Abstract
Repair of medial meniscus posterior root tear (MMPRT) is considered as an effective early intervention strategy for osteoarthritis. We aimed at evaluating whether or not single-photon emission computed tomography/computed tomography (SPECT/CT) could predict the treatment outcome.
Eleven patients with MMPRT who underwent preoperative SPECT/CT were retrospectively enrolled. Clinical symptoms were evaluated based on the knee injury and osteoarthritis outcome score (KOOS) and visual analogue scale (VAS) for pain. The uptake pattern of the medial tibial plateau (MTP) on SPECT/CT was visually assessed. Additionally, the maximum lesion-to-cortical counts ratio (LCRmax) for the anterior and posterior aspects of MTP and anterior-posterior MTP ratio (APR) were quantitatively assessed. Spearman correlation analyses were performed between the change in clinical symptom scores and preoperative SPECT/CT patterns.
All patients showed increased radiotracer uptake in MTP. Among them, 8 (73%) showed dominant uptake in the anterior aspect of MTP. The rest 3 (27%) showed posterior-dominant uptake. Patients with anterior-dominant patterns tended to show better outcomes in terms of the postoperative KOOS score (P = .07). Anterior MTP LCRmax showed a negative correlation with the change in VAS (ρ = −0.664, P < .03). APR showed a correlation with the change in the KOOS score (ρ = 0.655, P < .03).
Patients with MMPRT with relatively higher uptake in the anterior aspect of MTP could have better clinical outcomes after the repair. The preoperative SPECT/CT pattern may have a predictive value in selecting patients with good postoperative outcomes.
Keywords: bone scan, medial meniscus posterior root tear, meniscal root repair, osteoarthritis, single-photon emission computed tomography/computed tomography
1. Introduction
Medial meniscus posterior root tear (MMPRT) profoundly affects the meniscal biomechanics and kinematics, leading to accelerated degenerative changes of the knee joint.[1–4] It is associated with clinically significant meniscal extrusion, which can affect impairment of hoop stress force transmission causing accelerated degenerative articular wear.[5] A biomechanical study compared the peak tibiofemoral contact pressure of MMPRT as similar to a total medial meniscectomized knee.[6] In this regard, the treatment of meniscal root tears has recently evolved into various repair strategies to restore meniscal function both biomechanically and clinically, thus preventing degenerative changes of the knee.[7]
However, the effect of MMPRT repair is debatable, particularly in terms of the prognostic outcome after the treatment. Although arthroscopic pull-out repair of the MMPRT has shown favorable clinical and radiographic results,[8,9] results tend to vary among individuals, particularly at long-term follow-ups.[10] An explainable cause of variability in the effect of MMPRT repair is the heterogeneity of early osteoarthritis. For instance, varus alignment and chondral lesions were prone to inferior outcomes after MMPRT repair.[11] Meniscus extrusion is associated with poor results after conservative treatment for MMPRT.[12] Nonetheless, evidence of baseline characteristics predicting the future outcome of the MMPRT repair has been limited. Therefore, appropriate selection of patients who would benefit from the treatment by using functional characteristics could be a critical issue in the efficacy of MMPRT repair.
The purpose of this study was to evaluate whether or not preoperative single-photon emission computed tomography (SPECT)/computed tomography (CT) findings could predict the outcome of MMPRT repair. Bone scanning is the gold-standard modality for assessing skeletal disorders, particularly with its advancements through SPECT/CT. In contrast to magnetic resonance imaging (MRI), SPECT/CT as a hybrid imaging modality can provide information on osseous physiology and metabolism as well as structural abnormalities.[13] SPECT/CT can theoretically demonstrate an abnormality before a morphologic change is detectable with other anatomical imaging modalities.[14] As functional information provided by bone SPECT/CT may be associated with the heterogeneity of osteoarthritis, a specific type of osteoarthritis identified by the SPECT/CT pattern could be related to the outcome of MMPRT.
