Abstract
Background:
Hypertension is a silent disease of the masses with an increasing prevalence and poor control rates. This study aims to establish and test the efficacy of a nurse-led hypertension management model in the community.
Methods:
A single-blind, randomized controlled trial was performed. 156 hypertensive patients with uncontrolled blood pressure were equally and randomly allocated into 2 groups. Patients in the study group received a 12-week period of hypertension management. Blood pressure, self-care behaviors, self-efficacy, and satisfaction were assessed at the start of recruitment, 12 and 16 weeks thereafter.
Results:
After the intervention, blood pressure of patients in the study group had greater improvement in self-care behaviors and a higher level of satisfaction with the hypertensive care compared to the control group (both P < .05).
Conclusions:
The nurse-led hypertension management model is feasible and effective for patients with uncontrolled blood pressure in the community.
Keywords: community, hypertension, management, model, nurse, randomized controlled trial
1. Introduction
There is an estimated 244.5 million (23.2%) Chinese adults aged ≥18 years who have hypertension, with another 41.3% (estimated 435.3 million) having pre-hypertension based on Chinese guidelines.[1] Among individuals with hypertension, 46.9% were aware of their condition, 40.7% were taking prescribed antihypertensive medications, and 15.3% had controlled hypertension.[1] The prevalence of hypertension in China based on the 2017 ACC/AHA guidelines was twice as high as that based on 2010 Chinese guideline (46.4%),[1] with a prevalence rate increasing by about 10% from 2002 to 2010.[2–4] However, about 15% of hypertension patients in China successfully controlled their blood pressure, which is defined as an average systolic blood pressure (SBP) < 140 mm Hg and an average diastolic blood pressure (DBP) < 90 mm Hg,[1] which is lower than in high-income countries (37%–65%).[5,6]
Doctors and nurses are equally key players in hypertension management.[7–9] A meta-analysis done by Carter et al.[10] showed a 4.8 mm Hg reduction in SBP in hypertensive patients who were following a nurse-led healthcare management. However, the latter has been questioned about its efficacy,[11,12] calling for further evaluation.
Hypertension management at the community level in China is a recent development. Recent studies about the latter had laid a preliminary platform with positive results that needed to be further explored.[13,14]
Randomized controlled trials (RCT) of community-based hypertension interventions[15–17] had been conducted but, due to poor experimental designs and lack of standard operational protocols, they were not reliable results to be considered. Therefore, additional studies were required to reinforce the trend observed, given that most studies about hypertension management in community health centers focused more on doctors than on nurses as leaders empowering the community.[15,16]
This study aimed to test the importance of a nurse-led hypertension management model compared to usual care in community health centers. Efficacy was assessed by analyzing changes in blood pressure and patient reported self-care behaviors, self-efficacy, and satisfaction between groups.
2. Methods
2.1. Ethical consideration
Prior to the recruitment, written informed consent was obtained from each participant. Ethical approval was obtained from our institution's Ethical Board Committee.
2.2. Design
2.2.1. Setting and Sample
The study was a 2-group parallel block RCT with a single-blind design. The calculation of the study sample size was based on a change in SBP. We assumed that α = 0.05 and power = 0.8. The calculated sample size was 96. The study was conducted during January and April 2018 in a community health center in Heibei, China.
