Supplemental Digital Content is available in the text
Keywords: backward walking, meta-analysis, stroke, systematic review
Abstract
Background:
Backward walking (BW) training is increasingly used in rehabilitation for stroke, but relevant evidence remains unclear.
Objective:
To determine the effect of BW training on patients with stroke.
Methods:
A keyword search was conducted in PubMed, EMBASE, CINAHL, and China National Knowledge Infrastructure database for articles published until November, 2019. Two investigators screened the articles and extract data from each included study. Meta-analysis was performed to estimate the effect of BW on stroke. In addition, the quality of evidence was evaluated by GRADE (grading of recommendations, assessment, development, and evaluation; version:3.6) approach.
Results:
A total of ten studies were included according to the inclusion and exclusion criteria in the review. All included studies described some positive influences of BW on stroke relative to the control group (forward walking or conventional treatment). Compared to control group, there is a statistically significant improvement for BW group in gait velocity (mean difference [MD] = 6.87, 95%CI: [1.40, 12.33], P = .01, I2 = 3%), Berg balance score (MD =3.82, 95%CI: [2.12, 5.52], P < .0001, I2 = 0%), and walk test (MD =0.11, 95%CI: [0.02, 0.20], P = .02, I2 = 36%).
Conclusions:
For patients with stroke, BW training, as an adjunct an adjunct to conventional treatment, can improve Berg balance score (moderate evidence), walk test performance (very low evidence), gait velocity (very low evidence). More large-scale and high-quality studies are warranted.
1. Introduction
Stroke, as an acute neurological injury, including ischemic stroke and hemorrhagic stroke, which results in the sudden loss of focal brain function due to the death of cells caused by the interruption of blood flow or hemorrhage in the brain.[1] As a leading cause of death and disability, it has become a major health problem in China and the United States.[2,3] Among stroke survivors, disability is a common sequela.[4] They are often accompanied by reduced proprioception,[5] balance impairment,[6] gait alteration,[7] coordination deterioration[8] and high risk of falling.[9]
Backward walking (BW) is a simple and effective method for adjuvant treatment and rehabilitation.[10] On 1 hand, BW is helpful for improving proprioception,[11,12] muscle strength,[13] intralimb coordination[14] and balance.[15] On the other hand, it can also assess the severity of impairment of coordination and motor ability, and serve as a predictor of falls in the elderly.[16] Different from forward walking (FW), the gait and lower extremity biodynamics of stroke patients will significantly change during BW.[17] DeMark L et al[18] found that BW can improve walking function, balance, and prevent fall-risk in acute stroke.
There are 4 meta-analyses studies on BW in the previous articles.[19–22] It is reported that BW training can not only be a potentially useful tool to improve balance performance,[19] but also to change the spatial-temporal gait characteristics and useful for neurological rehabilitation.[20] And Elnahhas AM et al[21] reported that backward gait training had a good effect on improving motor function, balance, walking velocity and step length in children with cerebral palsy. Furthermore, Denissen S et al[22] documented interventions could reduce falling for post stroke more than exercises such as walking program. However, Balasukumaran T et al[23] suggested there was insufficient evidence to support the idea that BW is effective for balance, gait parameters and stability in people with gait impairments. In the light of the above-mentioned knowledge, what is the impact of the post-stroke patients who also have limb dysfunction? There is no evidence-based basis so far. Consequently, a meta-analysis of randomized controlled trial was carried out to investigate the effectiveness of BW on the stroke.
2. Methods
This meta-analysis was fulfilled according to the Preferred Reporting Items for Systematic Review and Meta-analyses.[24]
2.1. Ethics statement
Because all analyses were conducted according to previously published studies, no ethical approval or patient consent was required in this review.
2.2. Selection criteria
In this study, all the included literatures should meet the following criteria: ①Study design: clinical randomized controlled study; ②Patients: people affected by stroke; ③Intervention: BW, BW+ other treatments; ④Outcomes: at least one efficacy index, ⑤Language: English, Chinese and Korean. A literature would be excluded if it met any of the following criteria: ①Protocols, case reports, observational studies, cohort studies; full-text unavailable articles, such as a poster, studies in other languages except for Chinese and English, unpublished literatures; ②Repeated publications, animal experimental studies, reviews.
