Abstract
Background:
Pranayama (yogic breathing) has demonstrated numerous beneficial health effects. At present, there are no systematic reviews evaluating the beneficial health effects of pranayama alone as a practice.
Aim:
The aim of this study is to perform a systematic review about the beneficial health effects of pranayama.
Methods:
Data were obtained using a stepwise search process by searching the online PubMed, Web of Science, and SciVerse Scopus databases using keywords. Controlled clinical trials in humans, using “Pranayama” as an intervention with an appropriate control group and evaluating health-related outcomes were selected for inclusion.
Results:
Initial database searching indicated 669 potentially eligible articles, of which 18 studies satisfying the inclusion/exclusion criteria were selected. All were controlled trials, of which 13 were randomized and 1 was a crossover study. Number of participants ranged from 16 to 160, and the duration of pranayama practice varied from 4 days to 6 months. Studies demonstrated a significant effect on cardiorespiratory functions, in patients with bronchial asthma, with the improvement of pulse rate, systolic blood pressure, and respiratory function measurements. Furthermore, reduction in the frequency of attacks, severity, and medication requirement was also observed, with improved quality of life (QOL). In patients with chronic obstructive pulmonary disease, symptom, activity, and impact scores were improved. QOL improvement was also noted in cancer patients.
Conclusions:
Available evidence on pranayama indicates physiological and psychological benefits. Beneficial effects were mostly observed in patients with respiratory diseases such as bronchial asthma. It also helped those with cancer and cardiovascular disease. However, further high-quality randomized trials are required to provide definitive evidence.
Keywords: Pranayama, therapeutic benefit, yogic breathing
Introduction
Complementary and alternative medicine (CAM) is defined by the World Health Organization as the broad set of health-care practices that are not part of that country's own tradition and are not integrated into the dominant health-care system.[1] Over the years, the popularity of CAMs has increased globally, with 70%–80% of the population in developed countries having used some form of CAM during their lifetime.[2] CAMs can be grouped into two broad categories, natural products (herbs, etc.,) and mind-body practices. Mind and body practices are a group of techniques that are administered or taught by a trained practitioner and Yoga is a practice that fall under this domain.[3] Yoga is a 3000-year-old spiritual and ascetic discipline, which has gained wider popularity in the recent past as a CAM.[4] It has been designed to bring harmony to the physical, mental, emotional, and spiritual health of an individual. Therapeutic Yoga is defined as the application of Yoga postures and practice to the treatment of health conditions to prevent, reduce, or alleviate structural, physiological, emotional and spiritual pain, suffering, or limitations.[5] Hatha Yoga, the most widely practiced and studied form of Yoga in the modern world, emphasizes two main aspects, “asana” (physical postures) and “pranayama” (breathing exercises).[6]
Pranayama is a Sanskrit word formed by the conjunction of two words, namely “prana,” meaning breath of life/vital energy, and “ayama,” meaning expansion/regulation/control.[7] It is the yogic art of breathing, consisting of the deliberate modifications of the breathing process, such as rapid diaphragmatic breathing, slow/deep breathing, alternate nostril breathing, and breath holding/retention, which are usually done in a seated posture.[8] Pranayama practices four important aspects of breathing such as Pūraka (inhalation), Recaka (exhalation), Antaḥ kumbhaka (internal breath retention), and Bahiḥ kumbhaka (external breath retention).[7] According to the Yoga-Sutra of Patanjali, which is the most authoritative book on Yoga in India, pranayama is the fourth limb of the eight-fold holistic process defined as Yoga.[9]
Although Yoga has been practiced for 1000s of years in India, its recent popularity has led to much speculation on their effects on the health of individuals, leading to a multitude of studies investigating the impact of these practices on various diseases.[5] Majority of the research studies and reviews evaluating the health benefits of Yoga have considered Yoga “asana” and “pranayama” as a whole, without focusing on pranayama solely.[10,11,12,13] Pranayama alone has demonstrated numerous beneficial health effects, including stress relief,[14] beneficial cardiovascular effect,[14] improved respiratory function,[15] and enhanced cognition.[16] However, at present, there are no systematic reviews evaluating the beneficial health effects of pranayama alone as a practice. Therefore, the present study aims to perform a systematic review of the studies done about the beneficial health effects of pranayama.
Methods
The present systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Literature search
Data were obtained using a stepwise search process by searching the online PubMed® (U. S. National Library of Medicine, USA), Web of Science® (Thomson Reuters, USA), and SciVerse Scopus® (Elsevier Properties S. A, USA) databases using keywords “Pranayama,” “Pranayam,” “Pranayamas,” “Yogic Breathing Exercise,” and “Yoga Breathing Exercise.” The search was restricted to studies on humans with articles published in English before June 31, 2017, while conference proceedings, editorials, commentaries, case reports, qualitative studies, and book chapters/book reviews were excluded. In the second stage, the total hits obtained from searching the above databases were pooled together, and duplicates were removed. Subsequently, the studies were screened by reading the “title,” “abstract,” and “full-text” of the manuscripts. Studies not satisfying the inclusion criteria were excluded at this stage. To obtain additional data, a manual search was performed using the reference lists of articles selected in the final stage. This stepwise search process was conducted by two independent reviewers (RJ and HR), and the final group of articles to be included in the review was determined after an iterative consensus process among the reviewers.
Inclusion/exclusion criteria, data extraction, and analysis
The following inclusion criteria were applied: (a) controlled clinical trials involving human subjects, (b) using “Pranayama” as an intervention with an appropriate non-yoga control group, and (c) evaluating health-related outcomes between the intervention and control groups using either clinical and/or biochemical measurements. Results were limited to studies conducted in humans, published in English. Data were extracted from the included studies by one reviewer (HR) using a standardized form and checked for accuracy by a second reviewer (RJ). The data extracted from each study were as follows: (a) study details (first author, year of publication, country), (b) methods (sample size, age, duration of diabetes, male/female ratio of intervention and control groups), (c) study design (randomization, blinding, duration of the study), (d) details of intervention and control (method and type of yoga breathing exercise, its frequency and duration), and (e) outcome measurements (clinical and biochemical parameters). Discrepancies in the extracted data were resolved by discussion, with the involvement of a third reviewer when necessary (PR). Additional data not available in the published manuscript were obtained from corresponding authors or calculated using the published data.
