Supplemental Digital Content is available in the text
Keywords: gastrodin injection, hypertension, meta-analysis, systematic review
Abstract
Background:
Hypertension is a common chronic disease and poses a huge burden to health care systems. Recent studies have shown that gastrodin injection (GI) has a potential supplementary therapeutic effect on hypertension.
Objectives:
To systematically assess the efficacy and safety of GI in treatment of hypertension.
Methods:
Systematic search was conducted on 7 databases (PubMed, Cochrane Library, Embase, Wanfang database, China biomedical literature service system, VIP Chinese Sci-tech journal database and China national knowledge internet). The retrieval time was from the establishment of database to February 15, 2020. Two researchers independently selected literature, extracted data and evaluated the risk of bias in the study. The methodological quality was evaluated with Cochrane handbook. The meta-analysis was performed with Stata 14.0 software.
Results:
Thirteen studies were included in this study involving 1525 patients. Compared with using conventional therapy alone, GI combined with conventional therapy can decrease systolic blood pressure (weighted mean difference [WMD] −6.67, 95% confidence interval [CI]: −10.30, −3.04. number of estimates [k] = 9, I2 = 89.3%), diastolic blood pressure (WMD −4.52, 95% CI: −7.79, −1.26. k = 9, I2 = 92.3%), and improve the clinical efficacy (relative risk [RR] 1.18, 95% CI: 1.10, 1.26. k = 6, I2 = 12.6%).
Conclusions:
The current evidence showed that GI combined with conventional therapy can improve systolic blood pressure, diastolic blood pressure and clinical efficacy. GI can become a supplementary treatment for hypertension.
1. Introduction
Hypertension is one of the most common cardiovascular diseases and has become a huge threat to human health.[1] According to the 2012 World Health Statistics report, one-third of the worlds adults were suffering from hypertension, contributing to about half of the total deaths caused by stroke and heart diseases.[2] The pathobiology of hypertension is complex, including imbalance of renin-angiotensin-aldosterone system (RAAS), excessive sodium, dysfunction of vascular endothelial function, increase of blood viscosity, and many other mechanisms.[3] Among them, angiotension II (Ang II) has a strong contractive effect on blood vessels and is a main factor for the maintenance and deterioration of hypertension.[4] Endothelin (ET) can increase the flow of Ca2+, thus enhancing the pressor effect of other vasoconstrictors and reducing the synthesis of nitric oxide (NO), and destroy the antagonistic effect of both on maintaining the basic tension of blood vessels, which promotes the development of hypertension.[5] Several kinds of antihypertension medications have been proved to have therapeutic effects of lowering the blood pressure (BP). However, some patients still had serious side effects and did not have a good response to the existing conventional therapy. There is a demand to find an alternative therapy that may benefit these patients.
In recent years, traditional Chinese medicine (TCM) has shown a unique role in the treatment of hypertension.[6–9] According to the theory of TCM, hypertension usually belongs to vertigo and headache.[6,10] Gastrodin is the extract of Gastrodia elata, a famous TCM, which has the functions of stopping spasm caused by wind, calming the liver-yang, removing wind, and dredging collaterals and it is mainly used to treat dizziness and headache.[11] Modern pharmacological researches show that GI can improve the function of vascular endothelial cells, inhibit the stimulation of sympathetic nervous system and reduce the level of Ang II, aldosterone (ALD), and angiotensin type 1 receptor (AT1R) so as to intervene the RAAS to reduce BP.[12–15] It can also antagonize the vasoconstriction effect of catecholamine transmitters, non-competitively antagonize the potential dependent calcium channels and receptor-operated calcium channels and prevent the influx and release of Ca2+, leading to vasodilation and lowering BP.[14] In the past decades, numerous clinical studies using GI as a supplementary treatment to cure hypertension reported good effects.[12,16–27] However, there were differences in the results of related clinical trials. We collected all relevant available studies to carry out the meta-analysis. The main purpose of this study is to assess the efficacy and safety of GI combined with conventional therapy on hypertension.
2. Materials and methods
2.1. Search strategy and study eligibility
Our systematic review and meta-analysis was undertaken according to the PRISMA guidelines.[28] All analyses were based on previous published studies, thus no ethical approval and patient consent were required. We searched the following databases for relevant studies from the establishment date of the database to February 15, 2020: PubMed, Cochrane Library, Embase, Wanfang database, China biomedical literature service system, VIP Chinese Sci-tech journal database and China national knowledge internet. And we collected randomized controlled trials (RCTs) of GI combined with conventional therapy for hypertension. The search terms employed were as follows: (“gastrodin’” OR “gastrodine” OR “Tianxuanqing”) AND (“Hypertension, Essential” OR “Essential Hypertension” OR “Primary Hypertension” OR “Hypertension” OR “EH” OR “Blood pressure”), along with a combination of MeSH indexing approaches. There was no language limitation. At the same time, we also screened the references of the included articles to ensure that we can retrieve the relevant articles more comprehensively.
2.2. Inclusion/exclusion criteria
Studies that met the following criteria were included:
-
1.
RCTs on hypertensive patients;
-
2.
Conventional treatment as intervention measures in control group, GI plus conventional treatment as intervention measures in combination group;
-
3.
At least 1 of the relative outcomes or adverse effect was reported.
