Abstract
Purpose
This study compared riboflavin penetration in porcine corneas using two different solutions: dextran and hydroxypropyl methylcellulose (HPMC).
Methods
Porcine corneas were de-swollen and after prepared in an artificial anterior chamber with balanced saline solution. The pressure was checked with a portable tonometer. We used 0.1% riboflavin in 20% dextran for 30 min or 0.1% riboflavin in 1% HPMC for 10 min. The fluorescence intensity in multiphoton microscopy was used to evaluate concentration into the cornea, and ultrasonic pachymetry was performed before and after using riboflavin.
Results
Riboflavin concentration up to 340 μm was higher in the HPMC group (p 0.146). From 340 microns to 500 μm, the concentration was higher in the dextran group (p 0.248). There was no statistically significant difference between the groups when considering all the corneal thickness studied (p 0.528). Pachymetric measurements in the group with dextran showed a 12.9% corneal thickness decrease after 30 min, while the HPMC group showed a 9.1% increase after 10 min.
Conclusion
We concluded that 1% HPMC riboflavin for 10 min had the same level of safety when compared to the Dresden protocol with dextran riboflavin for 30 min. Ultrasonic pachymetry during corneal crosslinking has fundamental importance in controlling corneal hydration due to changes in thickness caused by different types of riboflavin. This study used different methods than previous studies to better simulate corneal physiological conditions and used 1% HPMC concentration which differs from previous studies performed with 1.1% HPMC.
Keywords: crosslinking, fluorescence, riboflavin
Introduction
Corneal collagen crosslinking is used to treat the progression of corneal ectasia diseases (e.g., keratoconus, pellucid marginal degeneration, and keratoglobus, and after refractive surgery), infections, and corneal edema.1 Crosslinking consists of forming bonds between polymer chains to produce a more rigid three-dimensional structure. Corneal polymeric crosslinking occurs in the presence of UVA (370 nm) radiation, and riboflavin, which acts as a photoinducer of the reaction.2 The minimum pachymetry for the procedure is 400 µm,3–5 which allows an acceptable level of safety when considering the wavelength and the time of UVA exposure. Seiler et al6 reported an experimental study of pig eye corneas in 1997, marking the beginning of corneal crosslinking. Since that study, some technical variations have resulted in greater safety and effectiveness of the procedure, whose primary objective of corneal crosslinking is to inhibit the progression of corneal ectasias.6–9
The first clinical study using corneal ectasia (Dresden protocol) was published in 2003 by Wollensak et al.10 It showed that crosslinking of corneal collagen was an effective procedure to stop the progression of keratoconus. The Dresden protocol use of 0.1% riboflavin in 20% dextran in de-epithelialized corneas for 30 min, with irradiation with UVA (370 nm) at 3 mW/cm2 for 30 min, for a total dose of 5.4 J/cm2. The results are effective in stopping the progression of corneal ectasias. Most studies and current knowledge of corneal crosslinking involve this protocol.
Riboflavin (vitamin B2) is a photosensitive agent that produces free radicals in the presence of light and oxygen. Free radicals (reactive oxygen species) induce covalent bonds between collagen fibers and/or proteoglycans. Another essential function of riboflavin in this procedure is its use as a filter, protecting structures such as crystalline lens, the retina, and the corneal endothelium. Riboflavin penetration is therefore a key step in corneal protection during this procedure.
Many studies have been performed to reduce the total time of crosslinking. Based on the Bunsen-Roscoe law (the same amount of total energy at different times and irradiation intensities), it is possible to accelerate the crosslinking process.11 Recent studies have determined a shorter procedure time, using different riboflavin solutions requiring less time to penetrate the cornea.
Refinements of the technique have resulted in different types of riboflavin, facilitating new protocols for the crosslinking procedure. However, a better understanding of the behavior of each type of riboflavin in corneal tissue is essential to increase safety. Riboflavin penetration in different solutions can affect the safety and saturation time before the application of radiation because it can affect the thickness of the cornea.
Two-photon fluorescence microscopy (TPF) makes it possible to evaluate riboflavin penetration in the cornea.12–14 It is a nonlinear optical microscopy technique, which uses a near-infrared femtosecond pulsed source. It can be used for fluorescence imaging (autofluorescence of tissues, cells expressing fluorescent proteins, or with exogenous contrast agents) and for imaging using a high order spreading phenomenon known as Second Harmonic Generation.