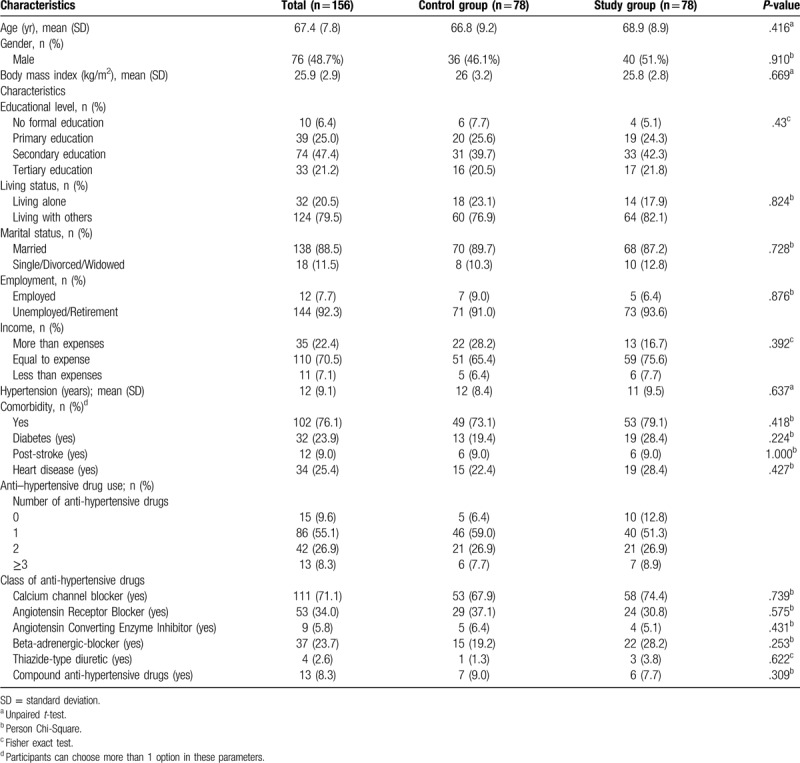
Participants were randomly allocated into the study group (nurse-led hypertension management model) or the control (usual care) group at a ratio of 1:1. As shown in Table 1, the 2 groups had equivalent socio-demographic and clinical features.
Table 1.
Socio-demographic and clinical characteristics of participants in study and control groups.
2.2.2. Inclusion criteria
Participants with a diagnosis of hypertension; with uncontrolled BP (SBP ≥140 mm Hg and/or DBP ≥90 mm Hg at the last 2 clinic visits and at recruitment);≥18 years old; within the service network of the community health center.
2.2.3. Exclusion criteria
Participants who had a diagnosis of secondary hypertension; took medicine that could increase BP; could not communicate or be contacted by phone; had a diagnosis of terminal illness; had co-morbidity in contradiction with the programmed intervention; were pregnant, breastfeeding or planning pregnancy.
Of 687 patients assessed for eligibility, only 156 satisfied the inclusion and exclusion criteria. A total of 31 (19.9%) participants dropped out of the study (Fig. 1). 318 patients did not meet the inclusion criteria while 84 declined their participation. The remaining 129 patients who were not included in the study were those who satisfied the inclusion criteria but followed treatment at other health care facilities. By using intention-to-treat analysis, those who dropped out were also included in data analysis.
Figure 1.

Flow diagram of selection criteria as per CONSORT Guidelines, including enrolment, allocation, follow-up and analysis.
The nurse-led hypertension management model was developed from the Chronic Care Model[18,19] and the 4-C Model (comprehensiveness, collaboration, coordination and continuity).[20,21] The nurse-led hypertension management model has adopted 4 components in the Chronic Care Model,[18,19] which is delivery system design, decision support, clinical information system and self-management.
A 36-h pre-intervention training program was conducted in this study to enhance the nurses’ decision-making.[22] The training contents included knowledge and skills for nurse-led hypertension management.
Self-management refers to the self-care behaviors, such as salt intake control, regular engagement in physical activities, home blood pressure monitoring management, and medicine storage, were also included. To emphasize the importance of self-management, a mutually agreed goal and self-care behavioral contract were made after sufficient negotiation.
The trained nurse assisted the patients to understand the importance of self-management, encouraging them to discuss health conditions, plan mutual goals and help patients how to achieve their set goal and perform self-monitoring, by providing and explaining to them relevant information and resources for self-management through illustrated, simple educational booklets.[4,22] During the home visit, the trained nurse would arrange for the general practitioner (a member of the research team) to visit community health center if the patient met the referral criteria.
2.3. Intervention
The intervention in the study was protocol-dependent. The protocol involved home visits, telephone follow-ups and referrals. Previous studies,[4,22,24] the national guidelines for hypertension management[25] and expert consultation were referenced in the protocol development.
Trained nurse, guided by the Omaha System,[23] conducted a 60-minutes home visit to patients within 3 days after recruitment. The patient's knowledge and behavior were assessed, as well as the status of their identified health problems. Based on the results, the trained nurses performed relevant interventions that included teaching/guidance/counseling in lifestyle modification changes, treatment and procedures such as timing and dosage adjustment as well as drug interactions and physical activity, and case management.[23]
Suggested non-pharmacological behaviors, including smoking cessation, alcohol restriction, salt restriction, regular physical activity, and home blood pressure monitoring were evaluated for the last 4 weeks. Self-efficacy was measured using the Chinese version of the Short-Form Chronic Disease Self-Efficacy Scale,[26] which included a rating of the patient's confidence in general disease and symptom management. The scale for each item ranged from 1 (not at all confident) to 10 (totally confident).
