Abstract
The first metatarsophalangeal joint (MTPJ) is vital to the biomechanics of the foot and supports a weight up to eight times heavier than the body during athletic activities. The first MTPJ comprises osseous and cartilaginous surfaces along with a complex of supporting structures, including the dorsal extensor tendons, collateral ligaments, and a plantar plate complex. In contradistinction to the lesser MTPJ plantar plates, a single dominant fibrocartilaginous capsular thickening does not exist at the first MTPJ. Instead, the plantar plate complex comprises a fibrocartilaginous pad that invests the hallux sesamoids and is inseparable from the plantar capsule, the intersesamoid ligament, paired metatarsosesamoid and sesamoid phalangeal ligaments (SPLs), and the musculotendinous structures. Acute injury at the first MTPJ is typically secondary to forced hyperextension—turf toe—and can involve multiple structures. During hyperextension, the resulting forces primarily load the distal SPLs, making these structures more susceptible to injury. SPL injuries are best seen in the sagittal plane at MRI. Radiography can also aid in diagnosis of full-thickness SPL tears, demonstrating reduced sesamoid excursion at lateral dorsiflexed (stress) views. Hallux valgus is another common condition, resulting in progressive disabling deformity at the first MTPJ. Without appropriate treatment, first MTPJ injuries may progress to degenerative hallux rigidus. The authors detail the anatomy of the first MTPJ in cadaveric forefeet by using high-resolution 3-T and 11.7-T MRI and anatomic-pathologic correlation. Injuries to the plantar plate complex, collateral ligaments, and extensor mechanism are discussed using clinical case examples.
Online supplemental material is available for this article.
©RSNA, 2020
SA-CME LEARNING OBJECTIVES
After completing this journal-based SA-CME activity, participants will be able to:
■ Identify the normal structures of the first MTPJ plantar plate complex at high-resolution MRI.
■ Discuss the potential role of MRI and radiography in assessment of turf toe injury at the first MTPJ.
■ Recognize first MTPJ injuries occurring in hallux valgus and the role of postoperative MRI.
Introduction
The first ray is vital to the overall mechanics of the foot, and biomechanical alterations are implicated in various foot disorders, including acquired orthopedic deformities and traumatic and overuse injuries (1). In part, this is because of the location of the metatarsophalangeal joint (MTPJ) at the intersection between the transverse and medial longitudinal arches of the foot (2).
Despite the importance of the first MTPJ, the anatomic descriptions in the literature are inconsistent. The anatomy is challenging, with broad agreement that supporting structures of the plantar surface are complex, including ligaments, tendons, sesamoid bones, and the joint capsule. Nomenclature varies significantly, especially with the term plantar plate, which may refer to individual ligaments, fibrocartilaginous joint capsule thickening, or even the entire complex of sesamoids and supporting structures (3).
The anatomic complexity of the first MTPJ is a reflection of the significant biomechanical demands placed on the joint, which is exposed to 40%–60% of loading force during normal gait and up to 800% of body weight during athletic activity (4–6). Not surprisingly, injuries to the first MTPJ plantar region, broadly termed turf toe, are common among athletes, especially those engaged in bursts of running and jumping. In particular, Rodeo and colleagues (7) found that 45% of active American football players had sustained turf toe injury during their professional career.
Hallux valgus is another common condition affecting the first MTPJ with a prevalence of up to one-third of the general public. The condition can be disabling and remains a major health care issue, with over 200 000 surgeries performed annually (8).
MRI of the first MTPJ provides a detailed depiction of injuries to the plantar plate complex, extensor tendons, collateral ligaments, cartilage, and osseous structures (9). In athletic injuries, this information is crucial for planning early surgical repair of the torn capsuloligamentous structures, which can restore first MTPJ stability and allow athletes to return to competition (10). In hallux valgus, MRI can depict additional cartilage and capsuloligamentous injury, which is useful for surgical planning and assessing postoperative complications. As part of a multidisciplinary team, the radiologist plays an important role in first MTPJ injury, which, if left untreated, can result in accelerated arthrosis and hallux rigidus.
We discuss the normal anatomy of the first MTPJ, which comprises a number of supporting structures, including the sesamoids, plantar plate complex, dorsal extensor tendons, and collateral ligaments. High-resolution 3-T and 11.7-T MRI of cadaveric specimens demonstrates these structures. The potential role of MRI and radiography in turf toe injuries involving the plantar plate complex and hallux valgus associated with osseous, chondral, and collateral ligament injuries is described with clinical case examples.
MRI Technique and Methods
Five fresh-frozen cadaveric forefeet were used to demonstrate the anatomy of the first MTPJ. Imaging of the first MTPJ was performed with a 3.0-T clinical MRI system (General Electric, Milwaukee, Wis) with a two-dimensional intermediate-weighted sequence (repetition time msec/echo time msec = 2000/35) and a three-dimensional fast spoiled gradient-echo sequence (50/5.2). Imaging was also performed with an 11.7-T MRI system with a spin-echo sequence (5000/10). Each specimen was subsequently examined and dissected by an orthopedic surgeon with gross anatomic correlation performed.
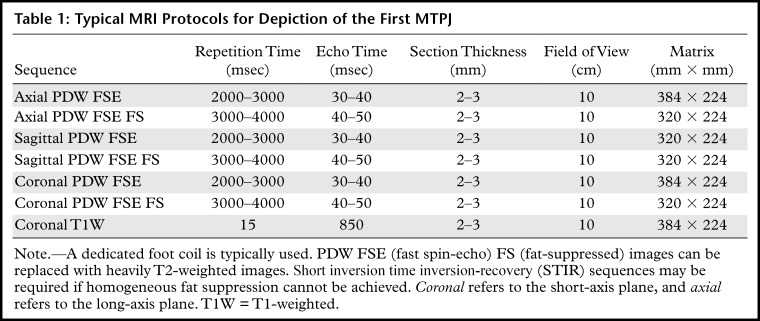
Imaging in patients was typically performed with a 3.0-T clinical MRI system (General Electric) with a dedicated foot coil. Standard axial, sagittal, and coronal proton density–weighted (PDW) and fat-saturated PDW or T2-weighted sequences were performed with 2.5-mm section thickness. In selected patients, additional coronal T1-weighted sequences were also performed. In this article, coronal refers to the short-axis plane though the great toe and axial refers to the long-axis plane. Intravenous contrast material was administered only in patients suspected of having an infection. Table 1 outlines suggested clinical MRI protocols for depiction of the first MTPJ.
Table 1:
Typical MRI Protocols for Depiction of the First MTPJ
Anatomy of the First MTPJ
The anatomic structures of the first MTPJ can be divided into the osseous components, plantar plate complex, collateral ligaments, dorsal extensor tendons, and sagittal bands.
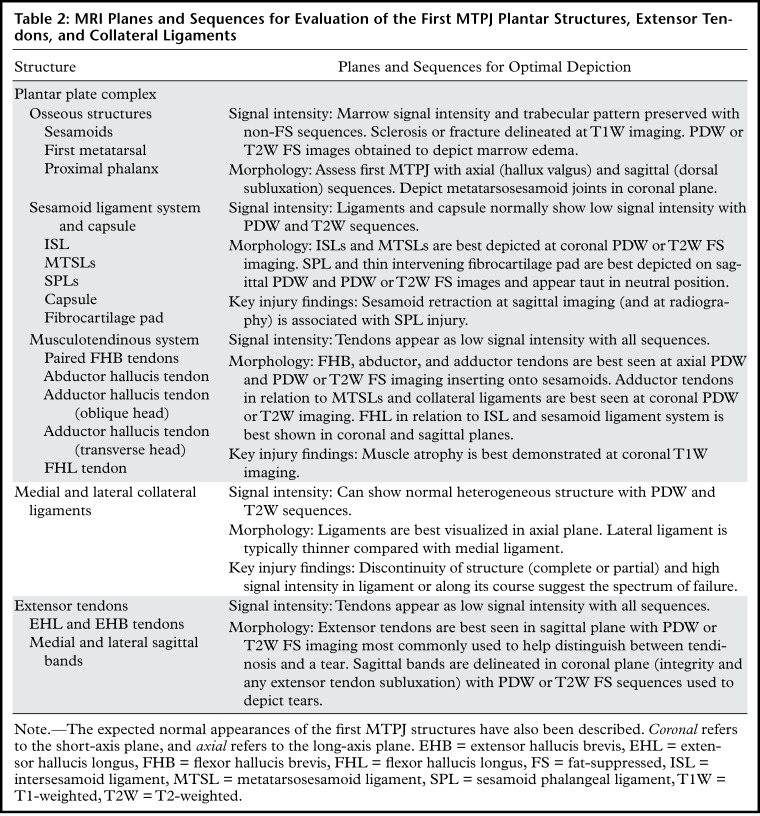
Table 2 describes the suggested MRI planes for best depiction of the first MTPJ plantar structures, extensor tendons, and collateral ligaments.
Table 2:
MRI Planes and Sequences for Evaluation of the First MTPJ Plantar Structures, Extensor Tendons, and Collateral Ligaments
Plantar Plate Complex
The plantar plate complex of the great toe disperses body weight to the sesamoids and protects the articular surfaces, allowing smooth gliding of the metatarsal head along the joint capsule and at the smaller sesamoid articulations (11). The complex forms part of a catapult that assists propulsion during gait and athletic activities, allowing effective acceleration and optimal body balance (12,13).
Compared with the lesser MTPJ plantar plates, there is discrepancy in the literature regarding the first MTPJ plantar plate nomenclature. Despite this discrepancy, there is general agreement that the plantar anatomy at the first MTPJ is complex and includes contributions from the plantar plate and osseous, capsular, fibrocartilaginous, ligamentous, and tendinous structures (14–18).
In the literature, the plantar plate is broadly referred to as fibrocartilaginous thickening of the plantar capsule encasing the sesamoids and extending from the first metatarsal head to the base of the proximal phalanx. Anatomic descriptions of the plantar plate have described a thick distal attachment to the base of the proximal phalanx with variable descriptions of a thin proximal attachment to the metatarsal head-neck junction, or even at the level of the intersesamoid ligament (ISL) (19–23). To further complicate matters, the term has also been used to describe individual ligaments such as the ISL, or more broadly, the entire tendinous and capsuloligamentous structures at the plantar first MTPJ (24).
The concept of a plantar plate complex is reinforced in the radiology literature, with several authors describing either a plantar capsuloligamentous complex or a hallucal sesamoid complex (9,17,25,26). In contradistinction to the lesser MTPJs, a single dominant fibrocartilaginous capsular thickening does not exist at the first MTPJ. Instead, the fibrocartilaginous pad at the plantar first MTPJ invests the sesamoids and is inseparable from the plantar capsule, ISL, paired metatarsosesamoid ligaments (MTSLs) and sesamoid phalangeal ligaments (SPLs), and musculotendinous structures. Together, these form a functional unit, which we refer to as the plantar plate complex (Figs 1, 2). An analogous structure to the lesser plantar plate is the fibrocartilaginous pad of tissue beneath the first MTPJ arising from the ISL and extending between the SPLs to the first proximal phalangeal base.
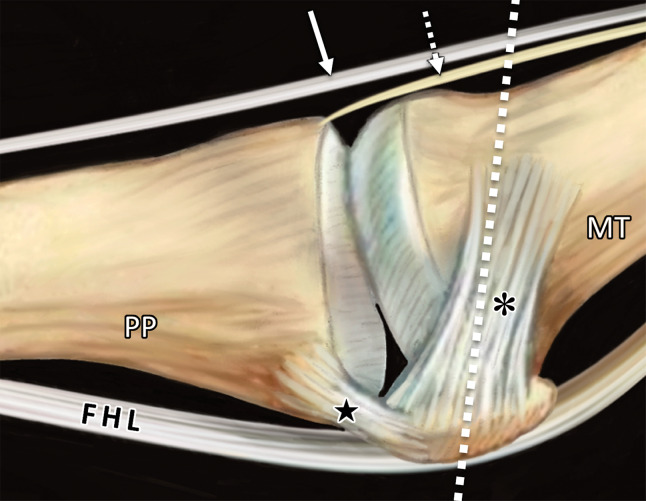
Figure 1a.
First MTPJ anatomy. Sagittal (a) and coronal cross-sectional (b) drawings (plane in b represented by the dotted line in a) show how the medial SPL (★), lateral SPL (not shown), and lateral (#) and medial (*) MTSLs secure the lateral (L) and medial (M) sesamoids. These ligaments form a plantar plate complex with the joint capsule, ISL, and musculotendinous structures. At the dorsal first MTPJ, the EHB (dotted arrow) attaches to the proximal phalanx (PP) and lies deep and slightly lateral to the EHL (solid arrow). The first metatarsal crest (arrowhead in b) is shown between the grooved sesamoid facets. FHL = flexor hallucis longus, IS = intersesamoid ligament, MT = metatarsal.
Figure 2a.
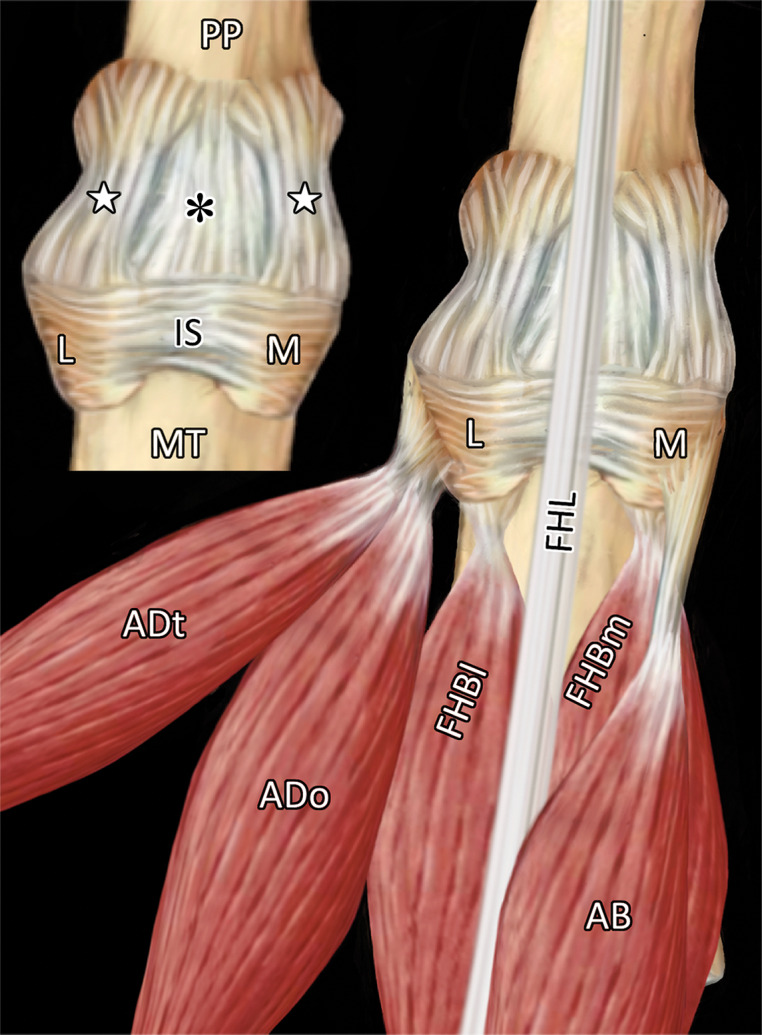
First MTPJ anatomy. (a) Drawing depicts a view from below the first MTPJ musculotendinous structures. Laterally, the oblique (ADo) and transverse (ADt) heads of the adductor hallucis provide resistance to medial displacement. Medially, the abductor hallucis tendon (AB) inserts at the medial sesamoid (M) and medial capsuloligamentous structures, preventing hallux valgus. The lateral (FHBl) and medial (FHBm) heads of the FHB insert at the respective sesamoids, preventing distal sesamoid migration. Inset in a shows the MTPJ with the FHL and tendons removed. IS = intersesamoid ligament. (b, c) Gross anatomy of a cadaveric first MTPJ specimen (b) is also shown with the medial structures dissected and then with plantar disarticulation, with the plantar plate complex (c) viewed from the dorsal aspect. Paired SPLs (☆) and the medial SPL (arrow in b) are continuous with the capsule and fibrocartilaginous pad (*), preventing proximal sesamoid migration. The ISL (dotted line in c) prevents sesamoid splaying. Chondral defects are noted at the metatarsal head (arrowheads in c). L = lateral sesamoid, MT = metatarsal, PP = proximal phalanx.
Figure 1b.
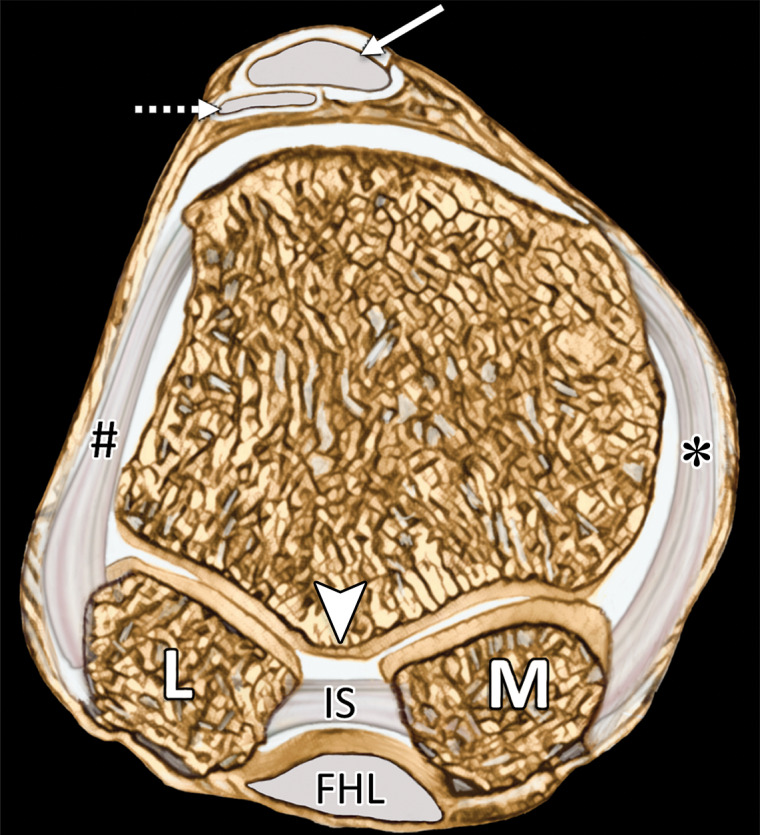
First MTPJ anatomy. Sagittal (a) and coronal cross-sectional (b) drawings (plane in b represented by the dotted line in a) show how the medial SPL (★), lateral SPL (not shown), and lateral (#) and medial (*) MTSLs secure the lateral (L) and medial (M) sesamoids. These ligaments form a plantar plate complex with the joint capsule, ISL, and musculotendinous structures. At the dorsal first MTPJ, the EHB (dotted arrow) attaches to the proximal phalanx (PP) and lies deep and slightly lateral to the EHL (solid arrow). The first metatarsal crest (arrowhead in b) is shown between the grooved sesamoid facets. FHL = flexor hallucis longus, IS = intersesamoid ligament, MT = metatarsal.