Quality assessment
The PEDro scale was used to assess the methodological quality of the trials included in the systematic review.[17] Each study was scored from 0 to 10 according to the following criteria: (1) random allocation, (2) concealed allocation, (3) similarity at baseline, (4) subject blinding, (5) therapist blinding, (6) assessor blinding, (7) more than 85% follow-up for at least one key outcome, (8) intention-to-treat analysis, (9) between-group statistical comparison for at least one key outcome, and (10) point and variability measures for at least one key outcome.[17] The PEDro scale categorizes studies as “good” quality (score 6–10), “fair” quality (score 4–5), and “poor” quality (score <4).
Results
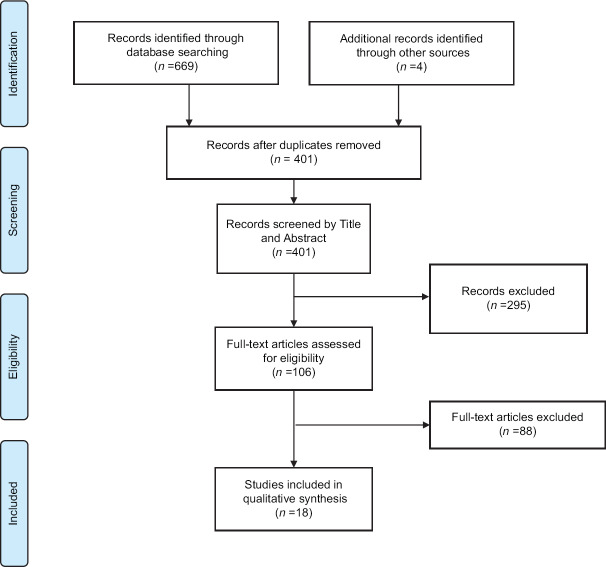
The initial database (PubMed, Web of Science, and SciVerse Scopus) searching indicated 669 potentially eligible articles, of which 401 remained after pooling the articles from the three databases and removing the duplicate article (four additional articles were included from other sources). Of these, 295 were excluded by screening the title and the abstract for failure to meet the inclusion criteria. Of the remaining 106 articles a full-text review yielded, 18 studies satisfying the inclusion/exclusion criteria. Of these, eight studies were conducted on respiratory diseases (including asthma, chronic obstructive pulmonary disease [COPD], and pleural effusion), five studies in patient with malignant diseases and four studies in patients with hypertension and cardiovascular diseases. The search strategy is summarized in Figure 1, and description of the characteristics of each study is provided in Table 1.
Figure 1.
Summarized search strategy (Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram)
Table 1.
Summary of included studies
| Author, Year of publication, Country (referebce) | Objective/s | Study design | Duration of Pranayama | Participants n intervention* n control* | Gender Age | Details of intervention | Outcome measure (s) | Result |
|---|---|---|---|---|---|---|---|---|
| Anitha 2016, India[18] | Effects of Pranayama on the level of anxiety in patients with myocardial infarction | C | 5 days | 30 30 | NM NM | 10 min of Pranayama once a day in the morning for 5 consecutive days | Speilberger State Anxiety Inventory (pre- and post-test score) |
Significantly lower posttest anxiety in intervention group compared to pretest anxiety of IG (P<0.01) with no significant pre-post change in CG |
| Bhatt and Rampallivar 2016, India[19] | Effect of Pranayama on ventilator functions in asthma patients | R, C | 3 months | 40 40 | NM 18-72 years | Different types of Pranayama (Bhastrika, Kapalbhati, Anuloma-Viloma, Bhramri and Ujjayi) Few days of expert supervised sessions, followed by home continuation |
PR, SBP, DBP, RR FVC, FEV1, FEV1/FVC %, PEFR | Significant reduction in PR (P<0.05), SBP (P<0.05) and increase in FVC (P<0.05), PEFR (P<0.05) and FEV1 (P<0.001) in the IG posttest compared to pretest. No significant change in CG |
| Mobini Bidgoli et al., 2016, Iran[20] | Effect of Pranayama on anxiety in patients undergoing coronary angiography | R, C DB | 5 min | 40 40 | Both 59.1 years | Sukha Pranayama for 5 min under the supervision | Spielberger State Anxiety Inventory before, 0.5 and 1 h postintervention |
Significant reduction in mean anxiety score (P<0.0001) in IG at 0.5 and 1 h compared to pretest anxiety of IG. Significant difference in postintervention mean anxiety scores between groups (P<0.01). No significant pre-post change in CG |
| Chakrabarty et al., 2015, India[21] | Effect of Pranayama on cancer-related fatigue in breast cancer patients undergoing radiotherapy | R, C | 1.5 months | 80 80 | Female >18 years |
Pranayama (Nadi shodana, Sheethali, Brahmari) for 30 min twice daily for 5 days a week, for 6 weeks | Cancer fatigue scale | Significant reduction in cancer-related fatigue in IG posttest compared to pretest (P<0.001). Significantly lower posttest cancer related fatigue in IG compared to CG (P<0.01) |
| Chakrabarty et al., 2013, India[22] | Effect of Pranayama on the antioxidant levels in breast cancer patients undergoing radiation therapy | R, C | 1.5 months | 80 80 | Female >18 years |
Pranayama (Nadi shodana, Sheethali, Brahmari) for 30 min twice daily for 5 days a week, for 6 weeks | Serum protein thiols and glutathione | Significantly higher levels of serum protein thiols (P=0.001) and glutathione (P=0.002) posttest in the IG compared to CG |
| Chakrabarty et al., 2016, India[23] | Effect of Pranayama on Emotional changes in breast cancer patients undergoing radiation therapy | R, C | 1.5 months | 80 80 | Female >18 years | Performance of pranayama (Nadi shodana, Sheethali, Brahmari) for 30 min twice daily for 5 days a week, for 6 weeks | Emotions according to an expert-validated scale devised by the investigators | Significantly less posttest negative emotions in the IG compared to CG (P=0.001) |