2. Methods
2.1. Subjects
As an observational study, we retrospectively enrolled patients with early osteoarthritis who had undergone MMPRT repair. Patients diagnosed with acute or chronic MMPRT on MRI were initially treated with non-surgical methods for 3 months. MMPRT was diagnosed on MRI and defined as radial tear within 5 mm of the posterior bony attachment of the medial meniscus.[15] Conservative therapy consisted of activity modification, which prohibited patients from squatting or climbing stairs, applying an ice pack, taking anti-inflammatory drugs or analgesics, and controlling weight. If pain and functional disability decreased after 3 months of conservative treatment, the patient was consistently followed-up without surgery. However, if the patient's pain persisted with an increased functional disability after 3 months of conservative treatment, arthroscopic meniscectomy or meniscus repair was performed according to the reparability of the meniscus. Contraindications of MMPRT repair included a Kellgren–Lawrence grade of 3 or more on plain radiographs and asymmetric varus alignment (hip–knee–ankle angle of more than 5°) on long cassette radiographs.
For MMPRT repair, a single experienced surgeon performed arthroscopic transosseous pullout suture repair for all patients at a single institution. The rehabilitation protocol applied for all patients was as follows: restriction of the range of motion within 90° with toe-touch weight-bearing and isometric quadriceps contraction in extension for 4 weeks, followed by a further range of motion exercise and weight-bearing after 4 weeks. Clinical results were evaluated using the pre- and post-operative knee injury and osteoarthritis outcome scores (KOOSs) and visual analog scale (VAS) for pain. The temporal variation in scores was recorded.
Between April 2014 and November 2016, 20 patients diagnosed with MMPRT underwent preoperative SPECT/CT and MMPRT repair. Among them, 11 patients (all women, 59.6 ± 5.2 years) underwent pre- and postoperative clinical evaluations for 12 months or more.
2.2. Imaging
Bone planar imaging was acquired 3 hours after an intravenous injection of 740 MBq (20 mCi) of 99mTc-3,3-diphosphono-1,2-propanedicarboxylic acid, followed by SPECT/CT of the distal femoral shaft to the proximal tibial shaft. SPECT/CT acquisition was performed on a hybrid dual-head gamma camera and 16-slice CT scanner (Discovery NM/CT 670, GE Healthcare, Waukesha, WI, US). SPECT scans were acquired using a low-energy high resolution collimator with 360° orbit, 120 steps (20 s/step), and 128 × 128 matrix, while the CT part of SPECT/CT used 16-detector row helical CT with 120 kVp, 40 mAs, 1 s gantry rotation, and reconstructed section thickness of 3.75 mm.
2.3. Image analysis
The tracer uptake was visually assessed for the anterior and posterior aspects of the medial tibial plateau (MTP). More specifically, more than 2 experienced nuclear medicine physicians visually reviewed the uptake pattern of the anterior and posterior aspects of MTP. The anterior and posterior aspects of MTPs were divided by a hypothetical line based on the tibial eminence. Accordingly, patients were divided into 2 groups based on the aspect of MTP with dominant uptake: anterior and posterior.
For quantitative analyses, the reference tracer uptake was measured in the cortex of the femoral diaphysis by using manually drawn volume-of-interests (VOIs). Subsequently, the maximum lesion-to-cortical count ratio (LCRmax) for both anterior and posterior MTPs was calculated. VOIs were drawn for the anterior and posterior aspects of MTP considering the hypothetical line based on the tibial eminence aforementioned. As another parameter, the anterior–posterior MTP LCRmax ratio (APR) was also assessed. Quantitative and visual analyses were performed with an imaging analysis software package (Syngo.via, Siemens Healthcare, Erlangen, Germany).
2.4. Statistical analysis
Spearman correlation analyses were performed to evaluate the association between changes in the clinical symptom score and SPECT parameters, including LCRmax and APR. A P-value < .05 was considered significantly different. All statistical calculations were performed using MedCalc Statistical Software version 19.0.5 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2019).
2.5. Ethics approval and consent to participate
All procedures in this study that involved human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and complied with tenets of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards (SNUH IRB No. 1908-083-1054).