Systolic blood pressure (SBP), diastolic blood pressure (DBP), and clinical efficacy were primary outcomes. ET, NO, and pulse pressure difference (PP) were secondary outcomes. When multiple publications reporting data from the same trial were available, only the study with the largest sample size was included. Single case reports, animal studies and studies of basic science were not included. Language was not restricted in this meta-analysis to minimize the publication bias.
2.3. Data extraction and bias/quality assessment
Two investigators reviewed the literature, extracted data and evaluated them independently. When there were disagreements, the decision was made by discussion or consultation to a third investigator. Information including author, year of publication, patients characteristics, intervention measures, intervention period, outcomes (DBP, SBP, clinical efficacy, ET, NO, PP) and adverse reactions were retreived from each study. The corresponding author of the original study was contacted by email when the data was incomplete or there was any uncertainty in the publications. We used the “risk of bias” evaluation tool in Cochrane Handbook to evaluate the quality of included studies, including the following aspects: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome date, selective reporting, and bias from other sources. Each of these aspects was evaluated separately and the following categories were used by us: low risk, high risk, and unclear.
2.4. Analysis
Relative risk (RR) and its 95% confidence interval (CI) were used to represent the curative effect analysis statistics for count data, and the weighted mean difference (WMD) and its 95% CI were used as the analysis statistic to represent continuous changes. We extracted RRs, WMDs and those 95% CIs from the publications, where available. When necessary, we calculated WMDs/CIs from original study data provided in the publication. We used I2 statistics and P value to evaluate the level of heterogeneity between the included studies. When I2 > 50% or P < .05, we chose the random effect model. Otherwise, the fixed effect model was chosen. Subgroup analyses were conducted to explore the potential sources of heterogeneity. Sensitivity analyses were conducted by removing each estimate one at a time and recalculating the pooled estimates to detect potential outliers. Funnel plots and Egger tests were used to determine whether there was publication bias. Meta-analysis was undertaken with Stata 14.0 software.[29]
3. Results
3.1. Search results and study characteristics
A total of 370 related literatures meeting the inclusion criteria were enrolled for the initial examination. 249 duplications were excluded. Then 121 related literatures were carefully reviewed by reading their titles and abstracts. Sixty eight articles further were excluded because of the following reasons: duplicate studies (n = 8), case reports (n = 9), animal experiments (n = 23), conference abstracts (n = 8), and pharmacokinetic studies (n = 20). The full text of the remaining 53 articles were reviewed and 40 of them were further excluded because of the following reasons: outcome measures did not meet the inclusion criteria (n = 32), other documents (n = 8). A total of 13 RCTs[12,16–27] containing 1525 patients were included in the final meta-analysis. The process and results of literature screening are shown in Figure 1. There are 766 patients in the combination group while 759 patients in control group. All of these trials were carried out in the hospitals of China. Included studies were published between 2004 and 2019. The sample sizes ranged from 63 to 220. Durations of the interventions ranged from 2 weeks to 3 months. The conventional therapy of the included studies included amlodipine, valsartan, benazepril, levamlodipine besylate, nifedipine, etc. The basic characteristics of the included studies are shown in Table 1. The quality of the included studies was relatively low. The assessment of bias risk and quality is shown in Figures 2 and 3.
Figure 1.
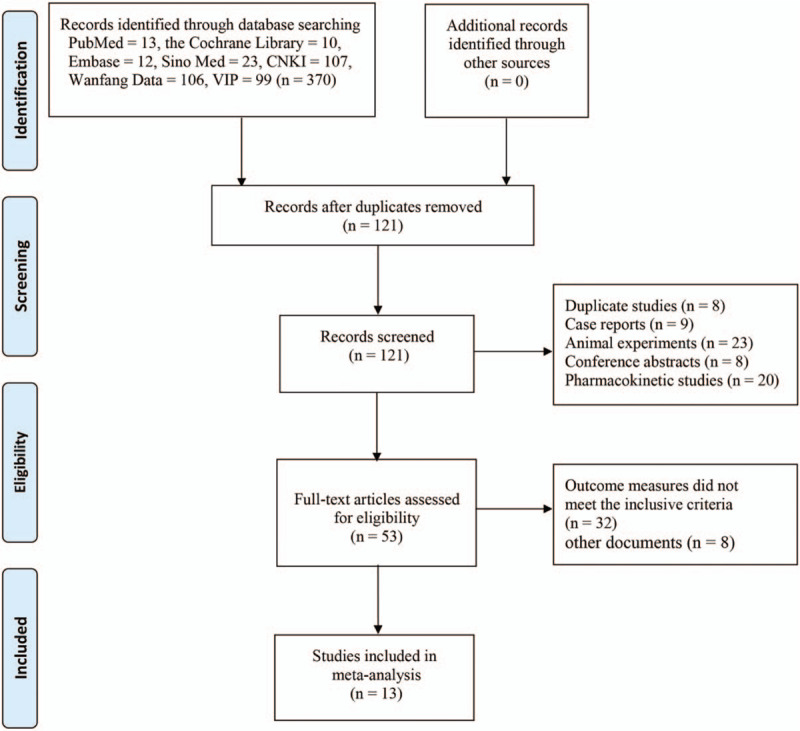
Flow-process diagram of literature retrieval.