In the present study, porcine corneas were evaluated with multiphoton microscopy after the application of two different types of riboflavin solutions: dextran and hydroxypropyl methylcellulose (HPMC). To compare the riboflavin penetration in different solutions (dextran and HPMC) in porcine corneas, this study used multiphoton microscopy to improve the assessment of corneal soaking in crosslinking.
Materials and Methods
The research started with the approval of the Animal Use Ethics Committee of the University of São Paulo, Medical School, São Paulo, Brazil, which approved the proper and ethical use of laboratory animals using the guidelines of the National Center for the Replacement, Refinement and Reduction of Animals in Research (NC3Rs).
Two groups were created with 10 porcine corneas in each group. The test was performed within 10 h of pig eye enucleation to improve corneal conditions. The corneoscleral discs were prepared in an artificial anterior chamber13 (Barron Precision Instruments, Grand Blanc, MI, USA). An 8-mm area was marked with a corneal trephine and corneal de-epithelialization was performed with a number 15 scalpel blade. The dextran group had the corneas de-swollen with Dextran T 500 20% (T500 Sigma-Aldrich, St. Louis, MO, USA) applied inside the anterior chamber and in a reservoir on the cornea. Ultrasonic pachymetry (SP-100 Tomey, Nagoya, Japan) was performed after assembly and de-epithelialization, until corneal thickness stability was achieved (the maximum allowable variation was 5% in 3 consecutive measurements every 5 minutes). HPMC group underwent the same steps but the de-swollen was made with 1% HPMC (Dow Portugal Chemicals, Estarreja, Portugal) solution. After the de-swollen, the artificial chamber was filled with balanced saline solution (BSS) inside the artificial chamber.
The pressure was measured using a portable tonometer (Icare TA01i Finland Oy, Vantaa, Finland). Only cases with pressures throughout the procedure between 10‒21 mmHg were included in the study.
Riboflavin monophosphate (0.1%) in 20% dextran and 0.1% riboflavin monophosphate in 1% HPMC were used the following protocols: riboflavin drops (according to the test group) were instilled every 3 min. Soaking time was 30 min in the dextran group and 10 min in the HPMC group. During soaking the reservoir was not used on the cornea. Pachymetry was also performed after the total time of riboflavin application.
TPF were captured using a 20x objective lens by a multi-photon microscope (LSM 780 microscope; Zeiss, Oberkochen, Germany) which operates pulsed infrared laser light generating images through the excitation of photons. Each image was recorded on z-stacks ranging from 20 μm over a depth of 500 μm with image area 425.10 x 425.10 μm.
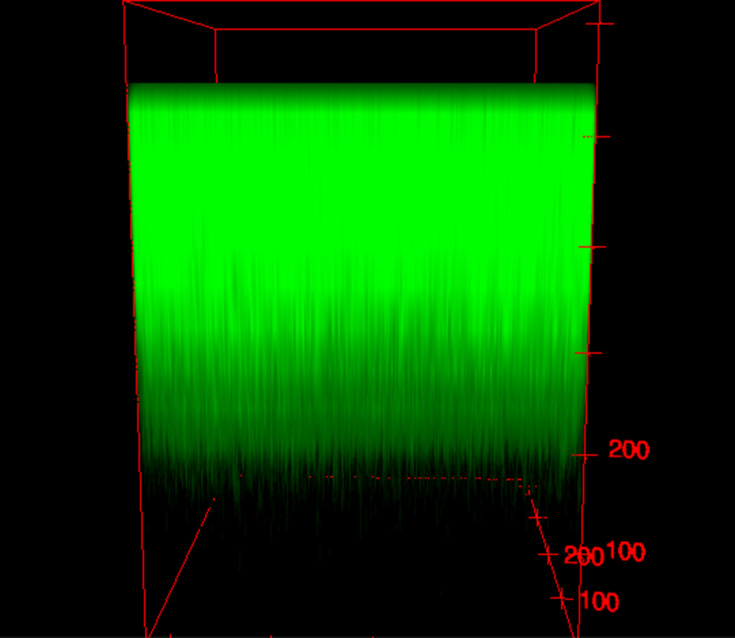
Multiphoton microscopy has the advantage of third-dimensional image capture and enables better sample analysis. Laser emission was set to 900 nm to avoid cornea second harmonic generation. The images were captured before riboflavin use to calibrate the baseline values, after 10 min in the HPMC group and 30 min in the dextran group and after 2 hours in each group to determine the value of the saturated corneas. The riboflavin film on the top of the cornea was removed with Merocel sponge before images were obtained. Riboflavin penetration was evaluated by the fluorescence intensity (FI) detected by the multiphoton microscope (Figure 1).
