Abstract
Background:
At present, accumulative attention has been paid to coronavirus disease 2019 (COVID-19) due to its global prevalence. Acupuncture may play a beneficial role in patients with breathlessness in COVID-19. This study is designed to determine the efficacy and safety of acupuncture for breathlessness in COVID-19.
Methods:
Randomized controlled trials (RCT) will be searched from 7 electronic databases, with the last search update being 30 June 2020. Studies by registers of clinical trials will be additionally searched. Two investigators will independently select studies, extract data and evaluate study quality. Finally, a meta-analysis will be used to evaluate the pooled intervention effect if possible.
Results:
Our present findings will indicate the application of acupuncture as an adjunctive treatment for dyspnea in COVID-19, which will be published in a peer-reviewed journal.
Conclusion:
Our study will provide a reference foundation for clinical optimization of treatment.
Prospero registration number:
CRD42020182323.
Keywords: acupuncture, COVID-19, protocol, randomized controlled trials, systematic review
1. Introduction
Coronaviruses (CoVs) is a type of enveloped positive-sense RNA virus that is diversely found in humans and wildlife.[1] Human coronaviruses (HCoVs) have been proven to be non-essential pathogens for a long period, which can result in “common cold” in other healthy population.[1,2] Nevertheless, two highly pathogenic HCoVs from animal reservoirs have led to worldwide pandemics with striking morbidity and mortality, including severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV).[2] At present, a new strain called the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus has become another outbreak. The coronavirus disease 2019 (COVID-19) was recognized in Wuhan, China in December, 2019, causing increasing morbidity and mortality ever since.[2] The ongoing COVID-19 pandemic is an exceptional challenge for the health systems throughout the world. Through the continuous accumulation of research data, the biological, epidemiological, and clinical characteristics of COVID -19 have been gradually improved. International attention has been paid to COVID-19 due to the quickly increasing number of diagnosed patients along with subsequently rising secondary outbreaks in various global regions. Hopefully, the rapid in-depth sequencing of viral genomes has enabled the development and research of diagnostic tests, as well as the initiation of vaccine and therapeutics research.[3] However, so far, no effective vaccine or causative therapy is available.[3] Existing studies have readily confirmed the interpersonal transmission of SARS-CoV-2,[3,4] with an incubation period varying from 1 to 14 days (median: 5–6 days), which could be 24 days under extreme conditions.[3,5] Additionally, patients with COVID-19 have a higher proportion of men, the elderly, patients with hypertension and/or diabetes.[6] There are also investigations concerning the risk factors as well as clinical outcomes in admission and intensive care unit. In an early study of patients with COVID-19 in China and Italian, older men, patients with smoking and cardiometabolic diseases were associated with poor prognosis.[7] In general, the clinical presentation of COVID-19 includes myalgias, fatigue dry cough and fever, as well as less common ones (including abdominal pain, breathlessness, headache diarrhea and sore throat).[3,8] A recent descriptive study found that there were 56.7% men among elderly diagnosed COVID-19 patients were male, and common symptoms included fatigue (23.3%), dyspnea (30.0%), cough (56.7%), and fever (78.3%).