Table 1.
Characteristics of 13 studies fulfilling the inclusion criteria.
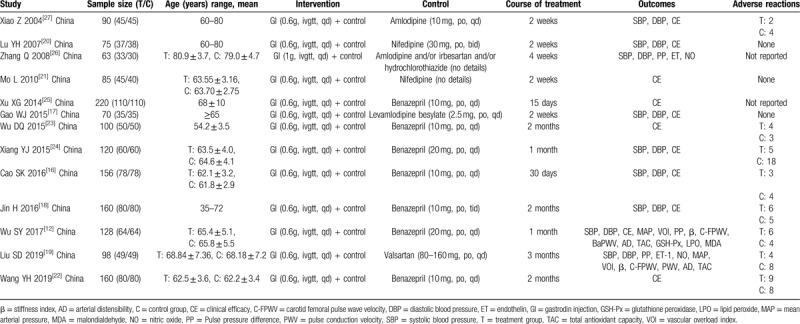
Figure 2.
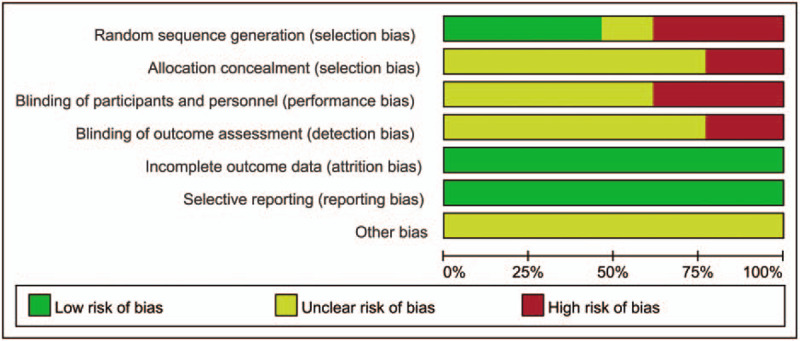
Risk of bias.
Figure 3.
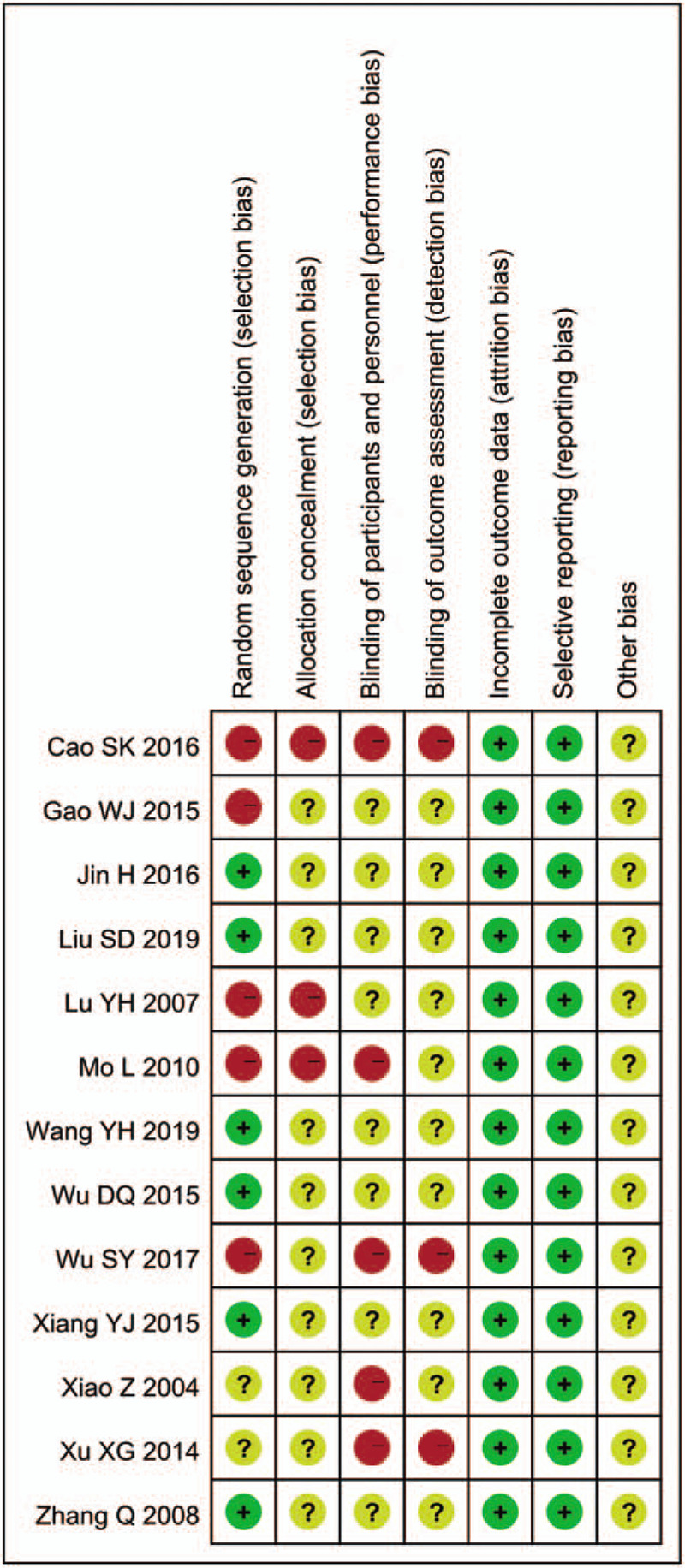
Risk of bias summary and graph.