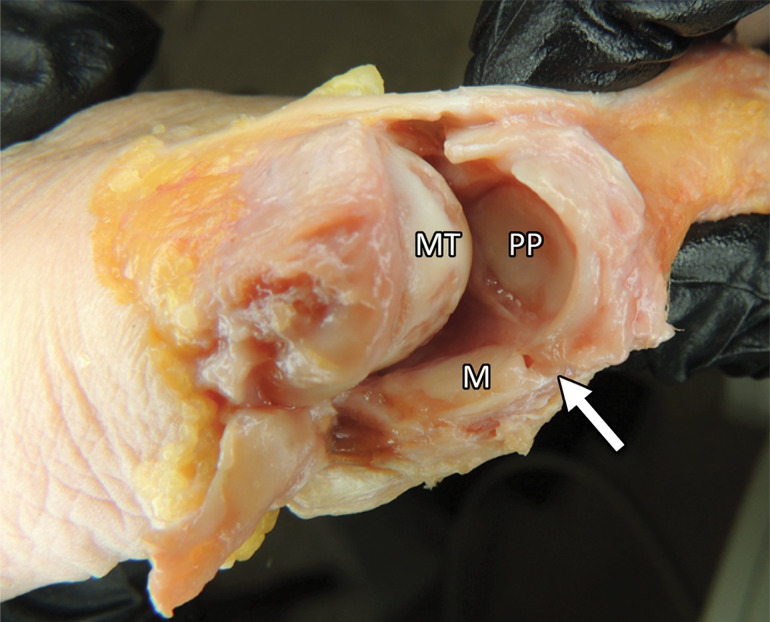
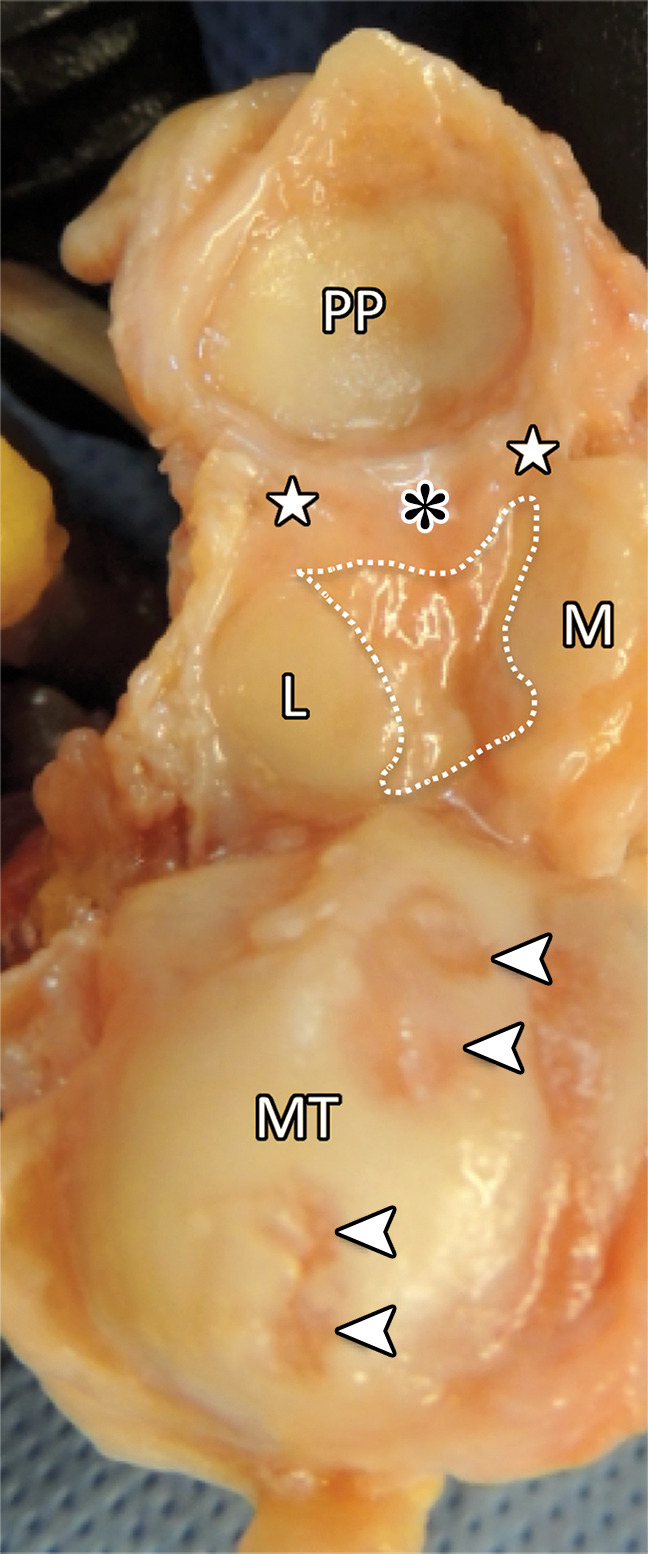
Figure 2b.
First MTPJ anatomy. (a) Drawing depicts a view from below the first MTPJ musculotendinous structures. Laterally, the oblique (ADo) and transverse (ADt) heads of the adductor hallucis provide resistance to medial displacement. Medially, the abductor hallucis tendon (AB) inserts at the medial sesamoid (M) and medial capsuloligamentous structures, preventing hallux valgus. The lateral (FHBl) and medial (FHBm) heads of the FHB insert at the respective sesamoids, preventing distal sesamoid migration. Inset in a shows the MTPJ with the FHL and tendons removed. IS = intersesamoid ligament. (b, c) Gross anatomy of a cadaveric first MTPJ specimen (b) is also shown with the medial structures dissected and then with plantar disarticulation, with the plantar plate complex (c) viewed from the dorsal aspect. Paired SPLs (☆) and the medial SPL (arrow in b) are continuous with the capsule and fibrocartilaginous pad (*), preventing proximal sesamoid migration. The ISL (dotted line in c) prevents sesamoid splaying. Chondral defects are noted at the metatarsal head (arrowheads in c). L = lateral sesamoid, MT = metatarsal, PP = proximal phalanx.
Figure 2c.
First MTPJ anatomy. (a) Drawing depicts a view from below the first MTPJ musculotendinous structures. Laterally, the oblique (ADo) and transverse (ADt) heads of the adductor hallucis provide resistance to medial displacement. Medially, the abductor hallucis tendon (AB) inserts at the medial sesamoid (M) and medial capsuloligamentous structures, preventing hallux valgus. The lateral (FHBl) and medial (FHBm) heads of the FHB insert at the respective sesamoids, preventing distal sesamoid migration. Inset in a shows the MTPJ with the FHL and tendons removed. IS = intersesamoid ligament. (b, c) Gross anatomy of a cadaveric first MTPJ specimen (b) is also shown with the medial structures dissected and then with plantar disarticulation, with the plantar plate complex (c) viewed from the dorsal aspect. Paired SPLs (☆) and the medial SPL (arrow in b) are continuous with the capsule and fibrocartilaginous pad (*), preventing proximal sesamoid migration. The ISL (dotted line in c) prevents sesamoid splaying. Chondral defects are noted at the metatarsal head (arrowheads in c). L = lateral sesamoid, MT = metatarsal, PP = proximal phalanx.
Key structures of the plantar plate complex can be organized into three main groups: (a) the sesamoids and osseous structures, (b) the sesamoid ligament system and plantar capsule, and (c) the musculotendinous system. We have chosen to exclude the proper collateral ligaments, although a minority of first MTPJ manuscripts include these structures in the anatomic and clinical spectrum of plantar plate injury (9,17,27).
Sesamoids and Osseous Structures
There are two grooves on the plantar surface of the first metatarsal head separated by a rounded ridge or crest, which accommodate the articular surfaces of the medial (tibial) and lateral (fibular) sesamoid bones (Fig 1). The base of the first proximal phalanx is broad with an elliptical concavity, which articulates with the large surface of the metatarsal head and receives muscular and ligamentous attachments. This structure allows a wide range of motion in flexion and extension and more restricted valgus and varus motion (19).
The sesamoids are well demonstrated in all three imaging planes and are elliptical. They are integral components of the plantar plate complex and serve as attachment points for most structures. Up to one-third of all sesamoids are bipartite with multipartite morphology less commonly seen (20). The medial sesamoid is most commonly involved, although up to 85% of partite sesamoids are seen bilaterally (20).
Sesamoid Ligament System and Plantar Capsule