Figure 1.
Corneal 3D image after soaking. Multiphoton microscopy processing with Fiji image package. Fluorescence intensity is characterized by the green color. The riboflavin decreased with increasing corneal depth.
The riboflavin concentration was determined by dividing FI in each group by the saturated corneal values of the correspondent group and multiplied by the riboflavin concentration (0.1%). The saturation process is very important to correct absorption and scattering data because fluorescence undergoes scattering and interference by extracellular matrix, keratocytes and by riboflavin itself.13
Numerical data were extracted from the images using the Fiji image processing package (https://fiji.sc/).
Statistical analysis was performed using the Mann–Whitney test with statistical package IBM SPSS (Statistical Package for Social Sciences). A value of P < 0.05 was considered statistically significant.
Results
Figure 2 shows FI in the HPMC group for 10 minutes and after corneal saturation. In both curves, the riboflavin concentration decreased with increasing corneal depths and increased riboflavin penetration with increasing time. FI was defined as “1” arbitrary unit (au).
Figure 2.
FI in the HPMC group for 10 minutes and after corneal saturation.
Figure 3 presents the Dextran group results by multiphoton microscopy performed at 30 minutes and two hours (saturated). The curves' behavior is similar to that presented in the HPMC group.
Figure 3.
FI in the dextran group for 30 minutes and after corneal saturation.
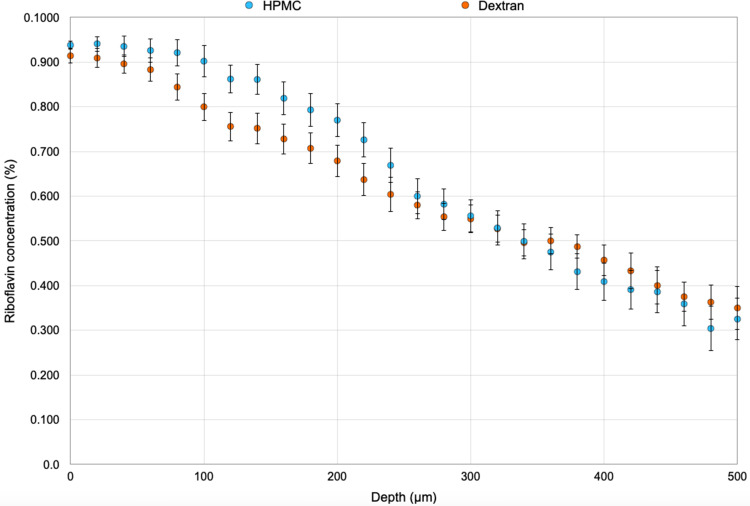
Figure 4 shows riboflavin concentration in the cornea obtained from multiphoton microscopy. The maximum scale of the concentration graph was standardized as 0.1% because the riboflavin solutions had the same concentration. Note that the concentration values of both curves cross at a depth of approximately 340 μm. A direct analysis of the graph shows that the curves have similar concentrations at all depths except in the range between 80 and 220 μm (p 0.012). The HPMC curve showed higher surface concentration up to 340 μm (p 0.146). The dextran curve at depths greater than 340 μm was higher (p 0.248). There was no statistically significant difference between the groups when considering all the corneal thickness studied (p 0.528).
Figure 4.
Riboflavin concentration curves in the HPMC (blue) and dextran (orange) groups.