When the patient reported uncontrolled blood pressure, a trained nurse would assess his adherence, and/or any current illnesses or living circumstances that may affect his blood pressure. If home blood pressure monitoring was consistent with guidance, it was suggested that the patient have a face-to-face interview with a trained nurse in a community health center. If the patient had symptoms that required medication adjustments or a further health check (SBP ≥180 mm Hg or DBP ≥110 mm Hg), referral to the general practitioner was needed, and relevant information included blood pressure, a self-report and, if necessary, a medication list, pharmacy refill information, and medication adjustments.
After the home visit, follow-up via telephone calls was conducted biweekly by a trained nurse. During the follow-up, the trained nurse monitored the previous health problems and current condition of patients, as well as modifications in their knowledge, behavior, and status. The previously signed self-care behavioral contract was also reviewed, and further modification was discussed. Thereafter, it was recommended by the trained nurse that the patient should participate in a face-to-face follow-up in a community health center, and if the patient met the referral criteria, a referral would be initiated. Each follow-up call of 10 minutes duration on average, was conducted strictly according to the procedure, and was recorded and saved.
Each participant in the Control Group received a free annual health check, health education leaflets, and a follow-up with pharmacological treatment. The follow-ups were arranged by general practitioners if necessary.
2.4. Outcome and measurement
Outcome measures included blood pressure, self-care behaviors, self-efficacy and satisfaction.
2.5. Data collection
Two time points were set to collect patients’ data: T0 indicated after recruitment, T1 indicated immediately after the intervention (12 weeks post-recruitment) and T2 indicated 4 weeks after the intervention (16 weeks post-recruitment). Satisfaction measurement was performed at T0 and T1, and the others were conducted at T0, T1 and T2.
Blood pressure was measured twice using the same calibrated sphygmomanometer and stethoscope, and measurement strictly followed assessment guidelines,[25] with the mean value recorded. Self-care behavior was defined as the patients’ adherence to anti-hypertensive drugs (scores ranged from 0 to 3) and suggested non-pharmacological behaviors (scores ranged from 0 to 8).
The adherence form was adopted in previous studies conducted in China.[4,20,22] A higher score meant better adherence. The assessment of adherence to anti-hypertensive drugs depended on time, frequency, and dose.
2.6. Data analysis
The study was a 2-group parallel block RCT with a single-blind design. The calculation of the study sample size was based on a change in SBP. We assumed that α = 0.05 and power = 0.8. The effect size was 0.59, obtained from Chiu and Wong's study,[24] which involved intervention strategies similar to those in the current study. The calculated sample size was 96. A total of 130 participants would allow for a 20% dropout rate. Chi-square test was used for categorical variables, while the unpaired t-test was used for continuous variables. The unpaired t-test was also used to analyze outcomes of the 2 groups. Repeated measures ANOVA was carried out to evaluate the outcome over time, and 1-way repeated measures ANOVA was performed if the difference was significant. For further analysis of the within-group differences at different time points, a Bonferroni post-hoc test was performed.[27] The Mann-Whitney test was used to determine the difference between the 2 groups at each time point in self-care behavior and satisfaction. The Friedman test was used to examine self-care behavior modification over time in each group. Data was analyzed using the SPSS Statistics Version 20.0 (IBM Corp. Armonk, NY). When a significant difference was detected, the Wilcoxon signed-ranks and post hoc tests were further performed. P < .05 was considered as statistically significant.
3. Results
Table 1 showed the bio-data and demographics of both study and control populations, Both groups had similar socio-demographic and clinical features.
3.1. Blood pressure
Our results showed that both systolic and DBP decreased significantly in patients of the study group with a mean decrease of 15.03 ± 23.75 mm Hg (P = .032) in systolic and 8.54 ± 8.86 mmHg (P = .026) in DBP. Both the systolic and DBP in both groups decreased significantly with time (P < .05). (Table 2).