2.3. Search strategy
We performed the literature search in PubMed, EMBASE, CINAHL and China National Knowledge Infrastructure database. A keyword such as “backward”, “step”, “walking”, “gait”, “locomotion”, “retro” and so on was used to search without restrictions, up to November 13, 2019. The search algorithm was detailed described in the supporting. All the literatures in this study were screened by 2 investigators (ZH Chen and XL Ye). First, literatures were preliminarily selected after careful reading of the topics and abstracts. Second, the uncertain documents were screened strictly according to the inclusion and exclusion criteria after reading the full text. Finally, the data and materials in the included literatures were extracted without controversy.
2.4. Data extraction
We collected the main information of the articles, including authors’ names, publication year, age, and gender of patients, poststroke duration, study design, intervention type, intervention dose, main outcomes and sample size.
2.5. Quality assessment
According to 5.1.0[25] of Cochrane manual, 2 reviewers (ZH Chen and WJ Chen) assessed the quality of the literature by the risk of bias table. The literature was evaluated from 7 aspects: sequence generation, allocation concealment, blind of participants and personnel, blind of outcome, incomplete outcome data, selective reporting and other biases. The risk of bias is divided into 3 levels: high, unclear and low. In addition, the quality of evidence was evaluated by GRADE (grading of recommendations, assessment, development, and evaluation; version:3.6) approach.[26]
2.6. Statistical analysis
The review manger 5.3 software was used to make a meta system analysis of the observation indicators in the included literature, and the results were illustrated by the forest map intuitively. In this study, all parameters were continuous variables. They were pooled by standard mean difference (MD) or MD with 95% confidence intervals. Heterogeneity was assessed by the Cochran Q-test and I2 index.[27] A random-effect model would be used when a high heterogeneity (I2 > 50% and PQ-test < .1) was detected, otherwise a fix-effect model was prime to be evaluated. The difference was statistically significant when P-values < .05.
3. Results
3.1. Study selection
A total of 547 related records were obtained by searching Chinese and English databases. The literatures were imported into EndNote X8 (Bld, 10063) to remove duplicate literature. After removing 242 duplicates and eliminating 292 articles through the preliminary screening, reading summary and full text, remaining 13 full-text articles were reviewed. According to the inclusion criteria and exclusion criteria, 10 articles[28–37] were selected and 255 stroke patients were included. Three studies were excluded: a poster, a protocol and one without full-text. All included studies described some positive influences of BW on stroke relative to the control group (CG) treated with FW or balance training or conventional methods focusing on strengthening, function, mobility activities and gait training. The selection flowchart is shown in Figure 1, and the basic information of each included literature is shown in Table 1.
Figure 1.
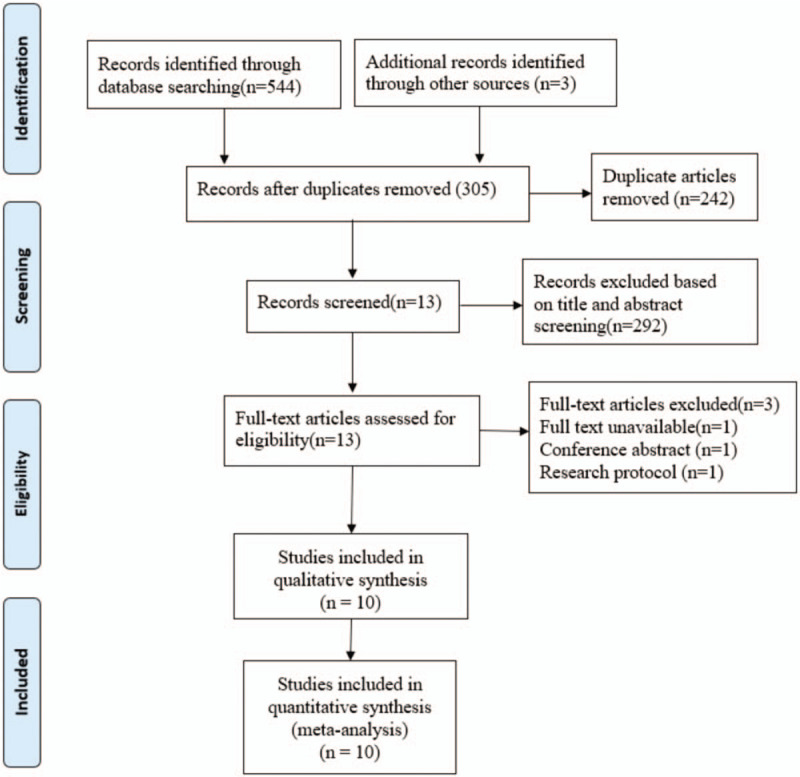
Flowchart of study selection. A total of 10 studies were included according to the inclusion and exclusion criteria in the review.