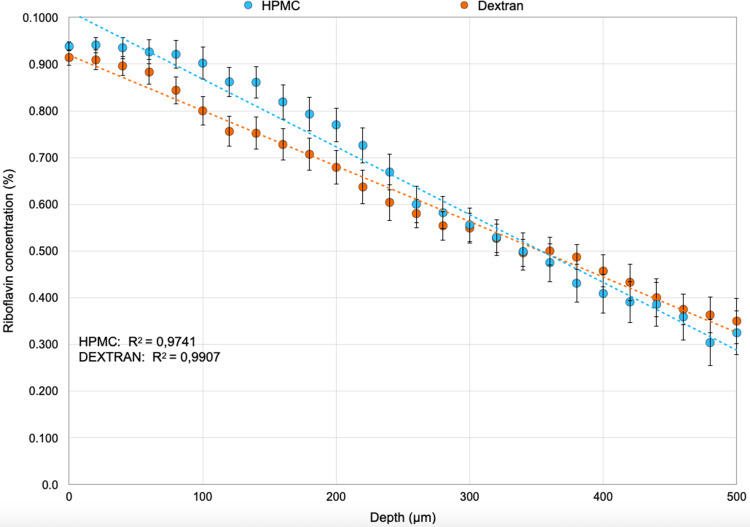
To simulate the total concentration up to 500 microns we adopted the linear (first degree) curve fitting, whose equations are shown in Figure 5, to estimate both areas. The adjustments of the linear curves (R2 = 0.9741 and 0.9907) are considered good because the R2 values are quite close to “1.0”.
Figure 5.
Linear curve fitting: HPMC (blue) and dextran (orange) groups.
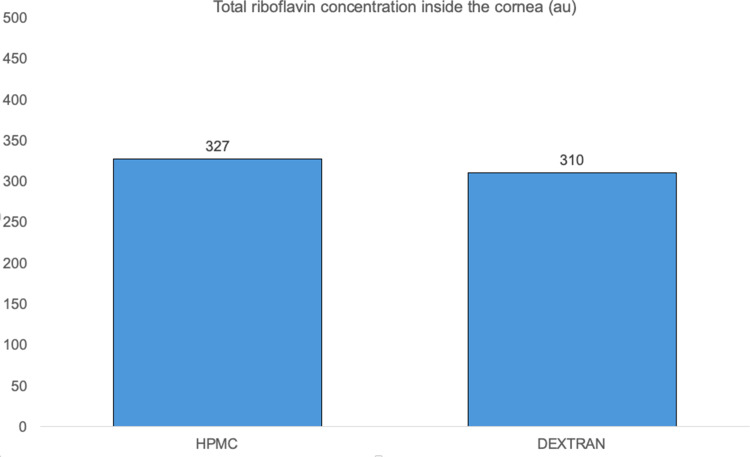
The areas obtained simulating the total amount of riboflavin in the cornea were very similar as we observed in Figure 6. There is no significant difference between these areas. Therefore, the curves are similar.
Figure 6.
Area corresponding total corneal riboflavin concentration.
The average of the central ultrasound pachymetric measurements is shown in Table 1. The mean pachymetry in the dextran group ranged from 696 μm to 606 μm, causing a decrease in corneal thickness of 12.9% in 30 min. In the HPMC group, there was a change from 684 μm to 746 μm in 10 min (an increase of 9.1%).
Table 1.
Comparison of the Average Corneal Thickness Obtained After Corneal Stabilization Prior to Application of Riboflavin (Before) and After the Use of Dextran Riboflavin for 30 min and HPMC Riboflavin for 10 min (After). Central Ultrasound Pachymetry (Mean ± Standard Error)
| Group | Before (μm) | Final (μm) | Variation |
|---|---|---|---|
| DEXTRAN 30 min | 696 +\−15 | 606 +\−13 | −12.9% |
| HPMC 10 min | 684 +\−17 | 746 +\−11 | + 9.1% |
The tonometry performed in the artificial chamber was within parameters considered physiological in all cases for the two groups, ranging from 11 to 16 mmHg. The mean tonometry obtained in the dextran group was 15 mmHg and 13 in the HPMC group.
Discussion
Riboflavin penetration is a key step in the protection and efficacy of corneal collagen crosslinking. It works as a photosensitizer for the induction of crosslinking and protects the underlying tissues as a filter from UVA irradiation. A better understanding of the behavior of each type of riboflavin in corneal tissue is essential to maximize safety.
