Abstract
Introduction:
Although decline in muscle mass and quality and resulting declines in muscle strength are associated with aging, more research is needed in general populations to assess the utility of handgrip strength as an indicator of muscle strength and cardiovascular disease risk.
Methods:
Data from 4,221 participants aged ≥20 years in the 2011–2012 cycle of National Health and Nutrition Examination Survey were analyzed during 2014–2015. Standing isometric relative handgrip strength (calculated as maximal absolute handgrip strength from both hands divided by BMI) was used to predict cardiovascular biomarkers, including blood pressure (measured systolic and diastolic blood pressure); serum lipids (total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglycerides); and plasma insulin and glucose.
Results:
Results from regression analyses showed that higher relative grip strength was significantly associated with lower systolic blood pressure, triglycerides, and plasma insulin and glucose, and higher high-density lipoprotein cholesterol in male and female participants (p<0.05 for all). Secondary descriptive analyses found that absolute handgrip strength increased significantly with increasing weight status, but relative handgrip strength decreased significantly with increasing weight status.
Conclusions:
Results suggest that increased relative handgrip strength may be associated with a better profile of cardiovascular health biomarkers among U.S. adults. Relative grip strength, which both adjusts for the confounding of mass and assesses concomitant health risks of increased body size and low muscle strength, may be a useful public health measure of muscle strength.
Introduction
Handgrip strength has shown prognostic utility in the assessment of a number of healthy aging and chronic disease outcomes in older adults. Specifically, studies have supported associations of grip strength with frailty,1 physical activity,2 diabetes,3 functional limitations,4 nutritional status,5 metabolic syndrome,6 and mortality.7,8 Grip strength may be important to examine in all adults given its relation with overall muscular strength and fitness.5 That is, when performed in a standing position, grip strength also captures lower body and core muscle strength used in balance and exertion of force. By contrast, grip strength performed in a seated position targets relatively smaller muscle groups and is more localized to the upper body. Although decline in muscle mass and quality and resulting declines in muscle strength are associated with aging,9 more research is needed in general populations to assess the utility of grip strength as an indicator of muscle strength and chronic disease development such as cardiovascular disease.
Previous research2,6,10 in older adults has shown that grip strength is associated with physiologic and clinical cardiovascular biomarkers. A study6 of adults aged 59–73 years showed that grip strength was associated with individual markers and summary definitions of metabolic syndrome. This study and others2,3,10 document a link between impaired muscle strength and cardiovascular disease risk factors in older adults; however, few studies have examined this in a general adult population. One recent study11 of more than 139,000 adults aged 35–79 years supported grip strength as a prognostic tool for all-cause death, cardiovascular death, and cardiovascular disease but did not include U.S. adults. In participants aged 15–69 years, one study12 showed equivocal patterns in mean differences across grip strength normative categories and a number of cardiovascular health indicators. These studies12–14 indicate that one difficulty with understanding the associations between grip strength and cardiovascular health is the confounding of body size. Relative grip strength (absolute strength corrected for a measure of body size such as BMI) has been recommended to address both the confounding of strength by body mass and concomitant health risks of increased body weight and low muscular strength.15 Relative grip strength is comparable to laboratory-based approaches16 and may increase the translational value of grip strength as a prognostic tool.
The purpose of the current study was to examine associations of grip strength with biomarkers of cardiovascular disease risk, including blood pressure, serum lipids, and plasma insulin and glucose, in U.S. adults in 2011–2012. A secondary aim was to compare differences in absolute and relative grip strength by weight status in U.S. adults.