The ISL forms a link between the sesamoids (Fig 3). It consists of transverse bundles of collagen fibers that are interwoven by longitudinal and vertical fiber bundles and is best depicted in the coronal plane. It functions as a flexible bridge connecting the two sesamoids and therefore also indirectly connects the flexor hallucis brevis (FHB), abductor hallucis, and adductor hallucis tendons. Furthermore, it is blended with the synovial tendon sheath of the flexor hallucis longus (FHL). As part of the synovial joint, the ISL is covered with a thick synovial fold (Fig 4) (17,28).
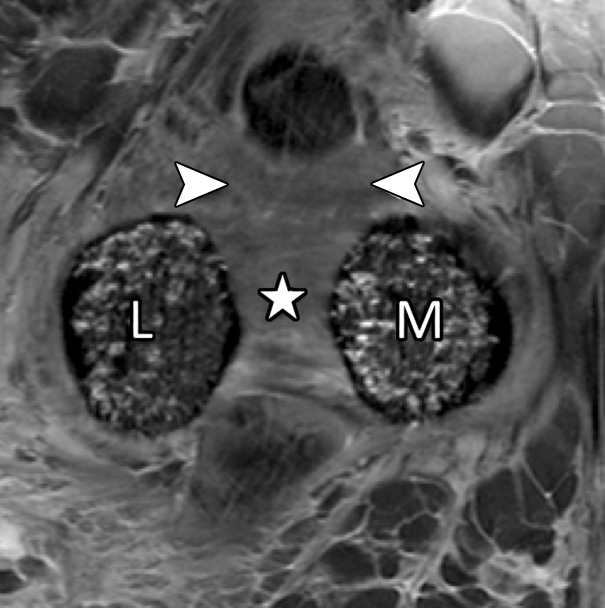
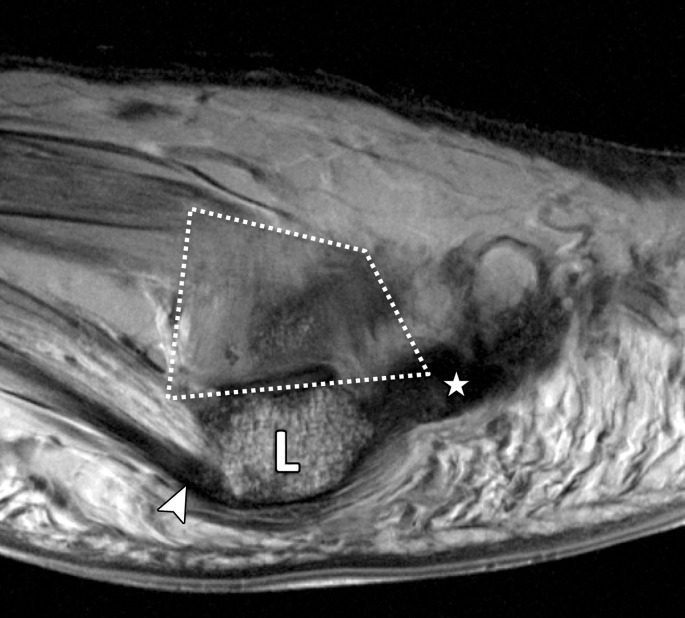
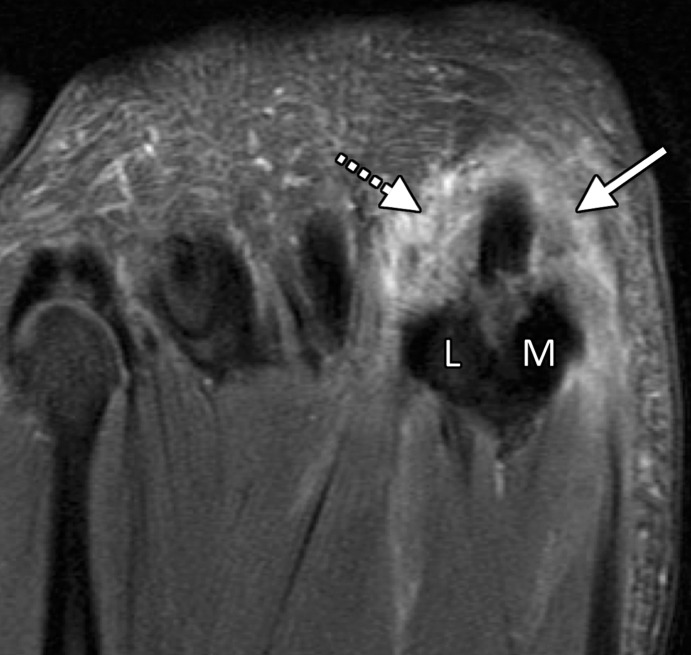
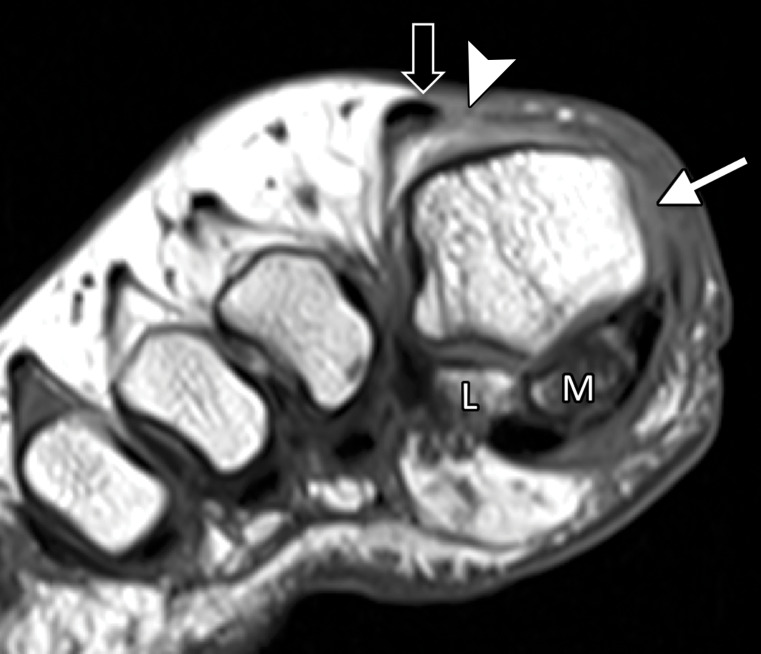
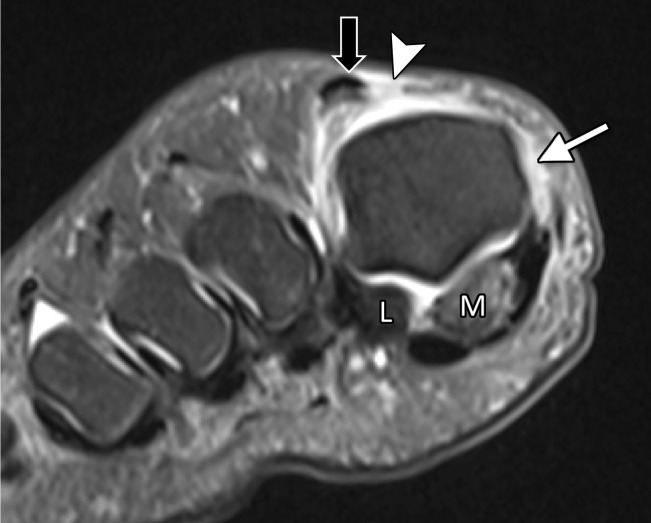
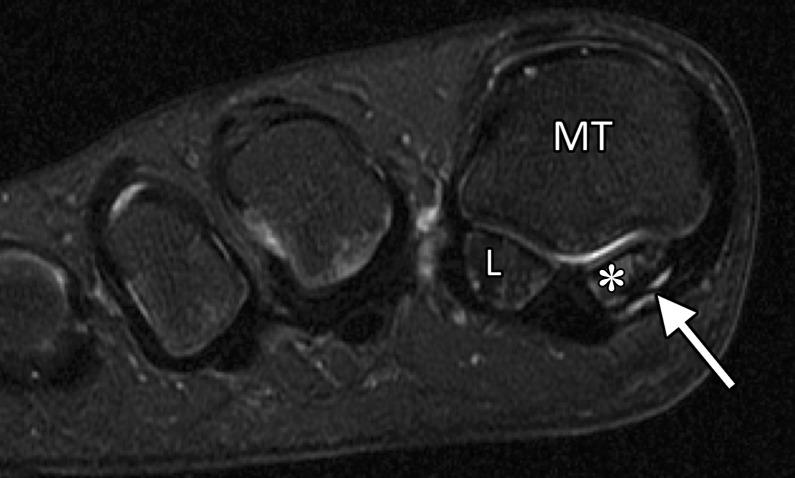
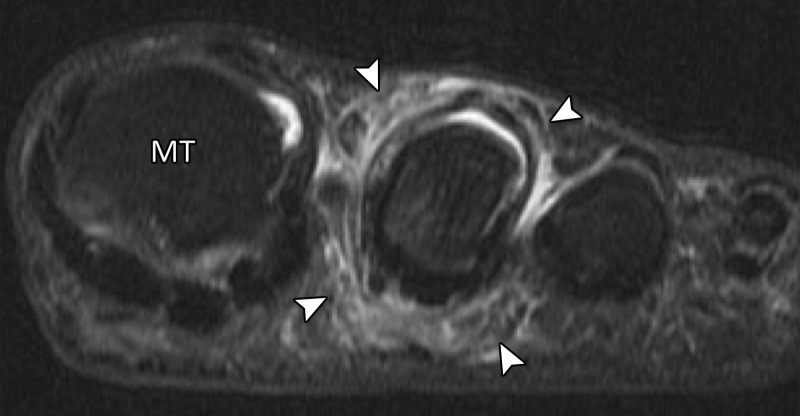
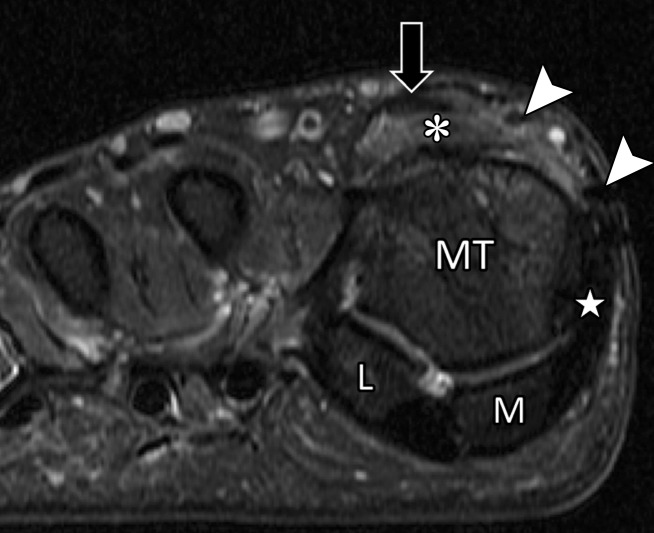
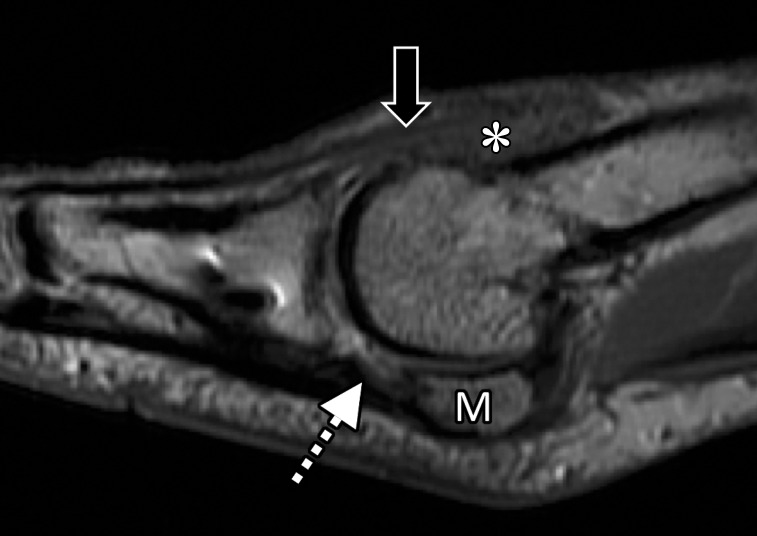
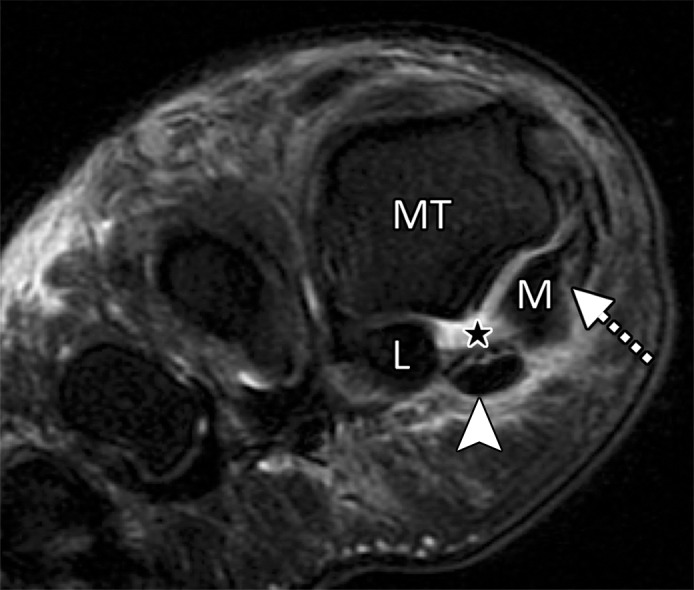
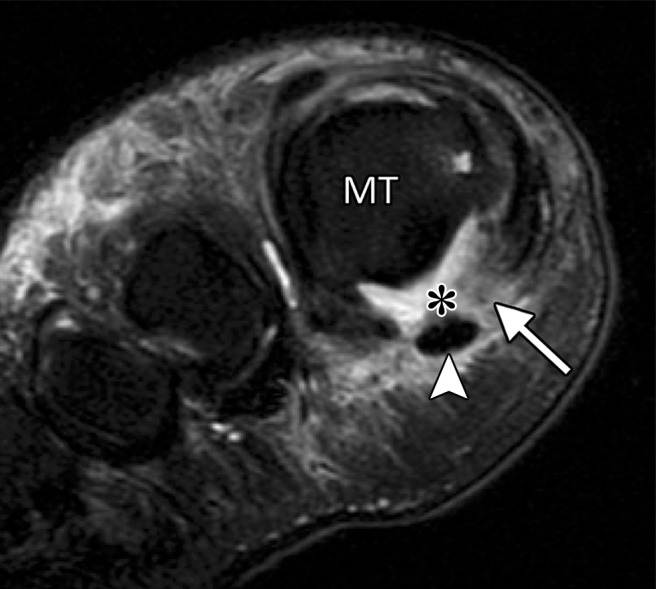
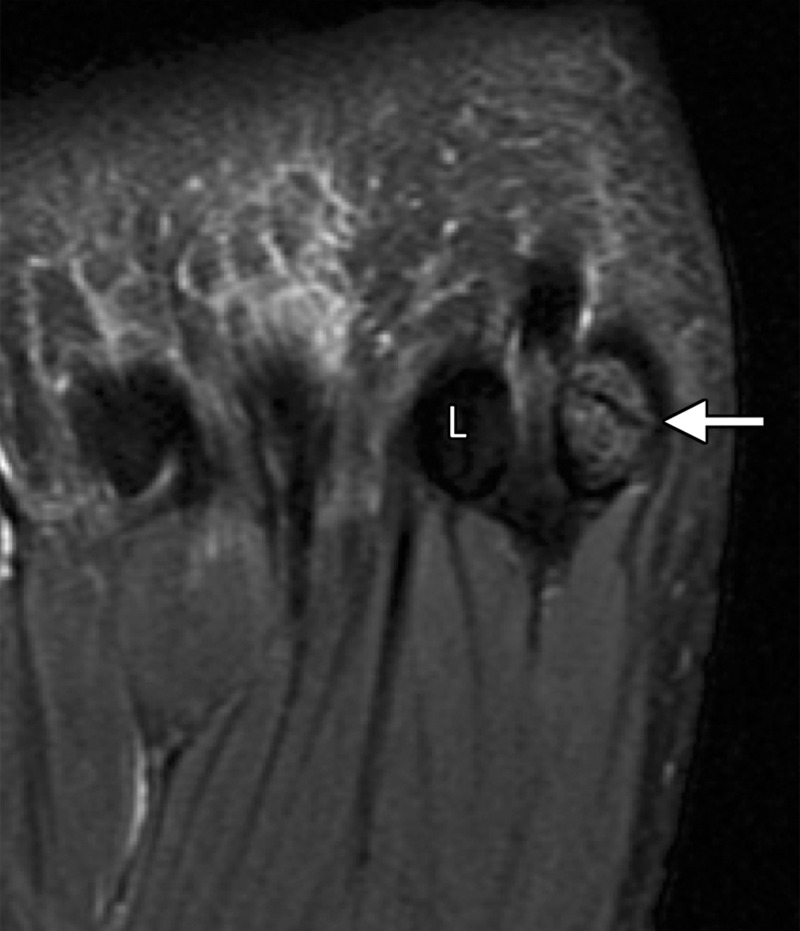
Figure 3a.
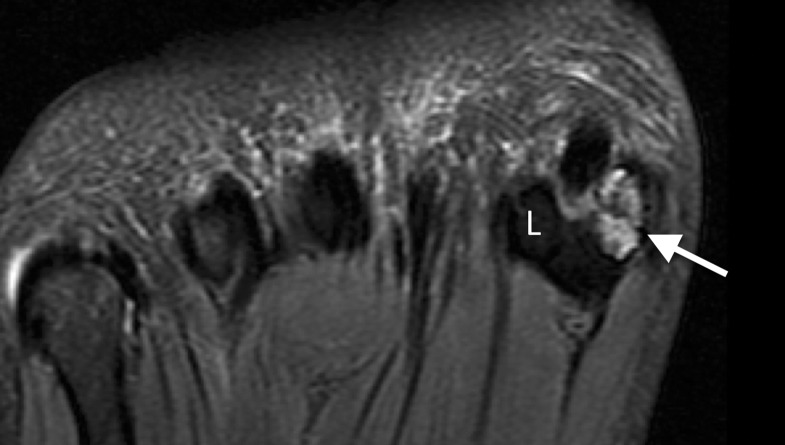
First MTPJ anatomy in a cadaveric specimen. Axial (a), central sagittal (b), and medial sagittal (c) gradient-echo images (5000/10) show how the lateral (L) and medial (M) sesamoids are connected by the ISL (☆). A fibrocartilaginous pad (arrowheads) is seen distal to the ISL, which merges with the medial SPL (black arrow) and lateral SPL (not shown). Dorsally, the EHB tendon (dotted arrow) attaches to the proximal phalanx and lies deep to the EHL tendon (white arrow).
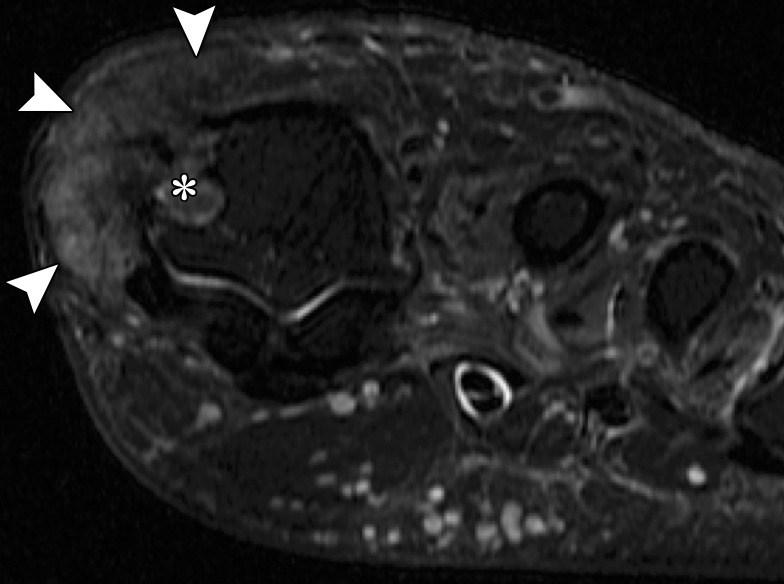
Figure 4.
First metatarsosesamoid joint anatomy in a cadaveric specimen. Coronal gradient-echo image (5000/10) shows how the paired lateral (#) and medial (*) MTSLs secure the lateral (L) and medial (M) sesamoids. These ligaments form a plantar plate complex along with the joint capsule, intersesamoid ligament (IS), and musculotendinous structures, including the abductor hallucis muscle and tendon (black arrow). The fibers of the ISL are intimately associated with the FHL tendon sheath and a deep synovial fold (arrowhead). At the dorsal first MTPJ, the EHB (dotted arrow) lies deep and slightly lateral to the EHL (white arrow).
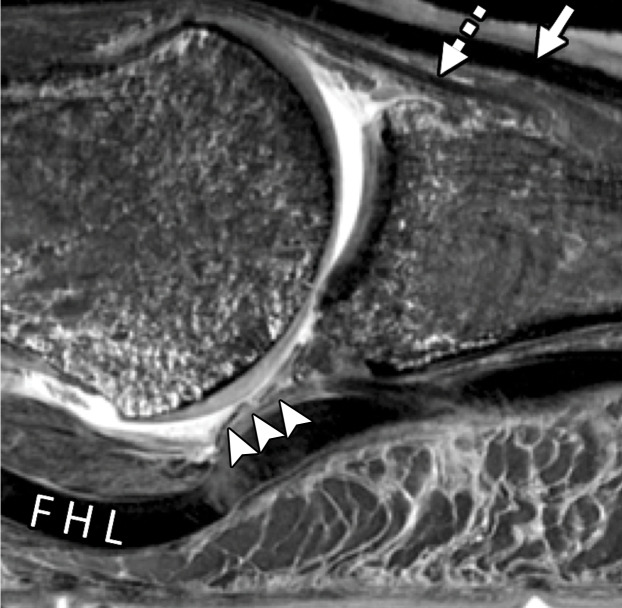
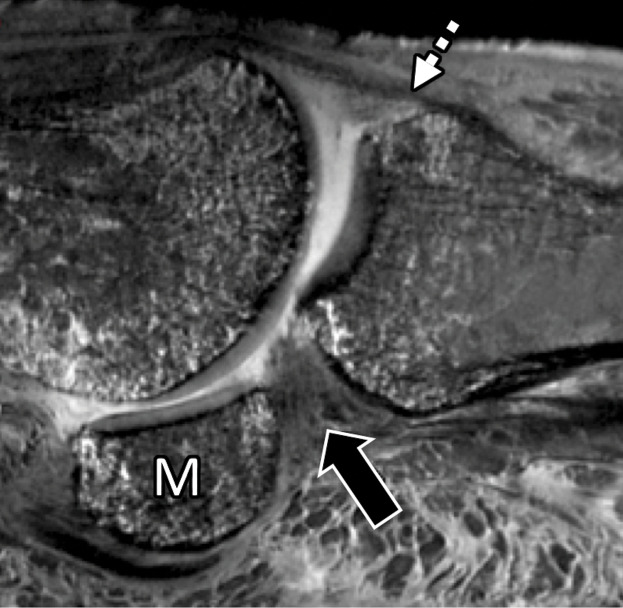
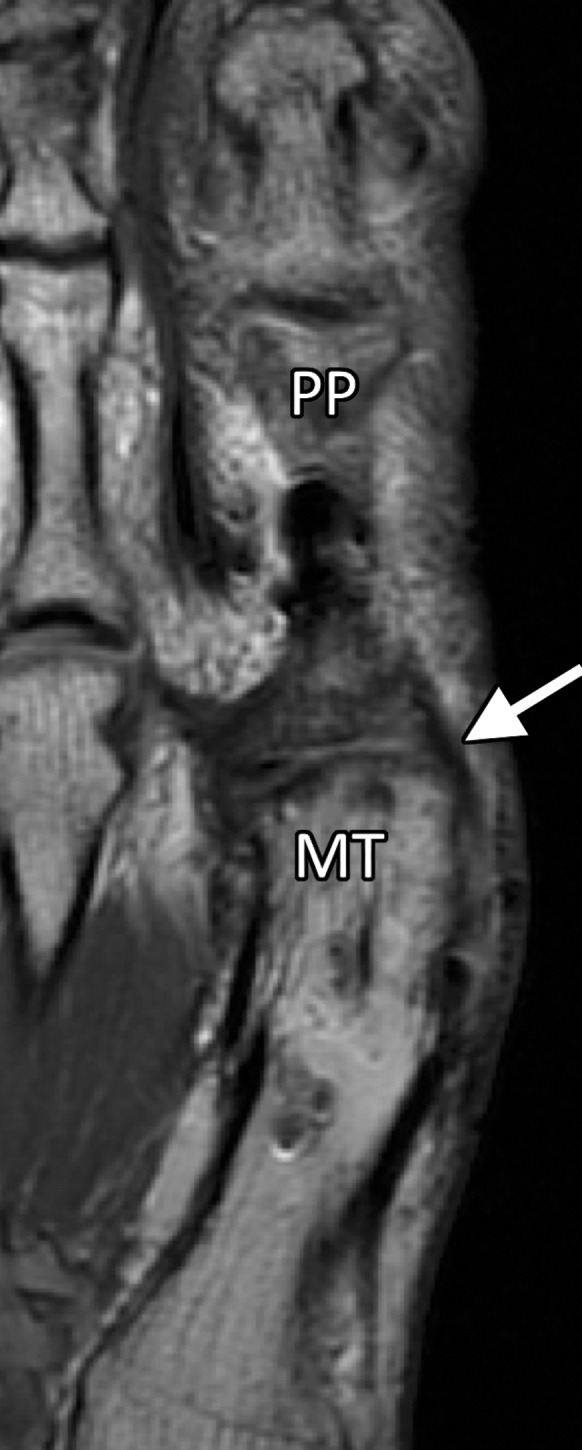
Figure 3b.
First MTPJ anatomy in a cadaveric specimen. Axial (a), central sagittal (b), and medial sagittal (c) gradient-echo images (5000/10) show how the lateral (L) and medial (M) sesamoids are connected by the ISL (☆). A fibrocartilaginous pad (arrowheads) is seen distal to the ISL, which merges with the medial SPL (black arrow) and lateral SPL (not shown). Dorsally, the EHB tendon (dotted arrow) attaches to the proximal phalanx and lies deep to the EHL tendon (white arrow).
Figure 3c.
First MTPJ anatomy in a cadaveric specimen. Axial (a), central sagittal (b), and medial sagittal (c) gradient-echo images (5000/10) show how the lateral (L) and medial (M) sesamoids are connected by the ISL (☆). A fibrocartilaginous pad (arrowheads) is seen distal to the ISL, which merges with the medial SPL (black arrow) and lateral SPL (not shown). Dorsally, the EHB tendon (dotted arrow) attaches to the proximal phalanx and lies deep to the EHL tendon (white arrow).
The SPLs are the thickest first MTPJ ligaments and are the main restraints to proximal sesamoid subluxation when high tensile forces are placed across them during hyperextension (dorsiflexion) on walking or running. As a result, the SPLs are also the most commonly injured when hyperextension occurs (1,17,29). The insertion and site of injury of these ligaments are best depicted in the sagittal plane (Fig 3).
The MTSLs or suspensory ligaments are part of the plantar plate complex and assist with stabilizing the sesamoids (Fig 4). The fibers of the medial and lateral MTSLs are thin compared with the SPLs. As the name implies, the MTSLs insert proximally at the plantar aspect of the first metatarsal neck along with the capsule and distally to the inferior surface and borders of the sesamoids (Fig 5). The insertion is close to its surrounding structures, and it is difficult to differentiate the MTSLs from the capsule and adjacent tendons (16).
