID-19 pandemic: a systematic review of current evidence. Crit Rev Oncol Hematol. 2020;150:102972. doi: 10.1016/j.critrevonc.2020.102972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pramesh C.S., Badwe R.A. Cancer management in India during Covid-19. N Engl J Med. 2020;382:e61. doi: 10.1056/NEJMc2011595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.