[8] In general, older population are more vulnerable to COVID-19 infection, and their mortality rate is higher, which deserves more attention.[8] The COVID-19 pandemic has triggered prevalent research interest in therapeutic and preventive interventions. However, due to the lack of specific antiviral therapeutics and vaccine, adjuvant therapy has become the major therapeutic strategy for COVID-19, along with the administration of corticosteroids, antivirals, broad-spectrum antibiotics and convalescent plasma.[9] At present, diverse trials have been launched, such as tocilizumab, losartan, hydroxychloroquine, remdesivir as well as convalescent plasma.[10]
Traditional Chinese medicine (TCM) plays an important role in the prevention and treatment of various infectious diseases. To be specific, the application of TCM has also obtained significant therapeutic efficacy during the SARS epidemic in 2003.[11] The combination of TCM and Western medicines could relieve symptoms, enhance life quality, absorb lung infiltration, while attenuate the corticosteroid dosage among SARS patients.[11] Similarly, recent clinical practice has also revealed the significant therapeutic effect of TCM in COVID-19.[12] China has issued guidelines for the diagnosis and treatment of COVID-19, recommending the use of conventional treatment methods plus TCM.[9,13] In the current Chinese medical system, licensed practitioners of TCM are allowed to prescribe western medicines after a formal course of study.[14] Therefore, the participation of TCM practitioners in the treatment of COVID-19 is legal and supported by the government. During the entire treatment period of COVID-19, Chinese medical staff volunteered to join the designated hospitals in Hubei Province,[12] who comprehensively adopted acupuncture, Chinese patent medicine, decoction and other characteristic therapies of TCM, shedding novel light on the control and prevention of COVID-19.[12] In total, 303 ongoing clinical trials concerning the assessment of the therapeutic safety and efficacy for COVID-19 patients have been launched in China by March 1, 2020, 50 of which focus on TCM, including 14 clinical trials aimed at evaluating the efficacy of TCM combined with Western medicine.[15] At present, there are various types of evidence for TCM treatment of COVID-19,[9,13,15] as shown in Figure 1.
Figure 1.
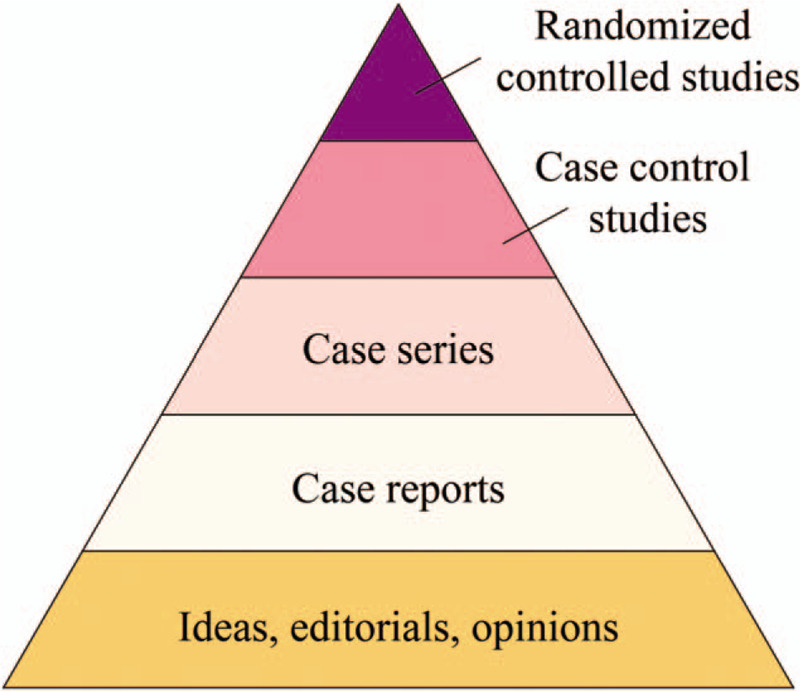
Types of current evidence on TCM treatment of COVID-19.
Acupuncture, a main component of TCM, has been widely adopted to treat respiratory diseases in clinical practice,[16,17] whose efficacy has been assessed by a number of randomized controlled trials (RTCs).[18] Breathlessness is one of the prevalent symptoms in COVID-19 patients.[8,19] Acupuncture may play a role in the prevention, treatment and rehabilitation of the COVID-19 and relieve the symptoms caused by COVID-19. Acupuncture has been demonstrated to effectively relieving common symptoms in supportive and palliative care, including anxiety disorders, nausea, insomnia, leukopenia, fatigue as well as vomiting,[20–25] which might also effectively treat abdominal pain and abdominal distension.[26,27] Coyle et al have proposed that acupuncture is an effective therapeutic approach for COPD-associated breathlessness.[28] Possible related symptoms of COVID-19 treated with acupuncture is shown as Figure 2. The recent systematic review and meta-analysis show that acupuncture can relieve breathlessness in subjects with advanced diseases.[16] Therefore, in this meta-analysis review, our goal is to systematically review the efficacy of acupuncture in relieving breathlessness, subsequently improving the physiological function and quality of life of patients with COVID-19 combined with dyspnea.
