Abstract
Background:
The goal of this study was to review relevant randomized controlled trials in order to determine the efficacy of decompression and lumbar interbody fusion in the treatment of lumbar spinal stenosis.
Method:
Using appropriate keywords, we identified relevant studies in PubMed, the Cochrane library, and Embase. Key pertinent sources in the literature were also reviewed, and all articles published through July 2019 were considered for inclusion. For each study, we assessed odds ratios, mean difference, and 95% confidence interval to assess and synthesize outcomes.
Result:
Twenty-one randomized controlled trials were eligible for this meta-analysis with a total of 3636 patients. Compared with decompression, decompression and fusion significantly increased length of hospital stay, operative time and estimated blood loss. Compared with fusion, decompression significantly decreased operative time, estimated blood loss and overall visual analogue scale (VAS) scores. Compared with endoscopic decompression, microscopic decompression significantly increased length of hospital stay, and operative time. Compared with traditional surgery, endoscopic discectomy significantly decreased length of hospital stay, operative time, estimated blood loss, and overall VAS scores and increased Japanese Orthopeadic Association score. Compared with TLIF, MIS-TLIF significantly decreased length of hospital stay, and increased operative time and SF-36 physical component summary score. Compared with multi-level decompression and single level fusion, multi-level decompression and multi-level fusion significantly increased operative time, estimated blood loss and SF-36 mental component summary score and decreased Oswestry disability index score. Compared with decompression, decompression with interlaminar stabilization significantly decreased operative time and the score of Zurich claudication questionnaire symptom severity, and increased VAS score.
Conclusion:
Considering the limited number of included studies, we still need larger-sample, high-quality, long-term studies to explore the optimal therapy for lumbar spinal stenosis.
Keywords: decompression, fusion, lumbar spinal stenosis, meta-analysis
1. Introduction
Lumbar spinal stenosis (LSS) is a group of syndromes due to the stenosis of the central, lateral recess and intervertebral foramen of the lumbar spinal canal, which causes nerve compression and blood circulation disorder. LSS patients present with lower limb pain, neurogenic intermittent claudication or back pain symptoms. LSS is a common and frequently occurring orthopedic disease. With an ever aging population, and increasingly tense social life and work, the incidence rate of LSS gradually increases, which not only seriously affects the life and work of patients, but also causes great economic losses to the society. In terms of etiology, the causes of LSS can be roughly divided into3 categories: congenital, degenerative, and other causes.[1–3] Among them, degenerative LSS is a common degenerative disease among middle-aged and elderly persons. Degenerative changes in the lumbar spine, including intervertebral disc degeneration, facet joint degeneration, facet joint hyperplasia, lamina thickening, and posterior labial osteophyte hyperplasia of the vertebral body, are all factors leading to degenerative spinal canal stenosis. Because a series of LSS symptoms including intermittent claudication, sciatica, and horsetail often cause great trouble in the lives of patients, and severely compromise patient's quality of life, treatment of degenerative LSS to improve the quality of life of elderly patients have great significance.[4–6]
Currently, LSS treatment includes non-surgical and surgical treatment. Non-operative treatment is suitable for patients with mild and moderate symptoms. Commonly used conservative treatments include manipulation, treatments, pharmacotherapy, closure therapy, lumbar back exercise, waist protection, and other treatments such as hyperthermia, cryotherapy, ultrasound, and massage, electrical stimulation, and traction. Surgical treatment is effective in cases of compromised patientʼs quality of life, intolerable pain, ineffective conservative treatment, recurrent symptoms, and obvious root symptoms. At present, strong fixation and solid bone graft fusion after full decompression are generally adopted in clinical practice, which is considered as the gold standard for LSS treatment.[7–9]
The aim of this study was to perform a meta-analysis of all available literature to obtain updated evidence about the efficacy of decompression and lumbar interbody fusion in the treatment of LSS.
2. Methods
2.1. Search strategy
To identify studies pertaining to the efficacy of decompression and lumbar interbody fusion in the treatment of LSS, we reviewed the Cochrane library, PubMed, and Embase databases for relevant articles published through July 2019. We also reviewed the references of all identified articles to identify additional studies. Search terms were as follows: lumbar spinal stenosis, lumbar stenosis, LSS, decompression, micro decompression, endoscopy decompression, fusion, transforaminal lumbar interbody fusion, TLIF, and MIS-TLIF. These terms were used in combination with “AND” or “OR”. This literature review was performed independently by 2 investigators, with a third resolving any disputes as needed.
Following the PICOS (Participants, Interventions, Comparisons, Outcomes, and Study design) principle, the key search terms included (P) patients with LSS; (I) decompression and/or fusion; (C/O) comparison of the clinical efficacy of different methods of decompression, or different methods of fusion, or decompression with fusion; the outcomes included clinical efficacy measures; (S) randomized controlled trial.
2.2. Study selection criteria
The inclusion criteria were:
-
(1)
randomized controlled trials;
-
(2)
the interventions of the treatment group and control group included different methods of decompression or/and fusion;
-
(3)
patients with LSS;
-
(4)
publications in English or Chinese.