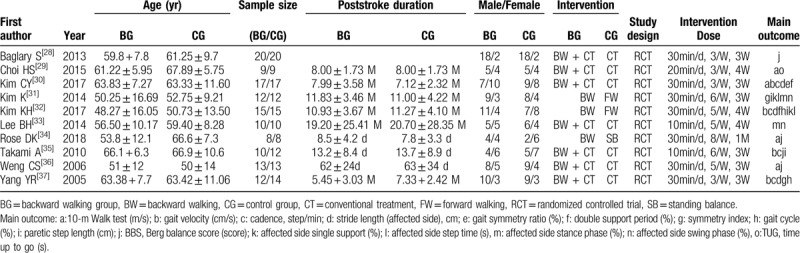
Table 1.
Characteristics of the included studies.
3.2. Risk of bias
All studies were described as random generation, but only 4 articles[30,32,35,36] recorded the methods of randomization in detail, in which the sealed envelope was selected. Blind methods were detailed in three studies30.32.34, and the drop-out rate was recorded in 4 articles.[30,32,35,37] The drop-out rate of one study[30] was up to 18.19%, which was considered as a high risk in attrition bias. If 2 investigators (ZH Chen and XL Ye) agreed there was not enough information to judge it as a high or low risk, it would be considered as an unknown risk. The detailed results are shown in Figure 2.
Figure 2.
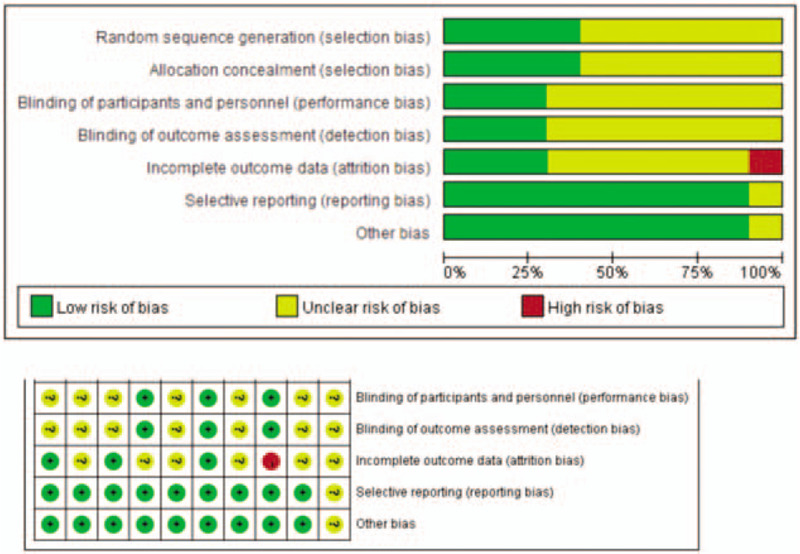
Risk of bias graph.
3.3. Meta-analysis
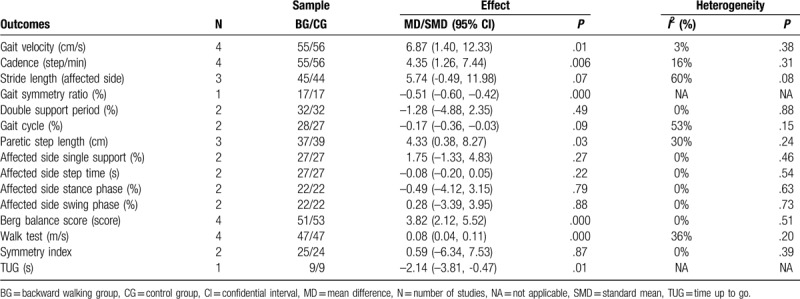
We summarize the data and meta-analysis results of gait characteristics, Berg balance score (BBS), walk test, symmetry index and time up to go (TUG) in Table 2.