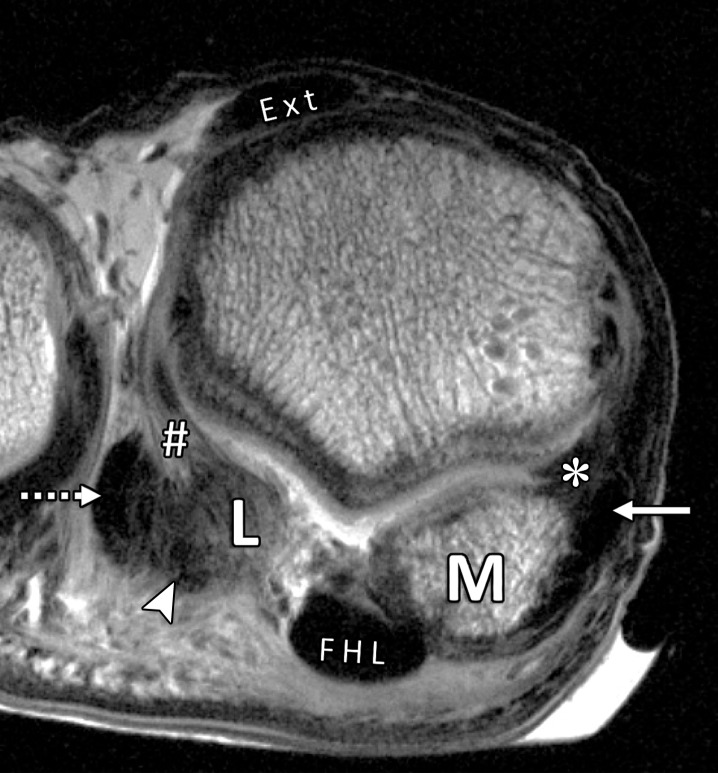
Figure 5a.
Normal anatomy of the first MTSLs. Coronal (a) and lateral sagittal (b) PDW images (2000/35) depict how the lateral (#) and medial (*) MTSLs secure the lateral (L) and medial (M) sesamoids. The MTSLs are components of the plantar plate complex and attach to the sesamoids in close relation to the FHB tendons. The insertion of the lateral head of the FHB tendon can be seen (arrowhead). The lateral MTSL inserts adjacent to the conjoint adductor hallucis tendon (dotted arrow), which resists varus stress. The medial MTSL inserts adjacent to the abductor hallucis tendon (solid arrow), which resists valgus stress. The rhomboid lateral MTSL (white dotted line in b) blends with the capsule and lateral SPL (☆). Ext = extensor tendons.
Figure 5b.
Normal anatomy of the first MTSLs. Coronal (a) and lateral sagittal (b) PDW images (2000/35) depict how the lateral (#) and medial (*) MTSLs secure the lateral (L) and medial (M) sesamoids. The MTSLs are components of the plantar plate complex and attach to the sesamoids in close relation to the FHB tendons. The insertion of the lateral head of the FHB tendon can be seen (arrowhead). The lateral MTSL inserts adjacent to the conjoint adductor hallucis tendon (dotted arrow), which resists varus stress. The medial MTSL inserts adjacent to the abductor hallucis tendon (solid arrow), which resists valgus stress. The rhomboid lateral MTSL (white dotted line in b) blends with the capsule and lateral SPL (☆). Ext = extensor tendons.
The joint capsule is an important component of the first MTPJ and is reinforced by the plantar fibrocartilaginous pad. As discussed, the plantar fibrocartilaginous tissue has been broadly described as the first MTPJ plantar plate in the literature. With the great toe in neutral position, the proximal capsule is redundant and appears thicker at the metatarsal neck attachment.
Musculotendinous System
The plantar plate complex includes dynamic stabilizing musculotendinous structures. An analogous synergistic complex is found at the patellofemoral compartment of the knee, where the patella can be likened to the first MTPJ sesamoids and the quadriceps to the plantar musculotendinous structures, which are composed of the FHB (lateral and medial heads), FHL, and abductor and adductor hallucis tendons.
The medial and lateral tendons of the FHB attach to the proximal and plantar surfaces of the medial and lateral sesamoids, respectively (Fig 2). The sesamoids also fortify the apparatus of the abductor hallucis and adductor hallucis muscles and tendons (24,30).
Surrounded by a fibrous sheath, the FHL tendon passes under the ISL in a groove between the sesamoids and the medial and lateral heads of the FHB tendons and inserts at the base of the distal phalanx (31). This anatomy is best visualized in the coronal and sagittal planes.
The main insertions of the FHB and abductor and adductor hallucis (transverse and oblique heads) tendons are at the sesamoids, although some fibers insert on the proximal part of the articular capsule (32). This anatomy and mechanism is similar to the quadriceps tendon insertion at the upper part of the articular capsule of the knee. The anatomy of these structures is best visualized in the coronal and axial planes (Fig 6).
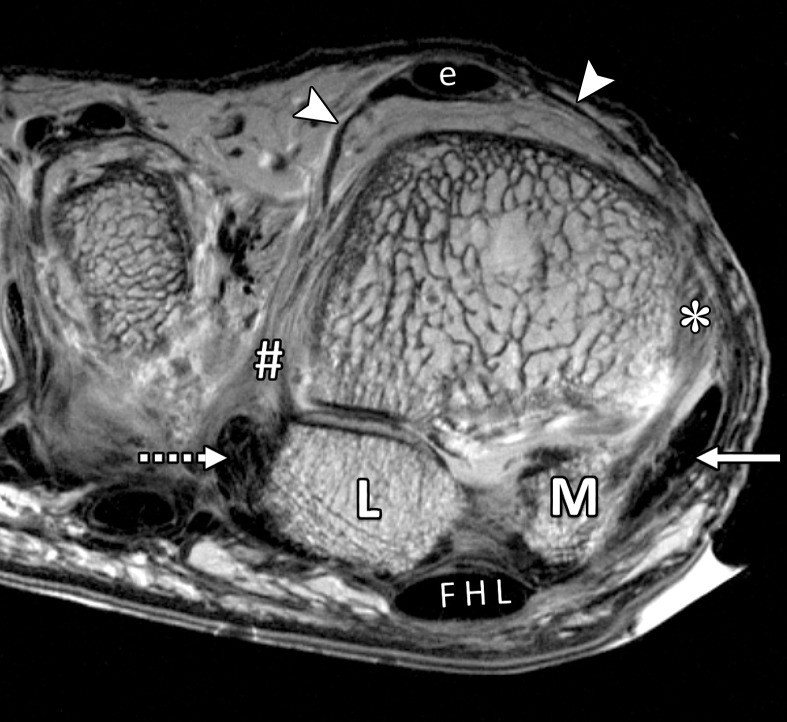
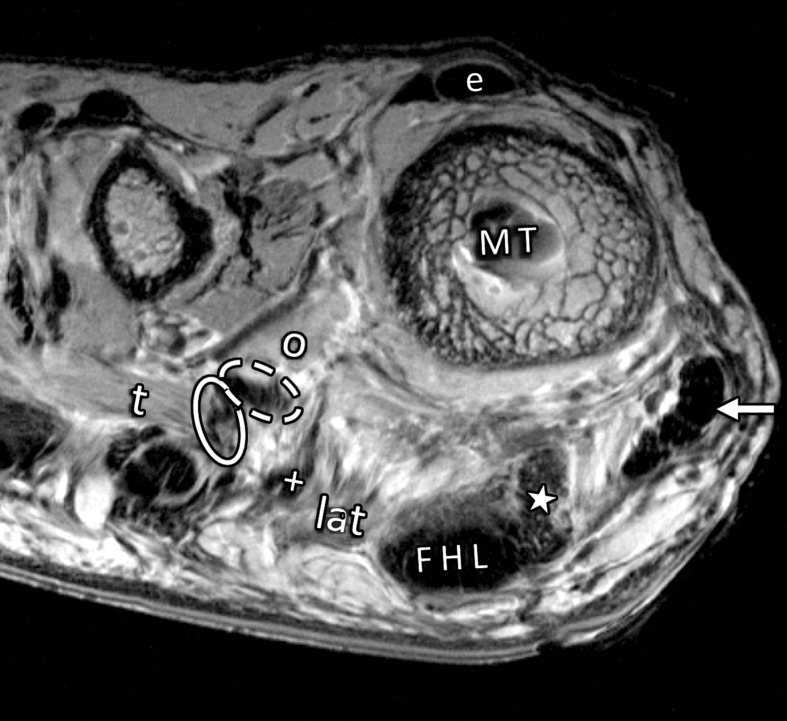
Figure 6a.
Musculotendinous structures of the first MTPJ. Coronal PDW images (2000/35) of the metatarsosesamoid joint (a) and the distal first metatarsal (MT) (b) depict the attachment of the adductor (dotted arrow) and abductor (solid arrow) hallucis tendons to the lateral (L) and medial (M) sesamoids. These tendons insert in close relation to the lateral (#) and medial (*) MTSLs and the lateral (+ = tendon, lat = muscle belly) and medial (☆) heads of the FHB. The adductor hallucis conjoint tendon is formed from the transverse (t = muscle, solid oval = tendon) and oblique (o = muscle, dashed oval = tendon) heads. Dorsally, the extensor tendons (e) can be seen secured by the lateral and medial sagittal bands (arrowheads).
Figure 6b.
Musculotendinous structures of the first MTPJ. Coronal PDW images (2000/35) of the metatarsosesamoid joint (a) and the distal first metatarsal (MT) (b) depict the attachment of the adductor (dotted arrow) and abductor (solid arrow) hallucis tendons to the lateral (L) and medial (M) sesamoids. These tendons insert in close relation to the lateral (#) and medial (*) MTSLs and the lateral (+ = tendon, lat = muscle belly) and medial (☆) heads of the FHB. The adductor hallucis conjoint tendon is formed from the transverse (t = muscle, solid oval = tendon) and oblique (o = muscle, dashed oval = tendon) heads. Dorsally, the extensor tendons (e) can be seen secured by the lateral and medial sagittal bands (arrowheads).
Collateral Ligaments
Although the medial and lateral metatarsophalangeal ligaments (collateral ligaments) are not part of the plantar plate complex, they play an important role as static stabilizers when valgus or varus forces are applied, respectively. They have an oblique orientation, originating from the metatarsal condyle tubercle and inserting on the tubercle at the base of the proximal phalanx (Fig 7). Some authors have described accessory collateral ligaments that arise along with the collateral ligaments at the first metatarsal head. These ligaments merge with the capsular structures and MTSLs to attach at the peripheral sesamoids (25,33).
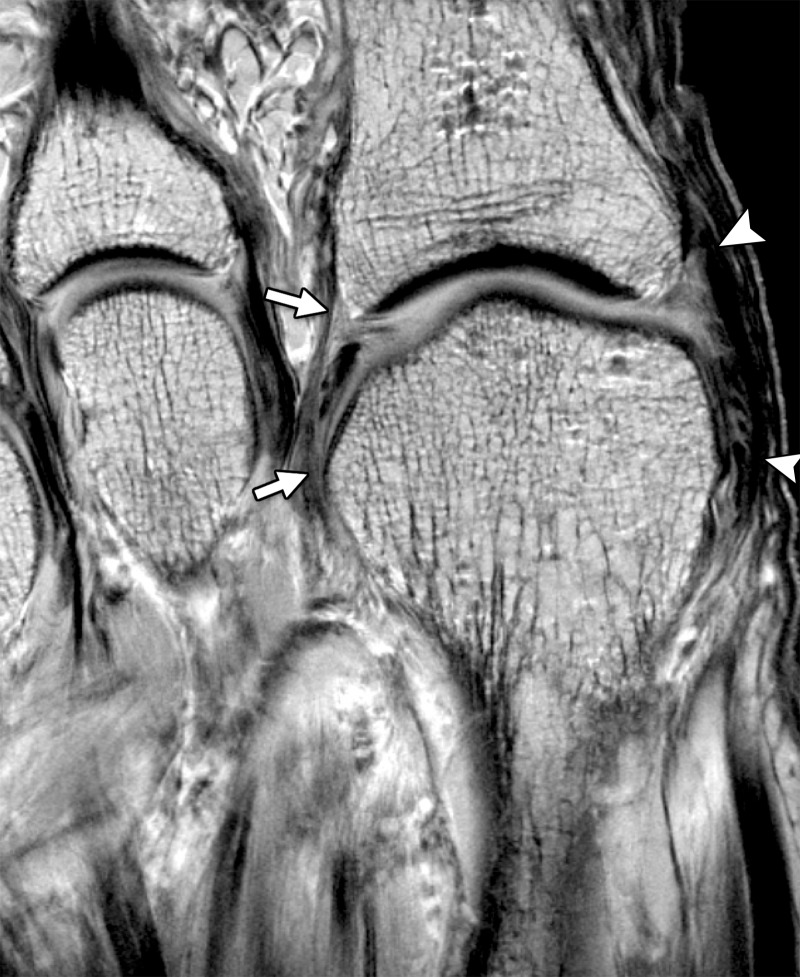
Figure 7.
Axial (long-axis) PDW image (2000/35) shows the first MTPJ collateral ligaments. Lateral (arrows) and medial (arrowheads) collateral ligaments resist varus and valgus first MTPJ forces, respectively.
Extensor Tendons
The extensor mechanism of the first toe consists of the extensor hallucis longus (EHL) and extensor hallucis brevis (EHB) tendons (Figs 1, 3, 4). The EHL muscle arises at the anterior compartment of the leg and has a long distal tendinous insertion at the dorsal base of the great toe terminal phalanx. The EHB muscle arises from the upper surface of the foot (mainly at the upper and lateral calcaneal surface) medial to the extensor digitorum brevis (Fig 3). The EHB tendon passes in a medial oblique fashion across the dorsal foot to insert at the dorsal base of the great toe proximal phalanx. Both tendons are anchored by the extensor hood, which consists of medial and lateral sagittal bands. These bands are contiguous with the joint capsule and extend from the tendons to the sesamoids. In addition, the EHB tendon inserts into the dorsal capsule and together with the EHL provides dynamic stability during plantar flexion (10,25).
First MTPJ Injuries
The first MTPJ osseous and supporting soft-tissue components may be injured because of acute trauma (eg, athletic injuries), degenerative osteoarthropathy, inflammatory arthropathies (eg, rheumatoid arthritis), crystalline arthropathies (eg, gout), or less commonly infection (25). We primarily focus on acute and degenerative plantar plate complex injuries and on pre- and postsurgical hallux valgus evaluation. Inflammatory and infective processes at the first MTPJ are discussed briefly.
Turf Toe and Other Traumatic Injuries
Turf toe is a clinical term for injury to the first MTPJ plantar structures, coined in 1976 at West Virginia University, where the medical team first attributed a football-related MTPJ injury to flexible shoes on a hard artificial playing surface. The term is now commonly used to encompass all injuries, regardless of playing surface, to the plantar aspect of the first MTPJ. The underlying mechanism of turf toe injury is multifactorial but typically involves hyperextension at the first MTPJ (34).
There is considerable variation in what anatomic structures are included in the spectrum of first MTPJ plantar lesions under the name of turf toe. Clinical grading systems for these lesions indicate that with increasing severity of injury, osseous structures, plantar capsuloligamentous structures, and tendons become involved (26). Similarly, the surgical body of literature remains somewhat vague, with broad reference to osseous and capsuloligamentous injury without precise designation of the specific structures that have been repaired (35).
The most common classification system for turf toe injury was described by Anderson et al (36). This system divides injuries into three grades on the basis of clinical evaluation, with MRI used to identify the injured structures of the plantar capsule or plantar plate (Movie). The concept of the first MTPJ plantar plate complex and three main groupings of anatomic structures allows a more accurate description of injuries under this classification. It is also useful in more chronic degenerative injury to the plantar plate complex, especially in respect to hallux valgus.
Movie 1:
Turf toe (1st MTPJ hyperextension injury) video demonstrating the mechanism of injury, sprains and full-thickness tears.
Grade I turf toe injuries are mild sprains, and MRI demonstrates mild edema surrounding intact sesamoids (no fracture or diastasis seen at MRI or radiography), plantar ligaments (eg, SPLs and MTSLs), and capsulotendinous structures. Treatment of grade I injuries is conservative and includes rest, ice, compression, and elevation (RICE), taping in a plantarflexed position, anti-inflammatory medication, and in-shoe orthotics (37). Patients can return to low-level activity after 3–5 days but are advised not to underestimate the grade of the injury and to get adequate rest (38).
Grade II injuries are partial tears with reduced range of motion, prominent swelling, and diffuse tenderness at the first MTPJ. In grade II injuries, MRI demonstrates partial fiber disruption and prominent edema at the plantar plate complex, most commonly involving the SPLs (36). These injuries are also typically treated conservatively, similar to grade I injuries, and a period of non–weight bearing is commonly advised. Patients with grade II injuries will normally lose at least 2 weeks of playing time (36,38).
Grade III injuries involve full-thickness tears of the plantar structures with an unstable first MTPJ, ecchymosis, and severe plantar swelling. MRI demonstrates full-thickness fiber disruption (typically of the SPLs), severe edema, and sesamoid fracture or diastasis (9,18). Most injuries are treated conservatively and require a prolonged period of recovery time, which can exceed 6 months away from the sport.
Indications for surgical repair of grade III injuries are uncommon but should be carefully assessed at MRI, radiography, or CT by the radiologist. Anderson et al (36) describe a large capsular avulsion with joint instability as an indication to perform surgery, which can relate to complete SPL or MTSL tears with involvement of the capsule or collateral ligaments in traumatic hallux varus or valgus (36–38). The injured plantar plate complex ligaments and capsulotendinous structures are typically repaired primarily with sutures. In traumatic hallux valgus with extensive medial plantar plate complex and collateral ligament injury, an adductor tenotomy can also be performed to prevent progressive deformity. Diastasis of a bipartite sesamoid or fracture, sesamoid retraction, and loose osteochondral bodies in the first MTPJ are other indications for surgical repair (37,38).