| Dhruva et al., 2012, USA[24] | Effect of Pranayama on cancer chemotherapy associated symptoms and QOL | R, C | Intervention between two therapy cycles | 8 8 | Both 54.2 years | Weekly Pranayama session lasting for 60 min (inclusive of breath observation, Ujjayi, Kaplabhati, and Nadi shodana pranayama) taught by instructors, and practice of pranayama techniques for 10-15 min, twice daily at home, during two consecutive cycles of chemotherapy | Revised Piper Fatigue Scale, General Sleep Disturbance Scale, Hospital Anxiety and Depression Scale, Perceived Stress Scale and QOL (SF-12) | Significantly improved sleep disturbance (P=0.04), anxiety (P=0.04), and mental component of QOL (P=0.05) in the IG posttest. No significant change in CG |
| Franzblau et al., 2008, USA[25] | Effects of Pranayama on depression in abused women | R, C | 4 days | 20 20 | Female 18-45 years | Division of participants into 4 groups. Intervention types are: practice of yogic breathing (45 min per day); giving testimony (45 min per day); practice of yogic breathing and giving testimony (90 min per day). CG group had no intervention | BDI-II | Significant reduction in BDI-II score posttest in groups who underwent yogic breathing (P<0.005), giving testimony (P<0.005) and the combination of both (P<0.005), but not in the CG |
| Goyal et al., 2014, India[26] | Effect of Pranayama in patients with hypertension (Stage 1) | C | 1.5 months | 25 25 | Both 20-50 years | Practice of pranayama (Nadi shodana: 2-10 min, Chandar bhedi: 2-10 min, Brahmari: 10 cycles, Omkar chanting: 10 cycles) daily for 6 weeks | PR, BP, RPP (HR*SBP) | PR decreased significantly in both the groups as compared to baseline. RPP decreased significantly in both groups compared to baseline, however the decrease was significantly more (P<0.01) in IG in comparison to CG |
| Katiyar and Bihari 2006, India[27] | Effect of Pranayama in patients with COPD | R, C SB | 3 months | 24 24 | Both 52.2 ears | Performance of pranayama (Bhastika, Kapalabhati, Vhasya, Anulom-Vilom, Bhramid and Udgeedh pranayama) for at least 30 min daily, 6 days a week, for 3 months | FVC, FEV1, PEFR, 6 min walk test, PO2, pCO2 and (SGRQ) score | Significant posttest increase of PEF (P<0.05), distance walked in 6 min test (P<0.05) and significant decrease in SGRQ score (P<0.02) in IG compared to CG |
| Kochupillai et al., 2005, India[28] | Effect of Pranayam on Immune Functions in cancer patients | C | 6 months | 21 6 | NM 22-65 years | Pranayama (Ujjayi and Bhastrika) followed by SK (taught at 6 a day workshop) daily at home for 6 months | Immune functions: CD3+, CD4+, CD8+, and NK cell count at baseline, week 1, 12 and 24 | Significant increase of NK cell count at 12 (P=0.001) and 24 weeks (P=0.0001) compared to baseline in IG. Significant increase in NK cell count in IG at week 24 compared to CG (P<0.05) |
| Mourya et al., 2009, India[29] | Effect of Pranayama in patients with hypertension (Stage 1) | R, C | 3 months | 20, 20 20 | Both 20-60 years |
Practice of breathing exercises (fast [n=20] or slow [n=20]) for 15 min twice daily 10-12 h apart, for 3 months | BP and autonomic function tests (SLR, immediate HR response to standing [30:15 ratio], Valsalva ratio, HR variation with respiration [EIR], hand-grip test and cold presser response) | Significant reduction in posttest SBP and DBP in slow-breathing group and fast-breathing group with a greater reduction in slow-breathing group. Significant increase in SLR, 30:15 ratio, EIR, DBP response in hand grip test, and rise in both SBP and DBP in cold pressor test in patients practicing the slow-breathing exercise compared to baseline (P<0.001) and CG (P<0.001) |
| Prakasamma and Bhaduri 1984, India[30] | Effect of Pranayama as a nursing intervention in the care of patients with pleural effusion | C | 20 days | 10 10 | Male 16-50 years |
Anuloma-viloma Pranayama for 30 min daily for 20 days after aspiration of pleural fluid | FVC, FEV1, MVV, PEFR, CE and RS | Significant increase in posttest FVC, CE in IG (P<0.1) compared to CG |
| Prem et al., 2013, India[31] | Effect of Pranayama on QOL and pulmonary function in patients with bronchial asthma | R, CSB | 3 months | 40 40 | Both 18-60 years | Patients trained to perform diaphragmatic breathing, thoracic breathing, upper lobe breathing and full yogic breathing progressing to right nostril breathing, left nostril breathing and alternate nostril breathing for 3-5 days with a session of 60 min each day. They were instructed to practice the exercise at home for 15 min twice daily for 3 months | AQLQ score, Asthma Control Questionnaire and FEV1, FEV1/FVC | IG showed a significant improvement (P=0.042) in total asthma QOL Questionnaire score The study also included a parallel 3rd group who practiced Buteyko techniques as an intervention (n=40) |
| Saxena and Saxena 2009, India[15] | Effect of Pranayama in patients with mild to moderate bronchial asthma | R, C | 3 months | 25 25 | Both 18-45 years |
Practice of breathing exercises (deep breathing, Sasankasana breathing, Anuloma-viloma, Bhramari, Omkara) for 20 min twice daily for 3 months | Symptoms score, FEV1%, PEFR | Significant improvement in posttest symptoms (P<0.01), FEV 1% (P<0.001) and PEFR (P<0.001) in IG compared to CG |
| Singh et al., 1990, UK[32] | Effect of Pranayama on airway reactivity in subjects with bronchial asthma | C CO |
0.5 months | 22 22 | Both 19-54 years | Practice of slow deep breathing through the Pink City Lung Exerciser for 15 min, twice a day, for 2 weeks | FEV1, FVC, PEFR, symptom score, inhaler use, PD20 histamine level | PD20 increased significantly in IG compared to CG (P=0.013) |