Table 2.
Summary of meta-analysis outcomes.
3.3.1. Gait characteristics
From fixed-effects model, the overall effect showed a statistically significant difference with high heterogeneity between the two groups (MD =-0.33, 95%CI: [-0.40, -0.26], P <.000001, I2 = 67%). Therefore, subgroup analysis was carried out for the results. Overall, compared to CG, the results indicated statistically significant improvement for BG group in gait velocity reported in 4 studies[30,32,35,37] (MD = 6.87, 95%CI: [1.40, 12.33], P = .01, I2 = 3%), cadence used in 4 studies[30,32,35,37] (MD = 4.35, 95%CI: [1.26, 7.44], P = .006, I2 = 16%), and paretic step length adopted in three studies[31,32,35] (MD = 4.33, 95%CI: [0.38, 8.27], P = .03, I2 = 30%), whereas BG has no significant difference in double support period[30,32] (MD = -1.28, 95%CI: [-4.88, 2.35], P = .006, I2 = 16%), gait cycle[32,37] (MD = -0.17, 95%CI: [-0.36, -0.03], P = .09, I2 = 53%), stance phase[31,33] (MD = -0.49, 95%CI: [-4.12, 3.15], P = .79, I2 = 0%), swing phase[31,33] (MD = 0.28, 95%CI: [-3.39, 3.95], P = .88, I2 = 0%). When the study[32] compared between BW and FW was excluded, it was further found that, in comparison with conventional therapy (CT), CT combination of BW could significantly improve gait velocity (MD = 6.60, 95%CI: [0.90, 12.20], P = .02, I2 = 32%) and paretic step length (MD = 4.10, 95%CI: [-2.04, 10.23], P = .19, I2 = 65%), but cadence (MD = 2.94, 95%CI: [-1.26, 7.15], P = 0.17, I2 = 24%) showed no difference. Meanwhile, there was no significant difference between FW and BW in single support[31,32] (MD = 1.75, 95%CI: [-1.33, 4.83], P = .27, I2 = 0%), step time[31,32] (MD = -0.08, 95%CI: [-0.20, 0.05], P = .22, I2 = 0%). In addition, affected side stride length in fixed-effects model showed a high-level heterogeneity (MD = 5.74, 95%CI: [-0.49, 11.98], Q-test P = .08, I2 = 60%), it turned to be a little lower when fixed-effects model was selected (standard MD = 0.44, 95%CI: [-0.16, 1.04], Q-test P = .14, I2 = 49%). However, no significant difference was shown in stride length between BG and CG (P = .15). Only 1 study[30] reported the gait symmetry ratio, a significant reduction was shown in BG in comparison to CG (MD = -0.51, 95%CI: [-0.60, -0.42], P <.00001). Meta-analysis and forest plots were shown in Figure 3 .
Figure 3.