Methods
Data from National Health and Nutrition Examination Survey (NHANES) 2011–2012 were used. The survey uses a complex sampling design to produce a nationally representative sample of the U.S. civilian non-institutionalized population. This cycle included oversampling of subgroups, including some racial/ethnic minorities (Hispanic, non-Hispanic black, and non-Hispanic Asian); non-Hispanic white people aged ≥80 years; and low-income non-Hispanic white people. The survey includes an in-person home interview. Examination data, including physiologic, laboratory, and anthropometric measures, are collected during a separate visit to a Mobile Examination Center. The National Center for Health Statistics Research Ethics Review Board approved the protocol, and informed consent was obtained for all adult participants. The overall survey examination response rate for 2011–2012 Was 69.5%. Additional National Health and Nutrition Examination Survey details are available elsewhere.17
For this analysis, non-pregnant participants aged ≥20 years who visited the Mobile Examination Center were considered eligible (N=5,291). Participants missing grip strength data (primarily because of coming late/leaving early/lack of time) were excluded from analyses (n=650). The fasting subsample was used for fasting laboratory analyses (n=2,053). Each participant was randomly assigned to either a morning or an afternoon/evening Mobile Examination Center exam session. Morning session participants were instructed to fast overnight. Participants missing data on covariates and any non-fasting (n=420) or fasting (n=130) biomarker outcomes were excluded, leaving a final sample size of 4,221 and a final fasting subsample size of 1,923. Unweighted sample sizes by sex, age, and race/Hispanic origin are shown in Table 1.
Table 1.
Unweighted Sample Sizes by Sex, Age, and Race/Hispanic Origin: U.S., 2011–2012
| Characteristic | Males | Females | Fasting subsample males | Fasting subsample females |
|---|---|---|---|---|
| Whole sample | 2,158 | 2,063 | 983 | 940 |
| Age (years) | ||||
| 20–29 | 410 | 358 | 185 | 157 |
| 30–39 | 392 | 337 | 178 | 165 |
| 40–49 | 353 | 355 | 159 | 165 |
| 50–59 | 339 | 362 | 159 | 160 |
| ≥60 | 664 | 651 | 302 | 293 |
| Race/Hispanic origin | ||||
| Non-Hispanic white | 841 | 788 | 393 | 372 |
| Non-Hispanic black | 533 | 556 | 199 | 239 |
| Non-Hispanic Asian | 289 | 275 | 153 | 129 |
| Hispanic | 421 | 395 | 210 | 177 |
Source: National Health and Nutrition Examination Survey, 2011–2012.
Note: Analytic sample includes non-pregnant individuals aged 20 years or older. Individuals missing data on grip strength, covariates, or biomarkers were excluded. Fasting subsample includes subset of individuals with fasting laboratory results. The whole sample includes race/ethnicity groups not shown separately.
Measures
Anthropometric measures (height, weight, waist circumference) were collected using standardized protocols. BMI was calculated as weight in kilograms divided by height in meters squared rounded to one decimal place. Weight status was defined as normal weight/underweight (BMI<25); overweight (30<BMI≥25); and obese (BMI≥30).
Isometric handgrip strength was measured using a hand-held Takei dynamometer (Model T.K.K.5401) in a standing position with the arm extended straight down to the side unless the participant was physically limited. After completing a practice trial in one hand, each hand was tested three times, alternating hands between trials with 60-second rests between measurements on the same hand. Participants were randomly assigned to begin trials with their dominant or non-dominant hand and were excluded if they reported hand or wrist surgery in the preceding 3 months or were unable to hold the dynamometer with either hand (e.g., paralyzed in both hands, missing limbs). Absolute grip strength was calculated as the sum of the largest reading from each hand and expressed in kilograms. Relative grip strength was calculated as absolute grip strength divided by BMI. Previous work15,16 supported strength corrected for BMI over other relative strength measures. To aid in cross-study comparisons, both absolute and relative grip strength were presented.
Biomarker outcomes included systolic blood pressure, diastolic blood pressure, total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides, plasma glucose, and plasma insulin.17 Blood pressure was averaged from up to three measures (or four measures if an interrupted/incomplete measure was made). A fasting subsample was used to measure LDL cholesterol, triglycerides, plasma glucose, and plasma insulin. All other biomarkers were tested using the full sample. Biomarkers were analyzed as continuous outcomes in order to facilitate clinical interpretation of effect sizes associated with grip strength. The current study defined “more-favorable” cardiometabolic outcomes to mean lower systolic and diastolic blood pressure, lower fasting insulin and glucose, lower total and LDL cholesterol, and higher HDL cholesterol.