| Sodhi et al., 2014, India[33] | Effect of Pranayama Yoga on the QOL in patients with bronchial asthma | R, C | 8 weeks | 60 60 | Both 17-50 years |
Pranayama (deep breathing, Kaplabhati, Bhastrika, Ujjayi and Sukha purvaka pranayama) for 45 min, twice daily on all days of the week for 8 weeks | AQLQ score, number and severity of asthmatic attacks, dosage of medication required | Significant improvement in total score of AQLQ compared to baseline (P<0.01) in IG, but not in CG. Significant reduction in daily number and severity of attacks in the IG posttest compared to baseline (P<0.01) and compared to CG (P<0.05). Significant reduction in the dosage of medication required in the IG compared to baseline (P<0.05), but not in the CG |
| Sodhi et al., 2009, India[34] | Effect of Pranayama on pulmonary functions in patients with bronchial asthma | R, C | 8 weeks | 60 60 | Both IG - 20-50 years CG - 17-50 years |
Yoga breathing exercises (deep breathing, Kaplabhati, Bhastrika, Ujjayi and Sukha purvaka pranayama) for 45 min, twice daily on all days of the week for 8 weeks | PEFR, FVC, FEV1, FEF25-75, FEV1/FVC % | Significant increase in PEFR, FVC, FEV1, FEF25-75, FEV1/FVC % at 4 weeks and 8 weeks in the IG compared to baseline (P<0.01), but not in the CG |
PEF=Peak expiratory flow, AQLQ=Asthma QOL Questionnaire, BP: Blood pressure, BDI-II=Beck depression inventory-II, C=Controlled, CE=Chest expansion, CG=Control group, CO=Cross-over, COPD=Chronic Obstructive Pulmonary Disease, DB=Double blind, DBP=Diastolic BP, FEV1=Forced expiratory volume in 1 s, FVC=Forced vital capacity, IG=Intervention group, NM=Not mentioned, PEFR=PEF rate, PR=Pulse rate, R=Randomized, RPP=Rate pressure product, RR=Respiratory rate, RS=Radiological score, SB=Single blind, SBP=Systolic BP, SGRQ=St. George’s Respiratory Questionnaire, SLR=Standing-to-lying ratio, NK=Natural killer, SLR=Standing-to-lying ratio, QOL=Quality of life, SK=Sudharshan Kriya, HR=Heart rate, SF=Short form, EIR=End inspiratory rate, MVV=Maximal voluntary ventilation, FEF25-75=Forced Expiratory Flow
All were controlled trials, of which 13 were randomized and 1 was a cross-over study. Most studies were conducted in India (n = 14). The number of participants ranged from 16 to 160, and the duration of pranayama practice varied from 4 days to 6 months. Most studies included participants from both genders (n = 10), whereas only females were included four studies and only males were included in one study. The PEDro scale analysis of the methodological quality of the trials included in the systematic review and identified six studies with “poor” quality (score 0–4), 7 studies with “fair” quality (score 4–5), and five studies with “good” quality (score 6–19).
Pranayama in patients with respiratory disease
There were six studies comparing the effects of pranayama in patients with bronchial asthma, whereas one study each included patients with COPD and pleural effusion, respectively. Bhatt and Rampallivar evaluated the effects of Pranayama on ventilatory functions in patients with bronchial asthma.[19] Patients with asthma (n = 80) were divided equally into two groups and the intervention group followed Pranayama in addition to medication for 3 months. Pulse rate (PR), systolic blood pressure (SBP), diastolic blood pressure (DBP), respiratory rate, peak expiratory flow rate (PEFR), forced expiratory volume in the 1st s (FEV1), and forced vital capacity (FVC) were determined in all participants. Test results revealed a significant improvement in PR (P < 0.05), SBP (P < 0.05), FVC (P < 0.05), PEFR (P < 0.05), and FEV1 (P < 0.001) in posttest values compared to pretest values in the intervention group. However, no significant changes were reported in the control group. A similar study by Saxena and Saxena evaluated the effect of pranayama in patients mild-to-moderate bronchial asthma (n = 50) for 12 weeks.[15] FEV1 and PEFR were measured in all participants at the initial stage and after 12 weeks. A significant reduction in symptoms, improvement in FEV1 and PEFR was observed in the intervention group (P < 0.001) as compared to the control group after the practice of pranayama.
A randomized controlled trial (RCT) conducted by Sodhi et al. in patients with bronchial asthma (n = 120) for 2 months, demonstrated a statistically significant increase (P < 0.01) in percentage of predicted PEFR, FEV1, FEF25-75, FVC, and FEV1/FVC% ratio at 4 and 8 weeks in the intervention group who practiced yoga breathing compared to control group.[34] Singh et al., studied the effects of slow-deep breathing through the Pink City Lung (PCL) exerciser, in patients with bronchial asthma.[32] Patients were asked to breathe through a matched placebo device during the control period. Mean FEV1 PEFR, Symptom score, and inhaler use over the past 3 days of each treatment period were assessed. All values improved more with the PCL exerciser than with the placebo device; however, these differences were not significant. A significant increase in the dose of histamine needed to provoke a 20% reduction in FEV1 (PD20) during pranayama breathing was reported with the PCL exerciser (P = 0.013) but not with the placebo device.