Figure 2.
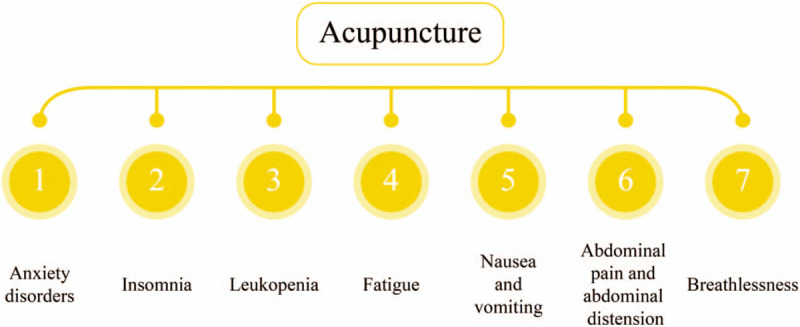
Possible related symptoms of COVID-19 treated with acupuncture.
2. Methods
The study will be conducted in accordance with the preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P).[29]
2.1. Inclusion criteria
2.1.1. Study type
Randomized controlled trials (RCTs) will be included in the review, without restriction on language or publication date.
2.1.2. Participant types
Patients with breathlessness due to lab-confirmed COVID-19 will be included, regardless of age, race, sex. Diagnosis of COVID-19 is based on the international or Chinese diagnostic criteria for COVID-19.[3,30,31]
2.1.3. Types of interventions
Acupuncture will be performed in the treatment group, combined with other treatments, including routine therapy and so on.[9] Patients in the control group will receive other therapeutic approaches other than acupuncture, including routine therapy, placebo, etc.
2.1.4. Types of outcomes
The primary outcomes include the changes on any subjective measurement of breathlessness severity made on a validated rating scale from baseline to endpoint, including visual analogue scale, numerical rating scale and the Borg Scale.[32,33]
Secondary outcomes include the assessment of quality of life activities using any validated questionnaire. In addition, anxiety will be evaluated by any validated scale. The safety of treatment will be assessed by the incidence and degree of adverse events.[34–36]