Covariates used in all models included age (years), race/Hispanic origin, self-reported statin use, and physical activity. Race/Hispanic origin was categorized as: non-Hispanic white, non-Hispanic black, non-Hispanic Asian, Hispanic (regardless of race), and other (including all non-Hispanic individuals reporting more than one race). Those in the “other” group were included in calculations of the total population but were not reported separately. Research18 has shown that a side effect of statin use may be muscle pain or weakness. Participants reported whether their doctor had prescribed statin medication for the treatment of high cholesterol and if they were currently taking the medication (coded yes if currently taking, no otherwise). Physical activity was measured based on the Global Physical Activity Questionnaire.19 Time spent in moderate-intensity and vigorous-intensity work and leisure activities were summed for each day, averaged across the participants’ reported days per week of engaging in the activities, and divided by ten, providing one measure of average 10-minute bouts of moderate to vigorous physical activity per day.
Previous studies have included anthropometric variables as covariates with absolute strength12,20,21 or used relative strength.15,22 Therefore, secondary analyses with absolute strength included BMI as a covariate. Alternative anthropometric covariates in the absolute strength analyses were also considered, including height, weight, and waist circumference (correlations with absolute strength were 0.73, 0.42, and 0.17, respectively, p<0.001 for all). The choice of anthropometric covariate made little difference in the outcomes, so only results with BMI (correlation with absolute strength, 0.08; p<0.001) are presented. Self-reported use of doctor-prescribed blood pressure medication (for blood pressure outcomes only) was initially included as a covariate. Results with and without inclusion of this covariate were similar, and only results without this covariate are presented. Sensitivity analyses excluding individuals reported to be on blood pressure or statin medications were similar to those presented.
Statistical Analysis
All analyses were conducted using the Survey package in R, version 3.0.3. Fasting subsample weights were used for analyses of LDL cholesterol, triglycerides, and plasma glucose and insulin. SEs were estimated using Taylor series linearization. Multiple linear regression analyses were used to test the relations of grip strength and covariates regressed on individual biomarker outcomes. Analyses were stratified by sex owing to large differences in men and women’s strength values. Analyses stratified by age (>40 years, <40 years) and sex were generally consistent with those presented and are therefore not shown. Statistical significance was set at p<0.05 using a two-tailed t-statistic. Descriptive means and SEs for absolute and relative grip strength were calculated by weight status within sex and age groups. Linear trends were examined using contrasts of normal and obese weight status categories with a t-statistic.
Results
Sample participants were aged 47.5 (SE=0.82) years, and 18.3% reported taking statin medications. Unadjusted mean values and SEs for biomarker outcomes, grip strength, physical activity, and BMI are shown by sex in Table 2. Absolute grip strength ranged from 11.4 to 169.6 kg (interquartile range [IQR]=78.2, 101.2 kg) in men and 12.5 to 104.4 kg (IQR=48.6, 63.1 kg) in women. Relative grip strength ranged from 2.7 to 3.7 kg/BMI (IQR=0.69, 6.4 kg/BMI) in men and 1.6 to 2.4 kg/BMI (IQR=0.4, 4.6 kg/BMI) in women. Results showed men and women differed significantly on mean values of grip strength, physical activity, blood pressure, total cholesterol, HDL cholesterol, and glucose. Results from linear regressions are shown in Table 3. In both male and female participants, higher relative grip strength was significantly associated with more favorable systolic blood pressure, HDL cholesterol, triglycerides, and plasma insulin and glucose. In men, relative grip strength was positively associated with LDL. Secondary analyses assessing absolute strength and including BMI as a covariate are shown in Appendix Table 1 (available online). When including BMI as a covariate, some significant adverse associations (higher absolute grip strength associated with higher diastolic BP and some lipids) between absolute grip strength and biomarker outcomes were observed, including diastolic blood pressure in men and women and total cholesterol and LDL in men only. These significant adverse associations remained regardless of the anthropometric covariate that was included or when no anthropometric covariate was included with absolute strength (data not shown). Secondary analyses defining relative strength as absolute strength divided by waist circumference and using absolute strength with waist circumference as a covariate showed results similar to those using BMI (data not shown).
Table 2.