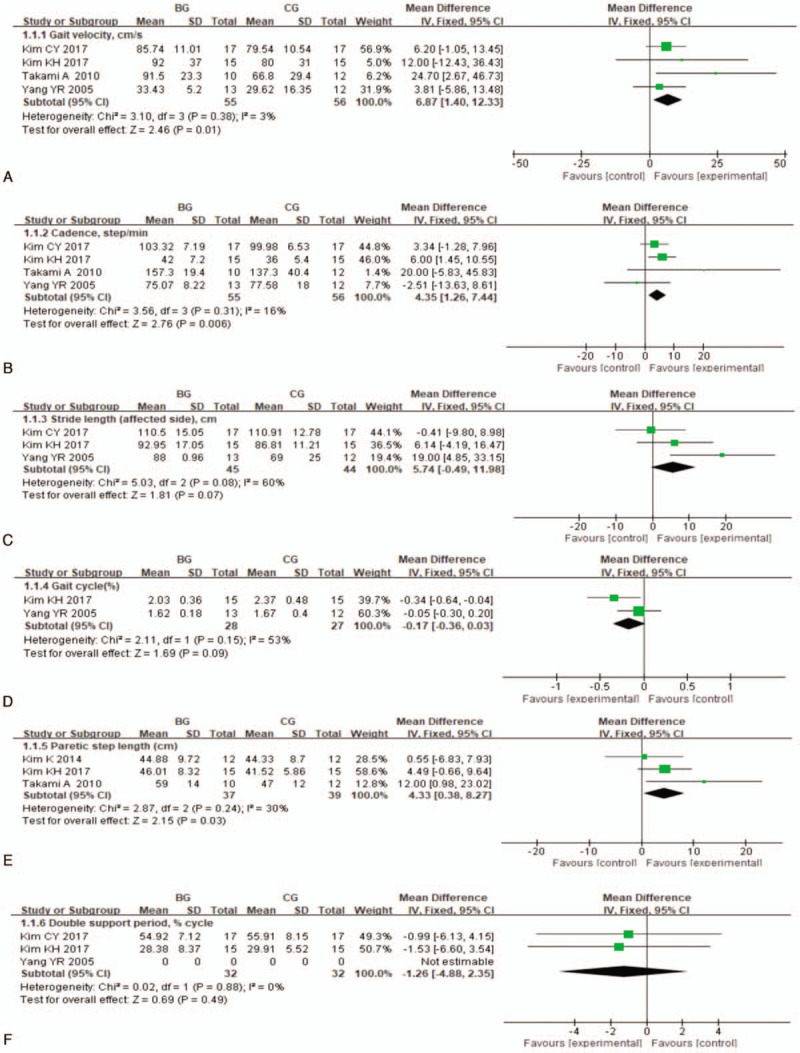
Meta-analysis and forest plot and for gait characteristics. Compared to CG, there is a statistically significant improvement for BG in gait velocity (MD = 6.87, 95%CI: [1.40, 12.33], P = .01, I2 = 3%), cadence (MD = 4.35, 95%CI: [1.26, 7.44], P = .006, I2 = 16%), paretic step length (MD = 4.33, 95%CI: [0.38, 8.27], P = .03, I2 = 30%). BG = backward walking group, CG = control group.
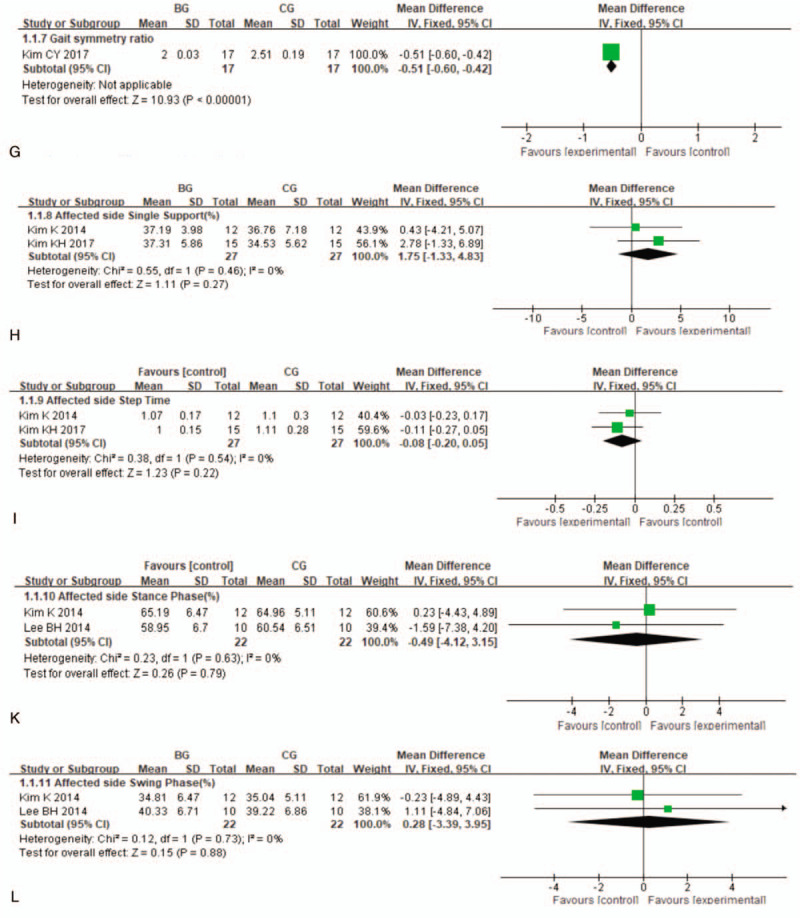
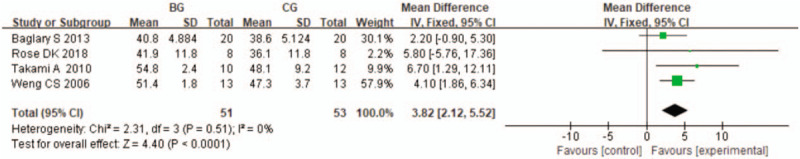
3.3.2. BBS, walk test, symmetry index, and TUG
Overall, the analysis result (Fig. 4) revealed a significant difference between BG and CG (MD = 3.82, 95%CI: [2.12, 5.52], P < .0001, I2 = 0%) in BBS reported in 4 studies[28,34,35,36]; 4 of the 10 included studies documented the walk test,[29,30,34,36] evaluated by a fix-effect model, a significant improvement (MD = 0.08, 95%CI: [0.04, 0.11], P <.0001, I2 = 36%) was found in BG in comparison to CG (Fig. 5). When the study[34] recording a comparison between BW and standing balance was excluded, the other 3 studies still demonstrated a significant difference between BW combination of CT and CT in BBS (MD = 3.78, 95%CI: [2.06, 5.50], P< .0001, I2 = 9%) and walk test (MD = 0.07, 95% CI: [0.03, 0.11], P <.0002, I2 = 0%). Data from the 2 studies,[31,37] no differences in symmetry index were observed between BG and CG (MD = 0.59, 95%CI: [-6.34, 7.53], P = .87, I2 = 0%). One study[29] focused on the effect of BW on TUG, a significant reduction in TUG was found in BG (MD = -2.14, 95%CI: [-3.81, -0.47], P = .01). Frost plots from meta-analysis for symmetry index and TUG were shown in Supplementary eFigure 1 and eFigure 2, respectively.