Our study differs from previous studies because we simulated physiological conditions using methodological change. After corneal hydration control, we filled the artificial chamber with a BSS, which had characteristics similar to aqueous humor, and which is already widely used in ophthalmic surgeries aiming test conditions as close as possible to clinical conditions. Pressure control was very important because it could influence the state of hydration of the cornea and change the rate of riboflavin penetration into the stroma. Moreover, elevated pressures may alter the final effects of crosslinking on porcine corneas.15 No reservoir was used on the cornea during soaking to simulate the exact conditions used during corneal crosslinking. Another factor also taken into account not to use the reservoir was the study16 that described the formation of the dextran riboflavin film with 70 μm and breakup time of 22 min, while HPMC riboflavin showed tear film of 300 μm and breakup time of 32 min.
The study of riboflavin penetration in the corneal stroma has been reported by several research groups. Many recent technical variations have emerged based on the Dresden protocol,10 including variations in irradiation time,17 in the type of riboflavin, without corneal de-epithelialization, the use of iontophoresis,18 as well as the use of personalized treatments.19 The current protocols are promising, but it is necessary to study the behavior of each riboflavin in the corneal stroma to standardize behaviors and compare results.
The corneal riboflavin concentration in the dextran 20% for 30 minutes was considered effective in the crosslinking procedure because it has been extensively studied. Lower absorption could affect safety. Fick’s second law of diffusion describes the diffusion of riboflavin solution into the cornea.20 The partial pressure of solved riboflavin most likely represents the driving force for diffusion, independent of the osmotic agent. The riboflavin diffusion is independent of the osmotic agent because partial pressure of solved riboflavin generates force for diffusion.
FI curve formed by the dextran group presented a behavior slightly different from standard diffusion curves, which can be explained by the variation in the optical properties of the dextran21 that can be caused by the temperature variation during the accomplishment of TPF.
Our results showed that the concentration curves of the groups dextran 30 min. and HPMC 10 min. have similar behavior throughout the corneal thickness studied. These data show that soaking with HPMC in 10 minutes has the same effectiveness as dextran in 30 minutes. The curves cross approximately at the depth of 340 μm. HPMC group showed higher concentration in the superficial layers, but when considering the range of 0 to 340 microns there was no statistical difference between the groups (p 0.146). We observed a higher dextran concentration of 340 to 500 microns, but with no statistically significant difference (p 0.248).
The similarity of the curves can be confirmed by complementary analysis adjusting the curves by the trend lines. The areas formed by the curves also showed by the total gradient of riboflavin concentration in the corneas studied did not present significant differences.
The majority of studies with HPMC have a concentration of 1.1%. Our study was done with HPMC riboflavin at 1% concentration.
Ehmke et al12 did not find statistically significant differences in riboflavin concentrations (1,1% HPMC and 20% dextran) from zero to 350 μm, but they reported a higher concentration of dextran riboflavin in the first 70 μm. These results differ from those found in our study, but it is possible that this difference resulted in differences in the methodology used and HPMC different concentration. Thorsrud et al demonstrated that HPMC riboflavin has faster diffusion than dextran riboflavin.22
HPMC riboflavin allows a shorter procedure time than the Dresden protocol; thus, our study favors the current tendency to decrease the total procedural time of corneal crosslinking.
Some authors have demonstrated the influence of different riboflavin solutions on corneal thickness during the soaking time. The pachymetric measurements varied after the use of riboflavin, and the group with dextran showed a decrease of 12.9% in thickness after 30 min. This result has great importance in clinical use because corneas with a thickness close to 400 μm can compromise the safety of the procedure. The reduction in corneal thickness can be explained by the oncotic effect of the 20% dextran solution. The HPMC group showed 9.1% corneal thickness increase after 10 min. A previous study reported a decrease in corneal thickness of 12.1% with dextran riboflavin (30 min) and a 26.1% increase pachymetry using 1.1% HPMC riboflavin (for 20 min).23 The saturation time of riboflavin in HPMC for 20 min in the study cited above may be the cause of the most significant increase in corneal thickness when compared to our study. Kymionis et al24 reported a 20% thickness reduction using dextran riboflavin within 30 min.
Pachymetric measurements showed corneas with increased thicknesses, consequently, lower collagen content per volume may influence the diffusion gradient. Corneal hydration has great importance in the penetration of riboflavin because the more compact the fibers are, the greater the difficulty of absorption of riboflavin.
