Abstract
Purpose:
To report two cases of typical multiple evanescent white dot syndrome (MEWDS), in which swept-source optical coherence tomography angiography (SS-OCTA) revealed transient areas of flow deficit at the level of the choriocapillaris.
Methods:
The SS-OCTA images of two female patients with typical MEWDS were analyzed at the onset of the disease and during follow-up.
Results:
The patients were aged 24 and 25 years, respectively. Previous medical history was unremarkable in both cases. The diagnosis of MEWDS was made on the basis of typical clinical findings and results of fundus autofluorescence, fluorescein angiography, and optical coherence tomography. At presentation, SS-OCTA showed a few small hypointense areas of flow deficit at the level of the choriocapillaris in both cases. During follow-up, SS-OCTA showed complete resolution of choriocapillaris flow voids.
Conclusion:
Both our patients with typical acute MEWDS showed SS-OCTA multifocal small areas of flow reduction at the level of the choriocapillaris, with full recovery during the follow-up. This finding supports the hypothesis of transient, primary, or secondary choriocapillaris hypoperfusion in typical MEWDS.
Keywords: Choriocapillaris, Optical coherence tomography angiography, Uveitis, White dot syndrome, Multiple evanescent white dot syndrome
INTRODUCTION
Multiple evanescent white dot syndrome (MEWDS) is a rare inflammatory disorder of unknown etiology that usually occurs unilaterally in healthy, young, white, myopic females.1 The condition typically causes multiple small, deep, white retinal lesions associated with macular granularity, which is a uniform and distinguishing feature of MEWDS. Other common clinical features include visual acuity reduction, mild vitritis, and optic disc swelling. The natural course of MEWDS is usually benign, with rapid resolution of white dots, and full recovery of visual function within weeks.1 Although the diagnosis of MEWDS is mainly clinical, multimodal imaging including conventional and new imaging modalities may be very useful in confirming the diagnosis and monitoring the disease course.1,2,3 Although the pathophysiology of MEWDS remains unclear, potential primary sites of disease process have been suggested, including outer retina, retinal pigment epithelium (RPE), and inner choroid.1,2,3,4,5 Data from recent optical coherence tomography angiography (OCTA) studies revealed a completely normal choriocapillaris flow on OCTA in all patients with MEWDS. This may suggest that the disease primarily corresponds to inflammation at the outer photoreceptor level, rather than the choriocapillaris, leading to a photoreceptoritis.3
We herein report two typical MEWDS cases in which swept-source OCTA (SS-OCTA) revealed transient areas of choriocapillaris flow deficit.
CASE REPORTS
Case 1
A 25-year-old woman was referred to our department with a 4-day history of sudden blurring vision and visual field defect in the left eye. The patient had an unremarkable previous medical history. Best corrected visual acuity was 20/20 in the right eye and 20/100 in the left eye. The pupils were equally round and reactive to light with no relative afferent pupillary defect. The results of the anterior segment examination were unremarkable, and there were no vitreous cells in either eye. Fundus examination of the left eye revealed multifocal, coalescent, deep, yellow–white dots in the posterior pole and mid-periphery and foveal granularity. The fundus of the right eye was unremarkable. Near-infrared fundus autofluorescence imaging showed hypoautofluorescent spots, corresponding to the white dots seen clinically. Fluorescein angiography revealed early punctate hyperfluoresence and late staining with a “wreath-like” configuration around the fovea and optic disc staining. Structural SS-OCT showed disruption of the ellipsoid zone and subretinal accumulations of hyperreflective material over the RPE [Figure 1]. Structural en-face SS-OCT of the outer retina revealed hyporeflective spots corresponding to the areas of ellipsoid zone disruption. The 3 mm × 3 mm SS-OCT angiograms (DRI OCT Triton plus; Topcon) showed small areas of loss of signal at the level of the choriocapillaris. There was no evidence of signal attenuation related to the overlying inflammatory tissue to explain the reduced inner choroidal flow [Figure 2]. All imaging findings in the right eye were normal. Six months after the initial presentation, visual acuity in the left eye was 20/20, with normal findings on fundus examination. Structural SS-OCT showed restitution of the outer retinal layers. SS-OCTA showed a complete resolution of choriocapillaris flow voids [Figures 1 and 2].