3. Results
Visual analyses revealed that all 11 (100%) patients showed increased tracer uptake in MTP on the injured side of the knee. Among them, 8 (73%) showed dominant uptake in the anterior aspect of MTP (Fig. 1a). The rest 3 (27%) showed dominant uptake in the posterior aspect of MTP (Fig. 1b). Table 1 summarizes the uptake pattern, whether anterior- or posterior-dominant uptake, in MTP. The group with anterior-dominant uptake tended to show better outcomes in terms of the postoperative change in the KOOS score, although without statistical significance (Fig. 1c, median: 127 vs 65.5, respectively; P = .07).
Figure 1.
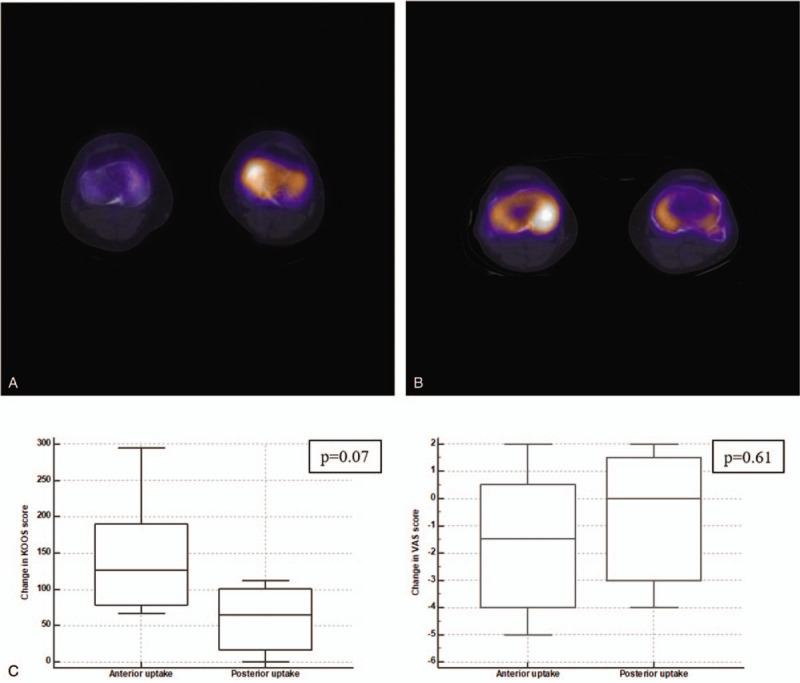
Visual patterns of single-photon emission computed tomography/computed tomography (SPECT/CT) and postoperative symptom improvement. a, b. Representative SPECT/CT images of the anterior- and posterior-dominant pattern of uptake in the medial tibial plateau. c. The group with anterior-dominant patterns tended to show better outcomes in terms of changes in the postoperative knee injury and osteoarthritis outcome score, although without statistical significance. The visual analogue scale did not show any noticeable correlation with the uptake pattern.
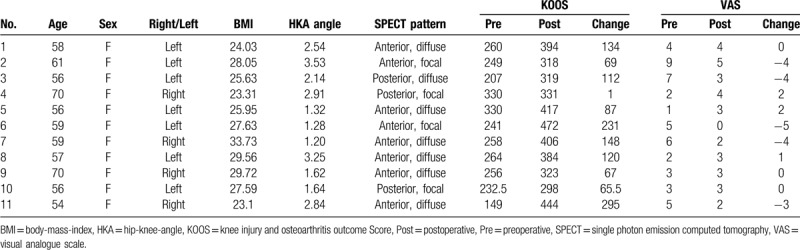
Table 1.
Baseline characteristics and qualitative results of patients.