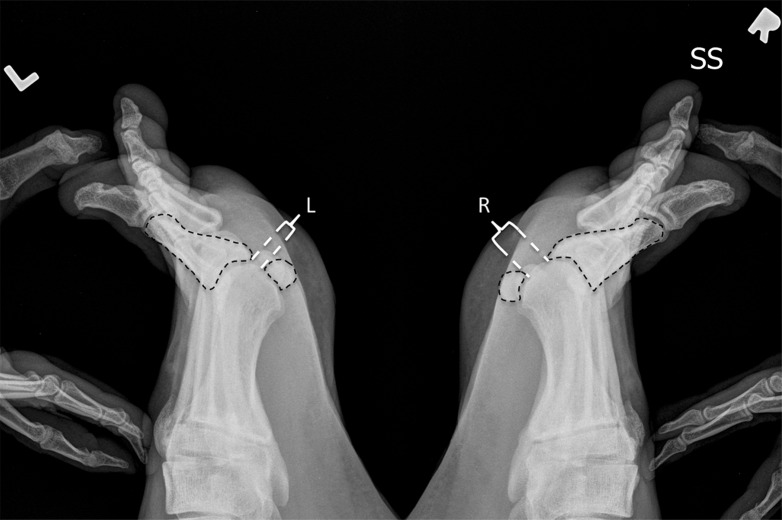
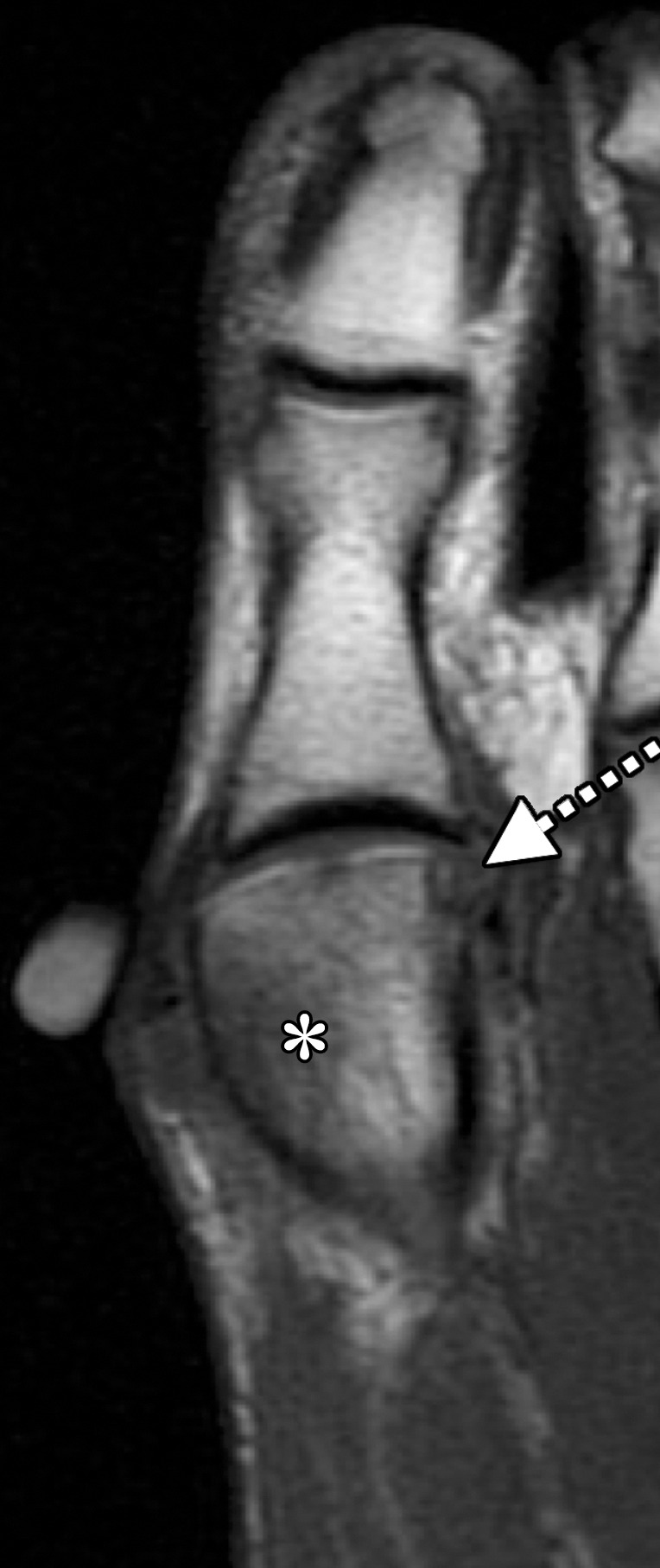
During hyperextension, the resulting forces applied to the first MTPJ primarily load the distal SPLs, making these structures more susceptible to injury when compared with the proximal complex. Tears of the SPLs may be unilateral, more common medially (Fig 8), or bilateral, leading to joint destabilization (Fig 9) (17,39,40). Injuries are best seen in the sagittal plane at MRI. Full-thickness tearing of the distal SPLs can result in proximal sesamoid displacement at MRI relative to the first MTPJ line. Radiography can also aid diagnosis of full-thickness SPL tears by demonstrating reduced sesamoid excursion on lateral dorsiflexed (stress) views relative to the contralateral first MTPJ (Figs 8, 9). Reduced sesamoid excursion can also be seen at dynamic US with a demonstrable gap in the SPL (9,41,42).
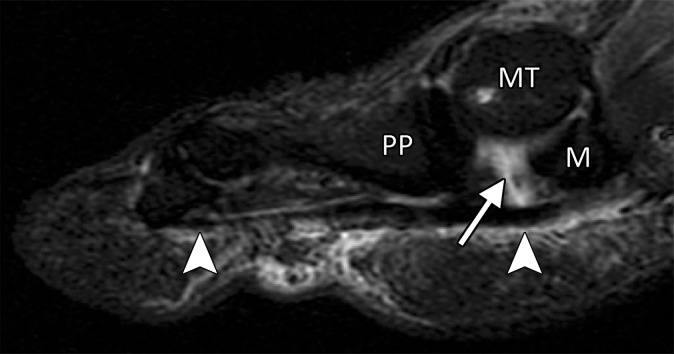
Figure 8a.
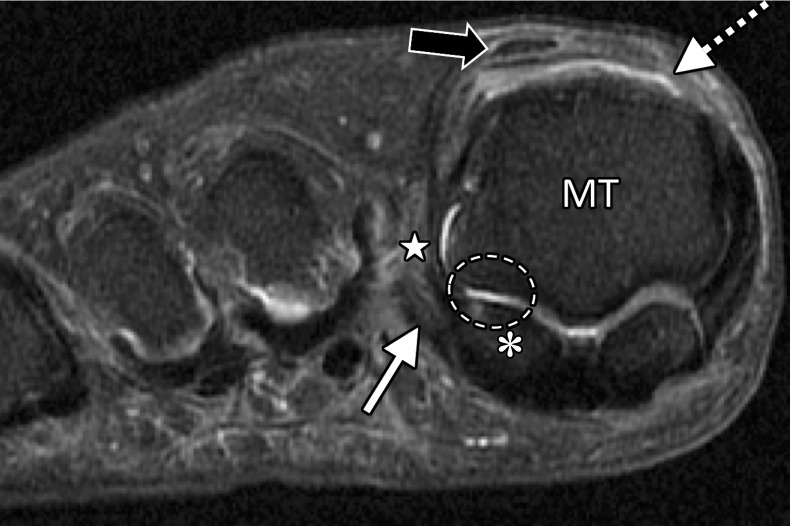
Turf toe in a 28-year-old professional American football player. Arrowheads = FHL, MT = first metatarsal. (a) Sagittal PDW FS image of the right first MTPJ shows complete tearing of the medial SPL (arrow). Additional high-grade tearing of the lateral SPL was apparent (not shown). PP = first proximal phalanx. (b, c) Coronal PDW FS images of the lateral (L) and medial (M) sesamoids (b) and just distal to the sesamoids (c) show the medial SPL tear extending into the ISL (★) and central plantar plate (*). Partial tearing of the medial MTSL (dotted arrow) is also seen. (d) Lateral dynamic dorsiflexed radiograph of both feet shows increased proximal migration of the right medial sesamoid compared to the left medial sesamoid. The medial sesamoids and proximal phalanges are outlined (dashed lines).
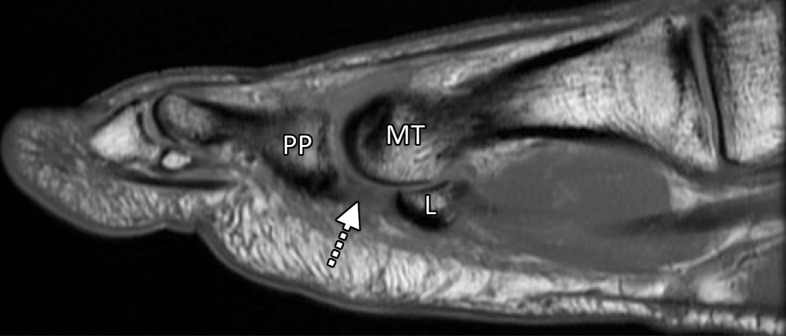
Figure 9a.
Turf toe in a 24-year-old professional football player. (a, b) Sagittal PDW (a) and sagittal PDW FS (b) images show complete tearing of the lateral SPL (arrow). Complete tearing of the medial SPL was also present (not shown). Slight proximal migration of the lateral (L) and medial (M) sesamoids is noted on the static MR images (a–c). MT = first metatarsal, PP = first proximal phalanx. (c) Axial (long-axis) PDW FS image shows marked edema at the plantar plate complex and lateral (dotted arrow) and medial (solid arrow) SPLs. (d) Lateral dynamic dorsiflexed radiograph of both feet shows proximal medial and lateral sesamoid migration in the right foot because of SPL tearing.
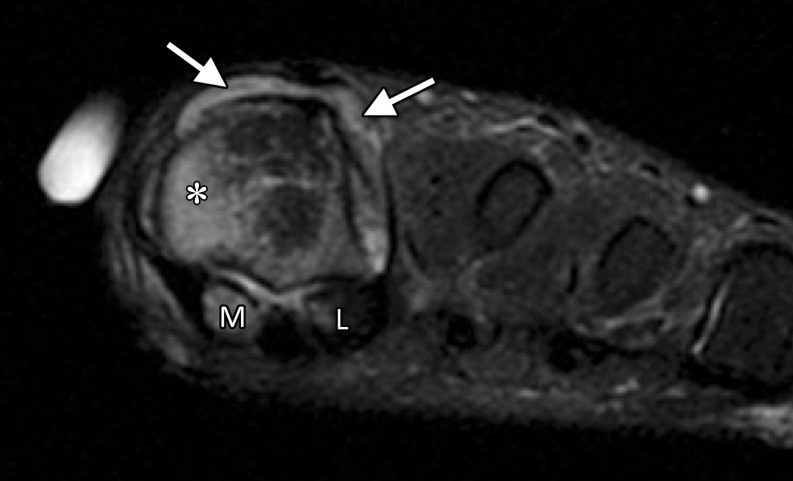
Figure 8b.
Turf toe in a 28-year-old professional American football player. Arrowheads = FHL, MT = first metatarsal. (a) Sagittal PDW FS image of the right first MTPJ shows complete tearing of the medial SPL (arrow). Additional high-grade tearing of the lateral SPL was apparent (not shown). PP = first proximal phalanx. (b, c) Coronal PDW FS images of the lateral (L) and medial (M) sesamoids (b) and just distal to the sesamoids (c) show the medial SPL tear extending into the ISL (★) and central plantar plate (*). Partial tearing of the medial MTSL (dotted arrow) is also seen. (d) Lateral dynamic dorsiflexed radiograph of both feet shows increased proximal migration of the right medial sesamoid compared to the left medial sesamoid. The medial sesamoids and proximal phalanges are outlined (dashed lines).
Figure 8c.
Turf toe in a 28-year-old professional American football player. Arrowheads = FHL, MT = first metatarsal. (a) Sagittal PDW FS image of the right first MTPJ shows complete tearing of the medial SPL (arrow). Additional high-grade tearing of the lateral SPL was apparent (not shown). PP = first proximal phalanx. (b, c) Coronal PDW FS images of the lateral (L) and medial (M) sesamoids (b) and just distal to the sesamoids (c) show the medial SPL tear extending into the ISL (★) and central plantar plate (*). Partial tearing of the medial MTSL (dotted arrow) is also seen. (d) Lateral dynamic dorsiflexed radiograph of both feet shows increased proximal migration of the right medial sesamoid compared to the left medial sesamoid. The medial sesamoids and proximal phalanges are outlined (dashed lines).
Figure 8d.
Turf toe in a 28-year-old professional American football player. Arrowheads = FHL, MT = first metatarsal. (a) Sagittal PDW FS image of the right first MTPJ shows complete tearing of the medial SPL (arrow). Additional high-grade tearing of the lateral SPL was apparent (not shown). PP = first proximal phalanx. (b, c) Coronal PDW FS images of the lateral (L) and medial (M) sesamoids (b) and just distal to the sesamoids (c) show the medial SPL tear extending into the ISL (★) and central plantar plate (*). Partial tearing of the medial MTSL (dotted arrow) is also seen. (d) Lateral dynamic dorsiflexed radiograph of both feet shows increased proximal migration of the right medial sesamoid compared to the left medial sesamoid. The medial sesamoids and proximal phalanges are outlined (dashed lines).
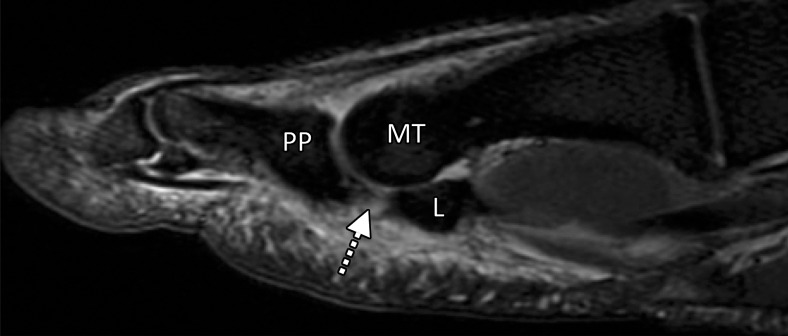
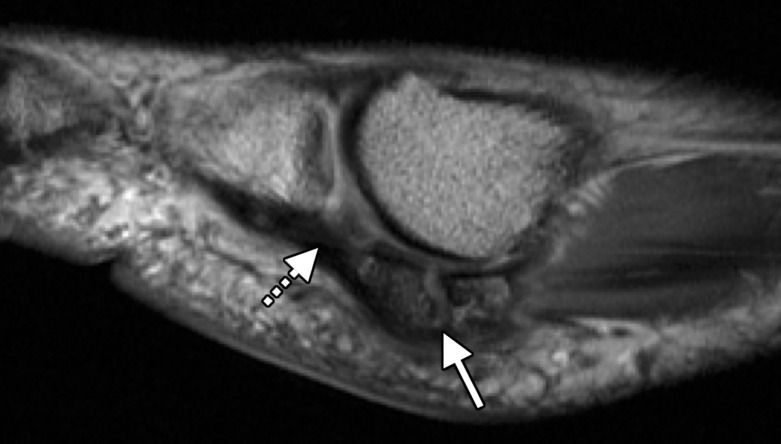
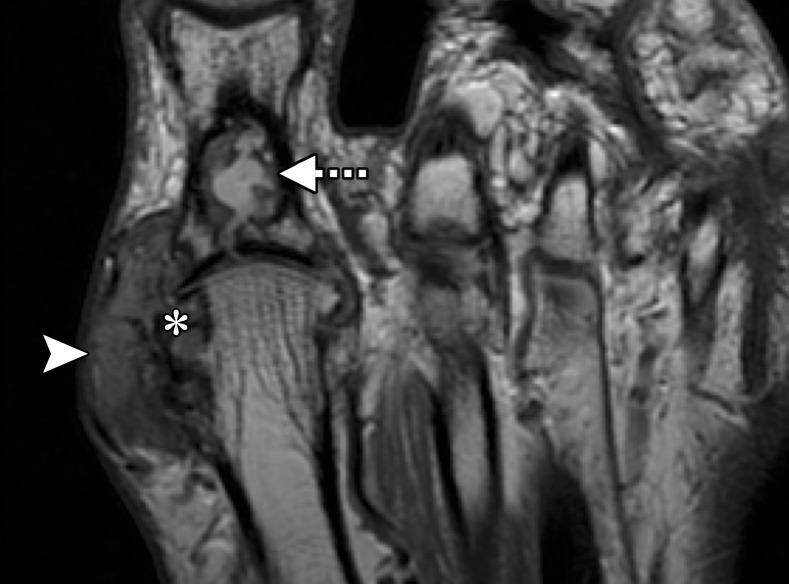
Figure 9b.
Turf toe in a 24-year-old professional football player. (a, b) Sagittal PDW (a) and sagittal PDW FS (b) images show complete tearing of the lateral SPL (arrow). Complete tearing of the medial SPL was also present (not shown). Slight proximal migration of the lateral (L) and medial (M) sesamoids is noted on the static MR images (a–c). MT = first metatarsal, PP = first proximal phalanx. (c) Axial (long-axis) PDW FS image shows marked edema at the plantar plate complex and lateral (dotted arrow) and medial (solid arrow) SPLs. (d) Lateral dynamic dorsiflexed radiograph of both feet shows proximal medial and lateral sesamoid migration in the right foot because of SPL tearing.
Figure 9c.
Turf toe in a 24-year-old professional football player. (a, b) Sagittal PDW (a) and sagittal PDW FS (b) images show complete tearing of the lateral SPL (arrow). Complete tearing of the medial SPL was also present (not shown). Slight proximal migration of the lateral (L) and medial (M) sesamoids is noted on the static MR images (a–c). MT = first metatarsal, PP = first proximal phalanx. (c) Axial (long-axis) PDW FS image shows marked edema at the plantar plate complex and lateral (dotted arrow) and medial (solid arrow) SPLs. (d) Lateral dynamic dorsiflexed radiograph of both feet shows proximal medial and lateral sesamoid migration in the right foot because of SPL tearing.
Figure 9d.
Turf toe in a 24-year-old professional football player. (a, b) Sagittal PDW (a) and sagittal PDW FS (b) images show complete tearing of the lateral SPL (arrow). Complete tearing of the medial SPL was also present (not shown). Slight proximal migration of the lateral (L) and medial (M) sesamoids is noted on the static MR images (a–c). MT = first metatarsal, PP = first proximal phalanx. (c) Axial (long-axis) PDW FS image shows marked edema at the plantar plate complex and lateral (dotted arrow) and medial (solid arrow) SPLs. (d) Lateral dynamic dorsiflexed radiograph of both feet shows proximal medial and lateral sesamoid migration in the right foot because of SPL tearing.
Skimboarder toe is another type of hyperextension injury at the first MTPJ (Fig 10). Skimboarders use their great toe for traction when mounting their boards. The board can slip posteriorly, leading to forced first MTPJ hyperextension and injury to the dorsal sagittal bands (extensor expansion). Unlike in turf toe, plantar plate involvement is less likely despite the similar mechanism of injury. This could relate to the reinforcement of the dorsal structures when wearing shoes in sports associated with turf toe injuries (43).
Figure 10a.
Skimboarder toe. Coronal T1-weighted (a) and T2-weighted FS (b) images show high-grade tearing of the medial sagittal band (arrowhead) and lateral subluxation of the extensor tendons (black arrow) due to forced hyperextension. Tearing of the medial capsular structures and collateral ligament is noted (white arrow) with additional medial sesamoiditis or degeneration. Skimboarders use their great toe for traction when mounting their waxed boards. The board can slip posteriorly, leading to forced first MTPJ hyperextension. L = lateral, M = medial.
Figure 10b.
