Primary open angle glaucoma is a leading cause of visual impairment that is characterized by cupping of the optic disc and stereotypical patterns of visual field loss. While high intraocular pressure (IOP) is a risk factor for developing disease, glaucoma can occur at any pressure. Glaucoma that occurs with maximum lOPs of less than 21 mm Hg has been termed normal tension glaucoma (NTG). Glaucoma is highly heritable and many genes that contribute to the pathogenesis of NTG have been discovered. Mutations in either optineurin (OPTN),1 TANK-binding kinase 1 (TBK1),2 or myocilin (MYOC)3 are each capable of causing glaucoma with little influence from other genetic or environmental factors. Mutations in these genes are responsible for approximately 3% of NTG.1–3
TBK1-associated NTG is caused by duplication or triplication of the normal TBK1 gene sequence. These TBK1 gene-dosage mutations have been detected in African American,2 Caucasian,2,4,5 and Asian6,7 NTG patients and have not been identified in the genomes of over 10,000 individuals in a large public database (gnomAD.broadinstitute.org). TBK1 gene duplication and triplication mutations are associated with early-onset glaucoma that frequently presents with large cup-to-disc ratios and maximum lOPs of < 21 mm Hg.2 Prior studies of TBK1-associated NTG have reported a mean age at diagnosis of 29 to 36 years; mean cup-to-disc ratio of 0.85 to 0.93 at first examination; and mean maximum IOP of 18 to 19 mm Hg.2 Some NTG patients with TBK1 mutations have thin central corneas, however, a broad range of corneal thickness has been observed in this patient population.2,5 Typical glaucomatous visual fields have been detected in patients with TBK1-associated glaucoma, including arcuate defects, nasal steps, central defects, and generalized constriction.2 Although many key features of the clinical phenotype of TBK1-associated glaucoma have been described, studies of disease progression for this molecularly-defined type of NTG have not yet been reported.
In this case-report, we present genetic testing results for a female with familial NTG and a retrospective 20-year review of her clinical course. Written informed consent was obtained from study participants and research was conducted with the approval and ethical review by the University of Iowa’s Internal Review Board and adhered to the tenets of the Declaration of Helsinki.
The patient, her mother, and her maternal aunt all have been diagnosed with NTG. Given our patient’s strong family history of NTG, we tested her DNA for the most commonly observed NTG mutations: Glu50Lys in OPTN, a gene duplication of TBK1, and Gln368Ter in MYOC using real-time PCR assays as previously described.2,3 While the OPTN and MYOC tests were negative, we did detect a TBK1 gene duplication. We subsequently confirmed the TBK1 gene duplication and determined the precise location of its borders on chromosome 12q14 (64,681,095–65,187,566) using chromosome microarray analysis. This TBK1 gene duplication has novel borders when compared to prior reports.2,5
The patient is a Hispanic Caucasian female with a complex ophthalmic history. She was initially evaluated by an ophthalmologist at age three because of anisocoria. At age ten she developed esotropia. She was determined to have a slowly progressive right third nerve palsy that spared her levator. Multiple magnetic resonance imaging scans and angiography failed to determine an etiology and a diagnosis of a schwannoma was considered. She has myopia with anisometropia (−1.50 +1.50 × 090 OD and −5.75 sphere OS) and has required three strabismus surgeries.
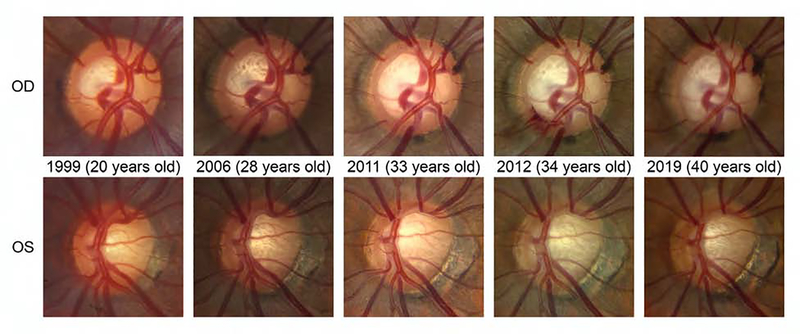
At age 17, during one of her many neuro-ophthalmology examinations, she was noted to have cup-to-disc asymmetry. By age 33 she had documented increased cupping (Figure 1) with thinning of the retinal nerve fiber layer on ocular coherence tomography (OCT) (Supplementary Figure 1). Her lOPs were 12 mmHg in both eyes. Central corneal thicknesses were 546 microns OU. Her Humphrey visual fields were normal (Supplemental Figure 2). Diurnal measurements of IOP were 9 –14 mmHg OD and 9 – 13 mmHg OS. She was diagnosed with pre-perimetric NTG. The patient had symptoms of orthostatic hypotension and typically maintained a blood pressure (BP) in the range of 90/55 mmHg. A 24-hour BP study revealed a minimum nocturnal BP of 80/46. She was treated with a high salt diet. At age 34 a disc hemorrhage was detected OD (Figure 1) when her IOP was 12 mm Hg. An OCT at this time demonstrated thinning of the retinal nerve fiber layer and marked ganglion cell loss (Supplementary Figure 1). Latanoprost was begun with no significant change in her lOPs. With or without treatment her lOPs were between 10 and 12 mmHg OU. It was determined that no medication would lower her IOP from this range and that the next step in treatment would be a trabeculectomy.