The exclusion criteria were:
-
(1)
duplicate articles or results;
-
(2)
obvious data errors;
-
(3)
case reports, case-control studies, theoretical research, conference reports, systematic reviews, meta-analyses, and other forms of research or comment not designed in a randomized controlled manner;
-
(4)
lack of clinical outcomes of interest;
-
(5)
lack of a control group.
Two investigators independently determined whether studies met the inclusion criteria, with a third resolving any disputes as needed.
2.3. Data extraction and quality assessment
For each included study, 2 categories of information were extracted: basic information and primary study outcomes. Basic information relevant to this meta-analysis included: author names, year of publication, sample size, mean age, gender, surgery strategy, and Jadad score. Primary clinical outcomes relevant to this analysis included: length of hospital stay, operative time, blood loss, complications, Oswestry disability index (ODI) score, visual analogue scale (VAS) score of overall, leg pain and back pain, Japanese Orthopeadic Association (JOA) score, the Short Form (36) Health Survey (SF-36) score of physical component summary and mental component summary, and Zurich claudication questionnaire (ZCQ) score of symptom severity and physical function.
Study quality was determined on the basis of Jadad scores, which were determined based on how well each study satisfied the following criteria: studies included a specific statement regarding randomization; the method used to randomize patients was appropriate; the study was conducted in a double-blinded manner; the approach to double-blinding was described appropriately; information on any patients who withdrew from or dropped out of the study was provided. A Jadad score < 3 indicated a study of low-quality, and thus was associated with a substantial risk of bias. This data extraction was performed independently by 2 investigators, with a third resolving any disputes as needed.
2.4. Statistical analysis
STATA v10.0 (TX) was used for all analyses. Heterogeneity in study results was assessed using Chi-squared and I2 tests and appropriate analysis models (fixed-effects or random-effects) were determined. A Chi-squared P ≤.05 and an I2>50% indicated high heterogeneity and the random-effects model was used in this case. A Chi-squared P>.05 and an I2≤50% indicated acceptable heterogeneity and the fixed-effects model was used instead. Continuous variables were given as mean ± standard deviation and compared on the basis of mean difference (MD), while categorical data was given as percentages and compared based on relative risk/odds ratios. MD and 95% CI were used to analyze all the indexes except complication.
3. Results
3.1. Overview of the included studies
We reviewed a total of 1159 articles identified by our initial keyword search, of which 1075 were excluded following title/abstract review. The remaining 84 articles were subject to a complete full-text assessment, and 63 articles that did not meet the study inclusion criteria were excluded. Reasons for exclusion of these studies included: theoretical research (n = 6), no clinical outcomes (n = 19), duplicate articles (n = 2), and case report or lack of a control group (n = 36). We ultimately identified a total of 21 randomized controlled trials[10–30] that met the inclusion criteria for this meta-analysis, including 3636 patients. Study selection is outlined in Figure 1.
Figure 1.
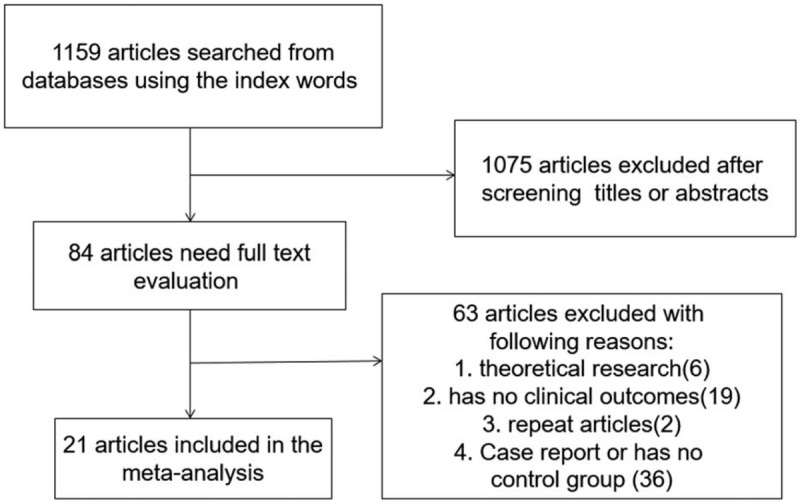
Literature search and selection strategy.
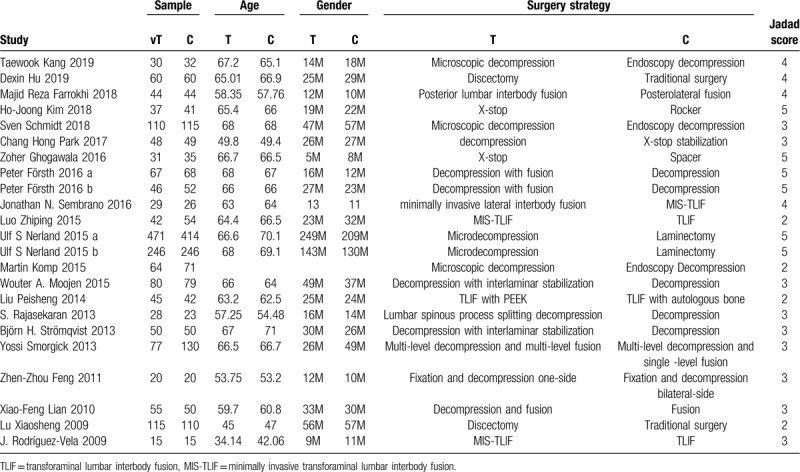
Table 1 summarizes the basic information for each study, including author names, year of publication, sample size, mean age, gender, surgery strategy and Jadad score. A mean Jadad score for these selected studies was 3.52, indicating that all included studies were of high quality.