Mean Biomarker Values by Sex in U.S. Adults Aged 20 Years and Older, 2011–2012
| Characteristic | Males, M (SE) | Females, M (SE) |
|---|---|---|
| BMIa | 28.7 (0.3) | 28.9 (0.3) |
| Height (cm)a | 176.2 (0.38) | 162.5 (0.41) |
| Weight (kg)a | 89.41 (0.76) | 76.04 (0.96) |
| Absolute grip (kg)a | 89.7 (0.8) | 56.1 (0.5) |
| Relative grip (kg/BMI)a | 3.2 (0.05) | 2.0 (0.02) |
| MVPA 10-minute boutsa | 10.55 (0.66) | 5.58 (0.29) |
| Systolic BP (mm Hg)a | 123.1 (0.6) | 120.4 (0.8) |
| Diastolic BP (mm Hg)a | 72.7 (0.6) | 70.6 (0.7) |
| Total cholesterol (mgdL−1)a | 191.5 (1.3) | 199.2 (1.4) |
| HDL cholesterol (mg dL−1)a | 47.8 (0.5) | 57.8 (0.7) |
| LDL cholesterol (mg dL−1)b | 114.0 (1.4) | 117.2 (1.3) |
| Triglycerides (mg dL−1)b,c | 115.5 (3.3) | 100.9 (3.0) |
| Plasma insulin (μU mL−1)b | 13.5 (0.7) | 12.7 (0.5) |
| Plasma glucose (mg dL−1)b | 106.0 (1.1) | 103.1 (1.3) |
Source: National Health and Nutrition Examination Survey, 2011–2012.
Note: Boldface indicates significant sex difference (p<0.05).
Calculated using examination sample (n=4,221).
Calculated using subsample with fasting data and corresponding fasting weights (n=1,923).
Calculated using geometric mean and variance.
BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; MVPA, moderate-to-vigorous physical activity.
Table 3.
Results of Multiple Linear Regression of Relative Handgrip Strength (Strength/BMI) on Biomarker Outcomes in U.S. Adults, 2011–2012
| Males | Females | |||||
|---|---|---|---|---|---|---|
| Characteristic | Estimate (SE) | B | t | Estimate (SE) | B | t |
| Systolic BP (mm Hg)a | −1.48 (0.53) | −0.08 | −2.77* | −3.16 (0.95) | −0.10 | −3.34* |
| Diastolic BP (mm Hg)a | −0.79 (0.43) | −0.05 | −1.84 | −0.05 (0.57) | −0.01 | −0.09 |
| Total cholesterol (mg dL−1)a | 0.70 (1.08) | 0.01 | 0.65 | 0.47 (1.97) | 0.01 | 0.24 |
| HDL cholesterol (mg dL−1)a | 4.06 (0.48) | 0.26 | 8.41** | 9.28 (1.31) | 0.34 | 7.07** |
| LDL cholesterol (mg dL−1)b | 3.29 (1.34) | 0.09 | 2.46* | −5.32 (3.38) | −0.14 | −1.58 |
| Triglycerides (mg dL−1)b | −13.58 (5.18) | −0.19 | −2.62* | −32.28 (6.84) | −0.44 | −4.72** |
| Plasma insulin (μU.mL−1)b | −5.77 (1.32) | −0.35 | −4.36** | −8.37 (1.03) | −0.51 | −8.16** |
| Plasma glucose (mg dL−1)b | −6.72 (1.75) | −0.23 | −3.84** | −9.31 (1.43) | −0.32 | −6.49** |
Source: National Health and Nutrition Examination Survey, 2011–2012.
Note: All models control for race/Hispanic origin, age, statin medication use, and physical activity. Absolute grip strength values were divided by BMI to create relative handgrip strength. Boldface indicates statistical significance
p<0.05;
p<0.01.
Weighted mean and variance estimates were used in creation of standardized coefficients.
Calculated using examination sample (n=4,221).
Calculated using subsample with fasting data and corresponding fasting weights (n=1,923).
BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Mean values of absolute and relative grip strength by weight status within sex and age groups are shown in Figure 1 and Appendix Table 2 (available online). Results showed differences in the patterns of absolute versus relative strength by weight status. Absolute strength increased significantly with increasing weight (linear trend tests, p<0.05 for all except women aged 40–49 and 50–59 years), whereas relative strength decreased significantly with increasing weight (linear trend tests, p<0.05 for all).
Figure 1.