Several controlled trials have evaluated the effects of Pranayama on quality of life (QOL) in patients with bronchial asthma. An RCT was carried out in India by Prem et al. to compare the effects of Buteyko and pranayama breathing techniques on QOL in patients with asthma (n = 120).[31] Patients were assigned to three equal groups. The control group (n = 40) underwent routine pharmacological management. Considering the two intervention groups, one group performed pranayama (n = 40), whereas the other group performed Buteyko (n = 40) for a training period of 3 months. Pre- and post-training values of the Asthma Quality of Life Questionnaire (AQLQ), Asthma Control Questionnaire, and pulmonary function tests were noted in all participants. In comparison between the pranayama and control groups, pranayama showed a significant improvement (P = 0.042) in total AQLQ score. However, Buteyko group showed better improvement in total AQLQ score than the pranayama (P = 0.056). Similar results were observed in the study conducted by Sodhi et al., who reported a significant improvement in “symptoms,” “activities,” and “environmental” domains of AQLQ at 8 weeks (P < 0.01) in the yoga group than the control group. They also observed a significant reduction in daily number and severity of attacks, and the dosage of medication required at 4 and 8 weeks (P < 0.01) in the yoga group compared to the baseline.[33]
An RCT conducted by Katiyar and Bihari evaluated the role of pranayama (3 months) in the rehabilitation of patients with COPD (n = 48).[27] The St. George's Respiratory Questionnaire (SGRQ) was used to measure the overall health status of the participants, while spirometry tests, 6-min walk test (6-MWT), and arterial blood gas (ABG) analysis were done in all participants. The study results indicated statistical significant decrease in the symptom score (P = 0.03), activity score (P < 0.005), impact score (P < 0.008), and total SGRQ score (P = 0.02) in the interventional group, but not in the control group. The increase in FVC and FEV1 in the interventional group was insignificant, but the increase in the PEF was statistically significant (P = 0.05) only in the interventional group. No significant changes were reported in either group in ABG analysis values. Considering the 6-MWT results, a small but significant increase in the distance (P = 0.05) were reported in the interventional group. Pranayama has also demonstrated beneficial effects on respiratory function (FVC) and chest expansion postpleural aspiration in patients with pleural effusions.[30]
Pranayama in patients with malignant diseases
A total of five studies assessed the short-term effects of pranayama in patients with malignancy and evaluated cancer-related fatigue, emotional changes, QOL, anti-oxidant status, and immune functions. Three studies were reported in patients with breast carcinoma, whereas the other studies involved patients with different types of malignant diseases undergoing chemoradiotherapy.[21,23]
Chakrabarty et al. assessed the effect of pranayama on cancer-related fatigue and emotional aspects of breast cancer patients (n = 160) undergoing radiation therapy.[21,23] Fatigue level was assessed using the cancer fatigue scale, and emotional aspects were assessed using five items as part of the assessment of cancer-related fatigue. The study results indicated a significant difference (P < 0.001) in the pre- and post-test scores of cancer-related fatigue in the interventional group compared to the control group (P < 0.001). Furthermore, a significant reduction (P < 0.01) in emotions such as worry, anxiety, and frustration was reported in breast cancer patients who performed pranayama compared to the control group. The effect of pranayama on anti-oxidant status was also evaluated in the same group of patients.[22] The results revealed that the interventional group had significantly higher posttest levels (P < 0.001) of serum protein thiols compared to the control group.
Dhruva et al. tested the effects of pranayama on QOL in patients receiving cancer chemotherapy (n = 16).[24] Patients receiving two consecutive cycles of cancer chemotherapy (cycle A and B) were randomized to receive pranayama immediately (interventional group) or after a waiting period (control group). The control group received only usual care during cycle A and pranayama along with usual care in cycle B. The symptom and QOL measures were self-administered. Fatigue level was measured using the revised Piper Fatigue Scale. Sleep disturbance of the participants was measured using the General Sleep Disturbance Scale. Anxiety and depression were measured by means of the 14-item Hospital Anxiety and Depression Scale. Stress was measured using the Perceived Stress Scale. The Short Form-12 version one was used to measure QOL. The study results indicated significant improvements in sleep disturbance (P = 0.04), level of anxiety (P = 0.04), and mental QOL (P = 0.05) of the participants who followed yoga breathing between the two consecutive cycles of chemotherapy (interventional group). Effect of pranayama on immune function of cancer patients in remission was assessed by Kochupillai et al.[28] Cancer patients (n = 21) who had completed the standard treatment had statistically significant (P < 0.001) increase in natural killer cells at 12 and 24 weeks of practice of pranayama and Sudarshan Kriya, with no similar effect observed in the control group.
Pranayama in patients with cardiovascular diseases
Anitha conducted a hospital-based study to evaluate the effect of pranayama on the level of anxiety in patients presenting with myocardial infarction (n = 60).[18] Standardized Spielberger State Anxiety Rating Scale (self-administered) was used to assess the level of anxiety. The study reported a statistically significant (P < 0.01) improvement in posttest anxiety in the interventional group compared to the control group. Similar beneficial results on anxiety were observed in another study on patients undergoing coronary angiography, where the mean anxiety score (Spielberger State Anxiety Rating Scale) of the interventional group was significantly decreased (P = 0.0001) after performing pranayama, but not in the control group.[20]
Goyal et al. carried out a study to evaluate the effect pranayama on PR, blood pressure and rate pressure product (RPP) (SBP * PR) in mild hypertensive patients (n = 50).[26] SBP decreased significantly in the intervention group and the decrease was significant as compared to control group. PR decreased significantly in both the groups as compared to baseline; however, the decrease was similar in both groups. RPP decreased significantly in both groups as compared to baseline; however, the decrease was significantly more (P < 0.01) in interventional group when compared to the control group. A hospital-based RCT by Mourya et al. investigated the effect of slow and fast yogic breathing exercises on blood pressure and autonomic function in patients with essential hypertension.[29] Patients with Stage 1 hypertension (n = 60) were equally divided into three groups: Group 1 (control group), whereas Group 2 and Group 3 followed slow and fast breathing exercises, respectively, for 3 months. The study results revealed a significant decrease in SBP and DBP in both Group 2 (P < 0.001) and Group 3 (P < 0.01). However, the decrease was greater in Group 2, with no significant changes observed in control group.