3.2. Primary outcome measures
3.2.1. Systolic blood pressure (SBP, mm Hg)
Nine studies[12,16–20,24,26,27] involving 992 participants reported the results of SBP in patients with hypertension. Six of them[12,16–19,24] found GI plus conventional treatment had a significant decrease of SBP in patients with hypertension while the remaining 3 of them[20,26,27] reported non-significant association. The meta-analysis indicated that GI combined with conventional therapy had a significant reduction of SBP compared with using conventional therapy alone in patients with hypertension (WMD −6.67, 95% CI: −10.30, −3.04. number of estimates [k] = 9, I2 = 89.3%, Figure 4).
Figure 4.
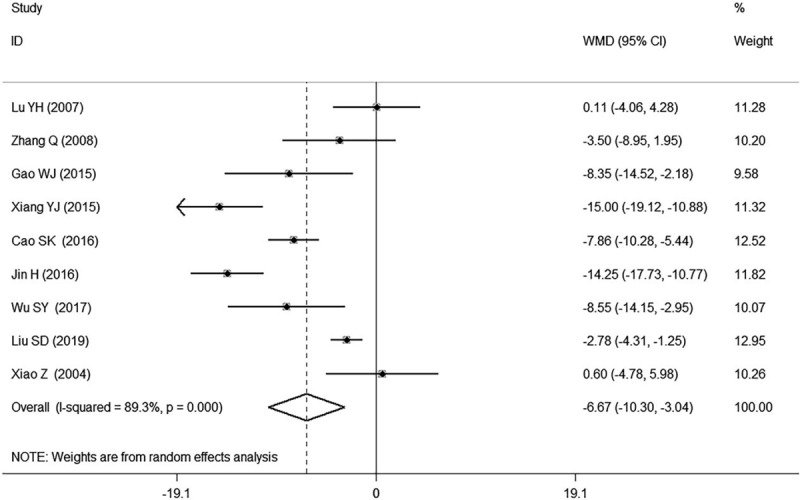
Forest plot of SBP of GI combined with conventional therapy vs conventional therapy.
3.2.2. Diastolic blood pressure (DBP, mm Hg)
Nine studies[12,16–20,24,26,27] reported the results of the DBP. Six of them[12,16–19,24] found GI plus conventional treatment had a significant decrease of DBP in patients with hypertension while the remaining 3 of them[20,26,27] reported non-significant association. The meta-analysis indicated that GI combined with conventional therapy had a significant reduction of DBP compared with using conventional therapy alone in patients with hypertension (WMD −4.52, 95% CI: −7.79, −1.26. k = 9, I2 = 92.3%, Fig. 5).
Figure 5.
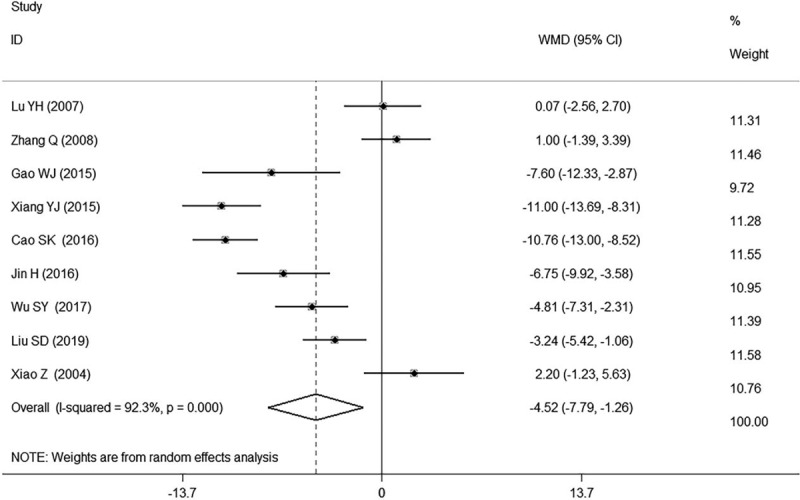
Forest plot of DBP of GI combined with conventional therapy vs conventional therapy.
3.3. Clinical efficacy
A total of 6 studies[16,18,20,24,25,27] reported the results of the total effective rate of lowing BP, involving 821 patients (410 in the combination group and 411 in the control group). Four of them[16,18,24,25] found GI plus conventional treatment had a significant increase of clinical efficacy in patients with hypertension while the remaining 2 of them[20,27] reported non-significant association. Our meta-analysis indicated that GI combined with conventional therapy had a significant increase of clinical efficacy compared with using conventional medicine alone in patients with hypertension (RR 1.18, 95% CI: 1.10, 1.26. k = 6, I2 = 12.6%, Fig. 6).
Figure 6.