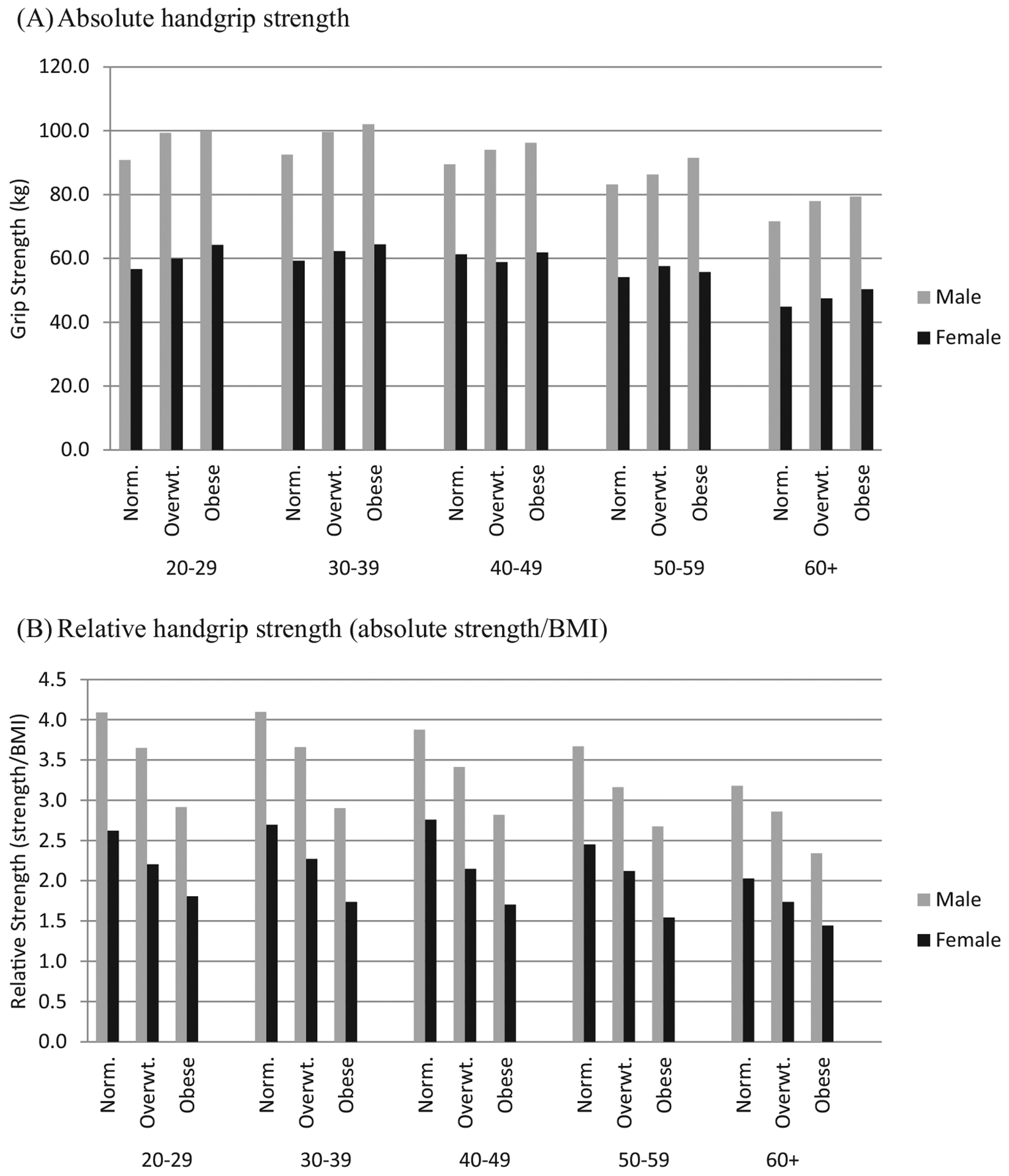
Mean values of absolute grip strength (kg) versus relative grip strength (strength/BMI) by weight status within sex and age groups in U.S. adults, 2011–2012.
Source: National Health and Nutrition Examination Survey, 2011–2012.