2.2. Search methods to identify studies
2.2.1. Search strategy
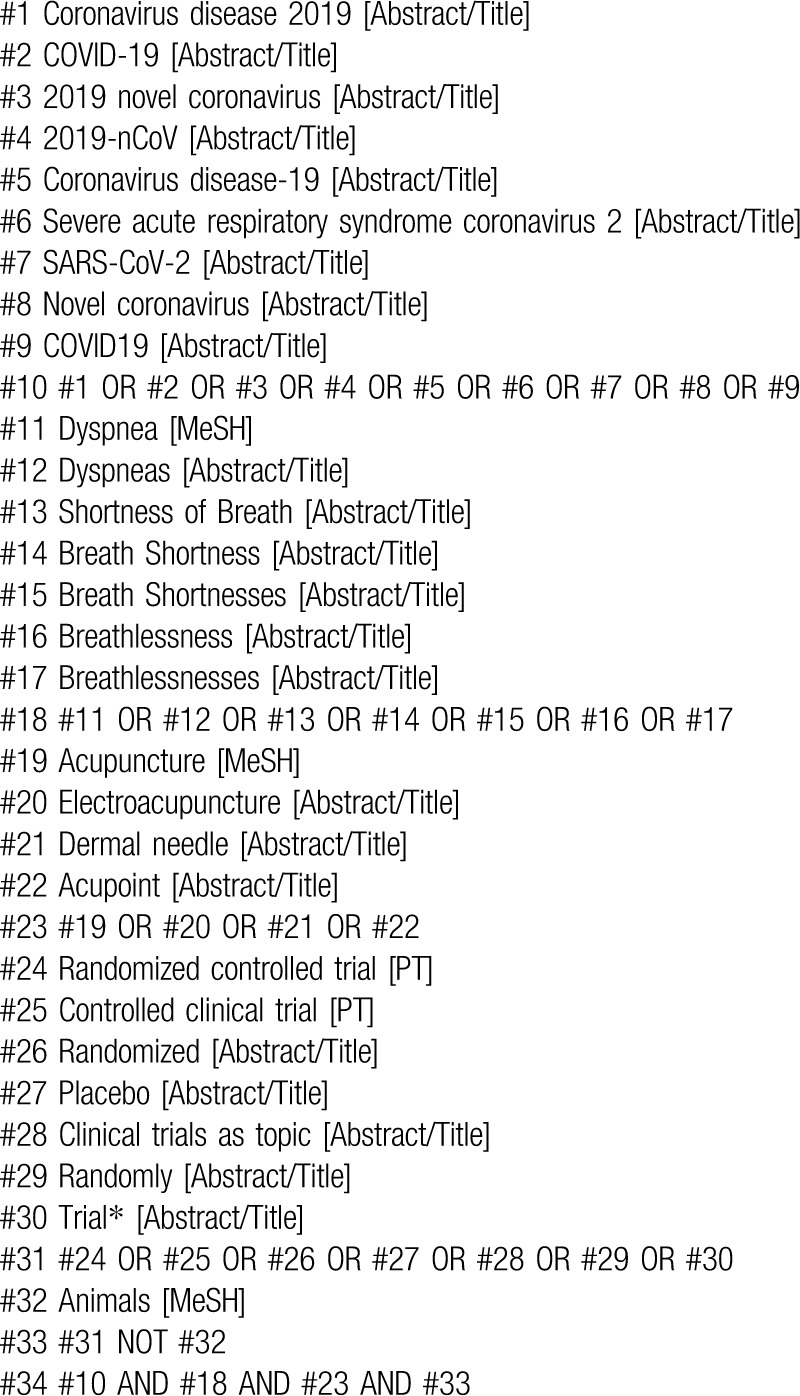
Two reviewers will independently search seven databases: EMBASE, Medline, Cochrane Central Register of Controlled Trials, Web of Science, Wan Fang Data, China National Knowledge Infrastructure as well as Chinese Scientific Journal Database (VIP) from inception until 30 June 2020 (search date). The same terms in China will be conducted in Chinese databases. The searching strategy for Medline is shown in Table 1.
Table 1.
Search strategy for Medline.
2.2.2. Searching other resources
Similar retrieval methods will be applied in the Clinical Trials.gov to obtain unpublished studies. There is no restriction on publication regions or language.
2.3. Data collection and analysis
2.3.1. Selection of studies
After searching studies, 2 investigators will review titles and abstracts, or full text if necessary. All investigators will reach agreement on the identification of study inclusion after evaluating their eligibility, and we will also record reasons why studies are eliminated. The selection process is summarized using PRISMA flow diagram. Details of the selection procedure for studies are shown in a PRISMA flow chart (Fig. 3). Any inconsistency is resolved by discussing with a third investigator.
Figure 3.