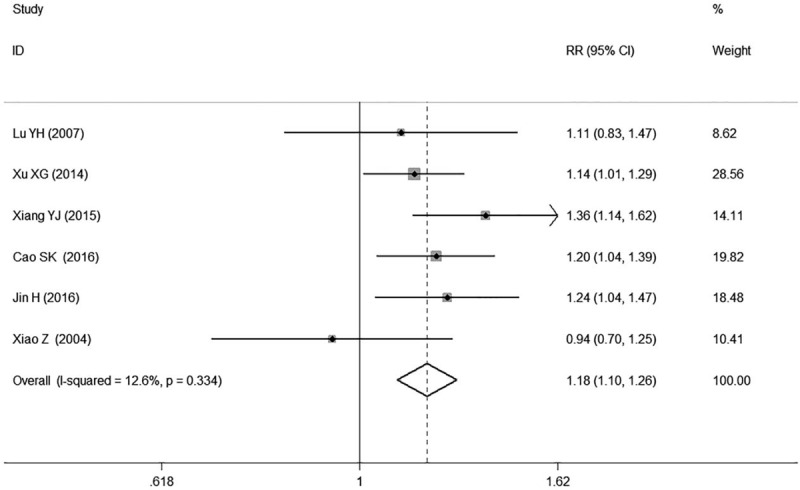
Forest plot of clinical efficacy of GI combined with conventional therapy vs conventional therapy.
3.4. Subgroup analysis
In subgroup analysis for different durations of treatment, the results showed a non-significant difference in SBP, DBP and clinical efficacy between the combination treatment group and the control group at the 2-week follow-up time point (SBP: WMD −2.21, 95% CI: −7.36, 2.93. k = 3, I2 = 66.0%; DBP: WMD −1.46, 95% CI: −6.26, 3.34. k = 3, I2 = 82.2%; clinical efficacy: RR 1.09, 95% CI: 0.98, 1.21. k = 3, I2 = 0.0%, Table 2, Supplemental Digital Content Figs. S1, S3 and S5). However the combination treatment showed a significant reduction in SBP, DBP, and clinical efficacy when the observation time was more than 4 weeks (SBP: WMD −8.63, 95% CI: −13.13, −4.14. k = 6, I2 = 91.8%; DBP: WMD −5.91, 95% CI: −9.72, −2.09. k = 6, I2 = 92.9%; clinical efficacy: RR 1.26, 95% CI: 1.14, 1.38. k = 3, I2 = 0.0%, Table 2, Supplemental Digital Content Figs. S1, S3, and S5).
Table 2.
Subgroup analyses of SBP, DBP and clinical efficacy.
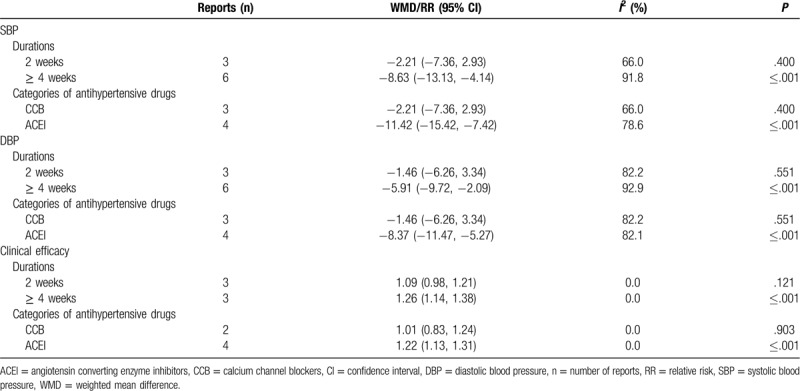
In subgroup analysis for different types of antihypertensive drugs, the results showed a non-significant difference in SBP, DBP, and clinical efficacy between the combination group and the control group with calcium channel blockers (CCB) (SBP: WMD −2.21, 95% CI: −7.36, 2.93. k = 3, I2 = 66.0%; DBP: WMD −1.46, 95% CI: −6.26, 3.34. k = 3, I2 = 82.2%; clinical efficacy: RR 1.01, 95% CI: 0.83, 1.24. k = 2, I2 = 0.0%, Table 2, Supplemental Digital Content Figs. S2, S4, and S6). However, the combination treatment showed a significant reduction in SBP, DBP and clinical efficacy with angiotensin converting enzyme inhibitors (ACEI) (SBP: WMD −11.42, 95% CI: −15.42, −7.42. k = 4, I2 = 78.6%; DBP: WMD −8.37, 95% CI: −11.47, −5.27. k = 4, I2 = 82.1%; clinical efficacy: RR 1.22, 95% CI: 1.13, 1.31. k = 4, I2 = 0.0%, Table 2, Supplemental Digital Content Figs. S2, S4, and S6).
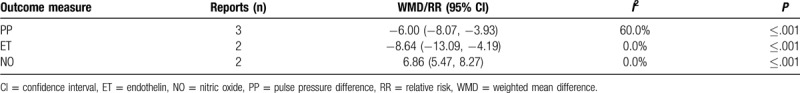
3.5. Secondary outcome measures
Three of studies[12,19,26] found GI plus conventional treatment had a significant decrease of PP in patients with hypertension (WMD −6.00, 95% CI: −8.07, −3.93. k = 3, I2 = 60.0%, Table 3 and Supplemental Digital Content Fig. S7). Two of studies[19,26] found GI plus conventional treatment had a significant decrease of ET (WMD −8.64, 95% CI: −13.09, −4.19, k = 2, I2 = 0.0%, Table 3 and Supplemental Digital Content Fig. S8) and a significant increase of NO in patients with hypertension (WMD 6.86, 95% CI: 5.45, 8.27. k = 2, I2 = 0.0%, Table 3 and Supplemental Digital Content Fig. S9).