The concentration of the 2 solutions is similar up to 500 μm. Evaluating the depth of 340 microns that the curves intersect, we observed that depth corresponds to physiological conditions of hydration at approximately 310 microns in the HPMC group (increase 9.1%) and 395 in the dextran group (fall 12.9%).
A limitation of our research is the variation of the state of corneal hydration during the procedure.
The control of pressure within values considered normal in the artificial chamber using the Icare tonometer simulated physiological conditions, and reduced variables that could interfere the riboflavin penetration.
Conclusion
This study used different methods than previous studies to better simulate corneal physiological conditions, and used different HPMC riboflavin concentration. We concluded that 1% HPMC riboflavin for 10 min showed corneal concentration similar dextran riboflavin for 30 min therefore had the same level of safety and effectiveness in soaking when compared to the standardized use of the Dresden protocol. Ultrasonic pachymetry during the crosslinking procedure has fundamental importance corneal hydration control, due to changes in thickness caused by different types of riboflavin. Finally, our study strengthens the hypothesis that soaking with 1% HPMC riboflavin for 10 minutes is safe and promotes greater effectiveness in the total crosslinking time of corneal collagen. Clinical studies should be done to prove this hypothesis.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ashwin PT, McDonnell PJ. Collagen cross-linkage: a comprehensive review and directions for future research. Br J Ophthalmol. 2010;94(8):965e970. doi: 10.1136/bjo.2009.164228 [DOI] [PubMed] [Google Scholar]
- 2.Wollensak G, Spoerl E, Wilsch M, Seiler T. Keratocyte apoptosis after corneal collagen cross-linking using riboflavin/UVA treatment. Cornea. 2004;23(1):43–49. doi: 10.1097/00003226-200401000-00008 [DOI] [PubMed] [Google Scholar]
- 3.Spoerl E, Wollensak G, Seiler T. Increased resistance of crosslinked cornea against enzymatic digestion. Curr Eye Res. 2004;29(1):35–40. doi: 10.1080/02713680490513182 [DOI] [PubMed] [Google Scholar]
- 4.Wollensak G, Spoerl E, Rebel F, Pillunat L, Funk R. Corneal endothelial cytotoxicity of riboflavin/UVA treatment in vitro. Ophthalmic Res. 2003;35:324–328. doi: 10.1159/000074071 [DOI] [PubMed] [Google Scholar]
- 5.Wollensak G, Spoerl E, Reber F, Seiler T. Keratocyte cytotoxicity of riboflavin/UVA treatment in vitro. Eye. 2004;18:718–722. doi: 10.1038/sj.eye.6700751 [DOI] [PubMed] [Google Scholar]
- 6.Seiler T, Spoerl E, Huhle M, Kamouna A. Conservative therapy of keratoconus by enhancement of collagen cross-links. Invest Ophthalmol Vis Sci. 1996;37:S1017. [Google Scholar]
- 7.Kohlhaas M, Spoerl E, Speck A, et al. A new treatment of keratectasia after LASIK with riboflavin/UVA light cross-linking. Klin Monatsbl Augenheilkd. 2005;222:430–436. doi: 10.1055/s-2005-857950 [DOI] [PubMed] [Google Scholar]
- 8.Coskunseven E, Jankov MR, Hafezi F. Comparative study of corneal collagen cross-linking with riboflavin and UVA irradiation in patients with keratoconus. J Refract Surg. 2009;25:371–376. doi: 10.3928/1081597X-20090401-02 [DOI] [PubMed] [Google Scholar]
- 9.Vinciguerra P, Albe E, Trazza S, et al. Refractive, topographic, tomographic, and aberrometric analysis of keratoconic eyes undergoing corneal cross-linking. Ophthalmology. 2009;116(3):369–378. doi: 10.1016/j.ophtha.2008.09.048 [DOI] [PubMed] [Google Scholar]
- 10.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620–627. doi: 10.1016/S0002-9394(02)02220-1 [DOI] [PubMed] [Google Scholar]