Skimboarder toe. Coronal T1-weighted (a) and T2-weighted FS (b) images show high-grade tearing of the medial sagittal band (arrowhead) and lateral subluxation of the extensor tendons (black arrow) due to forced hyperextension. Tearing of the medial capsular structures and collateral ligament is noted (white arrow) with additional medial sesamoiditis or degeneration. Skimboarders use their great toe for traction when mounting their waxed boards. The board can slip posteriorly, leading to forced first MTPJ hyperextension. L = lateral, M = medial.
Proximal MTSL tears are less common than those of the SPLs and are better delineated at coronal imaging (Fig 11). MTSL tears usually result in less marked joint dysfunction, as the FHB attachments to the sesamoids remain intact (Fig 12). An even rarer injury is a tear of the ISL, which can result in increased distance between the sesamoids (Fig 8). This is best seen at coronal imaging and can result from chronic degenerative attrition or acute extreme hyperextension with hallux dislocation and associated extensive capsular and fibrocartilage rupture (9,17).
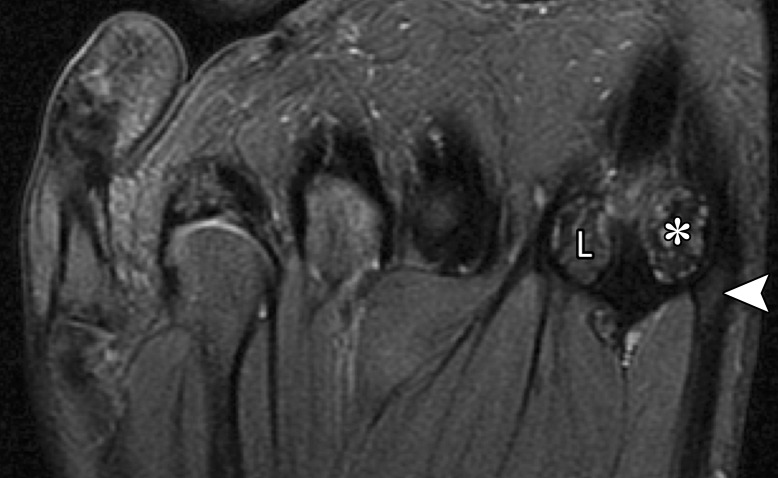
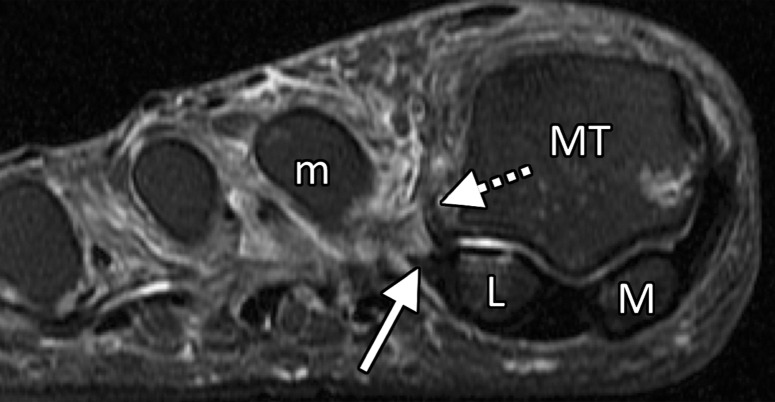
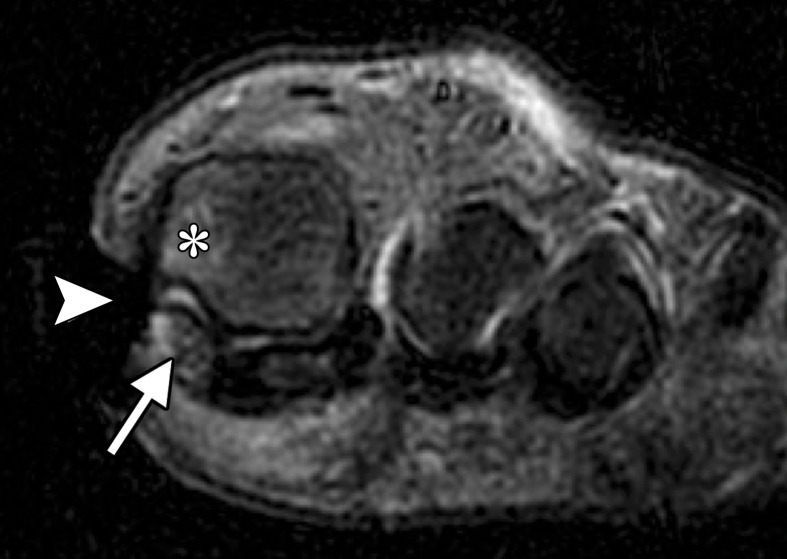
Figure 11a.
Medial MTSL tear in a 21-year-old man. Coronal (a) and axial (b) T2-weighted FS images show mild chondral loss (*) at the medial sesamoid and metatarsal head articulation. Partial tearing of the medial MTSL and capsular structures is seen with a fluid cleft at the sesamoid insertion (arrow). Thickening and altered signal intensity of the medial head of the FHB and abductor hallucis tendons (arrowhead) is compatible with tendinosis. These medial plantar structures interlink to prevent hallux valgus. L = lateral sesamoid, MT = first metatarsal.
Figure 12a.
Lateral MTSL tear in a 54-year-old woman with right hallux valgus and first web space pain. Coronal T2-weighted FS (a) and PDW (b) images show chondral loss at the lateral sesamoid (*) and first metatarsal articulation (dashed oval). There is partial tearing of the lateral MTSL (☆) with adjacent first web space edema and adductor hallucis tendinosis (solid white arrow). Medial sagittal band tearing (dotted arrow) and mild lateral subluxation of the extensor tendons (black arrow) are due to underlying hallux valgus. There is atrophy of the abductor hallucis and the FHB muscles (arrowheads) due to long-standing hallux valgus deformity. f = flexor hallucis longus tendon, MT = first metatarsal.
Figure 11b.
Medial MTSL tear in a 21-year-old man. Coronal (a) and axial (b) T2-weighted FS images show mild chondral loss (*) at the medial sesamoid and metatarsal head articulation. Partial tearing of the medial MTSL and capsular structures is seen with a fluid cleft at the sesamoid insertion (arrow). Thickening and altered signal intensity of the medial head of the FHB and abductor hallucis tendons (arrowhead) is compatible with tendinosis. These medial plantar structures interlink to prevent hallux valgus. L = lateral sesamoid, MT = first metatarsal.
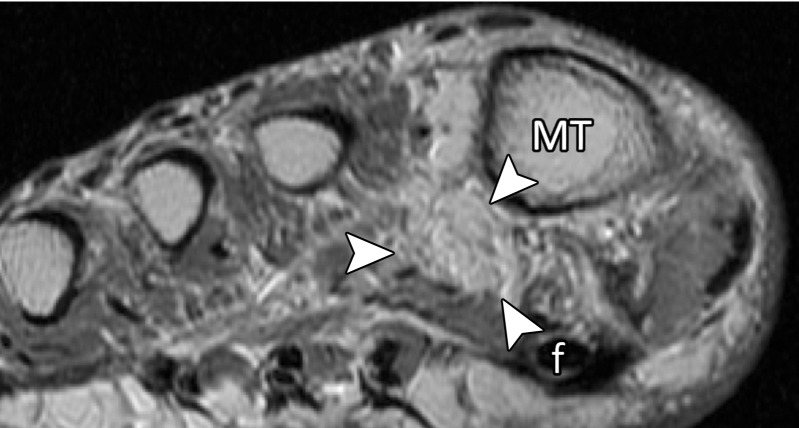
Figure 12b.
Lateral MTSL tear in a 54-year-old woman with right hallux valgus and first web space pain. Coronal T2-weighted FS (a) and PDW (b) images show chondral loss at the lateral sesamoid (*) and first metatarsal articulation (dashed oval). There is partial tearing of the lateral MTSL (☆) with adjacent first web space edema and adductor hallucis tendinosis (solid white arrow). Medial sagittal band tearing (dotted arrow) and mild lateral subluxation of the extensor tendons (black arrow) are due to underlying hallux valgus. There is atrophy of the abductor hallucis and the FHB muscles (arrowheads) due to long-standing hallux valgus deformity. f = flexor hallucis longus tendon, MT = first metatarsal.
Multidirectional hyperextension can result in varying degrees of associated varus or valgus injuries. Varus injuries are uncommon but can result in lateral capsular and adductor hallucis tendon injuries, along with lateral collateral ligament tears (Fig 13). Valgus injuries are more common and involve a traumatic hallux valgus with associated medial capsular, abductor hallucis, and medial collateral ligament tears (44,45).
Figure 13a.
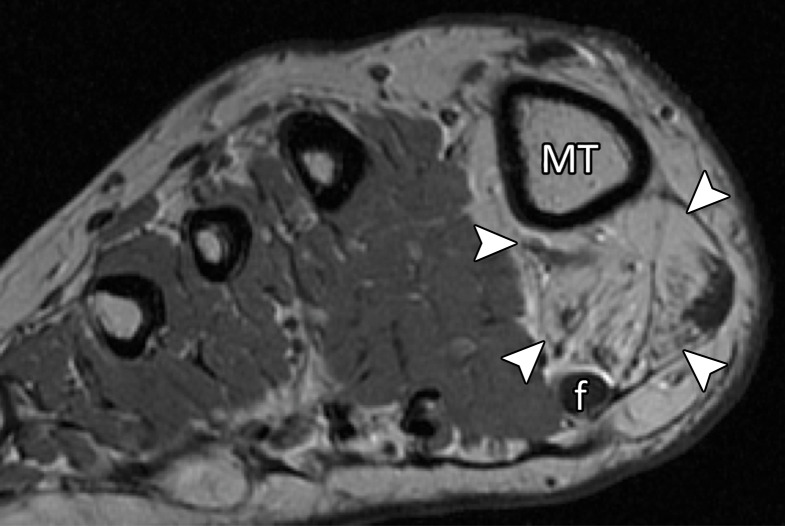
Lateral MTSL tear and adductor hallucis tendinosis and atrophy in a 69-year-old woman with hallux valgus and persistent foot pain. Coronal PDW (a, c) and T2-weighted FS (b) images show first MTPJ degenerative changes with chondral loss and subchondral edema most apparent at the lateral sesamoid (L) and metatarsal articulation. There is partial tearing of the lateral MTSL (dashed circle) and lateral collateral ligament (black arrow). More proximally in b, there is predislocation syndrome with edema surrounding the distal second (m) and third metatarsal shafts and MTPJs due to capsulitis. Tendinosis of the transverse (solid white arrow) and oblique (dotted arrow) heads of the adductor hallucis is apparent with fatty muscle atrophy (arrowheads) seen proximally in c. f = flexor hallucis longus tendon, M = medial sesamoid, MT = metatarsal.
Figure 13b.
Lateral MTSL tear and adductor hallucis tendinosis and atrophy in a 69-year-old woman with hallux valgus and persistent foot pain. Coronal PDW (a, c) and T2-weighted FS (b) images show first MTPJ degenerative changes with chondral loss and subchondral edema most apparent at the lateral sesamoid (L) and metatarsal articulation. There is partial tearing of the lateral MTSL (dashed circle) and lateral collateral ligament (black arrow). More proximally in b, there is predislocation syndrome with edema surrounding the distal second (m) and third metatarsal shafts and MTPJs due to capsulitis. Tendinosis of the transverse (solid white arrow) and oblique (dotted arrow) heads of the adductor hallucis is apparent with fatty muscle atrophy (arrowheads) seen proximally in c. f = flexor hallucis longus tendon, M = medial sesamoid, MT = metatarsal.
Figure 13c.
Lateral MTSL tear and adductor hallucis tendinosis and atrophy in a 69-year-old woman with hallux valgus and persistent foot pain. Coronal PDW (a, c) and T2-weighted FS (b) images show first MTPJ degenerative changes with chondral loss and subchondral edema most apparent at the lateral sesamoid (L) and metatarsal articulation. There is partial tearing of the lateral MTSL (dashed circle) and lateral collateral ligament (black arrow). More proximally in b, there is predislocation syndrome with edema surrounding the distal second (m) and third metatarsal shafts and MTPJs due to capsulitis. Tendinosis of the transverse (solid white arrow) and oblique (dotted arrow) heads of the adductor hallucis is apparent with fatty muscle atrophy (arrowheads) seen proximally in c. f = flexor hallucis longus tendon, M = medial sesamoid, MT = metatarsal.
Osseous and chondral injuries are common and occur in hyperextension injuries, chronic stress, or direct trauma. The sesamoids are the most commonly injured osseous structure (medial more commonly than lateral), as they overlie and shield the first metatarsal head and proximal phalanx (Fig 14). Trauma to the sesamoids may result in sesamoiditis, acute fracture, or diastasis of a partite sesamoid. Sesamoiditis is a painful inflammatory condition, which may manifest in the acute phase with increased signal intensity on fluid-sensitive MRI images because of marrow edema. The condition can also manifest with sclerosis in a more chronic phase, which can be difficult to differentiate from osteonecrosis (18,20). Radiography—or less commonly CT—is useful for depicting sesamoid sclerosis, which can appear with low signal intensity at MRI.
Figure 14a.
Bipartite sesamoiditis. (a–c) Axial (a) and sagittal T2-weighted FS (b) and sagittal (c) PDW images show medial sesamoiditis in a 24-year-old woman with pain at the plantar aspect of the right first MTPJ. There is a bifid appearance of the medial sesamoid with marrow edema (solid arrow in a and b) at both components. Smooth corticated margins and the presence of a waist at the superior margin of the sesamoid (arrow in c) are more suggestive of bipartite sesamoiditis rather than a fracture. Partial tearing of the medial SPL is also seen (dotted arrow). Radiographs were not available in this patient but are useful for assessment and follow-up. L = lateral sesamoid. (d, e) Dorsoplantar (d) and lateral (e) radiographs in a 15-year-old patient with plantar trauma show separation of two components at the medial sesamoid (dashed circles). This was a challenging case, with the proximal rounded margins of the distal component (arrowhead) suggestive of diastasis of a bipartite sesamoid rather than a fracture. Despite the challenges in differentiating the two conditions, fracture and diastasis are treated similarly with initial conservative management.
Figure 14b.
Bipartite sesamoiditis. (a–c) Axial (a) and sagittal T2-weighted FS (b) and sagittal (c) PDW images show medial sesamoiditis in a 24-year-old woman with pain at the plantar aspect of the right first MTPJ. There is a bifid appearance of the medial sesamoid with marrow edema (solid arrow in a and b) at both components. Smooth corticated margins and the presence of a waist at the superior margin of the sesamoid (arrow in c) are more suggestive of bipartite sesamoiditis rather than a fracture. Partial tearing of the medial SPL is also seen (dotted arrow). Radiographs were not available in this patient but are useful for assessment and follow-up. L = lateral sesamoid. (d, e) Dorsoplantar (d) and lateral (e) radiographs in a 15-year-old patient with plantar trauma show separation of two components at the medial sesamoid (dashed circles). This was a challenging case, with the proximal rounded margins of the distal component (arrowhead) suggestive of diastasis of a bipartite sesamoid rather than a fracture. Despite the challenges in differentiating the two conditions, fracture and diastasis are treated similarly with initial conservative management.
Figure 14c.
Bipartite sesamoiditis. (a–c) Axial (a) and sagittal T2-weighted FS (b) and sagittal (c) PDW images show medial sesamoiditis in a 24-year-old woman with pain at the plantar aspect of the right first MTPJ. There is a bifid appearance of the medial sesamoid with marrow edema (solid arrow in a and b) at both components. Smooth corticated margins and the presence of a waist at the superior margin of the sesamoid (arrow in c) are more suggestive of bipartite sesamoiditis rather than a fracture. Partial tearing of the medial SPL is also seen (dotted arrow). Radiographs were not available in this patient but are useful for assessment and follow-up. L = lateral sesamoid. (d, e) Dorsoplantar (d) and lateral (e) radiographs in a 15-year-old patient with plantar trauma show separation of two components at the medial sesamoid (dashed circles). This was a challenging case, with the proximal rounded margins of the distal component (arrowhead) suggestive of diastasis of a bipartite sesamoid rather than a fracture. Despite the challenges in differentiating the two conditions, fracture and diastasis are treated similarly with initial conservative management.
Figure 14d.

Bipartite sesamoiditis. (a–c) Axial (a) and sagittal T2-weighted FS (b) and sagittal (c) PDW images show medial sesamoiditis in a 24-year-old woman with pain at the plantar aspect of the right first MTPJ. There is a bifid appearance of the medial sesamoid with marrow edema (solid arrow in a and b) at both components. Smooth corticated margins and the presence of a waist at the superior margin of the sesamoid (arrow in c) are more suggestive of bipartite sesamoiditis rather than a fracture. Partial tearing of the medial SPL is also seen (dotted arrow). Radiographs were not available in this patient but are useful for assessment and follow-up. L = lateral sesamoid. (d, e) Dorsoplantar (d) and lateral (e) radiographs in a 15-year-old patient with plantar trauma show separation of two components at the medial sesamoid (dashed circles). This was a challenging case, with the proximal rounded margins of the distal component (arrowhead) suggestive of diastasis of a bipartite sesamoid rather than a fracture. Despite the challenges in differentiating the two conditions, fracture and diastasis are treated similarly with initial conservative management.
Figure 14e.
Bipartite sesamoiditis. (a–c) Axial (a) and sagittal T2-weighted FS (b) and sagittal (c) PDW images show medial sesamoiditis in a 24-year-old woman with pain at the plantar aspect of the right first MTPJ. There is a bifid appearance of the medial sesamoid with marrow edema (solid arrow in a and b) at both components. Smooth corticated margins and the presence of a waist at the superior margin of the sesamoid (arrow in c) are more suggestive of bipartite sesamoiditis rather than a fracture. Partial tearing of the medial SPL is also seen (dotted arrow). Radiographs were not available in this patient but are useful for assessment and follow-up. L = lateral sesamoid. (d, e) Dorsoplantar (d) and lateral (e) radiographs in a 15-year-old patient with plantar trauma show separation of two components at the medial sesamoid (dashed circles). This was a challenging case, with the proximal rounded margins of the distal component (arrowhead) suggestive of diastasis of a bipartite sesamoid rather than a fracture. Despite the challenges in differentiating the two conditions, fracture and diastasis are treated similarly with initial conservative management.