Table 1.
The basic characteristics description of included studies.
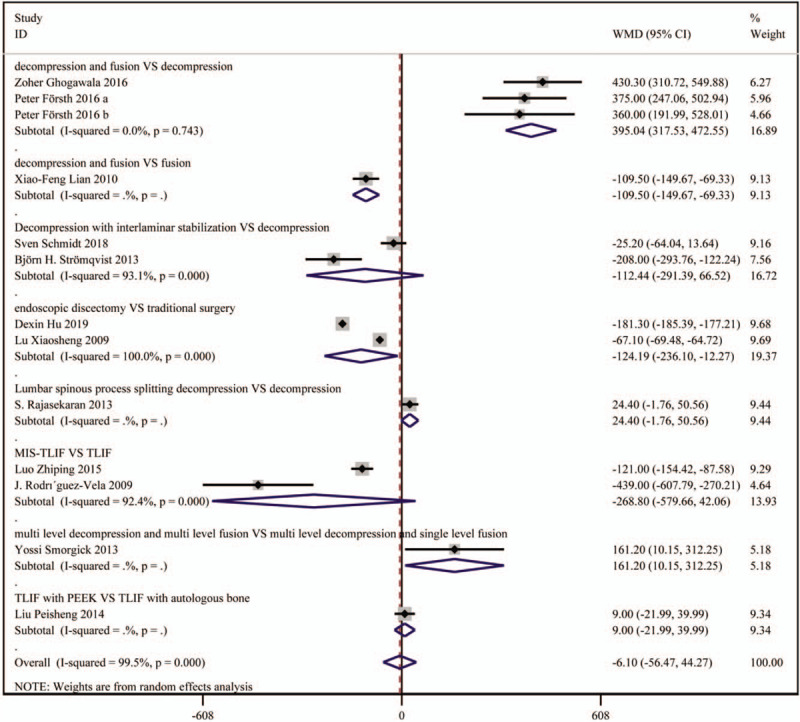
3.2. Length of hospital
Ten studies including 1160 patients reported on the result of length of hospital stay. The length of hospital stay was significantly lengthened in the decompression and fusion group vs the decompression group (weighted mean difference [WMD]: 2.19, 95%CI: 0.60–3.77), and the microscopic decompression group vs the endoscopy decompression group (WMD: 2.30, 95%CI: 2.00–2.60). The length of hospital stay was significantly shortened in the endoscopic discectomy group vs the traditional surgery group (WMD: –4.19, 95%CI: –5.76 to 2.63), and the MIS-TLIF group vs the TLIF group (WMD: –1.60, 95%CI: –2.42 to 0.78). There was no significant difference in the length of hospital stay in patients receiving decompression with interlaminar stabilization vs patients receiving decompression, patients receiving lumbar spinous process splitting decompression vs patients receiving decompression, patients receiving minimally invasive lateral interbody fusion vs patients receiving MIS-TLIF, patients receiving multi-level decompression and multi-level fusion vs patients receiving multi-level decompression and single level fusion, and patients receiving TLIF with PEEK vs patients receiving TLIF with autologous bone. The result is shown in Figure 2.
Figure 2.
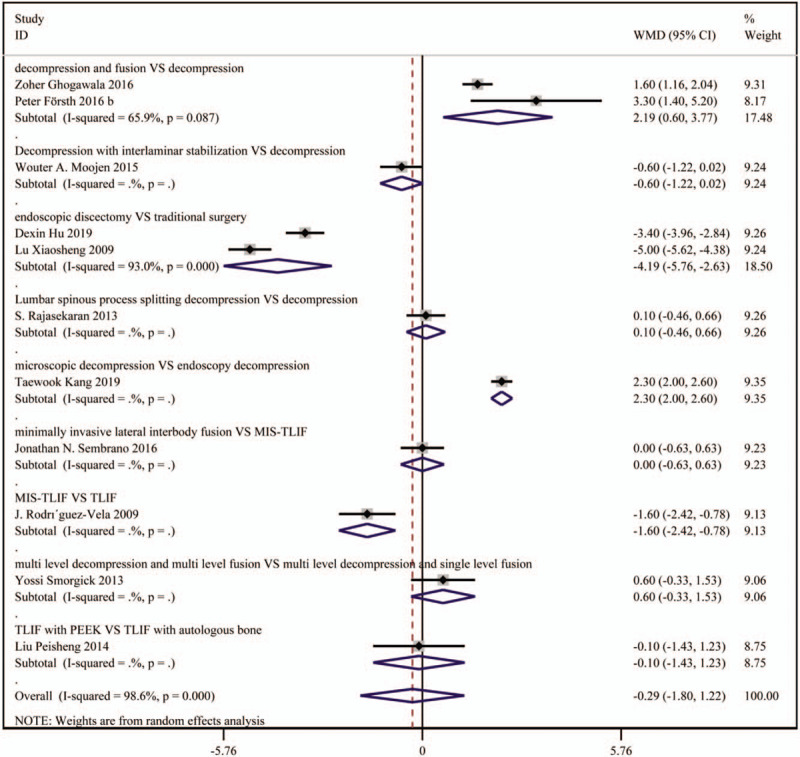
Forest plot for length of hospital stay.