We also performed a quantitative analysis for evaluating whether a pattern of preoperative SPECT finding was associated with postoperative outcome. The LCRmax of anterior MTP showed a significant negative correlation with the postoperative change in VAS (ρ = -0.664, P < .03) (Fig. 2). LCRmax of anterior MTP and the postoperative change in the KOOS score tended to show a positive correlation, although without statistical significance (ρ = 0.418, P = .20). The LCRmax of posterior MTP showed no correlation with either of the clinical symptom scores. As another quantitative value representing the ratio of the anterior uptake to the posterior uptake, APR showed a significant correlation with the postoperative change in the KOOS score (ρ = 0.655, P < .03) but not with the VAS score (ρ = -0.464, P = .15) (Fig. 3).
Figure 2.
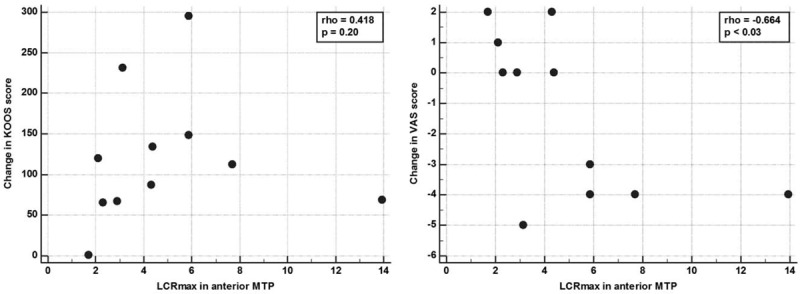
Correlation analysis of the maximum lesion to cortical count ratio (LCRmax) and postoperative symptom improvement. In the anterior medial tibial plateau, LCRmax showed a significant negative correlation with the postoperative change in visual analogue scale. The anterior LCRmax and change in the knee injury and osteoarthritis outcome score showed a positive correlation, although without statistical significance.
Figure 3.
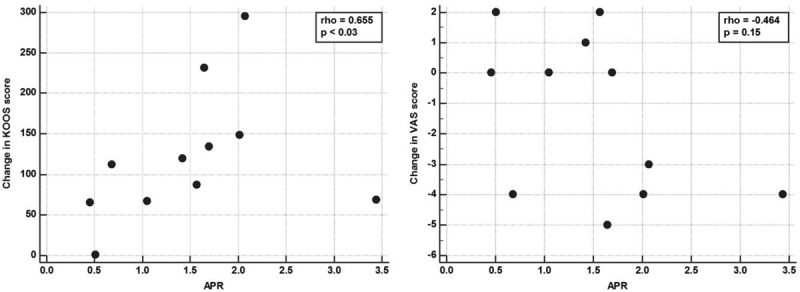
Correlation analysis of the ratio of anterior and posterior medial tibial plateau maximum lesion to cortical count ratio (APR) and postoperative symptom improvement. APR showed a significant correlation with the change in the knee injury and osteoarthritis outcome score (ρ = 0.655, P < .03) but not with the visual analogue scale score.
4. Discussion
The site of joint inflammation associated with bone uptake of radiotracers can be identified and anatomically localized by SPECT/CT, as it provides 3-dimensional localization of the lesion.[16] As the accumulation of radiotracers is associated with osseous metabolism before anatomical changes, we expect that SPECT/CT can demonstrate the early degeneration patterns of osteoarthritis in terms of the degree and anatomical location of mechanical and biochemical stresses.[17] Different patterns of radiotracer uptake were found in our study, and the patients divided on the basis of those patterns showed different clinical outcomes of the MMPRT repair. Despite the limited number of patients, this close association of the uptake pattern with the postoperative outcome not only supports the spatial heterogeneity of the osteoarthritic processes in the knees but also suggests its usefulness in predicting the prognosis using preoperative SPECT/CT.