Sesamoid fractures (Fig 15) and traumatic diastasis of a bipartite sesamoid occur most commonly through the medial sesamoid and are difficult to differentiate at imaging. Radiography plays an important role in differentiation and can demonstrate findings more suggestive of fractures, including jagged irregular edges with nonsclerotic margins. In contradistinction, a bipartite sesamoid is more likely to demonstrate smooth rounded margins and a “waist” between the bony margins. In the setting of acute trauma, the distinction between nondisplaced fractures and traumatic diastasis may not affect management. Both conditions are usually treated conservatively, although symptomatic nonunion can be treated with surgical fixation or sesamoidectomy (46). The referring clinician should be made aware of chondral injuries, including loose osteochondral fragments. These may warrant surgical repair, and if left untreated, especially in the context of destabilizing first MTPJ injury, can rapidly progress to end-stage arthrosis (hallux rigidus) (47,48).
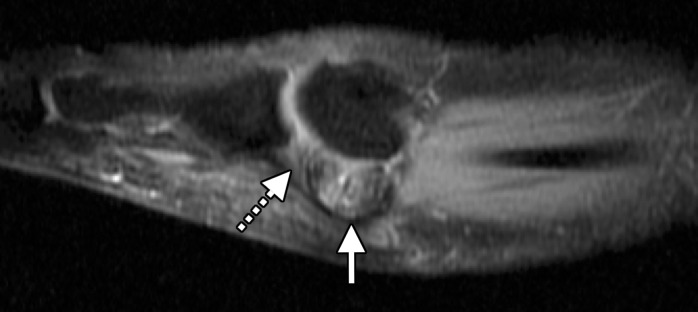
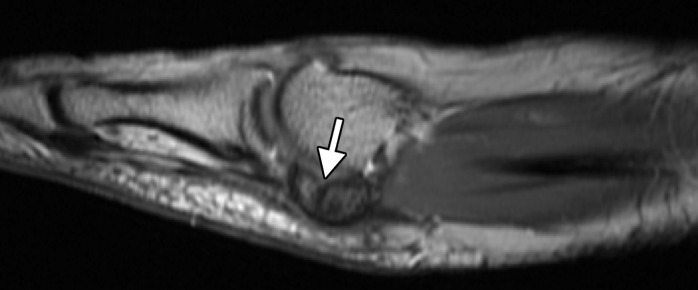
Figure 15a.
Sesamoid fracture. (a, b) Medial sesamoid fracture in a 32-year-old man after a fall. Axial T2-weighted FS (a) and sagittal PDW (b) images show an irregular cleft through the medial sesamoid with edema at the bony fragments and mild displacement likely caused by a fracture (solid white arrow). An intact medial SPL is apparent (dotted arrow). Differentiating a bipartite sesamoid from a fracture can be challenging. Irregular margins, displacement of the bony components, and a clear history of trauma are more suggestive of a fracture. Radiographs can be useful in assessment and follow-up, but radiographs were not available in this patient. L = lateral sesamoid. (c) Dorsoplantar radiograph in a 49-year-old woman with trauma to the medial sesamoid shows a cleft at the medial sesamoid with slightly irregular margins and no rounded waist (dashed circle). These imaging features are more suggestive of a fracture. (d, e) Dorsoplantar radiograph (d) obtained at 1-year follow-up and axial CT image (e) show interval osseous bridging due to healing. (f) Medial oblique radiograph in a 24-year-old woman shows an irregular fracture of the proximal lateral sesamoid (arrowhead) associated with a dislocation at the first MTPJ due to a motor vehicle accident.
Figure 15b.
Sesamoid fracture. (a, b) Medial sesamoid fracture in a 32-year-old man after a fall. Axial T2-weighted FS (a) and sagittal PDW (b) images show an irregular cleft through the medial sesamoid with edema at the bony fragments and mild displacement likely caused by a fracture (solid white arrow). An intact medial SPL is apparent (dotted arrow). Differentiating a bipartite sesamoid from a fracture can be challenging. Irregular margins, displacement of the bony components, and a clear history of trauma are more suggestive of a fracture. Radiographs can be useful in assessment and follow-up, but radiographs were not available in this patient. L = lateral sesamoid. (c) Dorsoplantar radiograph in a 49-year-old woman with trauma to the medial sesamoid shows a cleft at the medial sesamoid with slightly irregular margins and no rounded waist (dashed circle). These imaging features are more suggestive of a fracture. (d, e) Dorsoplantar radiograph (d) obtained at 1-year follow-up and axial CT image (e) show interval osseous bridging due to healing. (f) Medial oblique radiograph in a 24-year-old woman shows an irregular fracture of the proximal lateral sesamoid (arrowhead) associated with a dislocation at the first MTPJ due to a motor vehicle accident.
Figure 15c.

Sesamoid fracture. (a, b) Medial sesamoid fracture in a 32-year-old man after a fall. Axial T2-weighted FS (a) and sagittal PDW (b) images show an irregular cleft through the medial sesamoid with edema at the bony fragments and mild displacement likely caused by a fracture (solid white arrow). An intact medial SPL is apparent (dotted arrow). Differentiating a bipartite sesamoid from a fracture can be challenging. Irregular margins, displacement of the bony components, and a clear history of trauma are more suggestive of a fracture. Radiographs can be useful in assessment and follow-up, but radiographs were not available in this patient. L = lateral sesamoid. (c) Dorsoplantar radiograph in a 49-year-old woman with trauma to the medial sesamoid shows a cleft at the medial sesamoid with slightly irregular margins and no rounded waist (dashed circle). These imaging features are more suggestive of a fracture. (d, e) Dorsoplantar radiograph (d) obtained at 1-year follow-up and axial CT image (e) show interval osseous bridging due to healing. (f) Medial oblique radiograph in a 24-year-old woman shows an irregular fracture of the proximal lateral sesamoid (arrowhead) associated with a dislocation at the first MTPJ due to a motor vehicle accident.
Figure 15d.

Sesamoid fracture. (a, b) Medial sesamoid fracture in a 32-year-old man after a fall. Axial T2-weighted FS (a) and sagittal PDW (b) images show an irregular cleft through the medial sesamoid with edema at the bony fragments and mild displacement likely caused by a fracture (solid white arrow). An intact medial SPL is apparent (dotted arrow). Differentiating a bipartite sesamoid from a fracture can be challenging. Irregular margins, displacement of the bony components, and a clear history of trauma are more suggestive of a fracture. Radiographs can be useful in assessment and follow-up, but radiographs were not available in this patient. L = lateral sesamoid. (c) Dorsoplantar radiograph in a 49-year-old woman with trauma to the medial sesamoid shows a cleft at the medial sesamoid with slightly irregular margins and no rounded waist (dashed circle). These imaging features are more suggestive of a fracture. (d, e) Dorsoplantar radiograph (d) obtained at 1-year follow-up and axial CT image (e) show interval osseous bridging due to healing. (f) Medial oblique radiograph in a 24-year-old woman shows an irregular fracture of the proximal lateral sesamoid (arrowhead) associated with a dislocation at the first MTPJ due to a motor vehicle accident.
Figure 15e.

Sesamoid fracture. (a, b) Medial sesamoid fracture in a 32-year-old man after a fall. Axial T2-weighted FS (a) and sagittal PDW (b) images show an irregular cleft through the medial sesamoid with edema at the bony fragments and mild displacement likely caused by a fracture (solid white arrow). An intact medial SPL is apparent (dotted arrow). Differentiating a bipartite sesamoid from a fracture can be challenging. Irregular margins, displacement of the bony components, and a clear history of trauma are more suggestive of a fracture. Radiographs can be useful in assessment and follow-up, but radiographs were not available in this patient. L = lateral sesamoid. (c) Dorsoplantar radiograph in a 49-year-old woman with trauma to the medial sesamoid shows a cleft at the medial sesamoid with slightly irregular margins and no rounded waist (dashed circle). These imaging features are more suggestive of a fracture. (d, e) Dorsoplantar radiograph (d) obtained at 1-year follow-up and axial CT image (e) show interval osseous bridging due to healing. (f) Medial oblique radiograph in a 24-year-old woman shows an irregular fracture of the proximal lateral sesamoid (arrowhead) associated with a dislocation at the first MTPJ due to a motor vehicle accident.
Figure 15f.

Sesamoid fracture. (a, b) Medial sesamoid fracture in a 32-year-old man after a fall. Axial T2-weighted FS (a) and sagittal PDW (b) images show an irregular cleft through the medial sesamoid with edema at the bony fragments and mild displacement likely caused by a fracture (solid white arrow). An intact medial SPL is apparent (dotted arrow). Differentiating a bipartite sesamoid from a fracture can be challenging. Irregular margins, displacement of the bony components, and a clear history of trauma are more suggestive of a fracture. Radiographs can be useful in assessment and follow-up, but radiographs were not available in this patient. L = lateral sesamoid. (c) Dorsoplantar radiograph in a 49-year-old woman with trauma to the medial sesamoid shows a cleft at the medial sesamoid with slightly irregular margins and no rounded waist (dashed circle). These imaging features are more suggestive of a fracture. (d, e) Dorsoplantar radiograph (d) obtained at 1-year follow-up and axial CT image (e) show interval osseous bridging due to healing. (f) Medial oblique radiograph in a 24-year-old woman shows an irregular fracture of the proximal lateral sesamoid (arrowhead) associated with a dislocation at the first MTPJ due to a motor vehicle accident.
In contradistinction to turf toe, hyperflexion is a less common type of injury at the first MTPJ. This results in dorsal capsular and extensor tendon injury. It has been termed sand toe because of its relationship with beach volleyball (10).
Hallux Valgus and Hallux Rigidus
Osteoarthropathy at the first MTPJ and both metatarsosesamoid joints may result from prior traumatic injury but is typically associated with hallux valgus deformity and altered biomechanics (Fig 12). Hallux valgus manifests as lateral deviation of the great toe, and is usually diagnosed on the basis of standing dorsoplantar radiography, with the angle of the longitudinal axes of the proximal phalanx and metatarsal exceeding 15°. Hallux valgus is multifactorial and likely caused by a combination of anatomic variants such as a long first metatarsal, hypermobility, and extrinsic factors (eg, shoe type) (8).
Hallux valgus deformity typically begins with medial metatarsal head migration and lateral sesamoid subluxation followed by progressive valgus drift of the proximal phalanx. The medial capsular structures, especially the dorsal capsule, medial sagittal band, and collateral ligament, are stretched and partly torn. Tearing of the medial sagittal band may lead to lateralization of the extensor tendons (Fig 12). Over time, worsening deformity and prominent osteophytosis can result in attrition of the plantar plate complex, extensor tendons, lateral caspuloligamentous structures, and adductor hallucis tendons (8,49).
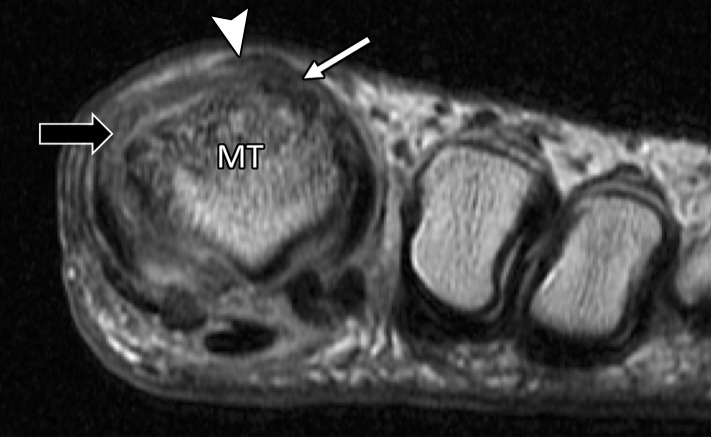
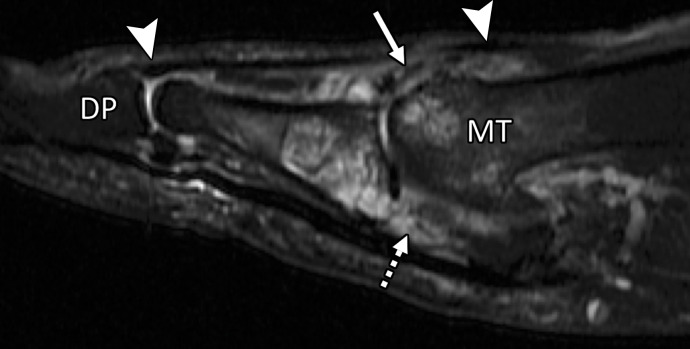
Tendinosis, partial tearing, or tenosynovitis of the extensor tendons may occur because of dorsal osteophytes and tendon lateralization in hallux valgus. These changes are typically most marked at the EHB, which is more closely related to the joint margin (Fig 16) (45).
Figure 16a.
Extensor tendon injury in a 70-year-old woman after resection of dorsal first MTPJ osteophytes (cheilectomy). Coronal PDW (a) and sagittal T2-weighted FS (b) images show partial tearing of the extensor tendons at the level of the metatarsal (MT) head, most marked at the EHB (solid white arrow) near the proximal phalanx insertion, with less marked changes at the EHL with an intact distal phalanx (DP) insertion (arrowheads). The dorsal medial sagittal band (black arrow) is partly torn with first MTPJ degeneration and subchondral cysts, along with tearing of the plantar plate complex distally (dotted arrow).
Figure 16b.
Extensor tendon injury in a 70-year-old woman after resection of dorsal first MTPJ osteophytes (cheilectomy). Coronal PDW (a) and sagittal T2-weighted FS (b) images show partial tearing of the extensor tendons at the level of the metatarsal (MT) head, most marked at the EHB (solid white arrow) near the proximal phalanx insertion, with less marked changes at the EHL with an intact distal phalanx (DP) insertion (arrowheads). The dorsal medial sagittal band (black arrow) is partly torn with first MTPJ degeneration and subchondral cysts, along with tearing of the plantar plate complex distally (dotted arrow).
Intermetatarsal bursitis of the first interspace, neuroma formation, and predislocation syndrome can also occur in hallux valgus. Predislocation syndrome is an inflammatory process in the lesser MTPJs, typically the second MTPJ, characterized by periarticular edema (adhesive capsulitis), which precedes lesser plantar plate disruption and dislocation (Fig 17) (50).
Figure 17a.
Collateral ligament tears and predislocation syndrome. Axial PDW (a) and coronal T2-weighted FS (b) images show hallux valgus with partial tears of the medial (solid arrow) and lateral (dotted arrow) collateral ligaments with first MTPJ degenerative changes. Capsular thickening and surrounding edema (arrowheads) are seen at the second MTPJ. These imaging features are consistent with adhesive capsulitis, which in association with hallux valgus is termed predislocation syndrome. As the name implies, if the underlying biomechanical abnormality is not corrected, the second MTPJ plantar plate will tear, resulting in instability and eventual dislocation. MT = first metatarsal.
Figure 17b.
Collateral ligament tears and predislocation syndrome. Axial PDW (a) and coronal T2-weighted FS (b) images show hallux valgus with partial tears of the medial (solid arrow) and lateral (dotted arrow) collateral ligaments with first MTPJ degenerative changes. Capsular thickening and surrounding edema (arrowheads) are seen at the second MTPJ. These imaging features are consistent with adhesive capsulitis, which in association with hallux valgus is termed predislocation syndrome. As the name implies, if the underlying biomechanical abnormality is not corrected, the second MTPJ plantar plate will tear, resulting in instability and eventual dislocation. MT = first metatarsal.
Surgical options for hallux valgus are numerous with over 100 different procedures described in the literature. The most basic surgery is described as a bunionectomy, consisting of resection of the medial eminence and medial capsular imbrication. This technique leads to a high rate of recurrence of symptoms, and most procedures now use a metatarsal osteotomy (eg, chevron) with the option of an additional proximal phalangeal osteotomy (eg, Akin procedure) for more severe hallux valgus (Fig 18) (8).
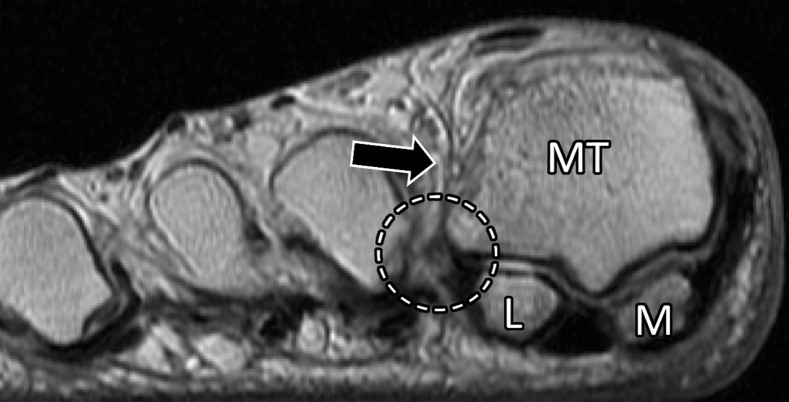
Figure 18a.
Treatment for hallux valgus. Axial PDW (a), coronal T2-weighted FS (b), and sagittal PDW (c) images in a 37-year-old man with reduced extension at the right first MTPJ who had hallux valgus corrective surgery 17 years earlier and hardware removed 1 year before. Postoperative changes and metallic artifacts are seen at the first metatarsal (MT) and proximal phalanx (PP) because of osteotomies. There is thickening of the medial collateral ligament (white arrow) and MTSL (☆) with postsurgical fibrosis appearing as low signal intensity along an attenuated medial sagittal band (arrowheads). Lateralization and tendinosis of the extensor tendons (black arrow) with underlying synovitis, fibrosis, and capsulitis (*) lead to reduced extension. The medial SPL (dotted arrow) shows only mild degeneration. L = lateral sesamoid, M = medial sesamoid.
Figure 18b.
Treatment for hallux valgus. Axial PDW (a), coronal T2-weighted FS (b), and sagittal PDW (c) images in a 37-year-old man with reduced extension at the right first MTPJ who had hallux valgus corrective surgery 17 years earlier and hardware removed 1 year before. Postoperative changes and metallic artifacts are seen at the first metatarsal (MT) and proximal phalanx (PP) because of osteotomies. There is thickening of the medial collateral ligament (white arrow) and MTSL (☆) with postsurgical fibrosis appearing as low signal intensity along an attenuated medial sagittal band (arrowheads). Lateralization and tendinosis of the extensor tendons (black arrow) with underlying synovitis, fibrosis, and capsulitis (*) lead to reduced extension. The medial SPL (dotted arrow) shows only mild degeneration. L = lateral sesamoid, M = medial sesamoid.
Figure 18c.
Treatment for hallux valgus. Axial PDW (a), coronal T2-weighted FS (b), and sagittal PDW (c) images in a 37-year-old man with reduced extension at the right first MTPJ who had hallux valgus corrective surgery 17 years earlier and hardware removed 1 year before. Postoperative changes and metallic artifacts are seen at the first metatarsal (MT) and proximal phalanx (PP) because of osteotomies. There is thickening of the medial collateral ligament (white arrow) and MTSL (☆) with postsurgical fibrosis appearing as low signal intensity along an attenuated medial sagittal band (arrowheads). Lateralization and tendinosis of the extensor tendons (black arrow) with underlying synovitis, fibrosis, and capsulitis (*) lead to reduced extension. The medial SPL (dotted arrow) shows only mild degeneration. L = lateral sesamoid, M = medial sesamoid.