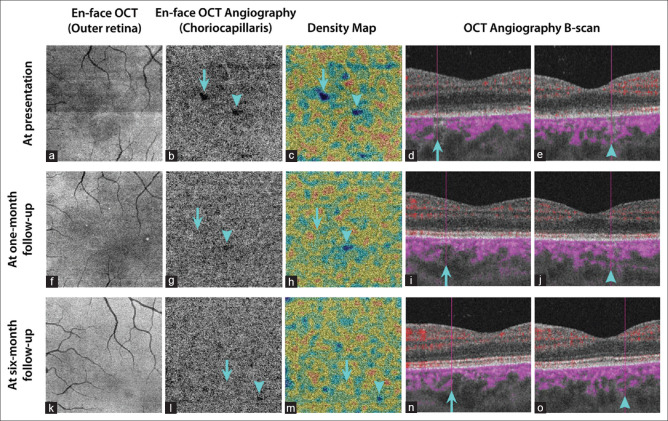
Figure 1.
Multimodal imaging of a 25-year-old patient during the acute phase of multiple evanescent white dots syndrome. (a) Composite color fundus photograph of the left eye showing multifocal, deep, white lesions in the posterior pole and mid-periphery associated with foveal granularity. (b) Structural swept-source optical coherence tomography (SS-OCT) demonstrating disruption of the ellipsoid zone and accumulations of a hyperreflective material over the retinal pigment epithelium. (c) Near-infrared fundus autofluorescence showing multiple hypoautofluorescent spots. (d) Fluorescein angiography showing late diffuse multifocal hyperfluorescence with a “wreath-like” configuration around the fovea and optic disc leakage. (e) Composite color fundus photograph of the left eye, 6 months after the initial presentation, showing the resolution of the white retinal lesions. (f) Structural SS-OCT, 6 months after the first presentation, showing normal outer retinal layers
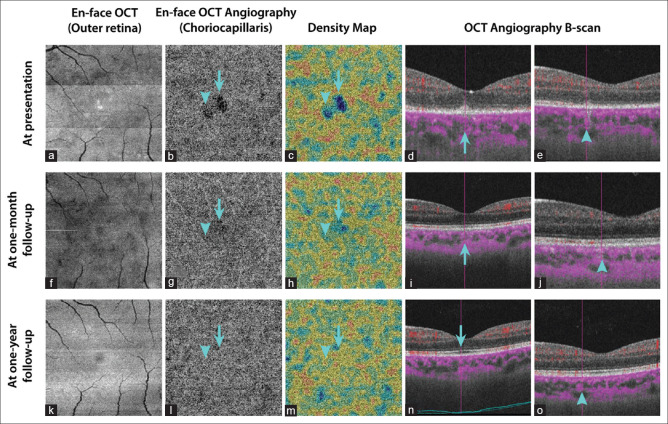
Figure 2.
En-face swept-source optical coherence tomography (SS-OCT) and SS-OCT angiography (SS-OCTA) at presentation in the same patient of Figure 1 (a-e): Structural en-face SS-OCT (3 mm × 3 mm scans) taken at the level of the outer retina revealing hyporeflective areas corresponding to the ellipsoid zone disruptions. En-face SS-OCTA at the level of choriocapillaris showing two small areas of hypointense flow deficit, which are highlighted by respectively an arrow and an arrowhead, with decreased flow signal in the choriocapillaris on respective SS-OCTA B-scans. No evidence of any shadow graphic or projection artifacts is appreciable. En-face SS-OCT and SS-OCTA, at 1-month follow-up (f-j): En-face SS-OCTA, 1 month after the initial presentation, showing the resolution of the choriocapillaris hypointense areas with the restitution of flow signals in the choriocapillaris on SS-OCTA B-scan, and the persistence of a diffuse hyporeflective area on en-face SS-OCT at the level of the outer retina. En-face SS-OCT and SS-OCTA, at 6-month follow-up (k-o): En-face SS-OCT at the level of the outer retina and SS-OCTA at the level of the choriocapillaris showing quite normal findings
Case 2