Table 2.
The mean reduction of blood pressure in 2 groups over time.
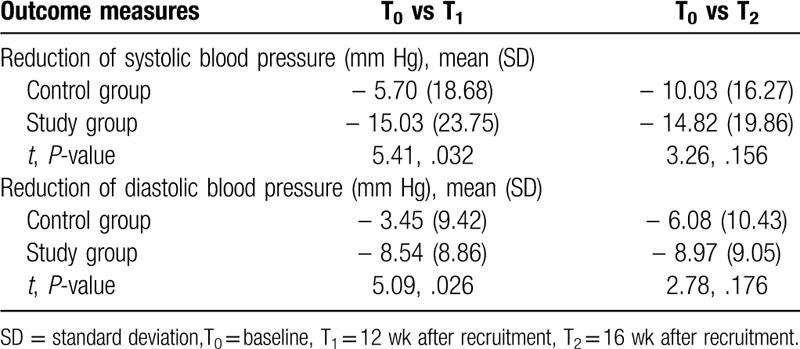
Therefore, both the nurse-led hypertension management model and usual care had positive effects on blood pressure reduction, which was more significant at T1 in the study group, compared to the control group. In addition, a sustained effect in blood pressure reduction was shown in the study group.
3.2. Self-care behaviors
As shown in Table 3, no significant difference was found in the score for adherence to anti-hypertensive drugs between the 2 groups at T0, T1, and T2. The median score for adherence to non-pharmacological suggestions was significantly higher in the study group than in the control group at T1 (P = .000) and T2 (P = .049).
Table 3.
Comparison analyses of median score of self-care behavior between 2 groups at 3 time points.

3.3. Self-efficacy
At T0, there were significant differences in self-efficacy between the study and control groups, which were measured at 5.94 and 6.71 respectively (P = . 015). Thus, they were used as covariates in the statistical testing. Two-way repeated measures ANOVA were performed. There was no significant difference between the 2 groups in interaction effect (time × group), between-group effect or time effect.
3.4. Patient satisfaction
In the study group, there was a median value increase from 4 to 29 (P = .000), while in the control group, it increased from 0 to 7 (P = .000). A remarkably higher satisfaction value was seen in the study group than in the control group at T1 (P = .000).
4. Discussion
World Health Organization[28] advocated the implementation of non-communicable disease intervention via a primary healthcare approach, community-based interventions were affordable and sustainable way to manage hypertension in Japan[29] and Canada.[30]
In the present study, both systolic and DBP were significantly reduced in the study group compared with those in the control group same. Patients of the study group showed a mean decrease of 15.03 ± 23.75 mm Hg (P = .032) in systolic and 8.54 ± 8.86 mm Hg (P = .026) in DBP respectively. The same has been previously demonstrated by Chiu and Wong[24] and Ma et al[17] after a six-month intervention.
A reduction of SBP by 5 mm Hg or of DBP by 2 mm Hg is usually considered as clinically significant.[31] Our data showed that the number of participants in the study group with more than 5 mm Hg reduction in SBP at T1, was much higher than in the control group. (Table 3)
Among participants, satisfaction was higher in the study group than the control group as reflected by other studies.[32–34] Keleher et al[8] and Laurant et al[9] both reported that patients with chronic diseases had a higher level of satisfaction with nurse-led care than with doctor-led care in the primary care setting.[24] This satisfaction may be linked to trained nurses who comprehensively assessed the health condition of patients, conducting home visits to facilitate care, with follow-ups via phone calls. Nurses interacted with general practitioners and managed health resources to such degree that neither time was wasted nor treatment plans were overlapped. Increased interaction, timely management and non-wastage of equipments in the nurse-led intervention model may have been factors associated with satisfaction.
The self-care behaviour of patients is enhanced in this study with a sustained effect throughout. Self-efficacy showed a significant difference between the 2 groups, but no significant difference in interaction effect (time × group), between-group effect or time effect. The latter may be related to the participants’ lower level of education in this study with 67% of participants with less than tertiary level, which correlates with previous study.[32] self-efficacy can also be due a long history of hypertension, with mean duration of 12 years, with poor hypertension control prior to joining the study.