Surgical options for established degenerative hallux rigidus include cheilectomy with removal of dorsal osteophytes and capsular release, and in more severe cases, arthrodesis or less commonly arthroplasty can be performed.
Postsurgical complications can be delineated at MRI and include infection, delayed bony union, ligamentous injury and fibrosis (Fig 18), and altered biomechanics leading to worsening first MTPJ osteoarthritis and insufficiency fractures of the lesser metatarsals (51,52).
Inflammation and Infection at First MTPJ
Crystalline arthropathies, such as gout, are common at the first MTPJ. Radiography is normally sufficient to demonstrate erosions and large tophi, although MRI can be used as a problem-solving tool to help assess the extent of any erosion, chondral defect, or injury to the soft-tissue supporting structures (Fig 19). Less commonly, inflammatory arthropathies, including rheumatoid arthritis (Fig 20) or psoriasis, can occur at the first MTPJ.
Figure 19a.
Gouty arthropathy at the first MTPJ in a 73-year-old man with left hallux valgus and first MTPJ pain and swelling. Coronal T2-weighted FS (a) and axial PDW (b) images show first MTPJ degenerative changes with a heterogeneous-signal-intensity soft-tissue mass medially (arrowheads) and bony erosion at the first metatarsal head (*). The underlying medial collateral ligament is poorly visualized, and there is a large proximal phalangeal cyst (dotted arrow) extending from the joint. These findings are compatible with a gouty tophus and intra-articular involvement.
Figure 20a.
Rheumatoid arthritis at the first MTPJ in a 32-year-old woman with known rheumatoid arthritis and first toe pain and stiffness. Coronal T2-weighted FS (a) and axial T1-weighted (b) images show prominent bone marrow edema at the first MTPJ, mainly involving the metatarsal head (*) as well as the medial (M) and lateral (L) sesamoids. These imaging findings are associated with joint effusion and synovial hypertrophy (solid arrows). An erosion is seen along the lateral aspect of the metatarsal head (dotted arrow). The constellation of findings suggests an inflammatory arthropathy.
Figure 19b.
Gouty arthropathy at the first MTPJ in a 73-year-old man with left hallux valgus and first MTPJ pain and swelling. Coronal T2-weighted FS (a) and axial PDW (b) images show first MTPJ degenerative changes with a heterogeneous-signal-intensity soft-tissue mass medially (arrowheads) and bony erosion at the first metatarsal head (*). The underlying medial collateral ligament is poorly visualized, and there is a large proximal phalangeal cyst (dotted arrow) extending from the joint. These findings are compatible with a gouty tophus and intra-articular involvement.
Figure 20b.
Rheumatoid arthritis at the first MTPJ in a 32-year-old woman with known rheumatoid arthritis and first toe pain and stiffness. Coronal T2-weighted FS (a) and axial T1-weighted (b) images show prominent bone marrow edema at the first MTPJ, mainly involving the metatarsal head (*) as well as the medial (M) and lateral (L) sesamoids. These imaging findings are associated with joint effusion and synovial hypertrophy (solid arrows). An erosion is seen along the lateral aspect of the metatarsal head (dotted arrow). The constellation of findings suggests an inflammatory arthropathy.
Infection of the first MTPJ is most commonly seen in patients with underlying diabetes (Fig 21) or a neuropathic osteoarthropathy. In the setting of severe degeneration with osseous sclerosis and subchondral cysts, diagnosis of osteomyelitis can be challenging. Radiography is useful in those with suspected first MTPJ or sesamoid osteomyelitis to help assess for erosions, bony destruction, or preexisting sclerosis, which can appear with low T1-weighted signal intensity at MRI. The MRI criteria for osteomyelitis, including low T1-weighted marrow signal intensity, will be more challenging to apply in preexisting sclerosis. In these cases, depiction of cortical destruction, surrounding soft tissue, or osseous collections at MRI provides a more specific diagnosis. Contrast-enhanced sequences are also useful to help assess the extent of bone marrow enhancement or involvement and to demonstrate any rim-enhancing soft tissue or osseous collections (40).
Figure 21a.
Methicillin-resistant Staphylococcus aureus (MRSA) osteomyelitis at the first MTPJ in a 70-year-old woman with a diabetic wound at the medial first toe. Coronal T1-weighted (a) and T2-weighted (b) FS images show a large soft-tissue ulcer along the medial aspect of the first MTPJ (arrowhead). There is irregularity and loss of the normal T1-weighted marrow signal at the medial sesamoid (arrow) with edema at the sesamoid and medial metatarsal head (*). These changes are suspicious for osteomyelitis. Soft-tissue swelling and edema around the first digit with a small first MTPJ effusion are also noted.
Figure 21b.
Methicillin-resistant Staphylococcus aureus (MRSA) osteomyelitis at the first MTPJ in a 70-year-old woman with a diabetic wound at the medial first toe. Coronal T1-weighted (a) and T2-weighted (b) FS images show a large soft-tissue ulcer along the medial aspect of the first MTPJ (arrowhead). There is irregularity and loss of the normal T1-weighted marrow signal at the medial sesamoid (arrow) with edema at the sesamoid and medial metatarsal head (*). These changes are suspicious for osteomyelitis. Soft-tissue swelling and edema around the first digit with a small first MTPJ effusion are also noted.
Conclusion
The first MTPJ is vital to the biomechanics of the foot, and injuries may lead to progressive orthopedic deformities along with eventual degenerative hallux rigidus. The plantar aspect of the first MTPJ comprises a plantar plate complex that provides static and dynamic stabilization.
In the setting of injury, providing precise descriptions of structures that contribute to first MTPJ stability enables optimal treatment choices. Turf toe injuries predominantly involve the paired SPLs of the plantar plate complex and can be depicted at high-resolution MRI and dorsiflexed lateral radiography. Hallux valgus is another common condition at the first MTPJ joint, and high-resolution MRI can help in pre- and postoperative assessment of associated osseous, chondral, and collateral ligament injuries.
Supported by grant R01 AR064321-01 from the National Institutes of Health and the VA Merit grant.
Recipient of a Cum Laude award for an education exhibit at the 2018 RSNA Annual Meeting.
For this journal-based SA-CME activity, the authors J.T.P.D.H. and C.B.C. have provided disclosures all other authors, the editor, and the reviewers have disclosed no relevant relationships.
Disclosures of Conflicts of Interest.—: J.T.P.D.H. Activities related to the present article: institution received a grant from the National Institutes of Health; institution received a U.S. Department of Veterans Affairs Merit Award. Activities not related to the present article: disclosed no relevant relationships. Other activities: disclosed no relevant relationships. C.B.C. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: institution received a grant from the National Institutes of Health; institution received funding from the Veterans Affairs San Diego Healthcare System. Other activities: disclosed no relevant relationships.
Abbreviations:
- EHB
- extensor hallucis brevis
- EHL
- extensor hallucis longus
- FHB
- flexor hallucis brevis
- FHL
- flexor hallucis longus
- FS
- fat-suppressed
- ISL
- intersesamoid ligament
- MTPJ
- metatarsophalangeal joint
- MTSL
- metatarsosesamoid ligament
- PDW
- proton density–weighted
- SPL
- sesamoid phalangeal ligament
References
- 1.Clanton TO, Ford JJ. Turf toe injury. Clin Sports Med 1994;13(4):731–741. [PubMed] [Google Scholar]
- 2.Wanivenhaus A, Pretterklieber M. First tarsometatarsal joint: anatomical biomechanical study. Foot Ankle 1989;9(4):153–157. [DOI] [PubMed] [Google Scholar]
- 3.Theumann NH, Pfirrmann CW, Mohana Borges AV, Trudell DJ, Resnick D. Metatarsophalangeal joint of the great toe: normal MR, MR arthrographic, and MR bursographic findings in cadavers. J Comput Assist Tomogr 2002;26(5):829–838. [DOI] [PubMed] [Google Scholar]
- 4.Schuenke M, Schulte E, Schumacher U. General Anatomy and Musculoskeletal System. New York, NY: Thieme, 2010; 410–419. [Google Scholar]
- 5.Stokes IA, Hutton WC, Stott JR. Forces acting on the metatarsals during normal walking. J Anat 1979;129(Pt 3):579–590. [PMC free article] [PubMed] [Google Scholar]
- 6.McCormick JJ, Anderson RB. Rehabilitation following turf toe injury and plantar plate repair. Clin Sports Med 2010;29(2):313–323, ix. [DOI] [PubMed] [Google Scholar]
- 7.Rodeo SA, O’Brien S, Warren RF, Barnes R, Wickiewicz TL, Dillingham MF. Turf-toe: an analysis of metatarsophalangeal joint sprains in professional football players. Am J Sports Med 1990;18(3):280–285. [DOI] [PubMed] [Google Scholar]
- 8.Smyth NA, Aiyer AA. Introduction: Why Are There so Many Different Surgeries for Hallux Valgus? Foot Ankle Clin 2018;23(2):171–182. [DOI] [PubMed] [Google Scholar]
- 9.Crain JM, Phancao JP. Imaging of Turf Toe. Radiol Clin North Am 2016;54(5):969–978. [DOI] [PubMed] [Google Scholar]
- 10.Linklater JM. Imaging of sports injuries in the foot. AJR Am J Roentgenol 2012;199(3):500–508. [DOI] [PubMed] [Google Scholar]
- 11.Potter HG, Pavlov H, Abrahams TG. The hallux sesamoids revisited. Skeletal Radiol 1992;21(7):437–444. [DOI] [PubMed] [Google Scholar]
- 12.Brenner E, Gruber H, Fritsch H. Fetal development of the first metatarsophalangeal joint complex with special reference to the intersesamoidal ridge. Ann Anat 2002;184(5):481–487. [DOI] [PubMed] [Google Scholar]
- 13.David RD, Delagoutte JP, Renard MM. Anatomical study of the sesamoid bones of the first metatarsal. J Am Podiatr Med Assoc 1989;79(11):536–544. [DOI] [PubMed] [Google Scholar]
- 14.Alvarez R, Haddad RJ, Gould N, Trevino S. The simple bunion: anatomy at the metatarsophalangeal joint of the great toe. Foot Ankle 1984;4(5):229–240. [DOI] [PubMed] [Google Scholar]
- 15.Burge AJ, Gold SL, Potter HG. Imaging of sports-related midfoot and forefoot injuries. Sports Health 2012;4(6):518–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucas DE, Philbin T, Hatic S, 2nd. The plantar plate of the first metatarsophalangeal joint: an anatomical study. Foot Ankle Spec 2014;7(2):108–112. [DOI] [PubMed] [Google Scholar]
- 17.McCormick JJ, Anderson RB. The great toe: failed turf toe, chronic turf toe, and complicated sesamoid injuries. Foot Ankle Clin 2009;14(2):135–150. [DOI] [PubMed] [Google Scholar]
- 18.Schein AJ, Skalski MR, Patel DB, et al. Turf toe and sesamoiditis: what the radiologist needs to know. Clin Imaging 2015;39(3):380–389. [DOI] [PubMed] [Google Scholar]
- 19.Haines RW, McDougall A. The anatomy of hallux valgus. J Bone Joint Surg Br 1954;36-B(2):272–293. [DOI] [PubMed] [Google Scholar]
- 20.Taylor JA, Sartoris DJ, Huang GS, Resnick DL. Painful conditions affecting the first metatarsal sesamoid bones. RadioGraphics 1993;13(4):817–830. [DOI] [PubMed] [Google Scholar]
- 21.Crain JM, Phancao JP, Stidham K. MR imaging of turf toe. Magn Reson Imaging Clin N Am 2008;16(1):93–103, vi. [DOI] [PubMed] [Google Scholar]
- 22.Doty JF, Coughlin MJ. Turf toe repair: a technical note. Foot Ankle Spec 2013;6(6):452–456. [DOI] [PubMed] [Google Scholar]
- 23.Drakos MC, Fiore R, Murphy C, DiGiovanni CW. Plantar-plate disruptions: “the severe turf-toe injury”—three cases in contact athletes. J Athl Train 2015;50(5):553–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Netter FH. Atlas of human anatomy. 6th ed. Philadelphia, Pa: Saunders/Elsevier, 2014. [Google Scholar]
- 25.Dedmond BT, Cory JW, McBryde A, Jr. The hallucal sesamoid complex. J Am Acad Orthop Surg 2006;14(13):745–753. [DOI] [PubMed] [Google Scholar]
- 26.Srinivasan R. The Hallucal-Sesamoid Complex: Normal Anatomy, Imaging, and Pathology. Semin Musculoskelet Radiol 2016;20(2):224–232. [DOI] [PubMed] [Google Scholar]
- 27.Allen LR, Flemming D, Sanders TG. Turf toe: ligamentous injury of the first metatarsophalangeal joint. Mil Med 2004;169(11):xix–xxiv. [PubMed] [Google Scholar]
- 28.Capasso G, Maffulli N, Testa V. Rupture of the intersesamoid ligament of a soccer player’s foot. Foot Ankle 1990;10(6):337–339. [DOI] [PubMed] [Google Scholar]
- 29.Douglas DP, Davidson DM, Robinson JE, Bedi DG. Rupture of the medial collateral ligament of the first metatarsophalangeal joint in a professional soccer player. J Foot Ankle Surg 1997;36(5):388–390. [DOI] [PubMed] [Google Scholar]
- 30.Appel M, Gradinger R. Morphology of the adductor hallux muscle and its significance for the surgical treatment of hallux valgus [in German]. Z Orthop Ihre Grenzgeb 1989;127(3):326–330. [DOI] [PubMed] [Google Scholar]
- 31.Standring S. Gray’s Anatomy. 40th ed. London, England: Churchill Livingstone/Elsevier, 2008; 1429–1462. [Google Scholar]
- 32.Le Double AF. Traité des Variations du Système Musculaire de l’Homme et de Leur Signification au Point de Vue de l’Anthropologie et Zoologique. Vol 2. Paris, France: Schleicher Frères, 1897; 373–428. [Google Scholar]
- 33.Nery C, Baumfeld D, Umans H, Yamada AF. MR Imaging of the Plantar Plate: Normal Anatomy, Turf Toe, and Other Injuries. Magn Reson Imaging Clin N Am 2017;25(1):127–144. [DOI] [PubMed] [Google Scholar]
- 34.Bowers KD, Jr, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports 1976;8(2):81–83. [PubMed] [Google Scholar]
- 35.Coughlin MJ, Kemp TJ, Hirose CB. Turf toe: soft tissue and osteocartilaginous injury to the first metatarsophalangeal joint. Phys Sportsmed 2010;38(1):91–100. [DOI] [PubMed] [Google Scholar]
- 36.Anderson RB. Turf toe injuries of the hallux metatarsophalangeal joint. Tech Foot Ankle Surg 2002;1(2):102–111. [Google Scholar]
- 37.Vopat ML, Hassan M, Poppe T, et al. Return to Sport After Turf Toe Injuries: A Systematic Review and Meta-analysis. Orthop J Sports Med 2019;7(10):2325967119875133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clough TM, Majeed H. Turf Toe Injury: Current Concepts and an Updated Review of Literature. Foot Ankle Clin 2018;23(4):693–701. [DOI] [PubMed] [Google Scholar]
- 39.Waldrop NE, 3rd, Zirker CA, Wijdicks CA, Laprade RF, Clanton TO. Radiographic evaluation of plantar plate injury: an in vitro biomechanical study. Foot Ankle Int 2013;34(3):403–408. [DOI] [PubMed] [Google Scholar]
- 40.Ashman CJ, Klecker RJ, Yu JS. Forefoot pain involving the metatarsal region: differential diagnosis with MR imaging. RadioGraphics 2001;21(6):1425–1440. [DOI] [PubMed] [Google Scholar]
- 41.Feuerstein CA, Weil L, Jr, Weil LS, Sr, Klein EE, Fleischer A, Argerakis NG. Static versus dynamic musculoskeletal ultrasound for detection of plantar plate pathology. Foot Ankle Spec 2014;7(4):259–265. [DOI] [PubMed] [Google Scholar]
- 42.Donegan RJ, Stauffer A, Heaslet M, Poliskie M. Comparing Magnetic Resonance Imaging and High-Resolution Dynamic Ultrasonography for Diagnosis of Plantar Plate Pathology: A Case Series. J Foot Ankle Surg 2017;56(2):371–374. [DOI] [PubMed] [Google Scholar]
- 43.Donnelly LF, Betts JB, Fricke BL. Skimboarder’s toe: findings on high-field MRI. AJR Am J Roentgenol 2005;184(5):1481–1485. [DOI] [PubMed] [Google Scholar]
- 44.York PJ, Wydra FB, Hunt KJ. Injuries to the great toe. Curr Rev Musculoskelet Med 2017;10(1):104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Linklater JM, Hayter CL, Vu D. Imaging of Acute Capsuloligamentous Sports Injuries in the Ankle and Foot: Sports Imaging Series. Radiology 2017;283(3):644–662. [DOI] [PubMed] [Google Scholar]
- 46.Bichara DA, Henn RF, 3rd, Theodore GH. Sesamoidectomy for hallux sesamoid fractures. Foot Ankle Int 2012;33(9):704–706. [DOI] [PubMed] [Google Scholar]
- 47.Kubitz ER. Athletic injuries of the first metatarsophalangeal joint. J Am Podiatr Med Assoc 2003;93(4):325–332. [DOI] [PubMed] [Google Scholar]
- 48.Mason LW, Molloy AP. Turf toe and disorders of the sesamoid complex. Clin Sports Med 2015;34(4):725–739. [DOI] [PubMed] [Google Scholar]
- 49.Schweitzer ME, Maheshwari S, Shabshin N. Hallux valgus and hallux rigidus: MRI findings. Clin Imaging 1999;23(6):397–402. [DOI] [PubMed] [Google Scholar]
- 50.Mendicino RW, Statler TK, Saltrick KR, Catanzariti AR. Predislocation syndrome: a review and retrospective analysis of eight patients. J Foot Ankle Surg 2001;40(4):214–224. [DOI] [PubMed] [Google Scholar]
- 51.Tomlinson M. Pain after cheilectomy of the first metatarsophalangeal joint: diagnosis and management. Foot Ankle Clin 2014;19(3):349–360. [DOI] [PubMed] [Google Scholar]
- 52.Sofka CM. Postoperative magnetic resonance imaging of the foot and ankle. J Magn Reson Imaging 2013;37(3):556–565. [DOI] [PubMed] [Google Scholar]