Pranayama in other groups of patients
Franzblau et al. tested the short-term effects of having battered women's provide testimony about their abuse and/or the effects of yogic breathing on depression which measured by the Beck Depression Inventory (BDI)-II.[25] Participants (n = 40) who self-identified as verbally, emotionally, physically, and/or sexually abused within the past 2 years were assigned into four groups as: testimony only, yogic breathing only, testimony and yogic breathing, and control. The study results indicated a significant reduction in posttest BDI-II score in groups who underwent yogic breathing (P < 0.005), giving testimony (P < 0.005), and the combination of both (P < 0.005), but not in the control group.
Discussion
The present systematic review is the first to systematically evaluate the literature on the beneficial health effects of Pranayama yoga practice. We observed a significant effect on the cardio-respiratory functions, in patients with bronchial asthma, with the improvement of PR, SBP, FVC, FEV1, and PEFR. Furthermore, reduction in the frequency of attacks, severity, and medication requirement was also observed, in addition to improved QOL. In patients with COPD, symptom, activity, and impact scores were improved with Pranayama practice. QOL improvement has been noted in cancer patients, with improved emotions, fatigue, sleep, and reduced anxiety. Reduction in anxiety has also been observed in patients with cardiovascular diseases. In patients with hypertension, both SBP and DBP were reduced with Pranayama practices. Hence, the available evidence from controlled studies indicates both physiological and psychological benefits of Pranayama.
The predominant beneficial effect of Pranayama practice was observed in patients with respiratory illnesses such as bronchial asthma. Several mechanisms are thought to be responsible for the beneficial respiratory effects of Pranayama. Pranayama may allow bronchio-dilatation by correcting abnormal breathing patterns and reducing muscle tone of respiratory muscles.[35] Furthermore, yoga training is likely to improve the strength of expiratory as well as inspiratory muscles, with resultant improvement in pulmonary function.[36] For example, “Bhastrika” Pranayama is a type of breathing, in which one breath rapidly and forcefully, exercising both inspiratory and expiratory muscles.[37] Furthermore, breathing exercises like Kapalbhati, which utilizes the abdominal and diaphragmatic muscles train the subject to make full use of the diaphragm and abdominal muscles in breathing.[38] This is also likely to help in the removal of secretions from bronchial tree and the alveoli, making room for more air.[37] Lung inflation near to total lung capacity is known to be a major stimulus for the release of lung surfactant into alveolar spaces, leading to increased lung compliance.[39] The slow and gentle breathing in some of the Pranayama techniques reduces frictional stress, thereby stabilizing the mast cell degranulation, thereby reducing airway inflammation and airway obstruction.[38] The deep inspiration, retention of air, and slow expiration increases the overall capacity of the lungs and gradually improves the pulmonary functions.[38] This improved pulmonary function is likely to be responsible for the observed reduction in severity, frequency, and medication requirement in patients with bronchial asthma, which ultimately is responsible for the enhanced QOL in these patients. The improvements observed in COPD are also likely to be due to similar mechanisms. However, it is important to note that there has been a case report of occurrence of pneumothorax with practice of Kapalabhati Pranayama.[40] Hence, appropriate selection of the most suitable Pranayama methods, careful supervision, and training may be required in patients with already compromised respiratory functions.
Another long-term effect of pranayamic breathing is the improvement in autonomic function.[41] Recent controlled trials suggest that yoga training programs can reduce perceived stress, improve mood, and lower catecholamine and cortisol levels, cardiovascular response to stress, blood pressure, and other indices of sympathetic activation in both healthy and clinical populations.[42] Yogic practices shift the autonomic nervous system balance from primarily sympathetic to parasympathetic, by directly enhancing parasympathetic output, possibly through vagal stimulation, resulting in positive changes in cardiovagal function and associated neuroendocrine, hemodynamic, and inflammatory profiles, in sleep and affect, and in related downstream metabolic parameters.[42] Slow pranayamic breathing generates inhibitory signals and hyperpolarizing current within neural and nonneural tissue by mechanically stretching tissues during breath inhalation and retention.[43] It is likely that these inhibitory impulses in cooperation with hyperpolarization current initiate the synchronization of neural elements in the central nervous system, peripheral nervous system, and surrounding tissues ultimately causing shifts in the autonomic balance toward parasympathetic dominance.[43] This shift toward parasympathetic dominance is likely to be responsible for the observed cardiovascular effects of Pranayama practice, such as reduced heart rate, SBP, and DBP in patients with hypertension.
Our results also indicate several psychological benefits of Pranayama practice, including improved emotional responses, fatigue, stress, and reduced anxiety in cancer patients, as well as in patients with cardiovascular disease. Increased melatonin production after a regimen of slow breathing pranayamic exercises has been attributed to pranayama's tendency to create a sense of relaxation and well-being in the subject.[44] Breath-holding, an essential part of pranayama, is known to induce theta waves in the electroencephalography.[43] The particular contribution of pranayama to stress/anxiety reduction might also be contributed by the sympathetic-parasympathetic shift. Vagal afferents from peripheral receptors are connected with the nucleus tractus solitarius from which fibers ascend to the thalamus, limbic areas, and anterior cortical areas.[16] During controlled breathing exercises, stretch of lung tissue produces inhibitory signals in the vagus nerve, which ultimately shifts the autonomic nervous system into parasympatho dominance, that results in a calm and alert state of mind.[43] Furthermore, during both fast and slow types of pranayama practice, when participants intentionally focus on breathing at different frequencies of respiration and intend to relax, attention is drawn away from extraneous distracting stimuli.[16] Hence, it is evident that the beneficial psychological effects observed with Pranayama practice are likely to be a result of both neurohumoral mechanisms, predominantly involving the sympathetic-parasympathetic nervous system.