Our results suggested that bone SPECT/CT could be a sensitive imaging modality for assessing patients with MMPRT, as shown by positive tracer uptake at MTP in 100% of patients, although our study was primarily aimed at predicting the postoperative outcome using SPECT/CT. As mechanical stress causes osseous metabolic changes before causing anatomical changes, SPECT/CT could sensitively demonstrate the functional abnormality with the accurate location. It provides incremental values in the evaluation of knee pain over other radionuclide imaging, such as a planar bone scan or SPECT alone, and now increasingly used in patients who present with knee pain or considered the candidate of arthroplasty.[18]
In this study, a trend of symptom improvement after the MMPRT repair was found when the tracer uptake was dominant in the anterior aspect of MTP. However, the trend of improvement after the repair was not definite in patients who showed a posterior-dominant pattern of uptake on SPECT/CT. Many previous studies have repeatedly shown that a posterior root tear results in the increased peak contact pressure and decreased contact area compared to an intact knee.[1,6,19] These studies have suggested that a meniscus root repair could restore the effect of mechanical stress causing the progression of osteoarthritis to the level of a native knee joint. Notably, since previous biomechanical studies were performed with cadaveric models, the variable uptake patterns identified by SPECT/CT may shed some light on the in vivo consequences of impaired biomechanics caused by a root tear. As part of the study that still needs further investigation, the reason why symptom improvement was seen in a patient with tracer uptake dominance in the anterior aspect of MTP is difficult to explain. A plausible explanation is that the inflammatory process dominant in the posterior aspect of MTP implies irreversible inflammatory or biomechanical change, which may hardly be improved by the repair of MMPRT. These assumptions can be further confirmed by correlating biomechanical studies, structural findings of knee MRI, such as anatomical variability in MM extrusion.[20]
Despite the lack of biomechanical explanation, this study importantly revealed that quantitative parameters derived by SPECT/CT, LCRmax of the anterior MTP and APR, were associated with the improvement in clinical symptom scores after the MMPRT repair. According to our results, the anterior-dominant tracer uptake of MTP in preoperative SPECT/CT could be a positive prognostic factor of the MMPRT repair. Of note, this hardly means the other pattern of uptake is against the operation as the repair of MMPRT should be determined by considering various clinical factors, such as age and initial symptoms.
The study had some limitations. First, the number of subjects was too small to have a strong statistical power because subjective clinical symptom scores largely vary among individuals. Nonetheless, we found a significant correlation between symptom scores and quantitative values derived from SPECT/CT. Second, the clinical factor of whether or not the meniscus healed successfully with surgery was not included in the prediction analysis. Third, the clinical outcomes were obtained from a short-term clinical evaluation; therefore, more long-term outcome data should be studied in the future. Finally, as a retrospective study, postoperative SPECT/CT was not included in the analysis because SPECT/CT was not performed routinely in the postsurgical management. The uptake patterns in postoperative SPECT/CT could provide additional information related to clinical outcome as a future study.
5. Conclusion
Bone SPECT/CT is a sensitive imaging modality for evaluating MMPRT with early osteoarthritis and might have a predictive value for a postoperative outcome of the MMPRT repair. Patients with stronger tracer uptake in the anterior aspect of MTP and relatively lower uptake in the posterior aspect of MTP showed better clinical outcomes after the MMPRT repair. Our results suggest that the preoperative SPECT/CT pattern may be a predictive marker to select appropriate patients who would benefit from the MMPRT repair as an early intervention for osteoarthritis.
Acknowledgments
We thank our colleagues from Seoul National University Hospital, who provided insight and expertise that greatly assisted the research.
Author contributions
HC and HSH designed this study. WW and JYP performed data collection and analysis. JCP, GJC, KWK, and DSL supported the image interpretation and discussion. JYP and HSH performed clinical assessment. All authors interpreted data results, drafted and edited manuscript.
Footnotes
Abbreviations: APR = anterior-posterior MTP counts ratio, CT = computed tomography, KOOS = knee injury and osteoarthritis outcome score, LCRmax = maximum lesion-to-cortical counts ratio, MM = medial meniscus, MMPRT = medial meniscus posterior root tear, MRI = magnetic resonance imaging, MTP = medial tibial plateau, SPECT = single-photon emission computed tomography, VAS = visual analogue scale.
How to cite this article: Whi W, Park JY, Choi H, Paeng JC, Cheon GJ, Kang KW, Lee DS, Han HS. Predicting outcome of repair of medial meniscus posterior root tear with early osteoarthritis using bone single-photon emission computed tomography/computed tomography. Medicine. 2020;99:27(e21047).