Note: Significant positive linear trends observed (p<0.05 for all) in absolute strength by weight status in all sex and age groups except women in the 40–49- and 50–59-year age groups. Significant negative linear trends observed (p<0.05 for all) in relative strength by weight status in all sex and age groups. Norm, normal; overwt, overweight.
Discussion
The current study examined associations between relative handgrip strength and cardiovascular health biomarkers in a nationally representative sample of U.S. adults, with two key findings.
First, the current study found significant associations between higher relative muscular strength and more-favorable cardiovascular disease biomarkers, including systolic blood pressure, HDL cholesterol, triglycerides, and plasma insulin and glucose in men and women. These findings are in line with physiologic research on functional and metabolic benefits of muscle strength, including potential causal pathways,23 and are consistent with studies in older adults.2,6,10,24 However, these findings are inconsistent with three studies that included younger adults and showed some counterintuitive associations of grip strength (absolute) with poorer lipids,12,21 higher blood pressure, and increased waist circumference,12 and no correlation with glycated hemoglobin.3,12,21Another study22 using relative strength showed the expected beneficial association with lower metabolic syndrome prevalence. The current study’s findings expand on research on resistance training and blood lipids,25 insulin action,26 and cardiovascular health27 by including a nationally representative sample and using relative grip strength as a feasible measure of muscular strength.
One explanation for contradictory findings among previous studies may be the use of absolute versus relative strength. Some health outcomes may be more strongly associated with a relative measure that concomitantly assesses excess weight and poor strength, which are distinct although related health risks. Previous research15 on mobility demonstrated a synergistic association using relative strength compared with examining strength and BMI independently. The use of BMI and absolute strength measures as two variables in the same model would aim to capture independent contributions of body composition and strength. However, previous studies15,22 and the current study support the utility of a joint measure of strength and weight status, such as relative strength, to examine associations with cardiometabolic health and aging. That is, rather than holding constant an independent effect of weight status, strength relative to weight status may be conceptualized as an assessment of concomitant health risks.
Next, and contrary to the study’s main findings, secondary analyses that assessed absolute strength and included BMI as a covariate showed significant counterintuitive relationships, with some cardiovascular biomarkers and null associations with others. Though the sex difference found between grip strength and LDL cholesterol may be related to the fact that testosterone is linked to both lipid levels and muscle tissue,28 differences in covariates may explain differences in the literature. Controversy exists regarding the most appropriate controls for body mass when assessing strength,13,14 and studies12,20,21 have traditionally assessed a variety of covariates and analytic strategies. Covariates have included waist circumference,12,20 BMI,20,21 obesity history,13 unadjusted body weight,13,21 height,2,20 sum of seven skinfolds,21 and skeletal muscle mass from dual-energy x-ray absorption.2 Some14 have argued that two highly correlated independent variables (e.g., weight and obesity history) statistically induce inverse associations with strength and confuse parameter interpretation. Others13 have indicated that muscle strength only makes sense when body size is taken into account, and additional risk factors or confounders may be important. Absolute strength has been shown in some cases, but not all,2,29 to be positively associated with BMI and adversely associated with some cardiovascular disease risk factors.12,20,21,30 The direct relation between mass and force (force = mass × acceleration) and the positive association between fat mass and muscle mass limit the prognostic utility of absolute grip strength. Use of relative strength or more sophisticated modeling techniques may be appropriate in some cases.6,15
Some researchers12,23 have suggested that qualitative weakness is the primary concern when assessing strength, and a threshold effect of sufficient muscle strength could be assessed with the use of normative categories. However, previous research12 suggests that normative categories for grip strength, regardless of body size covariate choice, may not be adequately addressing the issue of body size when assessing cardiovascular health. Adequate treatment of body size and consideration of relative strength may improve the prognostic utility of handgrip strength.
Limitations
Strengths of the current study include the recent data from a nationally representative sample, investigation of a number of key cardiovascular biomarkers, and comparison of absolute strength to relative grip strength (a measure of muscle strength corrected for weight status). Limitations include the use of handgrip strength as the sole indicator of muscular strength, the smaller sample used in fasting outcomes, the lack of a direct adiposity measure, and the cross-sectional design.