The present study has several notable strengths, including the comprehensive and easily replicable search strategy applied to three major medical databases. In addition, we systematically selected the studies through the application of well-defined inclusion/exclusion criteria. However, there are several limitations that need to be considered before drawing conclusions from the results of the present analysis. There was minimal uniformity between the different studies. The yogic interventions, outcomes assessed, study populations, sample sizes, and duration of intervention in the studies were heterogeneous. This prevented the authors from conducting a meta-analysis of the included studies. Furthermore, in the quality assessment using the PEDro scoring system, majority of the studies had a “poor” (n = 6) and “fair” score (n = 7). However, one of the reasons for the low scores in these studies might have been the use of single blinding, due to the inherent nature of the studies.
Conclusions
Pranayama is a simple, cost-effective method with evidence indicating the presence of therapeutic benefits for diseased populations. The available evidence indicates both physiological and psychological benefits. Beneficial effects were mostly observed in patients with respiratory diseases such as bronchial asthma. It also helped to reduced fatigue, anxiety, and other emotional responses in those with cancer and cardiovascular disease. However, the studies were heterogeneous, in terms of the methodological quality, pranayama technique used and sample size. Therefore, further high-quality RCTs are required to provide definitive evidence and also to enable a deeper understanding of the underlying mechanisms of the therapeutic benefits of pranayama.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. WHO Traditional Medicine Strategy 2014-2023. Geneva: World Health Organization; 2013. [Google Scholar]
- 2.World Health Organization. Traditional Medicine Fact Sheet N134. Geneva: World Health Organization; 2008. [Google Scholar]
- 3.National Center for Complementary and Integrative Health. Strategic Plan 2016: Exploring the Science of Complementary and Integrative Health. Maryland: National Center for Complementary and Integrative Health; 2016. [Google Scholar]
- 4.Williams K, Steinberg L, Petronis J. Therapeutic application of iyengar yoga for healing chronic low back pain. Int J Yoga Ther. 2003;13:55–67. [Google Scholar]
- 5.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4:49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang K. A review of yoga programs for four leading risk factors of chronic diseases. Evid Based Complement Alternat Med. 2007;4:487–91. doi: 10.1093/ecam/nem154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nivethitha L, Mooventhan A, Manjunath NK. Effects of various Prāṇāyāma on cardiovascular and autonomic variables. Anc Sci Life. 2016;36:72–7. doi: 10.4103/asl.ASL_178_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joshi KS. Yogic Pranayama: Breathing for Long Life and Good Health. India: Orient Paperbacks; 2006. [Google Scholar]
- 9.Hartranft C. The Yoga-Sutra of Patanjali: A New Translation With Commentary. India: Shambhala Classics; 2003. [Google Scholar]
- 10.Büssing A, Michalsen A, Khalsa SB, Telles S, Sherman KJ. Effects of yoga on mental and physical health: A short summary of reviews. Evid Based Complement Alternat Med. 2012;2012:165410. doi: 10.1155/2012/165410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khalsa SB. Yoga as a therapeutic intervention: A bibliometric analysis of published research studies. Indian J Physiol Pharmacol. 2004;48:269–85. [PubMed] [Google Scholar]
- 12.Jeter PE, Slutsky J, Singh N, Khalsa SB. Yoga as a therapeutic intervention: A bibliometric analysis of published research studies from 1967 to 2013. J Altern Complement Med. 2015;21:586–92. doi: 10.1089/acm.2015.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cramer H, Lauche R, Dobos G. Characteristics of randomized controlled trials of yoga: A bibliometric analysis. BMC Complement Altern Med. 2014;14:328. doi: 10.1186/1472-6882-14-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma VK, Trakroo M, Subramaniam V, Rajajeyakumar M, Bhavanani AB, Sahai A. Effect of fast and slow pranayama on perceived stress and cardiovascular parameters in young health-care students. Int J Yoga. 2013;6:104–10. doi: 10.4103/0973-6131.113400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saxena T, Saxena M. The effect of various breathing exercises (pranayama) in patients with bronchial asthma of mild to moderate severity. Int J Yoga. 2009;2:22–5. doi: 10.4103/0973-6131.53838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma VK, Rajajeyakumar M, Velkumary S, Subramanian SK, Bhavanani AB, Madanmohan, et al. Effect of fast and slow pranayama practice on cognitive functions in healthy volunteers. J Clin Diagn Res. 2014;8:10–3. doi: 10.7860/JCDR/2014/7256.3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust J Physiother. 2009;55:129–33. doi: 10.1016/s0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 18.Anitha A. Effectiveness of pranayama on level of anxiety among clients with myocardial infarction. Res J Pharm Biol Chem Sci. 2016;7:2857–9. [Google Scholar]
- 19.Bhatt A, Rampallivar S. Effect of pranayam on ventilatory functions in patients of bronchial asthma. J Evol Med Dent Sci. 2016;5:1453–55. [Google Scholar]