- 11.Schumacher S, Heftier L, Mrochen M. Equivalence of biomechanical changes induced by rapid and standard corneal cross-linking, using riboflavin and ultraviolet radiation. Invest Ophthalmol Vis Sci. 2011;52(12):9048–9052. doi: 10.1167/iovs.11-7818 [DOI] [PubMed] [Google Scholar]
- 12.Ehmke T, Seiler TG, Fischinger I, et al. Comparison of corneal riboflavin gradients using dextran and HPMC solutions. J Refract Surg. 2016;32(12):798–802. doi: 10.3928/1081597X-20160920-03 [DOI] [PubMed] [Google Scholar]
- 13.Seiler TG, Ehmke T, Fischinger I, et al. Two-photon fluorescence microscopy for determination of the riboflavin concentration in the anterior corneal stroma when using the dresden protocol. Invest Ophthalmol Vis Sci. 2015;56(11):6740–6746. doi: 10.1167/iovs.15-17656 [DOI] [PubMed] [Google Scholar]
- 14.Gore DM, Margineanu A, French P, et al. Two-photon fluorescence microscopy of corneal riboflavin absorption. Invest Ophthalmol Vis Sci. 2014;55(4):2476–2481. doi: 10.1167/iovs.14-13975 [DOI] [PubMed] [Google Scholar]
- 15.McQuaid R, Li J, Cummings A, Mrochen M, Vohnsen B. Second-harmonic reflection imaging of normal and accelerated corneal crosslinking using porcine corneas and the role of intraocular pressure. Cornea. 2014;33(2):125–130. doi: 10.1097/ICO.0000000000000015 [DOI] [PubMed] [Google Scholar]
- 16.Wollensak G, Aurich H, Wiberlauer C, Sel S. Significance of the riboflavin film in corneal collagen crosslinking. J Cataract Refract Surg. 2010;36(1):114–120. doi: 10.1016/j.jcrs.2009.07.044 [DOI] [PubMed] [Google Scholar]
- 17.Ozgurhan EB, Akcay BI, Kurt T, Yildirim Y, Demirok A. Accelerated corneal collagen cross-linking in thin keratoconic corneas. J Refract Surg. 2015;31:386–390. doi: 10.3928/1081597X-20150521-11 [DOI] [PubMed] [Google Scholar]
- 18.Jouve L, Borderie V, Sandali O, et al. Conventional and iontophoresis corneal cross-linking for keratoconus: efficacy and assessment by optical coherence tomography and confocal microscopy. Cornea. 2017;36(2):153–162. doi: 10.1097/ICO.0000000000001062 [DOI] [PubMed] [Google Scholar]
- 19.Cassagne M, Pierné K, Galiacy SD, et al. Customized topography-guided corneal collagen cross-linking for keratoconus. J Refract Surg. 2017;33(5):290–297. doi: 10.3928/1081597X-20170201-02 [DOI] [PubMed] [Google Scholar]
- 20.Siepmann J, Kranz H, Bodmeier R, et al. HPMC-matrices for controlled drug delivery: a new model combining diffusion, swelling, and dissolution mechanisms and predicting the release kinetics. Pharm Res. 1999;16(11):1748–1756. doi: 10.1023/A:1018914301328 [DOI] [PubMed] [Google Scholar]
- 21.Xu X, Wang RK, Elder JB, Tuchin VV. Effect of dextran-induced changes in refractive index and aggregation on optical properties of whole blood. Phys Med Biol. 2003;48(9):1205–1221. doi: 10.1088/0031-9155/48/9/309 [DOI] [PubMed] [Google Scholar]
- 22.Thorsrud A, Hagem AM, Sandvik GF, Drolsum L. Superior outcome of corneal collagen cross-linking using riboflavin with methylcellulose than riboflavin with dextran as the main supplement. Acta Ophthalmol. 2019;97(4):415–421. doi: 10.1111/aos.13928 [DOI] [PubMed] [Google Scholar]
- 23.Zaheer N, Khan WA, Khan S, Khan MAM. Comparison of changes in central corneal thickness during corneal collagen cross-linking, using isotonic riboflavin solutions with and without dextran, in the treatment of progressive keratoconus. Cornea. 2018;37(3):340–346. doi: 10.1097/ICO.0000000000001496 [DOI] [PubMed] [Google Scholar]
- 24.Kymionis GD, Kounis GA, Portaliou DM, et al. Intraoperative pachymetric measurements during corneal collagen cross-linking with riboflavin and ultraviolet A irradiation. Ophthalmology. 2009;116(12):2336–2339. doi: 10.1016/j.ophtha.2009.09.018 [DOI] [PubMed] [Google Scholar]