Figure 3 (Continued).
Meta-analysis and forest plot and for gait characteristics. Compared to CG, there is a statistically significant improvement for BG in gait velocity (MD = 6.87, 95%CI: [1.40, 12.33], P = .01, I2 = 3%), cadence (MD = 4.35, 95%CI: [1.26, 7.44], P = .006, I2 = 16%), paretic step length (MD = 4.33, 95%CI: [0.38, 8.27], P = .03, I2 = 30%). BG = backward walking group, CG = control group.
Figure 4.
Meta-analysis and forest plot and for BBS. Compared to CG, BBS showed a significant improvement for BG (MD = 3.82, 95%CI: [2.12, 5.52], P < .0001, I2 = 0%). BBS = Berg balance score, BG = backward walking group, CG = control group.
Figure 5.
Meta-analysis and forest plot and for walk test. Compared to CG, BG demonstrated a greater improvement in walk test (MD = 0.11, 95%CI: [0.02, 0.20], P = .02, I2 = 36%). BG = backward walking group, CG = control group.
3.3.3. Sensitivity analysis
In this study, the heterogeneity of each index was acceptable. Therefore, the overall heterogeneities and results were stable, when gait velocity was selected for sensitivity analysis (Supplementary Table 1). The study[28] with all unclear biases were excluded when we conducted the evaluation of sensitivity analysis.
3.3.4. Evidence quality assessment according to GRADE
According to GRADE guidelines, the quality of evidence is evaluated from 5 aspects: risk of bias, inconsistency, indirectness, imprecision, publication bias. In the comparison between the BG and CG, there is moderate evidence in BBS, low evidence in symmetry index and cadence, and very low evidence in the remaining. Corresponding information was shown in Supplementary efigure 3.