Table 3.
Meta-analyses of secondary outcome measures.
3.6. Safety
Eleven of the included studies reported adverse events.[12,16–24,27] There were 8 cases of digestive tract reaction, 8 cases of nausea and vomiting, 8 cases of cough, 6 cases of flushing, 5 cases of rash, 4 cases of nausea and vomiting, 4 cases of vertigo, 4 cases of asthenia, 3 cases of cough, 2 cases of mild edema of ankle, 2 cases of lower extremity edema, and 1 case of headache in combination therapy groups. There were 13 cases of vertigo, 11 cases of flushing, 6 cases of digestive tract reaction, 4 cases of asthenia, 2 cases of flushing, and 2 cases of mild ankle edema in control groups. Three studies[17,20,21] reported that there were no adverse events related to combination therapy. The remaining 2[25,26] did not report adverse events in their studies. All these symptoms were relieved after symptomatic treatment and did not affect the implementation of the trials.
3.7. Sensitivity analysis and publication bias
We found high heterogeneity according to the test for heterogeneity of SBP and DBP (SBP: I2 = 89.3%, DBP: I2 = 92.3%, Figs. 4 and 5), and the random effect model was used. The heterogeneity in the results of clinical efficacy was low (I2 = 12.6%, Fig. 6), and fixed effect model was used. We used the sensitivity analyses to judge the stability of the results and 1 study[16] for DBP had some effect on the pooled association estimate (Supplemental Digital Content Figs. S10, S11, and S12). Funnel plots and Egger tests were used to determine the publication bias, and no publication bias was found (Egger tests: SBP: P = 0.420, DBP: P = 0.916, clinical efficacy: P = 0.500, Supplemental Digital Content Table S1, Figs. S13, S14, and S15).
4. Discussion
This meta-analysis found that the level of SBP, DBP, PP, and ET in patients treated with combination therapy were significantly lower than those in patients treated with conventional therapy alone, and the clinical efficacy and level of NO was significantly higher in patients treated with combination therapy when compared with patients in the control group. This meta-analysis suggested that GI can be an effective supplementary treatment for hypertension.
Different antihypertensive drugs decrease the BP through different mechanisms (eg, reducing blood volume, inhibiting blood flow, inhibiting RAAS, blocking Ca2+ flow, reducing peripheral resistance, etc.).[30] Although modern medications have certain curative effects in the treatment of hypertension, the symptoms in some patients still cannot be relieved to a satisfying level. Our finding indicated GI combined with conventional medicine had positive effects on lowering the BP in patients with hypertension. Gastrodin is the extract of Gastrodia elata. It has the effect of calming wind, reducing BP, clearing heat, activating blood circulation, and calming nerves in the theory of TCM.[11] GI can regulate the BP through inhibiting RAAS system and preventing the influx and release of Ca2+.[14,15] It indicated the combination of GI with conventional therapy may have a synergistic effect through above mechanisms.
In subgroup analyses for different intervention durations, we found that the treatment course longer than 4 weeks can lead to a significant reduction of BP. Hypertension is a chronic disease with complex etiologies and it usually takes a certain course before the treatment come into effect. The synergistic effect of GI combined with conventional treatment may accumulate with time. In subgroup meta-analysis for GI combined with different types of antihypertensive drugs, we found that patients using GI combined with ACEI had a significant reduction in BP. It has been reported[12,14,15,31] that gastrodin can inhibit the stimulation of sympathetic nervous system, reduce the concentration of serum AngII, ALD, and AT1R so as to effectively inhibit the RAAS and peroxisome proliferator-activated receptor γ to reduce the BP. Chen HH reported[32] gastrodin can decrease the levels of superoxide dismutase and malondialdehyde, protect the vascular through reducing lipid peroxidation injury and reduce BP in hypertensive rats. GI can also improve the hemodynamic state, protect the function of vascular endothelial cells, inhibit the synthesis of endothelin and dilate vessels. All of the above mentioned mechanisms work together to reduce BP.[13,33,34] ACEI is one of the commonly used antihypertensive drugs. It can reduce BP by affecting RAAS. It can reduce the production of Ang II, inhibit sympathetic excitation, and regulate the function of vascular endothelium. The combination of GI and ACEI may produce a synergistic effect of lowering the BP through these mechanisms. The conventional medications reported in the included studies only cover CCB, ACEI, and ARB. The effects of GI combining with other categories of conventional medications (eg, beta blockers or diuretics or renin inhibitors) are unclear. Studies including more types of antihypertensive drugs with large samples are needed to supply our findings.