Conclusions
The current study shows that relative handgrip strength is significantly associated with some more-favorable cardiovascular health biomarkers. Furthermore, the differences in results across absolute and relative strength measures support the utility of relative grip strength to simultaneously assess for health risks of increased body mass and low muscle strength. Relative grip strength may be a feasible measure to use in future muscle strength and body composition research given it is relatively simple, quick, reliable, and inexpensive to use. More research in the general population may be needed to disentangle the relations among body size; muscular strength, function, and quality; and meaningful cardiovascular health outcomes.
Supplementary Material
Footnotes
The findings and conclusions in this article are those of the authors and not necessarily those of CDC.
No financial disclosures were reported by the authors of this paper.
References
- 1.Purser JL, Kuchibhatla MN, Fillenbaum GG, Harding T, Peterson ED, Alexander KP. Identifying frailty in hospitalized older adults with significant coronary artery disease. J Am Geriatr Soc. 2006;54(11): 1674–1681. 10.1111/j.1532-5415.2006.00914.x. [DOI] [PubMed] [Google Scholar]
- 2.Rolland Y, Lauwers-Cances V, Pahor M, Fillaux J, Grandjean H, Vellas B. Muscle strength in obese elderly women: effect of recreational physical activity in a cross-sectional study. Am J Clin Nutr. 2004;79(4): 552–557. [DOI] [PubMed] [Google Scholar]
- 3.Cetinus E, Buyukbese MA, Uzel M, Ekerbicer H, Karaoguz A. Hand grip strength in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2005;70(3):278–286. 10.1016/j.diabres.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 4.Kuh D, Bassey EJ, Butterworth S, Hardy R, Wadsworth ME. Grip strength, postural control, and functional leg power in a representative cohort of British men and women: associations with physical activity, health status, and socioeconomic conditions. J Gerontol A Biol Sci Med Sci. 2005;60(2):224–231. 10.1093/gerona/60.2.224. [DOI] [PubMed] [Google Scholar]
- 5.Norman K, Stobaus N, Gonzalez MC, Schulzke JD, Pirlich M. Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr. 2011;30(2):135–142. 10.1016/j.clnu.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Sayer AA, Syddall HE, Dennison EM, et al. Grip strength and the metabolic syndrome: findings from the Hertfordshire Cohort Study. QJM. 2007;100(11):707–713. 10.1093/qjmed/hcm095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruiz JR, Sui X, Lobelo F, et al. Association between muscular strength and mortality in men: prospective cohort study. BMJ. 2008;337:a439 10.1136/bmj.a439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Izawa KP, Watanabe S, Osada N, et al. Handgrip strength as a predictor of prognosis in Japanese patients with congestive heart failure. Eur J Cardiovasc Prev Rehabil. 2009;16(1):21–27. 10.1097/HJR.0b013e32831269a3. [DOI] [PubMed] [Google Scholar]
- 9.Rantanen T, Avlund K, Suominen H, Schroll M, Frandin K, Pertti E. Muscle strength as a predictor of onset of ADL dependence in people aged 75 years. Aging Clin Exp Res. 2002;14(3 suppl):10–15. [PubMed] [Google Scholar]
- 10.Stenholm S, Sallinen J, Koster A, et al. Association between obesity history and hand grip strength in older adults—exploring the roles of infiammation and insulin resistance as mediating factors. J Gerontol A Biol Sci Med Sci. 2011;66(3):341–348. 10.1093/gerona/glq226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leong DP, Teo KK, Rangarajan S, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015;386(9990):266–273. 10.1016/S0140-6736(14)62000-6. [DOI] [PubMed] [Google Scholar]
- 12.Fowles J, Roy J, Clarke J, Dogra S. Are the fittest Canadian adults the healthiest? Health Rep. 2014;25(5):13–18. [PubMed] [Google Scholar]
- 13.Stenholm S, Koster A, Rantanen T. Response to the letter “Overadjustment in regression analyses: considerations when evaluating relationships between body mass index, muscle strength, and body size”. J Gerontol A Biol Sci Med Sci. 2014;69(5):618–619. 10.1093/gerona/glt194. [DOI] [PubMed] [Google Scholar]
- 14.Keevil VL, Khaw K-T. Overadjustment in regression analyses: considerations when evaluating relationships between body mass index, muscle strength, and body size. J Gerontol A Biol Sci Med Sci. 2014; 69(5):616–617. 10.1093/gerona/glt186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choquette S, Bouchard D, Doyon C, Sénéchal M, Brochu M, Dionne IJ. Relative strength as a determinant of mobility in elders 67–84 years of age. A NuAge study: nutrition as a determinant of successful aging. J Nutr Health Aging. 2010;14(3):190–195. 10.1007/s12603-010-0047-4. [DOI] [PubMed] [Google Scholar]
- 16.Straight C, Brady A, Schmidt M, Evans E. Comparison of laboratory and field-based estimates of muscle quality for predicting physical function in older women. J Aging Res Clin Pract. 2013;2:276–279. [Google Scholar]
- 17.CDC. National Health and Nutrition Examination Surveys: NHANES 2011–2012. wwwn.cdc.gov/nchs/nhanes/search/nhanes11_12.aspx. Pubilished 2012. Accessed December 15, 2014.