Figure 1. Serial optic disc photos in a patient with pre-perimetric NTG caused by a TBK1 gene duplication.
Optic disc photos obtained over 20 years demonstrate progressive cupping and progressive peripapillary atrophy in both eyes. In 2012, a disc hemorrhage was detected in the right eye at 7–8 o’clock. In 2019, increased cupping was detected in the right eye in the same location (7–8 o’clock). The configuration of retinal vessels at the optic disc was also noted to shift during course of progressive cupping.
Over the course of the next 6 years of follow up examinations the patient’s IOP remained < 12 mm of Hg OU and no obvious glaucomatous visual field changes were observed. Mild, nonspecific reductions in visual field sensitivity were, however, detected (OS > OD) that might represent early functional damage from glaucoma (Supplementary Figure 2).
In summary, we present a patient with a duplication in TBK1 who demonstrates progressive optic nerve cupping with low IOP at a young age that is consistent with pre-perimetric NTG. Her right third nerve palsy is most likely unrelated to the bilateral cupping and glaucoma. To our knowledge, TBK1 gene duplications have not been detected in other patients with third nerve palsy. Her complex ophthalmic history did, however, bring her to the attention of ophthalmologists who could document her progressive cupping at low-normal lOPs. One should consider testing for mutations in TBK1 in young patients with progressive optic nerve cupping at normal lOP’s and those NTG patients with TBK1 mutations may require very low target IOP to limit progression (i.e. < 10–12 mmHg).
Supplementary Material
Supplemental Figure 1. Serial OCT in a patient with pre-perimetric NTG caused by a TBK1 gene duplication. OCT tests obtained over 8 years demonstrate a thin nerve fiber layer in both eyes, especially in the superior and inferior quadrants. Macular thickness scans also demonstrate a thin retinal ganglion cell complex in both eyes. These OCT tests demonstrate relatively stable optic nerve parameters.
Supplemental Figure 2. Serial visual field tests in a patient with pre-perimetric NTG caused by a TBK1 gene duplication. A. HVF 24-2 tests obtained over 17 years demonstrate a gradual generalized decrease in sensitivity in the right eye and a persistence of essentially full visual fields in the left eye. B. Full HVF 10-2 tests in both eyes. While these visual field tests do not identify changes specific for glaucoma, the progressive reduction in sensitivity of the visual field tests of the right eye could be due to early glaucoma.
Acknowledgements
This research was supported in part by NIH RO1EY023512 and Research to Prevent Blindness, The Hadley-Carver Chair in Glaucoma, and the Don Heineking Research Fund.
Footnotes
We present a young patient with progressive optic disc cupping characteristic of normal tension glaucoma. Genetic testing revealed a TBK1 gene duplication and clinic characteristics of her pre-perimetric glaucoma are discussed in this context.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rezaie T, Child A, Hitchings R, et al. Adult-onset primary open-angle glaucoma caused by mutations in optineurin. Science 2002;295:1077–1079. [DOI] [PubMed] [Google Scholar]
- 2.Fingert JH, Robin AL, Roos Ben R, et al. Copy number variations on chromosome 12q14 in patients with normal tension glaucoma. Hum Mol Genet 2011;20:2482–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alward WLM, van der Heide CJ, Khanna CL, et al. Myocilin mutations in normal tension glaucoma patients. JAMA ophthalmology 2019;in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ritch R, Darbro B, menon G, et al. TBK1 Gene Duplication and Normal-Tension Glaucoma. JAMA ophthalmology 2014;132:544–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Awadalla MS, Fingert JH, Roos BE, et al. Copy Number Variations of TBK1 in Australian Patients With Primary Open-Angle Glaucoma. Am J Ophthalmol 2015;159:124–130.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kawase K, Allingham RR, Meguro A, et al. Confirmation of TBK1 duplication in normal tension glaucoma. Exp Eye Res 2012;96:178–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaurani L, Vishal M, Ray J, et al. TBK1 duplication is found in normal tension and not in high tension glaucoma patients of Indian origin. J Genet 2016;95:459–461. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Serial OCT in a patient with pre-perimetric NTG caused by a TBK1 gene duplication. OCT tests obtained over 8 years demonstrate a thin nerve fiber layer in both eyes, especially in the superior and inferior quadrants. Macular thickness scans also demonstrate a thin retinal ganglion cell complex in both eyes. These OCT tests demonstrate relatively stable optic nerve parameters.
Supplemental Figure 2. Serial visual field tests in a patient with pre-perimetric NTG caused by a TBK1 gene duplication. A. HVF 24-2 tests obtained over 17 years demonstrate a gradual generalized decrease in sensitivity in the right eye and a persistence of essentially full visual fields in the left eye. B. Full HVF 10-2 tests in both eyes. While these visual field tests do not identify changes specific for glaucoma, the progressive reduction in sensitivity of the visual field tests of the right eye could be due to early glaucoma.