Our meta-analysis indicated GI plus conventional treatment had a significant decrease of ET and increase of NO in patients with hypertension. ET can increase the flow of Ca2+ and reduce the synthesis of NO to promote the occurrence and development of hypertension.[4] Modern pharmaceutical studies have shown that GI can decrease the BP by protecting the function of vascular endothelial cells and inhibiting the synthesis of ET.[13,33,34] The results of this study suggested that the antihypertensive effect of GI may be achieved by inducing vasodilatation and balancing the plasma levels of NO and ET and intervening the RAAS.[33,35–37]
There were some limitations in the meta-analysis. The sample size of the included studies was generally small. Medications used in the conventional therapy of the included studies only include CCB, ACEI, ARB and the effect of GI combined with other conventional therapy are unclear. More types of antihypertensive drugs are needed to make the finding more generally applicable. The quality of the included studies is relatively low, therefore careful cautions should be paid in interpretation of the results. The types of intervention methods and the length of intervention time were not uniform, which may affect the general applicability of the results.
5. Conclusions
Our meta-analysis indicated that GI combined with conventional therapy can reduce BP, improve endothelial function and clinical symptoms of patients with hypertension. It can improve the quality of life and extend the lifetime of patients with hypertension.
Author contributions
Conceptualization: Lichao Qian, Zhuyuan Fang.
Data curation: Shihai Yan, Yizhuo Li.
Formal analysis: Lihua Wu, Yawei Zheng, Yixuan Wang.
Project administration: Lichao Qian, Zhuyuan Fang.
Supervision: Zhuyuan Fang, Shihai Yan.
Writing – original draft: Lichao Qian.
Writing – review & editing: Yizhuo Li, Shihai Yan.
Supplementary Material
Footnotes
Abbreviations: ACEI = angiotensin converting enzyme inhibitor, ALD = aldosterone, Ang II = angiotension II, AT1R = angiotensin type 1 receptor, BP = blood pressure, CI = confidence interval, DBP = diastolic blood pressure, ET = endothelin, GI = gastrodin injection, k = number of estimates, NO = nitric oxide, PP = pulse pressure difference, RAAS = renin-angiotensin-aldosterone system, RCTs = randomized controlled trials, RR = relative risk, SBP = systolic blood pressure, TCM = traditional Chinese medicine, WMD = weighted mean difference.
How to cite this article: Qian L, Yan S, Li Y, Wu L, Zheng Y, Wang Y, Fang Z. The effects of gastrodin injection on hypertension: a systematic review and meta-analysis. Medicine. 2020;99:27(e20936).
LQ, SY, and YL contributed equally to the paper.
This study was supported by National Natural Science Foundation of China (81873258), Postgraduate Research & Practice Innovation Program of Jiangsu Province (KYCX20_1477 and KYCX20_1455), Jiangsu Province “333 Talents Project” (2018-III-2195), Jiangsu Province “Six Talents Peak” Project (2016-WSN-057), Scientific Research Projects of Jiangsu Administration of Traditional Chinese Medicine (JD201805). The Open Projects of the Discipline of Chinese Medicine of Nanjing University of Chinese Medicine Supported by the Subject of Academic priority discipline of Jiangsu Higher Education Institutions (NO. ZYX03KF073).
The authors state that the study was conducted without any commercial or financial relationship.
Supplemental Digital Content is available for this article.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Touyz RM. Hypertension guidelines: effect of blood pressure targets. Can J Cardiol 2019;35:564–9. [DOI] [PubMed] [Google Scholar]
- [2].New WHO statistics show that the incidence rate of hypertension and diabetes is increasing. China's Gen Pract 2012;15:2844. [Google Scholar]
- [3].Htoo PT, Stürmer T, Jonsson-Funk M, et al. Renin-angiotensin-aldosterone system-based antihypertensive agents and the risk of colorectal cancer among medicare beneficiaries. Epidemiology 2019;30:867–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].He WJ, Li CW, Rao DC, et al. Associations of renin-angiotensin-aldosterone system genes with blood pressure changes and hypertension incidence. Am J Hypertens 2015;28:1310–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Palmer JC, Tayler HM, Dyer L, et al. Zibotentan, an endothelin a receptor antagonist, prevents amyloid-(-induced hypertension and maintains cerebral perfusion. J Alzheimers Dis 2020;73:1185–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Dong HY, Zhang SQ, Du WX, et al. Pharmacodynamics and metabonomics study of Tianma Gouteng Decoction for treatment of spontaneously hypertensive rats with liver-yang hyperactivity syndrome. J Ethnopharmacol 2020;253:112661. [DOI] [PubMed] [Google Scholar]
- [7].Zhang L, Cai QY, Lin S, et al. Prevention of systemic inflammation and neuroprotective effects of Qingda granules against angiotensin II-mediated hypertension. Pak J Pharm Sci 2020;33:469–79. [PubMed] [Google Scholar]