A 24-year-old woman presented with a 1-day history of sudden vision loss in her left eye. The patient had an unremarkable previous medical history. Best corrected visual acuity was 20/20 in the right eye and 20/200 in the left eye. The pupils were reactive to light with no relative afferent pupillary defect. The anterior segment and the vitreous of both eyes were quiet. Fundus examination of the left eye demonstrated multiple, deep, yellow–white spots in the posterior pole and mid-periphery, foveal granularity, and optic disc hyperemia. Fundus examination of the right eye showed normal findings. Near-infrared fundus autofluorescence imaging of the left eye showed hypoautofluorescent spots. Fluorescein angiography showed early patchy hyperfluorescence and late staining of white dots and optic disc leakage. Structural SS-OCT showed disruption of the ellipsoid zone with areas of the subretinal hyperreflective material of variable shapes and sizes [Figure 3]. Structural en-face SS-OCT of the outer retina revealed hyporeflective spots corresponding to the areas of ellipsoid zone disruption, as well as hyperreflective dots corresponding to the intraretinal hyperreflective foci resting over the RPE. The 3 mm × 3 mm SS-OCT angiograms showed small areas of loss of signal in the choriocapillaris. Some areas of loss of signal at the level of the choriocapillaris were associated with the overlying inflammatory outer retina or RPE changes [Figure 4]. All imaging findings in the right eye were unremarkable. One year after the first presentation, visual acuity was 20/20 in the left eye, with no evident lesion on fundus examination. Structural SS-OCT showed normal outer retinal layers. SS-OCTA showed no areas of choriocapillaris flow deficit [Figures 3 and 4].
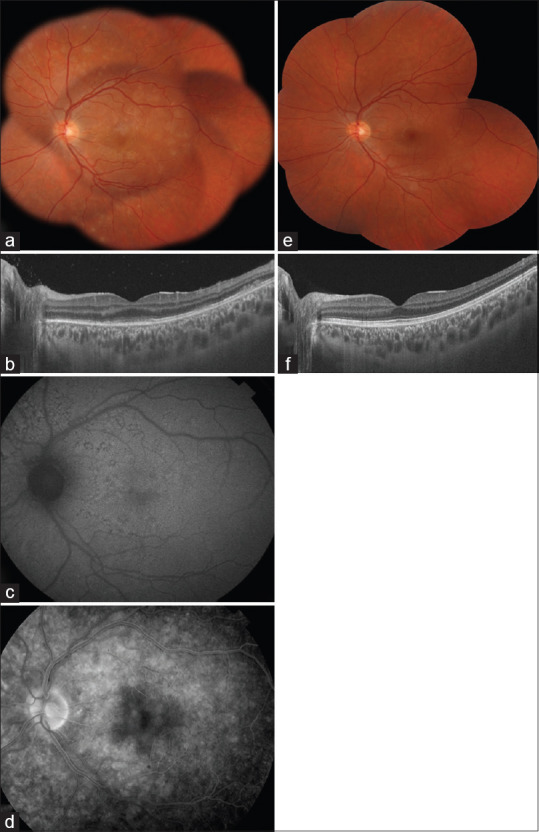
Figure 3.
Multimodal imaging of a 24-year-old patient during the acute phase of multiple evanescent white dots syndrome. (a) Composite color fundus photograph of the left eye showing multiple, deep, white dots in the posterior pole and mid-periphery and macular granularity. (b) Structural swept-source optical coherence tomography (SS-OCT) demonstrating disruption of the ellipsoid zone with small accumulations of hyperreflective material resting over the retinal pigment epithelium and extending toward the outer nuclear layer. (c) Near-infrared fundus autofluorescence showing hypoautofluorescent spots. (d) Fluorescein angiography during late-frames showing the multifocal hyperfluorescence at the posterior pole associated with optic disc leakage. (e) Composite color fundus photograph of the left eye and (f) SS-OCT, 1 year after the first presentation, showing the complete resolution of abnormal findings
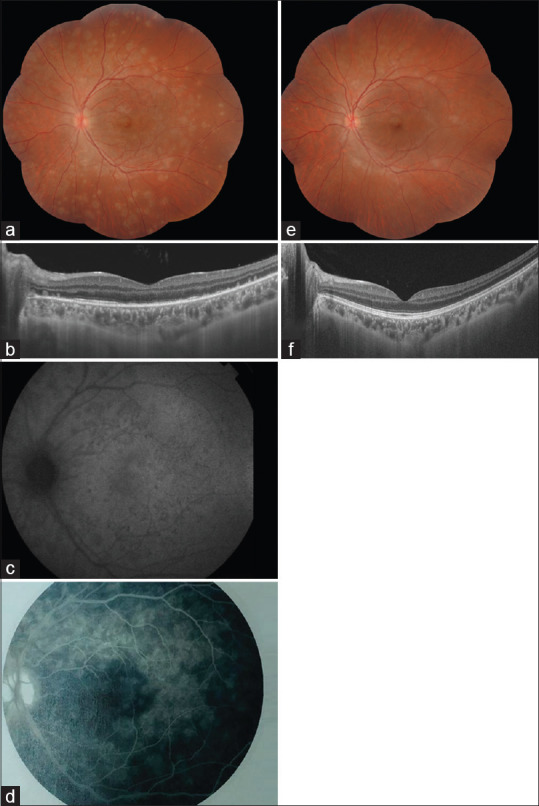
Figure 4.