3.3. Operative time
Seventeen studies including 1906 patients reported operative time. The operative time was significantly lengthened in patients receiving decompression and fusion vs patients receiving decompression (WMD: 95.12, 95%CI: 41.53–148.89), patients receiving microscopic decompression vs patients receiving endoscopic decompression (WMD: 20.38, 95%CI: 16.53–24.23), patients receiving MIS-TLIF vs patients receiving TLIF (WMD: 17.24, 95%CI: 6.99–27.48), and patients receiving multi-level decompression and multi-level fusion vs patients receiving multi-level decompression and single level fusion (WMD: 63.50, 95%CI: 39.31–87.69). The operative time was significantly shortened in patients receiving decompression and fusion vs patients receiving fusion (WMD: –28.10, 95%CI: –39.44 to 10.07), patients receiving endoscopic discectomy vs patients receiving traditional surgery (WMD: –50.30, 95%CI: –56.40 to 44.40), and patients receiving decompression with interlaminar stabilization vs patients receiving decompression (WMD: –20.38, 95%CI: –30.70 to 10.07). There was no significant difference in operative time among other subgroups. The result is shown in Figure 3.
Figure 3.
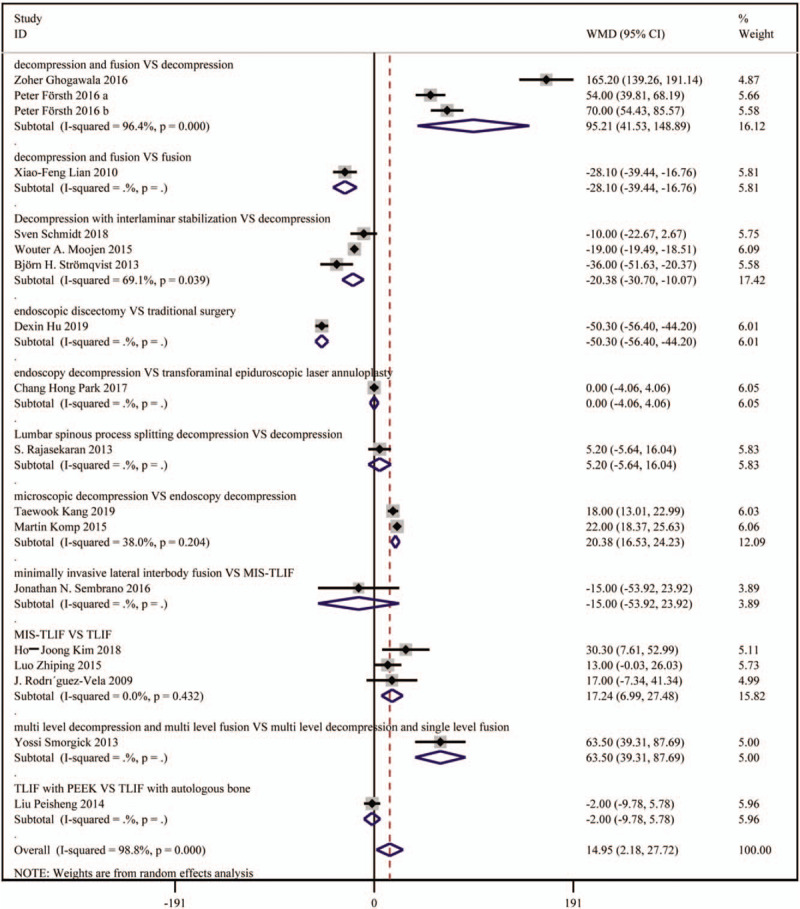
Forest plot for operative time.
3.4. Estimated blood loss
Twelve studies including 1545 patients reported estimated blood loss. The estimated blood loss was significantly higher in patients receiving decompression and fusion than patients receiving decompression (WMD: 395.04, 95%CI: 317.53–472.55), and patients receiving multi-level decompression and multi-level fusion than patients receiving multi-level decompression and single level fusion (WMD: 161.20, 95%CI: 10.15–312.25). The estimated blood loss significantly decreased in patients receiving decompression and fusion vs patients receiving fusion (WMD: –109.50, 95%CI: –149.67 to 69.33), and patients receiving endoscopic discectomy vs patients receiving traditional surgery (WMD: –124.19, 95%CI: –236.10 to 12.27). There was no significant difference in estimated blood loss among other subgroups. The result is shown in Figure 4.
Figure 4.
Forest plot for estimated blood loss.
3.5. ODI
Eight studies including 926 patients reported on the result of ODI. The ODI score significantly decreased in the multi-level decompression and multi-level fusion group vs the multi-level decompression and single level fusion group (WMD: –0.90, 95%CI: –1.54 to 0.26). There was no significant difference in ODI score in other subgroups. The result is shown in Figure 5.