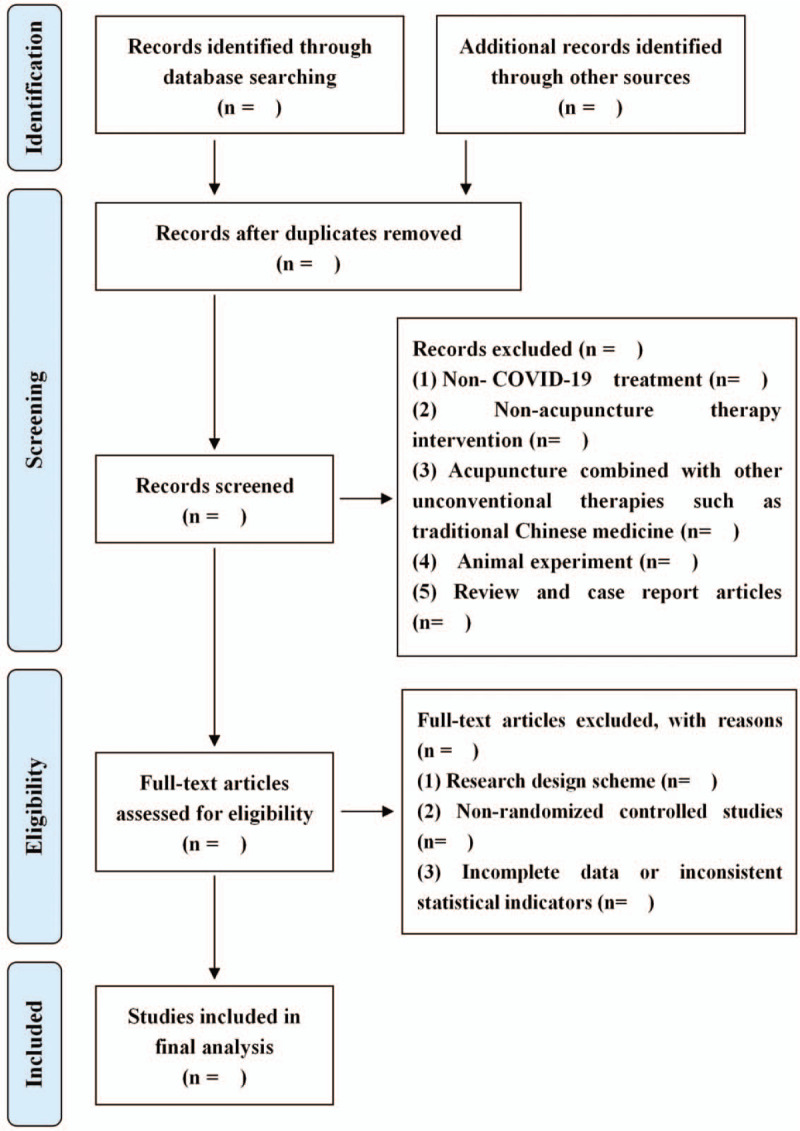
Study selection flow diagram.
2.3.2. Data extraction and management
Two investigators will extract relevant data independently, including study design, general information, characteristics of patients, comparison interventions, and outcomes. For articles with incomplete or uncertain data, the authors will be contacted for complete data. And the study will be further excluded without adequate information. If there is any dispute in the data extraction process, it will be submitted to a third researcher for processing.
2.3.3. Evaluation of bias risk in included studies
Two investigators will independently evaluate the bias risks among enrolled researches according to the Cochrane Collaboration.[37] Discrepancy will be resolved by discussion and judgment by an arbiter. The following seven aspects in all RCTs will be evaluated: outcome assessment blinding, participants and personnel blinding, selective outcome reporting, allocation concealment, inadequate outcome data, generation of random sequences as well as other potential sources of bias.[37] The bias risk in each aspect will be assessed and divided into 3 levels: low risk, high risk, and unclear risk.
2.3.4. Measurement of therapeutic effect
Review Manager (RevMan 5.3) software will be used for statistical analysis if a meta-analysis is allowed. Risk ratio will be calculated for dichotomous data. The intervention effect will be shown as the mean difference for continuous outcomes. Additionally, 95% confidence intervals will be calculated.