En-face swept-source optical coherence tomography (SS-OCT) and SS-OCT angiography (SS-OCTA) at presentation in the same patient of Figure 3 (a-e): Structural en-face SS-OCT (3 mm × 3 mm scans) at the level of the outer retina revealing hyporeflective areas corresponding to the ellipsoid zone disruption and a few hyperreflective spots due to the accumulations of hyperreflective material over the retinal pigment epithelium. En-face SS-OCTA (3 mm × 3 mm scans) at the level of choriocapillaris showing areas of hypointense flow deficit, which are highlighted by an arrow and an arrowhead, respectively, with decreased flow signal in the choriocapillaris on respective SS-OCTA B-scans. Both the areas of flow voids that are shown are associated with inflammatory changes of the overlying outer retina, and a projection artifact with a signal attenuation could not be excluded. En-face SS-OCT and SS-OCTA, at 1-month follow-up (f-j): En-face SS-OCTA, 1 month after the first presentation, showing a resolution of the hypointense areas at the level of the choriocapillaris with a restitution of flow signals on SS-OCTA B-scans. En-face SS-OCT, 1 month after the first presentation, showing some persistent hyporeflective areas. En-face SS-OCT and SS-OCTA, at 12-month follow-up (k-o): En-face SS-OCT at the level of the outer retina and SS-OCTA at the level of the choriocapillaris, 1 year after the first presentation, showing no obvious abnormalities
DISCUSSION
These two young female patients presented with a complaint of acute, painless, unilateral blurred vision. A diagnosis of typical MEWDS could be made in both cases based on characteristic clinical and imaging findings at presentation and a transient and self-limiting course. Both the patients exhibited multiple, deep, white dots distributed over the posterior pole and mid-periphery with foveal granularity in the absence of associated clinically evident vitritis. They also showed typical fluorescein angiography findings including early hyperfluorescence and late staining of the white dots with a wreath-like configuration. Fairly typical structural SS-OCT findings also were seen including the disruption of the ellipsoid zone and accumulation of hyperreflective material of variable size and shape, resting on the RPE and extending inward through the interdigitation zone, ellipsoid zone, and outer nuclear layer toward the inner retina. Structural en-face SS-OCT findings were also typical in our patients, including hyporeflective spots, corresponding to the areas of ellipsoid zone disruption with or without associated hyperreflective dots, corresponding to the intraretinal hyperreflective foci in the outer nuclear layer.1,2,3,4,5
Recent data on OCTA provide evidence of flow reduction at the level of choriocapillaris or inner choroid in various white dot syndromes, including acute posterior multifocal placoid pigment epitheliopathy (APMPPE) and related placoid disorders.6 This suggests a primary inner choroidal involvement with secondary RPE and outer retinal changes in all these specific white dot syndromes. Conversely, recent OCTA and SS-OCTA studies revealed a completely normal choriocapillaris flow in all patients with MEWDS.3,7 By combining multimodal imaging, including OCTA, it has been proposed that MEWDS is primarily the result of inflammation at the outer photoreceptor level, leading to a photoreceptoritis, rather than the choricapillaris being at the origin of photoreceptor damage.3,4,7 However, a completely normal choriocapillaris flow on OCTA cannot exclude a transient or undetectable choriocapillaris flow changes in patients with acute MEWDS.8 It has been suggested that failure of OCTA to detect choriocapillaris non-perfusion in MEWDS might be explained by the predominant location of choriocapillaris pathology in the endcapillary sector where flow is very low and therefore not detected whether it is impaired or not by the current OCTA technology.8