Figure 5.
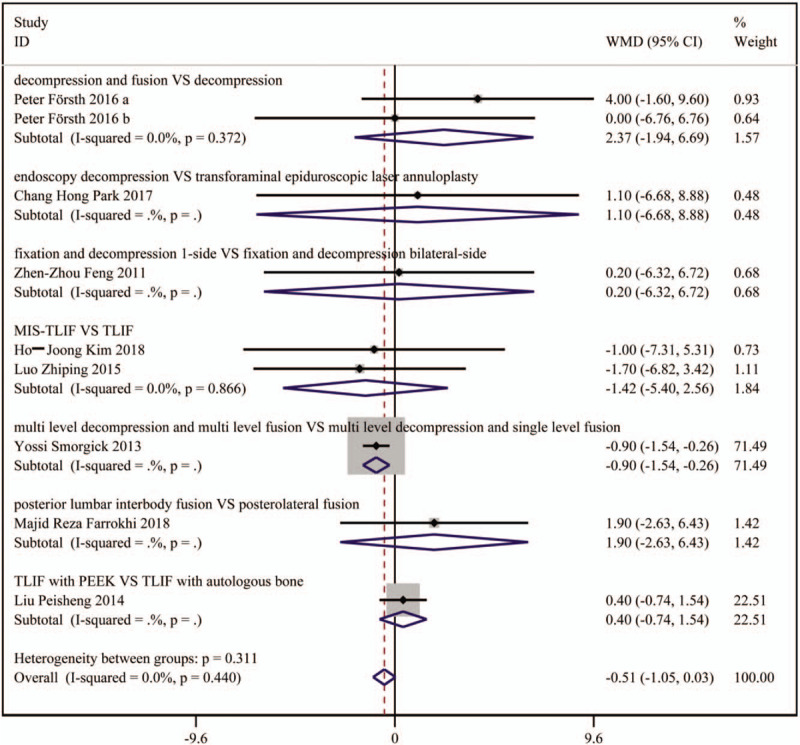
Forest plot for Oswestry disability index scores.
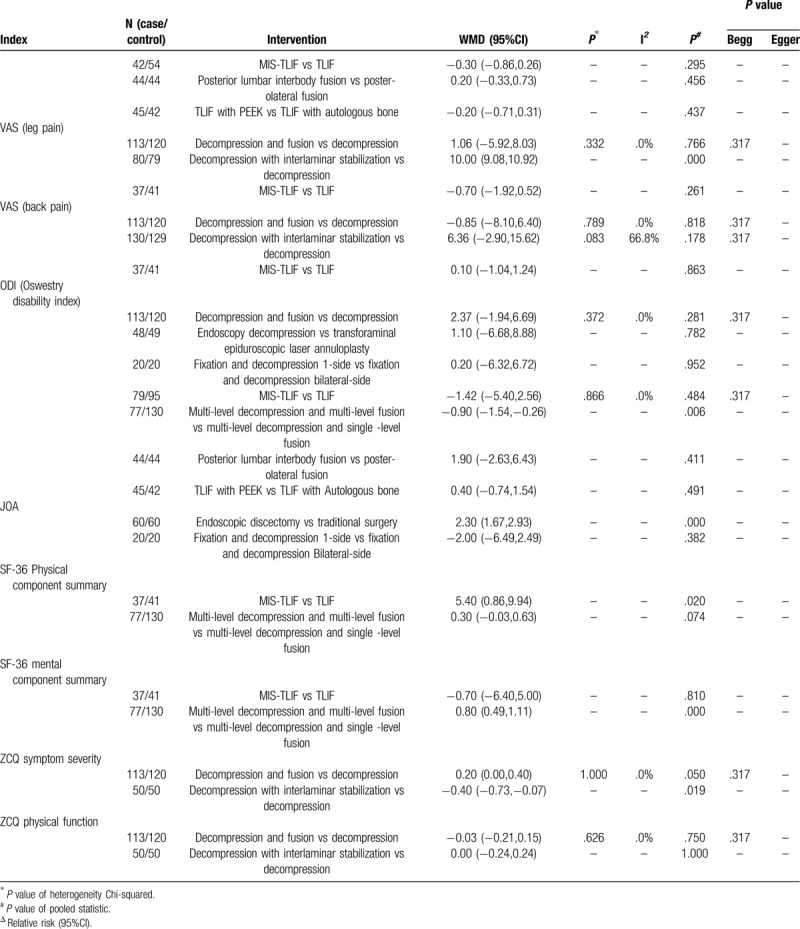
3.6. Other results
No significant difference was observed in the incidence of complications in all the subgroup analysis. The overall VAS score was significantly lower in patients receiving decompression and fusion than patients receiving fusion (WMD: –5.90, 95%CI: –10.38 to 1.42), as well as in patients receiving endoscopic discectomy than patients receiving traditional surgery (WMD: –1.30, 95%CI: –1.57 to 1.03). The VAS score of leg pain significantly increased in patients receiving decompression with interlaminar stabilization group vs patients receiving decompression (WMD: 10.00, 95%CI: 9.08–10.92). The JOA score was significantly higher in patients receiving endoscopic discectomy than patients receiving traditional surgery (WMD: 2.30, 955CI: 1.67–2.93). The score of SF-36 physical component summary significantly increased in the MIS-TLIF group vs the TLIF group (WMD: 5.40, 95%CI: 0.86–9.94). The score of SF-36 mental component summary was significantly higher in the multi-level decompression and multi-level fusion group than the multi-level decompression and single level fusion group (WMD: 0.80, 95%CI: 0.49–1.11). The score of ZCQ symptom severity was significantly lower in the decompression with interlaminar stabilization group than the decompression group (WMD: –0.40, 95%CI: –0.73 to 0.07). The results are shown in Table 2 .