2.3.5. Heterogeneity evaluation
After stratifying the study according to the therapeutic duration and region, the chi-square test will be utilized to evaluate the heterogeneity and depressive symptoms. I2 statistic will be utilized for quantification of heterogeneity degree, where I2 >50% indicates the significant heterogeneity.[37–40]
2.3.6. Publication bias
The publication bias will be evaluated by funnel plots by determining whether there are 10 or more studies with the same outcome. In the case of asymmetric funnel plot, subgroup analysis or sensitivity analysis will be performed to investigate possible causes.[37,41]
2.3.7. Data synthesis
RevMan 5.3 software will be utilized for statistical analysis. The fixed-effects model will be employed to analyze data in the case of insignificant heterogeneity (I2 < 50%). In the case of heterogeneity (I2 ≥ 50%), subgroup analysis will be further conducted to decrease the clinical heterogeneity by taking into consideration of possible factors. If the heterogeneity is still significant, the random-effect model or qualitative description will be used.
2.3.8. Sensitivity analysis
Sensitivity analysis will be conducted by sequential omission of single study at a time, followed by simultaneously excluding 2 studies for identification of factors making the most contribution to heterogeneity.
2.3.9. Assessment of evidence quality
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) evaluation method of evidence quality will be used to evaluate the primary and secondary results of this study. The evidence quality will be categorized into high, moderate, low or very low according to five parameters (publication bias, indirectness, inconsistency, imprecision, and study limitations).
2.4. Ethics and publication
Since this study does not involve the patient privacy, ethical approval is not required. Our research results will be shared and shown through conference reports and peer-reviewed journals.
3. Discussion
The pathogenesis and clinical symptoms related to severe respiratory disease were described many years ago in TCM texts.[42] There are many studies on current application of TCM in COVID-19,[42,43] such as the clinical outcome, pathogenesis and the current application of TCM on COVID-19. The strength of our review includes the following 3 points. First, it is the first systematic review concerning the safety and effectiveness of acupuncture for breathlessness in COVID-19. Second, only RCTs are included in our systematic review, which are more likely to provide unbiased information than other study designs. Third, the comprehensive search strategy renders in-depth searching lists as well as trial registries associated with acupuncture and COVID-19.
However, the intrinsic methodological challenges among these enrolled trials will limit our systematic review. As a manipulated intervention, it is difficult to implement the blindness of therapeutic modes on acupuncturists.[44–48] Acupuncture therapy could be further categorized into manipulation and needling instrument. In addition, there might be great variation on acupuncture therapy in these enrolled studies. Although the above problem might be resolved and the consistency of interventions might be ensured by subgroup analysis, the comparability of enrolled researches will be decreased and the difficulty in meta-analysis will be increased.
Author contributions
Conceptualization: Baozhen Zhang and Kai Zhang.
Data curation: Kai Zhang and Zhenzhen Han.
Formal analysis: Kai Zhang and Zhenzhen Han.
Investigation: Baozhen Zhang and Kai Zhang.
Methodology: Baozhen Zhang.
Software: Qilin Tang and Kaihang Sun.
Supervision: Qilin Tang.
Writing – original draft: Baozhen Zhang, Kai Zhang, and Kaihang Sun.
Writing – review & editing: Qilin Tang.
Footnotes
Abbreviations: COVID-19 = coronavirus disease 2019, CoVs = coronaviruses, GRADE = grading of recommendations assessment, development and evaluation, HCoVs = human coronaviruses, MERS-CoV = Middle East respiratory syndrome coronavirus, PRISMA-P = preferred reporting items for systematic review and meta-analysis protocols, RCTs = randomized controlled trials, SARS-CoV = severe acute respiratory syndrome coronavirus, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2.
How to cite this article: Zhang B, Zhang K, Tang Q, Sun K, Han Z. Acupuncture for breathlessness in COVID-19: a protocol for systematic review and meta-analysis. Medicine. 2020;99:27(e20701).
BZ, KZ, QT, KS, and ZH contributed equally to this work and are considered co-first authors.
This study is supported by Health bureau of logistics support department of the military commission of China (grant number: 16BJZ46).