WW and J-YP contributed equally to this work.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI19C0339).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Kim JG, Lee YS, Bae TS, et al. Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc 2013;21:2121–5. [DOI] [PubMed] [Google Scholar]
- [2].Papalia R, Vasta S, Franceschi F, et al. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull 2013;106:91–115. [DOI] [PubMed] [Google Scholar]
- [3].Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med 2011;39:1439–43. [DOI] [PubMed] [Google Scholar]
- [4].Sung JH, Ha JK, Lee DW, et al. Meniscal extrusion and spontaneous osteonecrosis with root tear of medial meniscus: comparison with horizontal tear. Arthroscopy 2013;29:726–32. [DOI] [PubMed] [Google Scholar]
- [5].Lerer DB, Umans HR, Hu MX, et al. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol 2004;33:569–74. [DOI] [PubMed] [Google Scholar]
- [6].Allaire R, Muriuki M, Gilbertson L, et al. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 2008;90:1922–31. [DOI] [PubMed] [Google Scholar]
- [7].Bhatia S, LaPrade CM, Ellman MB, et al. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 2014;42:3016–30. [DOI] [PubMed] [Google Scholar]
- [8].Chung HH, Kim JW, Han KH, et al. Prognostic value of metabolic tumor volume measured by FDG-PET/CT in patients with cervical cancer 2011;120:270–4. [DOI] [PubMed] [Google Scholar]
- [9].Lee JH, Lim YJ, Kim KB, et al. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy 2009;25:951–8. [DOI] [PubMed] [Google Scholar]
- [10].Cruz RS, Ferrari MB, Metsavaht L, et al. Understanding posterior meniscal roots lesions: from basic science to treatment. Rev Bras Ortop (Sao Paulo) 2017;52:463–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Moon HK, Koh YG, Kim YC, et al. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med 2012;40:1138–43. [DOI] [PubMed] [Google Scholar]
- [12].Kwak YH, Lee S, Lee MC, et al. Large meniscus extrusion ratio is a poor prognostic factor of conservative treatment for medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc 2018;26:781–6. [DOI] [PubMed] [Google Scholar]
- [13].Hirschmann MT, Konala P, Iranpour F, et al. Clinical value of SPECT/CT for evaluation of patients with painful knees after total knee arthroplasty-a new dimension of diagnostics? BMC Musculoskelet Disord 2011;12.1:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Horger M, Eschmann SM, Pfannenberg C, et al. Added value of SPECT/CT in patients suspected of having bone infection: preliminary results. Arch Orthop Trauma Surg 2007;127:211–21. [DOI] [PubMed] [Google Scholar]
- [15].Johnson DL, Swenson TM, Livesay GA, et al. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy 1995;11:386–94. [DOI] [PubMed] [Google Scholar]
- [16].Lu S-J, Hassan FU, Vijayanathan S, et al. Radionuclide bone SPECT/CT in the evaluation of knee pain: comparing two-phase bone scintigraphy, SPECT and SPECT/CT. Brit J Radiol 2018;91.1090:20180168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Deneweth JM, Newman KE, Sylvia SM, et al. Heterogeneity of tibial plateau cartilage in response to a physiological compressive strain rate. J Orthop Res 2013;31:370–5. [DOI] [PubMed] [Google Scholar]
- [18].De Laroche R, Simon E, Suignard N, et al. Clinical interest of quantitative bone SPECT-CT in the preoperative assessment of knee osteoarthritis. Medicine (Baltimore) 2018;97.35:e11943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].LaPrade CM, Foad A, Smith SD, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med 2015;43:912–20. [DOI] [PubMed] [Google Scholar]
- [20].Guermazi A, Hayashi D, Jarraya M, et al. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: the multicenter osteoarthritis study. Radiology 2013;268:814–21. [DOI] [PMC free article] [PubMed] [Google Scholar]