Current study adds to the growing evidence that informed, prepared and motivated patients are key players in the control of their own blood pressure. The model established in the study provides an efficient approach for managing a large volume of hypertensive patients in a community-level setting in which there is a shortage of doctors, where the well-trained nursing staff can emphasize on health promotion and patient-empowerment. In the nurse-led hypertension management model, the training program provided a structured curriculum enabling nurses to enhance their decision-making abilities, thus expanding the nurse's current traditional dependent role in hypertension management, by enabling more independent roles, such as assessment and counseling. A longer interaction by the nurses at 16 weeks will be beneficial to keep following-up the patients and ensure compliance and lifestyle modifications.
The limitations of the present study were that this intervention was tested in a single community health center, which restrained the ability to generalize results. The community health center was in an urban setting; it is unknown if responses would be similar among rural adults who may have lower levels of education. [32] This study was single-blinded, but health care providers may not have been blinded to the intervention strategies which may have lessened the effect of the intervention.
To assess secondary parameters such as self-care, self-efficacy and patient satisfaction, the author proposed that study targeting newly diagnosed hypertensive be conducted.
5. Conclusion
Empowering the nurses to manage hypertension at the community level is feasible with the possibility of good positive outcome to the patients. This current study contributes to the ascending trend of nurse-led program for hypertension management but also provides the platform for more studies to be continued in both the rural and urban settings.
Acknowledgments
The Authors would like to thank the nursing and medical staff of our institutions, Heibei Province.
Author contributions
Mrs. Miao designed the research together with Mrs. Liu.
Mrs. Wang led the formation of the specialised nurses and gathered data.
Mrs. Liu analysed the collected data.
Mrs. Miao led the write-up.
Footnotes
Abbreviations: DBP = diastolic blood pressure, RCT = randomized controlled trial, SBP = systolic blood pressure.
How to cite this article: Miao JH, Wang HS, Liu N. The evaluation of a nurse-led hypertension management model in an urban community healthcare: a randomized controlled trial. Medicine. 2020;99:27(e20967).
Availability of data: Study data will be made available upon request.
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Wang Z, Chen Z, Zhang L, et al. Status of Hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation 2018;137:20. [DOI] [PubMed] [Google Scholar]
- [2].Gao Y, Chen G, Tian HM, et al. For the China National Diabetes and Metabolic Disorders Study Group, 2013. Prevalence of hypertension in China: a cross-sectional study. PLoS One 2013;8:e65938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wang JW, Zhang LX, Wang F, et al. The China National Survey of Chronic Kidney Disease Working Group, 2014. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens 2014;27:1355–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Zhu X, Wong FKY, Wu CLH. Development and evaluation of a nurse-led hypertension management model: a randomized controlled trial. Int J Nurs Stud 2018;77:171–8. [DOI] [PubMed] [Google Scholar]
- [5].McAlister FA, Wilkins K, Joffres M, et al. Changes in the rates of awareness, treatment and control of hypertension in Canada over the past two decades. CMAJ 2011;183:1007–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Nwankwo T, Yoon SS, Burt V, et al. Hypertension among adults in the United States: National health and nutrition examination survey, 2011–2012. NCHS Data Brief 2013;133:1–8. [PubMed] [Google Scholar]
- [7].Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002;324:819–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Keleher H, Parker R, Abdulwadud O, et al. Systematic review of the effectiveness of primary care nursing. Int J Nurs Prac 2009;15:16–24. [DOI] [PubMed] [Google Scholar]
- [9].Laurant M, Reeves D, Hermens R, et al. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev 2005. CD001271. [DOI] [PubMed] [Google Scholar]
- [10].Carter BL, Rogers M, Daly J, et al. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med 2009;169:1748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Clark CE, Smith LFP, Taylor RS, et al. Nurse-led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ 2010;341:c3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Glynn LG, Murphy AW, Smith SM, et al. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010. CD005182. [DOI] [PubMed] [Google Scholar]