Table 2.
The results of meta-analysis.
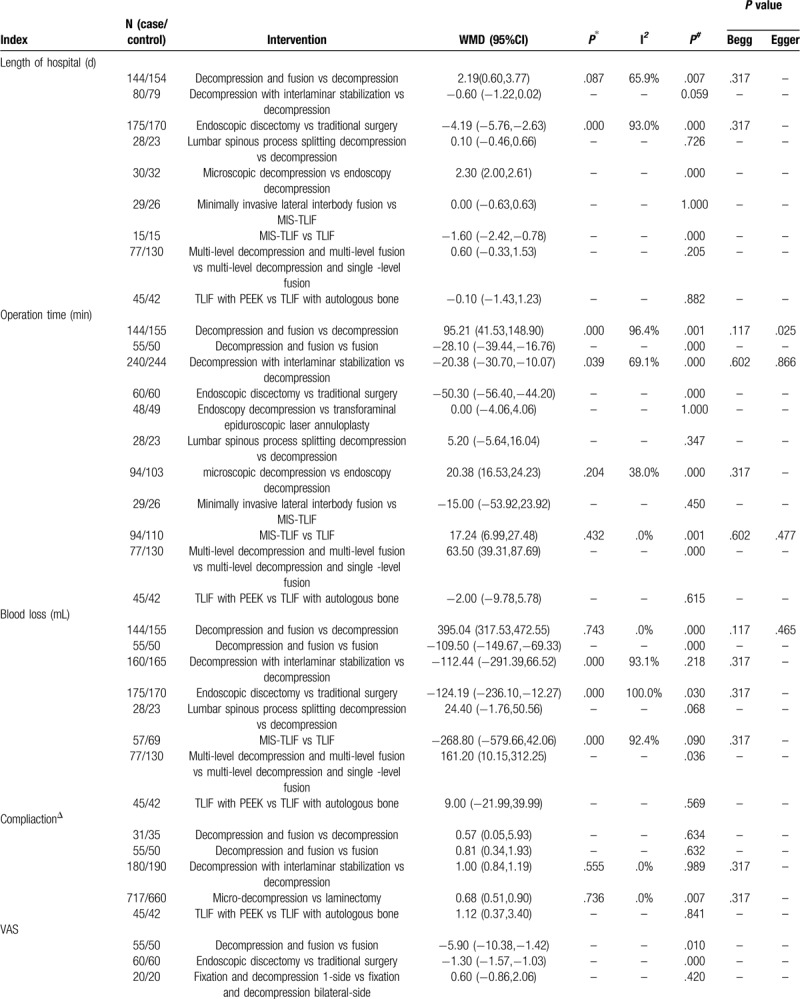
Table 2 (Continued).
The results of meta-analysis.
4. Discussion
The purpose of LSS surgery is not to cure, but to relieve the clinical symptoms such as intermittent claudication, lumbago pain and neurological dysfunction, and improve the patients’ quality of life. Most investigators believe that the indications of surgical treatment of LSS mainly include:
-
(1)
moderate and severe nerve root radiation pain or nerve root function damage, with or without back pain;
-
(2)
intermittent claudication, walking distance less than 100 to 200 m or progressive aggravation;
-
(3)
progressive scoliosis and slippage accompanied by increasing clinical signs and symptoms, affecting life activities;
-
(4)
symptoms of cauda equina nerve injury;
-
(5)
after conservative treatment for 3 to 6 months without significant relief, in general, patients can tolerate the operation. In recent years, LSS has become a common indication in spinal surgery. LSS surgery can be divided into lumbar laminectomy and decompression, pedicle screw internal fixation and bone graft fusion.