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol 2015;1282:1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Paules CI, Marston HD, Fauci AS. Coronavirus Infections-More Than Just the Common Cold. JAMA 2020. [DOI] [PubMed] [Google Scholar]
- [3].Del Rio C, Malani PN. COVID-19-new insights on a rapidly changing epidemic. JAMA 2020. [DOI] [PubMed] [Google Scholar]
- [4].Wang C, Horby PW, Hayden FG, et al. A novel coronavirus outbreak of global health concern. Lancet 2020;395:470–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 2020;323:1239–42. [DOI] [PubMed] [Google Scholar]
- [8].Niu S, Tian S, Lou J, et al. Clinical characteristics of older patients infected with COVID-19: a descriptive study. Arch Gerontol Geriatr 2020;89:104058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jin YH, Cai L, Cheng ZS, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res 2020;7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Dong L, Hu S, Gao J. Discovering drugs to treat coronavirus disease 2019 (COVID-19). Drug Discov Ther 2020;14:58–60. [DOI] [PubMed] [Google Scholar]
- [11].Liu X, Zhang M, He L, et al. Chinese herbs combined with Western medicine for severe acute respiratory syndrome (SARS). Cochrane Database Syst Rev 2012;10:CD004882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ren JL, Zhang AH, Wang XJ. Traditional Chinese medicine for COVID-19 treatment. Pharmacol Res 2020;155:104743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Zhang K. Is traditional Chinese medicine useful in the treatment of COVID-19? Am J Emerg Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zhang K, Tang Q. The dilemma and hope of Traditional Chinese Medicine practitioners in China. Integr Med Res 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yang Y, Islam MS, Wang J, et al. Traditional Chinese medicine in the treatment of patients infected with 2019-new coronavirus (SARS-CoV-2): a review and perspective. Int J Biol Sci 2020;16:1708–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].von Trott P, Oei SL, Ramsenthaler C. Acupuncture for breathlessness in advanced diseases: a systematic review and meta-analysis. J Pain Symptom Manage 2020;59:327–38. e3. [DOI] [PubMed] [Google Scholar]
- [17].Zhang K, Li Y, Tang Q. Acupuncture for breathlessness in advanced diseases: methodological issues. J Pain Symptom Manage 2020;59:e3–4. [DOI] [PubMed] [Google Scholar]
- [18].Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med March 2002;136:374–83. [DOI] [PubMed] [Google Scholar]
- [19].Lovell N, Maddocks M, Etkind SN, et al. Characteristics,symptom management and outcomes of 101 patients with COVID-19 referred for hospital palliative care. J Pain Symptom Manage 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Cheong KB, Zhang JP, Huang Y, et al. The effectiveness of acupuncture in prevention and treatment of postoperative nausea and vomiting--a systematic review and meta-analysis. PLoS One 2013;8:e82474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zhang Y, Lin L, Li H, et al. Effects of acupuncture on cancer-related fatigue: a meta-analysis. Support Care Cancer 2018;26:415–25. [DOI] [PubMed] [Google Scholar]
- [22].Tang Q, Wang S, Zhang K, et al. Interventions for sleep problems during pregnancy: a systematic review. Sleep Med Rev 2020;51:101287. [DOI] [PubMed] [Google Scholar]
- [23].Lee SH, Lim SM. Acupuncture for insomnia after stroke: a systematic review and meta-analysis. BMC Complement Altern Med 2016;16:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Amorim D, Amado J, Brito I, et al. Acupuncture and electroacupuncture for anxiety disorders: a systematic review of the clinical research. Complement Ther Clin Pract 2018;31:31–7. [DOI] [PubMed] [Google Scholar]
- [25].Tang Q, Zhang K. Association of acupuncture and acupressure with improved cancer pain. JAMA Oncol 2020. [DOI] [PubMed] [Google Scholar]
- [26].Zhang K, Gao C, Li C, et al. Acupuncture for acute pancreatitis: a systematic review and meta-analysis. Pancreas 2019;48:1136–47. [DOI] [PubMed] [Google Scholar]