- [13].Chen XJ, Gao XL, You GY, et al. Higher blood pressure control rate in a real life management program provided by the community health service center in China. BMC Public Health 2014;14:801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Liang XH, Chen J, Liu YX, et al. The effect of hypertension and diabetes management in Southwest China: a before-and-after intervention study. PLoS One 2014;9:e91801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Gao JL, Li Y, Dai JM, et al. Evaluation of group visits for Chinese hypertensives based on primary health care center. Asia Pac J Pub Health 2015;27:350–60. NP. [DOI] [PubMed] [Google Scholar]
- [16].Lu ZX, Cao SY, Chai Y, et al. Effectiveness of interventions for hypertension care in the community −a meta-analysis of controlled studies in China. BMJ Health Serv Res 2012;12:216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ma CH, Zhou Y, Zhou W, et al. Evaluation of the effect of motivational interviewing counselling on hypertension care. Patient Educ Couns 2014;95:231–7. [DOI] [PubMed] [Google Scholar]
- [18].Wagner EH, Austin BT, Davis C, et al. 2001 Improving chronic illness care: translating evidence into action. Health Aff (Millword) 2014;20:64–78. [DOI] [PubMed] [Google Scholar]
- [19].Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Prac 1998;1:2–4. [PubMed] [Google Scholar]
- [20].Wong FKY, Chow SK, Chan TMF. Nurse follow-up of patients with diabetes: randomized controlled trial. J Adv Nurs 2005;50:391–402. [DOI] [PubMed] [Google Scholar]
- [21].Wong FKY, Chow SK, Chan TMF. Evaluation of a nurse-led disease management programme for chronic kidney disease: a randomized controlled trial. Int J Nurs Stud 2010;47:268–78. [DOI] [PubMed] [Google Scholar]
- [22].Zhu X, Wong FKY, Wu LH. Development and evaluation of a nurse-led hypertension management model in a community: a pilot randomized controlled trial. Int J Clin Exp Med 2014;7:4369–77. [PMC free article] [PubMed] [Google Scholar]
- [23].Martin KS. The Omaha System: a key to practice, documentation, and information management. 2nd ed.Omaha: Health Connections Press; 2005. [Google Scholar]
- [24].Chiu CW, Wong FKY. Effects of 8 weeks sustained follow-up after a nurse consultation on hypertension: a randomized trial. Int J Nurs Stud 2010;47:1374–82. [DOI] [PubMed] [Google Scholar]
- [25].Liu LS. Writing group of 2010 Chinese Guidelines for the management of hypertension. Guidelines for prevention and treatment of hypertension in China version). Front Med China 2010;3:42–93. [Google Scholar]
- [26].Chow KY, Wong KY. The reliability and validity of the Chinese version of the Short-form Chronic Disease Self-Efficacy Scales for older adults. J Clin Nurs 2014;23:1095–104. [DOI] [PubMed] [Google Scholar]
- [27].Portney LG, Watkins MP. Foundations of Clinical Research Applications to Practice. 3rd ed.New Jersey: Prentice Hall Health; 2009. [Google Scholar]
- [28].World Health Organization, 2013. A Global Brief on Hypertension. Retrieved from. Available at: http://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/. [Google Scholar]
- [29].Community-based Efforts to Reduce Blood Pressure and Stroke in Japan. 2013. Available a: http://www.who.int/features/2013/japan_blood_pressure/en/. [Google Scholar]
- [30].Kaczorowski J, Chambers LW, Karwalajtys T, et al. Cardiovascular health awareness program (CHAP): a community cluster-randomised trial among elderly canadians. Pre Med 2008;46:537–44. [DOI] [PubMed] [Google Scholar]
- [31].Verdecchia P, Gentile G, Angeli F, et al. Influence of blood pressure reduction on composite cardiovascular endpoints in clinical trials. J Hypertens 2010;28:1356–65. [DOI] [PubMed] [Google Scholar]
- [32].Leganger A, Karaft P. Control constructs: do they mediate the relation between educational attainment and health behaviour? J Health Psychol 2003;8:361–72. [DOI] [PubMed] [Google Scholar]
- [33].Bebb C, Kendrick D, Coupland C, et al. A cluster randomized controlled trial of the effect of a treatment algorithm for hypertension in patients with type 2 diabetes. Br J Gen Pract 2007;57:136–43. [PMC free article] [PubMed] [Google Scholar]
- [34].Caldow J, Bond C, Ryan M, et al. Treatment of minor illness in primary care: a national survey of patient satisfaction, attitudes and preferences regarding a wider nursing role. Health Expect 2007;10:30–45. [DOI] [PMC free article] [PubMed] [Google Scholar]