- 18.Thompson PD, Clarkson PM, Rosenson RS. An assessment of statin safety by muscle experts. Am J Cardiol. 2006;97(8):S69–S76. 10.1016/j.amjcard.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 19.Armstrong T, Bull F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ). J Public Health. 2006;14(2):66–70. 10.1007/s10389-006-0024-x. [DOI] [Google Scholar]
- 20.Hardy R, Cooper R, Sayer AA, et al. Body mass index, muscle strength and physical performance in older adults from eight cohort studies: the HALCyon programme. PLoS One. 2013;8(2):e56483 10.1371/journal.pone.0056483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kohl HWI, Gordon N, Scott C, Baandrager H, Blair SN. Musculoskeletal strength and serum lipid levels in men and women. Med Sci Sports Exerc. 1992;24(10):1080–1087. 10.1249/00005768-199210000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Jurca R, Lamonte MJ, Church TS, et al. Associations of muscle strength and fitness with metabolic syndrome in men. Med Sci Sports Exerc. 2004;36(8):1301–1307. 10.1249/01.MSS.0000135780.88930.A9. [DOI] [PubMed] [Google Scholar]
- 23.Wolfe R The underappreciated role of muscle in health and disease. Am J Clin Nutr. 2006;84(3):475–482. [DOI] [PubMed] [Google Scholar]
- 24.Izawa KP, Watanabe S, Oka K, et al. Upper and lower extremity muscle strength levels associated with an exercise capacity of 5 metabolic equivalents in male patients with heart failure. J Cardiopulm Rehabil Prev. 2012;32(2):85–91. 10.1097/HCR.0bi013e31824bid886. [DOI] [PubMed] [Google Scholar]
- 25.Tambalis KD, Panagiotakos DB, Kavouras SA, Sidossis LS. Responses of blood lipids to aerobic, resistance, and combined aerobic with resistance exercise training: a systematic review of current evidence. Angiology. 2009;60(5):614–632. [DOI] [PubMed] [Google Scholar]
- 26.Borghouts L, Keizer H. Exercise and insulin sensitivity: a review. Int J Sports Med. 2000;21(01):1–12. 10.1055/s-2000-8847. [DOI] [PubMed] [Google Scholar]
- 27.Williams MA, Haskell WL, Ades PA, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update; a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116(5):572–584. 10.1161/CIRCULATIONAHA.107.185214. [DOI] [PubMed] [Google Scholar]
- 28.Mendelsohn ME, Rosano GM. Hormonal regulation of normal vascular tone in males. Circ Res. 2003;93(12):1142–1145. 10.1161/01.RES.0000108694.68635.1C. [DOI] [PubMed] [Google Scholar]
- 29.Ruiz JR, Sui X, Lobelo F, et al. Muscular strength and adiposity as predictors of adulthood cancer mortality in men. Cancer Epidemiol Biomarkers Prev. 2009;18(5):1468–1476. 10.1158/1055-9965.EPI-08-1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Budziareck M, Duarte R, Barbosa-Silva M. Reference values and determinants for handgrip strength in healthy subjects. Clin Nutr. 2008;27:357–362. 10.1016/j.clnu.2008.03.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