- 20.Mobini Bidgoli M, Taghadosi M, Gilasi H, Farokhian A. The effect of sukha pranayama on anxiety in patients undergoing coronary angiography: A single -blind randomized controlled trial. J Cardiovasc Thorac Res. 2016;8:170–5. doi: 10.15171/jcvtr.2016.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chakrabarty J, Vidyasagar M, Fernandes D, Joisa G, Varghese P, Mayya S. Effectiveness of pranayama on cancer-related fatigue in breast cancer patients undergoing radiation therapy: A randomized controlled trial. Int J Yoga. 2015;8:47–53. doi: 10.4103/0973-6131.146062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chakrabarty J, Vidyasagar MS, Fernandes D, Bhat V, Nagalakshmi, Joisa G, et al. Effectiveness of pranayama on the levels of serum protein thiols and glutathione in breast cancer patients undergoing radiation therapy: A randomized controlled trial. Indian J Physiol Pharmacol. 2013;57:225–32. [Google Scholar]
- 23.Chakrabarty J, Vidyasagar MS, Fernandes D, Mayya S. Emotional aspects and pranayama in breast cancer patients undergoing radiation therapy: A randomized controlled trial. Asia Pac J Oncol Nurs. 2016;3:199–204. doi: 10.4103/2347-5625.177390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dhruva A, Miaskowski C, Abrams D, Acree M, Cooper B, Goodman S, et al. Yoga breathing for cancer chemotherapy-associated symptoms and quality of life: Results of a pilot randomized controlled trial. J Altern Complement Med. 2012;18:473–9. doi: 10.1089/acm.2011.0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Franzblau SH, Echevarria S, Smith M, Van Cantfort TE. A preliminary investigation of the effects of giving testimony and learning yogic breathing techniques on battered women's feelings of depression. J Interpers Violence. 2008;23:1800–8. doi: 10.1177/0886260508314329. [DOI] [PubMed] [Google Scholar]
- 26.Goyal R, Lata H, Walia L, Narula MK. Effect of pranayama on rate pressure product in mild hypertensives. Int J Appl Basic Med Res. 2014;4:67–71. doi: 10.4103/2229-516X.136776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katiyar S, Bihari S. Role of pranayama in rehabilitation of COPD patients – A randomized controlled study. Indian J Allergy Asthma Immunol. 2006;20:98–104. [Google Scholar]
- 28.Kochupillai V, Kumar P, Singh D, Aggarwal D, Bhardwaj N, Bhutani M, et al. Effect of rhythmic breathing (Sudarshan Kriya and pranayam) on immune functions and tobacco addiction. Ann N Y Acad Sci. 2005;1056:242–52. doi: 10.1196/annals.1352.039. [DOI] [PubMed] [Google Scholar]
- 29.Mourya M, Mahajan AS, Singh NP, Jain AK. Effect of slow- and fast-breathing exercises on autonomic functions in patients with essential hypertension. J Altern Complement Med. 2009;15:711–7. doi: 10.1089/acm.2008.0609. [DOI] [PubMed] [Google Scholar]
- 30.Prakasamma M, Bhaduri A. A study of yoga as a nursing intervention in the care of patients with pleural effusion. J Adv Nurs. 1984;9:127–33. doi: 10.1111/j.1365-2648.1984.tb00353.x. [DOI] [PubMed] [Google Scholar]
- 31.Prem V, Sahoo RC, Adhikari P. Comparison of the effects of Buteyko and pranayama breathing techniques on quality of life in patients with asthma – A randomized controlled trial. Clin Rehabil. 2013;27:133–41. doi: 10.1177/0269215512450521. [DOI] [PubMed] [Google Scholar]
- 32.Singh V, Wisniewski A, Britton J, Tattersfield A. Effect of yoga breathing exercises (pranayama) on airway reactivity in subjects with asthma. Lancet. 1990;335:1381–3. doi: 10.1016/0140-6736(90)91254-8. [DOI] [PubMed] [Google Scholar]
- 33.Sodhi C, Singh S, Bery A. Assessment of the quality of life in patients with bronchial asthma, before and after yoga: A randomised trial. Iran J Allergy Asthma Immunol. 2014;13:55–60. [PubMed] [Google Scholar]
- 34.Sodhi C, Singh S, Dandona PK. A study of the effect of yoga training on pulmonary functions in patients with bronchial asthma. Indian J Physiol Pharmacol. 2009;53:169–74. [PubMed] [Google Scholar]
- 35.Jain N, Srivastava RD, Singhal A. The effects of right and left nostril breathing on cardiorespiratory and autonomic parameters. Indian J Physiol Pharmacol. 2005;49:469–74. [PubMed] [Google Scholar]
- 36.Madanmohan, Thombre DP, Balakumar B, Nambinarayanan TK, Thakur S, Krishnamurthy N, et al. Effect of yoga training on reaction time, respiratory endurance and muscle strength. Indian J Physiol Pharmacol. 1992;36:229–33. [PubMed] [Google Scholar]
- 37.Subbalakshmi NK, Saxena SK, Urmimala JA. Immediate effect of nadi -shodhana pranayama on some selected parameters of cardiovascular, pulmo-nary and higher functions of brain. Thai J Physiol Sci. 2005;18:10–6. [Google Scholar]
- 38.Karthik PS, Chandrasekhar M, Ambareesha K, Nikhil C. Effect of pranayama and suryanamaskar on pulmonary functions in medical students. J Clin Diagn Res. 2014;8:BC04–6. doi: 10.7860/JCDR/2014/10281.5344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Joshi LN, Joshi VD, Gokhale LV. Effect of short term 'pranayam' practice on breathing rate and ventilatory functions of lung. Indian J Physiol Pharmacol. 1992;36:105–8. [PubMed] [Google Scholar]
- 40.Johnson DB, Tierney MJ, Sadighi PJ. Kapalabhati pranayama: Breath of fire or cause of pneumothorax? A case report. Chest. 2004;125:1951–2. doi: 10.1378/chest.125.5.1951. [DOI] [PubMed] [Google Scholar]
- 41.Singh S, Malhotra V, Singh KP, Madhu SV, Tandon OP. Role of yoga in modifying certain cardiovascular functions in type 2 diabetic patients. J Assoc Physicians India. 2004;52:203–6. [PubMed] [Google Scholar]
- 42.Innes KE, Selfe TK. Yoga for adults with type 2 diabetes: A systematic review of controlled trials. J Diabetes Res. 2016;2016:6979370. doi: 10.1155/2016/6979370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jerath R, Edry JW, Barnes VA, Jerath V. Physiology of long pranayamic breathing: Neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Med Hypotheses. 2006;67:566–71. doi: 10.1016/j.mehy.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 44.Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, et al. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10:261–8. doi: 10.1089/107555304323062257. [DOI] [PubMed] [Google Scholar]