Both our patients with typical acute MEWDS showed SS-OCTA multifocal small areas of flow reduction at the level of the choriocapillaris, both in the absence and in the presence of overlying inflammatory outer retina or RPE changes. There was a full recovery of areas of choriocapillaris flow deficits within several months after the initial presentation. This imaging finding supports the hypothesis of transient, primary, or secondary choriocapillaris hypoperfusion. Cross-sectional structural SS-OCT with flow overlay (B-scan OCT angiogram) is useful in excluding signal attenuation related to the overlying inflammatory tissue to explain this reduced inner choroidal flow. The areas of choriocapillaris flow reduction in our patients were scarce, as compared to the extent of central structural lesions on fundus photography, fundus autofluorescence, and OCT. Further hypoperfusion involving endcapillary circulation might be associated but not detected by the OCTA.8
Recent data show that the signs of MEWDS can overlap with the manifestations of APMPPE in the same patient, with evidence of choriocapillaris ischemia on dye-based angiography and OCTA that dramatically improves over time. Both the white dot syndromes might therefore represent the spectrum of the same disease involving the choriocapillaris, with different degrees of severity.5,8 Further studies are required to better understand the pathogenesis of MEWDS and to clarify the role of choriocapillaris as a potential primary or secondary site of inflammation in typical and atypical clinical presentations of MEWDS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
This work has been supported by the Ministry of Higher Education and Research of Tunisia.
REFERENCES
- 1.Jampol LM, Sieving PA, Pugh D, Fishman GA, Gilbert H. Multiple evanescent white dot syndrome. I Clinical findings. Arch Ophthalmol. 1984;102:671–4. doi: 10.1001/archopht.1984.01040030527008. [DOI] [PubMed] [Google Scholar]
- 2.Herbort CP. Multiple evanescent white dot syndrome (MEWDS) In: Zierhut M, Pavesio C, Ohno S, Orefice F, Rao NA, editors. Intraocular Inflammation. Berlin: Springer-Verlag Berlin Heidelberg; 2016. [Google Scholar]
- 3.Pichi F, Srvivastava SK, Chexal S, Lembo A, Lima LH, Neri P, et al. En face optical coherence tomography and optical coherence tomography angiography of multiple evanescent white dot syndrome: New Insights Into Pathogenesis. Retina. 2016;36(Suppl 1):S178–88. doi: 10.1097/IAE.0000000000001255. [DOI] [PubMed] [Google Scholar]
- 4.Gaudric A, Mrejen S. Why the dots are black only in the late phase of the indocyanine green angiography in multiple evanescent white dot syndrome. Retin Cases Brief Rep. 2017;11(Suppl 1):S81–5. doi: 10.1097/ICB.0000000000000422. [DOI] [PubMed] [Google Scholar]
- 5.Khochtali S, Abroug N, Ksiaa I, Zina S, Attia S, Khairallah M. Atypical white dot syndrome with choriocapillaris ischemia in a patient with latent tuberculosis. J Ophthalmic Inflamm Infect. 2018;8:20. doi: 10.1186/s12348-018-0162-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klufas MA, Phasukkijwatana N, Iafe NA, Prasad PS, Agarwal A, Gupta V, et al. Optical coherence tomography angiography reveals choriocapillaris flow reduction in placoid chorioretinitis. Ophthalmol Retina. 2017;1:77–91. doi: 10.1016/j.oret.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Pereira F, Lima LH, de Azevedo AG, Zett C, Farah ME, Belfort R., Jr Swept-source OCT in patients with multiple evanescent white dot syndrome. J Ophthalmic Inflamm Infect. 2018;8:16. doi: 10.1186/s12348-018-0159-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lages V, Mantovani A, Papadia M, Herbort CP. MEWDS is a true primary choriocapillaritis and basic mechanisms do not seem to differ from other choriocapillaritis entities. J Curr Ophthalmol. 2018;30:281–6. doi: 10.1016/j.joco.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]