LSS is often treated by decompression, bone grafting, and fusion internal fixation. In other words, on the basis of sufficient decompression, rigid fixation and solid bone grafting and fusion are performed. According to long-term follow-up data, this technique is safe and effective, and has become the gold standard for the treatment of spinal degenerative diseases such as LSS. After decompression for LSS in recent years, especially with the new development of the concept of spine surgery, fusion surgery gradually becomes the hot topic in the study of spinal surgery, many experts and scholars try to use varied elastic fixation approaches that fit more closely the biomechanical environment of the spine. However, after decompression, rigid fixation and bone graft fusion were not performed at the same time, and postoperative lumbar spondylolisthesis was reported. Therefore, lumbar decompression, especially after extensive decompression, with rigid fixation and bone graft fusion, remains indispensable. In addition, many patients received effective fusion in clinical treatment, but the effect was not satisfactory. From the perspective of biomechanics, the strong fixation system bears most of the load, while the load shared by the relatively fixed segments is greatly reduced, which produces stress shielding effect and reduces physiological pressure. At the same time, with the strength of rigidly fixed small joints of the adjacent segments and increased activity range of the intervertebral disc, bearing stress changes, and higher pressure on the intervertebral disc, trigger a series of issues such as fixed segment osteoporosis and bone atrophy, lower quality of bone fusion, stress concentration caused by broken nails, broken rod, adjacent segment disc, and small joint degeneration,. Therefore, the ideal approach is to increase stress conduction and load sharing, reduce stress shielding and stress concentration, while ensuring that the spine is firm and stable.
Strengths of this meta-analysis include the following: the systematic nature of this analysis makes the results more convincing than those of individual studies, given that these results rely upon a large pooled sample size. Strict inclusion and exclusion criteria were used to select qualified studies. All the data were analyzed by standard statistical analyses to ensure accuracy. Furthermore, all the included studies were high-quality RCTs, making the conclusion more clinically significant.
However, there are certain limitations to the present analysis, which are as follows:
-
(1)
only RCTs were included;
-
(2)
the technique levels of operations were varied among the studies;
-
(3)
the number of included studies was limited;
-
(4)
pooled data were analyzed, as individual patient data was not available, precluding more in-depth analyses.
Our results indicate that compared with decompression, decompression, and fusion significantly increase the length of hospital stay, operative time and estimated blood loss. Compared with fusion, decompression significantly decreased operative time, estimated blood loss and overall VAS scores. Compared with endoscopic decompression, microscopic decompression significantly increased length of hospital stay and operative time. Compared with traditional surgery, endoscopic discectomy significantly decreased length of hospital stay, operative time, estimated blood loss, and overall VAS score; increased JOA score. Compared with TLIF, MIS-TLIF significantly decreased length of hospital stay, and increased operative time, and the score of SF-36 physical component summary. Compared with multi-level decompression and single level fusion, multi-level decompression and multi-level fusion significantly increased operative time, estimated blood loss and the score of SF-36 mental component summary, and decreased ODI score. Compared with decompression, decompression with interlaminar stabilization significantly decreased operative time and the score of ZCQ symptom severity, and increased VAS score. Considering the limitations of this study, larger-sample, high-quality, long-term studies are needed to explore the optimal therapy.
Ethical approval: Since animal experiment or human was not involved in this study, the ethical approval was not necessary.
Author contributions
LHY and LZ have made substantial contributions to conception and design of the study, written the manuscript; WL, JL, WYZ, LKA, SY and HK searched literature, extracted data from the collected literature and analyzed the data; LHY revised the manuscript; All authors approved the final version of the manuscript.
Footnotes
Abbreviations: JOA = Japanese Orthopaedic Association, LSS = lumbar spinal stenosis, MD = mean difference, ODI = Oswestry disability index, SF-36 = the Short Form (36) Health Survey, VAS = visual analogue scale, ZCQ = Zurich claudication questionnaire.
How to cite this article: Yang L-H, Liu W, Li J, Zhu WY, An L-K, Yuan S, Ke H, Zang L. Lumbar decompression and lumbar interbody fusion in the treatment of lumbar spinal stenosis: a systematic review and meta-analysis. Medicine. 2020;99:27(e20323).
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010;303:1259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mobbs RJ, Sivabalan P, Li J. Minimally invasive surgery compared to open spinal fusion for the treatment of degenerative lumbar spine pathologies. J Clin Neurosci 2012;19:829–35. [DOI] [PubMed] [Google Scholar]
- [3].Thome C, Zevgaridis D, Leheta O, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine 2005;3:129–41. [DOI] [PubMed] [Google Scholar]
- [4].Usman M, Ali M, Khanzada K, et al. Unilateral approach for bilateral decompression of lumbar spinal stenosis: a minimal invasive surgery. J Coll Physicians Surg Pak 2013;23:852–6. [PubMed] [Google Scholar]