- [8].Liu TH, Chen WH, Chen XD, et al. Network pharmacology identifies the mechanisms of action of TaohongSiwu decoction against essential hypertension. Med Sci Monit 2020;26:e920682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Tai J, Zou J, Zhang X, et al. Randomized controlled trials of tianma gouteng decoction combined with nifedipine in the treatment of primary hypertension: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2020;2020:5759083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Tian H, Zhang DS. Research progress of neuroprotective mechanism of gastrodin. J Neuropharmacol 2013;3:58–64. [Google Scholar]
- [11].Liu X. Using traditional Chinese medicine theory, modern pharmacological research and clinical thinking to learn and use Gastrodia elata. Inner Mongolia Trad Chin Med 2008;1:62–5. [Google Scholar]
- [12].Wu SY. Effects of gastrodin injection combined with RAAS inhibitor on arterial elasticity, vascular overload index and oxidation antioxidant system in elderly patients with essential hypertension. J Mod Chin West Med 2017;26:3242–5. [Google Scholar]
- [13].Chen WK. Pharmacological action and clinical application progress of gastrodin injection. Strait Pharmaceut J 2012;24:13–6. [Google Scholar]
- [14].Li S, Xia H, Liu ZB, et al. Research progress of Gastrodin in cardiovascular and cerebrovascular diseases. Res Pract Mod Chin Med 2019;33:76–81. [Google Scholar]
- [15].Liu W, Wang LY, Yu JH, et al. Gastrodin reduces blood pressure by intervening with RAAS and PPAR (in SHRs). Evid Based Complement Alternat Med 2015;2015:828427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cao SK. Therapeutic effect of gastrodin injection combined with benazepril on hypertension. Med Theory Pract 2016;29:3040–2. [Google Scholar]
- [17].Gao WJ, Xiong XL. Gastrodin injection in the treatment of 70 cases of senile hypertension vertigo. Sichuan Trad Chin Med 2015;33:113–5. [Google Scholar]
- [18].Jin H. Therapeutic effect of gastrodin injection combined with benazepril on hypertension. Guangming Trad Chin Med 2016;31:1427–9. [Google Scholar]
- [19].Liu SD, Wang JR, Huang JJ. Therapeutic effect of Gastrodin Injection on elderly patients with refractory hypertension. Contemp Med Rev 2019;13:129–30. [Google Scholar]
- [20].Lu YH. Clinical observation of gastrodin injection combined with Nifedipine in the treatment of senile hypertension. J Pract Med Technol 2007;14:1432–4. [Google Scholar]
- [21].Mo L. 45 cases of hypertension vertigo treated with gastrodin injection. Guangxi Trad Chin Med 2010;33:16–7. [Google Scholar]
- [22].Wang YH. Observation on the efficacy and adverse reactions of gastrodin injection combined with benazepril in the treatment of hypertension. Chin Med Guidelines 2019;17:157. [Google Scholar]
- [23].Wu DQ. Analysis of the effect of gastrodin injection combined with benazepril in the treatment of hypertension. Contemp Med Rev 2015;13:155–6. [Google Scholar]
- [24].Xiang YJ. Therapeutic effect observation of gastrodin injection combined with benazepril on hypertension. J Mod Integr Chinese Western Med 2015;24:3490–1. [Google Scholar]
- [25].Xu XG. Curative effect of gastrodin injection combined with benazepril in the treatment of hypertension. Chin J Integr Chin West Med 2014;21:314. [Google Scholar]
- [26].Zhang Q, Yang YM. Effects of gastrodin injection on blood pressure and vasoactive substances in treatment of old patients with refractory hypertension: a randomized controlled trial. Zhong Xi Yi Jie He Xue Bao 2008;6:695–9. [DOI] [PubMed] [Google Scholar]
- [27].Xiao Z, Wan QN. Clinical observation of gastrodin injection in the treatment of elderly hypertension. J Yunnan Univ Trad Chin Med 2004;27:38–41. [Google Scholar]
- [28].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Melsen WG, Bootsma MC, Rovers MM, et al. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect 2014;20:123–9. [DOI] [PubMed] [Google Scholar]
- [30].Weng YJ, Li WD. Research progress of antihypertensive drugs. China Pharmaceut 2014;23:94–6. [Google Scholar]
- [31].Li Y, Wang ZW, Geng YL, et al. Research progress on pharmacological mechanism and clinical application of gastrodin injection. Chin Pharmacy 2016;27:4602–4. [Google Scholar]
- [32].Chen HH, Huang T, Liu H. Effects of gastrodin on blood pressure change, vascular protection and oxidative stress response mechanism in hypertensive rats. World J Trad Chin Med 2016;11:2385–8. [Google Scholar]
- [33].Xiao ZY, Li G, Liu QM, et al. Clinical observation of gastrodin injection combined with transcranial magnetic stimulation for vertebrobasilar insufficiency vertigo. Chin Med Emerg 2014;24:1532–4. [Google Scholar]
- [34].Zhang ZX, Cao KG, Wang CD, et al. Effects of gastrodin on neuropeptide and nitric oxide system in rats with vasomotor abnormalities induced by dopamine and nitroglycerin. Chin J Trad Chin Med 2013;31:1514–7. [Google Scholar]
- [35].Liao HT, Tang QP, Zhang X, et al. Research progress in the protection of endothelial cells by traditional Chinese medicine monomer against atherosclerosis. Chin J Basic Med Trad Chin Med 2019;25:1619–22. [Google Scholar]
- [36].Yang S, Ma CR, Wu H, et al. Tectorigenin attenuates diabetic nephropathy by improving vascular endothelium dysfunction through activating AdipoR1/2 pathway. Pharmacol Res 2020;153:104678. [DOI] [PubMed] [Google Scholar]
- [37].Luo LX, Wang T, Sun LJ. Research progress of Gastrodia elata in the treatment of hypertension. J Cardio Cerebrovasc Dis Integr Chin West Med 2014;12:1392–3. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