- [27].Zhang K, Li C, Gao C, et al. Efficacy and safety of acupuncture as an adjuvant treatment for acute pancreatitis: a protocol of systematic review and meta-analysis. BMJ Open 2019;9:e029327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Coyle ME, Shergis JL, Huang ET, et al. Acupuncture therapies for chronic obstructive pulmonary disease: a systematic review of randomized, controlled trials. Altern Ther Health Med 2014;20:10–23. [PubMed] [Google Scholar]
- [29].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- [30].National Health Commission of the People's Republic of China.<Guideline on diagnosis and treatment of COVID-19 (Trial 6th edition). http://www.nhc.gov.cn/xcs/zhengcwj/202002/8334a8326dd94d329df351d7da8aefc2.shtml. [access date February 23, 2020]. [Google Scholar]
- [31].Ahn DG, Shin HJ, Kim MH, et al. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19). J Microbiol Biotechnol 2020;30:313–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Aitken RC. Measurement of feelings using visual analogue scales. Proc R Soc Med 1969;62:989–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982;14:377–81. [PubMed] [Google Scholar]
- [34].Zhang K, Li Y, Tang Q. Acupuncture for stable angina pectoris: A few noteworthy additions. Eur J Prev Cardiol 2019. [DOI] [PubMed] [Google Scholar]
- [35].Wang Q, Tang Q, Zhang K. Letter to the editor regarding “acupuncture-induced cranial epidural abscess: case report and review of the literature”. World Neurosurg 2019;132:443. [DOI] [PubMed] [Google Scholar]
- [36].Tang Q, Tian L, Gao C, et al. The efficacy and safety of Xuebijing injection as an adjunctive treatment for acute pancreatitis: Protocol for a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2020;99:e18743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://www.handbook.cochrane.org. [Google Scholar]
- [38].Zhang K. Is Nigella Sativa Supplementation Effective for Asthma? Am J Emerg Med 2020. [DOI] [PubMed] [Google Scholar]
- [39].Tang Q, Zhang K. Is endoscopic retrograde cholangiopancreatography safe during pregnancy? Saudi J Gastroenterol 2020;26:61–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Zhang K. Water exchange versus air insufflation for colonoscopy: methodological issues of the meta-analysis are a cause for concern. Saudi J Gastroenterol 2019;25:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Zhang K. Xuebijing combined with ulinastation for sepsis:a few noteworthy additions. Am J Emerg Med 2020. [DOI] [PubMed] [Google Scholar]
- [42].Li M, Yang X, Li K, et al. Traditional Chinese medicine for novel coronavirus pneumonia treatment: main force or supplement? Trad Med Res 2020;5:62–4. [Google Scholar]
- [43].Cui HT, Li YT, Guo TY, et al. Traditional Chinese medicine for treatment of coronavirus disease 2019: a review. Trad Med Res 2020;5:65–73. [Google Scholar]
- [44].Zhang K, Tang Q. Acupuncture on aromatase inhibitor-induced arthralgia in patients with breast cancer. Breast 2019;45:119. [DOI] [PubMed] [Google Scholar]
- [45].Zhang K, Gao C, Tang Q. Acupuncture for reduction of symptom burden in multiple myeloma patients undergoing autologous hematopoietic stem cell transplantation: a randomized sham-controlled trial. Respond to author. Support Care Cancer 2019;27:3171–2. [DOI] [PubMed] [Google Scholar]
- [46].Tang Q, Zhang K. Is acupuncture effective for knee osteoarthritis? Comment on a recent trial. Clin Rehabil 2019;33:1697–8. [DOI] [PubMed] [Google Scholar]
- [47].Zhang K, Tang Q, Zhao C. Traditional manual acupuncture combined with rehabilitation therapy for shoulder hand syndrome after stroke within the Chinese healthcare system. Clin Rehabil 2019;33:1699–700. [DOI] [PubMed] [Google Scholar]
- [48].Zhang K, Tang Q, Gao C. Non-pharmacologic treatments for symptoms of diabetic peripheral neuropathy: a systematic review-methodological issues are a matter for concern. Curr Med Res Opin 2019;35:1319–20. [DOI] [PubMed] [Google Scholar]