- [5].Bisschop A, van Dieen JH, Kingma I, et al. Torsion biomechanics of the spine following lumbar laminectomy: a human cadaver study. Eur Spine J 2013;22:1785–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Du Bois M, Szpalski M, Donceel P. A decade's experience in lumbar spine surgery in Belgium: sickness fund beneficiaries, 2000-2009. Eur Spine J 2012;21:2693–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lund T, Oxland TR. Adjacent level disk disease – is it really a fusion disease? Orthop Clin North Am 2011;42:529–41. [DOI] [PubMed] [Google Scholar]
- [8].Polikeit A, Nolte LP, Ferguson SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine (Phila PA 1976) 2003;28:991–6. [DOI] [PubMed] [Google Scholar]
- [9].Imai A, Kaneoka K, Okubo Y, et al. Trunk muscle activity during lumbar stabilization exercises on both a stable and unstable surface. J Orthop Sports Phys Ther 2010;40:369–75. [DOI] [PubMed] [Google Scholar]
- [10].Kang T, Park SY, Kang CH, et al. Is biportal technique/endoscopic spinal surgery satisfactory for lumbar spinal stenosis patients? A prospective randomized comparative study. Medicine (Baltimore) 2019;98:e15451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hu D, Fei J, Chen G, et al. Treatment for lumbar spinal stenosis in elderly patients using percutaneous endoscopic lumbar discectomy combined with postoperative three-dimensional traction. Expert Rev Med Devices 2019;16:317–23. [DOI] [PubMed] [Google Scholar]
- [12].Farrokhi MR, Yadollahikhales G, Gholami M, et al. Clinical outcomes of posterolateral fusion vs. posterior lumbar interbody fusion in patients with lumbar spinal stenosis and degenerative instability. Pain Physician 2018;21:383–406. [PubMed] [Google Scholar]
- [13].NSW, Department of, health., policies for developmental disability, services. Lamp 1985;42:23–4. https://pubmed.ncbi.nlm.nih.gov/2978165/?from_single_result=Department+of%2C+health.%2C+policies+for+developmental+disability%2C+AQ8+services.+Lamp+1985%3B42%3A23%E2%80%934 [PubMed] [Google Scholar]
- [14].Schmidt S, Franke J, Rauschmann M, et al. Prospective, randomized, multicenter study with 2-year follow-up to compare the performance of decompression with and without interlaminar stabilization. J Neurosurg Spine 2018;28:406–15. [DOI] [PubMed] [Google Scholar]
- [15].Park CH, Lee SH. Endoscopic epidural laser decompression versus transforaminal epiduroscopic laser annuloplasty for lumbar disc herniation: a prospective, randomized trial. Pain Physician 2017;20:663–70. [PubMed] [Google Scholar]
- [16].Ghogawala Z, Dziura J, Butler WE, et al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 2016;374:1424–34. [DOI] [PubMed] [Google Scholar]
- [17].Forsth P, Olafsson G, Carlsson T, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 2016;374:1413–23. [DOI] [PubMed] [Google Scholar]
- [18].Sembrano JN, Tohmeh A, Isaacs R, et al. Two-year comparative outcomes of mis lateral and mis transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: Part I: Clinical Findings. Spine (Phila PA 1976) 2016;41: Suppl 8: S123–32. [DOI] [PubMed] [Google Scholar]
- [19].Luo Z, Rao H, Huang D, et al. Comparison of minimally invasive using a tubular retraction system versus open transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases. Zhonghua Yi Xue Za Zhi 2015;95:2681–5. [PubMed] [Google Scholar]
- [20].Nerland US, Jakola AS, Solheim O, et al. Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ 2015;350:h1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Komp M, Hahn P, Oezdemir S, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician 2015;18:61–70. [PubMed] [Google Scholar]
- [22].Moojen WA, Arts MP, Jacobs WC, et al. IPD without bony decompression versus conventional surgical decompression for lumbar spinal stenosis: 2-year results of a double-blind randomized controlled trial. Eur Spine J 2015;24:2295–305. [DOI] [PubMed] [Google Scholar]
- [23].Liu P, Liu X, Qiao X, et al. Comparison of clinical efficacies of single segment transforaminal lumbar interbody fusion with cage versus autogenous morselized bone for degenerative lumbar spinal stenosis: a prospective randomized controlled study. Zhonghua Yi Xue Za Zhi 2014;94:2731–5. [PubMed] [Google Scholar]
- [24].Rajasekaran S, Thomas A, Kanna RM, et al. Lumbar spinous process splitting decompression provides equivalent outcomes to conventional midline decompression in degenerative lumbar canal stenosis: a prospective, randomized controlled study of 51 patients. Spine (Phila PA 1976) 2013;38:1737–43. [DOI] [PubMed] [Google Scholar]
- [25].Stromqvist BH, Berg S, Gerdhem P, et al. X-stop versus decompressive surgery for lumbar neurogenic intermittent claudication: randomized controlled trial with 2-year follow-up. Spine (Phila PA 1976) 2013;38:1436–42. [DOI] [PubMed] [Google Scholar]
- [26].Smorgick Y, Park DK, Baker KC, et al. Single- versus multilevel fusion for single-level degenerative spondylolisthesis and multilevel lumbar stenosis: four-year results of the spine patient outcomes research trial. Spine (Phila PA 1976) 2013;38:797–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Feng ZZ, Cao YW, Jiang C, et al. Short-term outcome of bilateral decompression via a unilateral paramedian approach for transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Orthopedics 2011;34:364. [DOI] [PubMed] [Google Scholar]
- [28].Lian XF, Xu JG, Zeng BF, et al. Noncontiguous anterior decompression and fusion for multilevel cervical spondylotic myelopathy: a prospective randomized control clinical study. Eur Spine J 2010;19:713–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Lu X, Peng H, Ling S, et al. Comparison of microendoscopic discectomy with open discectomy for degenerative lumbar spinal stenosis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2009;23:1200–3. [PubMed] [Google Scholar]
- [30].Rodriguez-Vela J, Lobo-Escolar A, Joven-Aliaga E, et al. Perioperative and short-term advantages of mini-open approach for lumbar spinal fusion. Eur Spine J 2009;18:1194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]