4. Discussion
BW is increasingly used in rehabilitation and sports because of its different movement patterns.[38] To the best of our knowledge, it has been reported that BW exhibits a positive effect on the rehabilitation of post stroke,[18] knee osteoarthritis,[39] diabetic foot syndrome,[16,40] Parkinson's,[41] pediatric cerebral palsy,[42] low back pain,[43] and anterior cruciate ligament reconstruction.[12] morever, Thomas KS et al[44] suggested that greater cardiovascular, neuromuscular, perceptual and metabolic demands were required for BW. In addition, it is also proven to be beneficial to improve cardiopulmonat function.[45,46]
Different from Balasukumaran T's study,[21] we selected the studies in which people suffering from stroke severed as observation objects. It greatly eliminated the interference of different subgroups. Most importantly, more literatures on the treatment with BW for stroke were included, which was helpful for us to analyze the impact of BW on stroke. In our study, overall, it was found that gait characteristics indices-gait velocity, cadence and paretic step length- significantly increased after a period of BW training added in comparison to CG. This is inseparable from the fact that BW training can improve the flexibility and coordination of the lower limbs. Improved gait velocity is beneficial to improve walking ability. The larger paretic step length maybe related to the factor[47] that BW can increase muscle strength. However, when compared to CT, BW combination of CT showed no significant improvement in cadence and paretic step length. It may be explained by the reason that CT included some exercise which also could contribute to cadence and paretic step length for stroke patients. In addition, BBS and walk test performance in BG became better than that in the CG. BBS can reflect the degree of walking improvement for patients with stroke,[48] and predict the risk of falls.[49] All in all, it is suggested that BW can be used as an effective method to improve some gait indices, balance and walking ability of stroke patients.
There are some limitations in this review. First, there is a lack of large-scale studies in the 10 literatures included, and random and blind methods are rarely used. Second, the treatment cycle and exercise intensity of reverse walking are not consistent, which will affect the results. Third, the effect for stroke by training on the treadmill and the ground with BW will also be different. Fourthly, different machines selected in the measurement of gait parameters will also have different degrees of impact on the analysis results.
5. Conclusion
In this paper, the effect of BG on stroke patients was systematically reviewed and quantified. For patients with stroke, BW training, as an adjunct an adjunct to conventional treatment, can improve BBS (moderate evidence), walk test performance (very low evidence), gait velocity (very low evidence). More large-scale and high-quality studies are warranted.
Author contributions
ZH-C and XM-X designed the study.
ZH-C and XL-Y did the literature searches and designed the data-extraction form
ZH-C, XL-Y and GQ-C selected studies.
ZH-C, JT-W and WJ-C extracted the data.
GQ-C and H-W did statistical analyses.
XM-X supervised the study.
H-W did the language editing.
All authors read and approved the submitted version.
Supplementary Material
Footnotes
Abbreviations: 95% CI = 95% confidence intervals, BBS = Berg balance score, BG = backward walking group, BW = backward walking, CG = control group, FW = forward walking, MD = mean difference, TUG= time up to go.
How to cite this article: Chen ZH, Ye XL, Chen WJ, Chen GQ, Wu JT, Wu H, Xu XM. Effectiveness of backward walking for people affected by stroke: A systematic review and meta-analysis of randomized controlled trials. Medicine. 2020;99:27(e20731).
ZHC, XLY and WJC authors contributed equally to this work.
This work was supported by Guangdong Provincial Special Fund for Industrial and Information Development (Guangdong Finance and Industry (2016) 69), Breakthrough Project of Superiority Diseases of Traditional Chinese Medicine of Guangdong Province (Letter No. 19, 2015), Scientific research Project of Traditional Chinese Medicine Bureau of Guangdong Province (No. 20194002), Soft Science Research Program of Guangdong Province (No. 2018B020207009), and Science and Technology Plan Project of Guangdong Province (2019A141401008).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Lachance CC, Ford C. Portable Stroke Detection Devices for Patients with Stroke Symptoms: A Review of Diagnostic Accuracy and Cost-Effectiveness [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2019 Aug. Available at: http://www.ncbi.nlm.nih.gov/books/NBK549206/PubMed PMID: 31682388. [PubMed] [Google Scholar]
- [2].Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study. Lancet 2019;394:1145–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Barthels D, Das H. Current advances in ischemic stroke research and therapies. Biochim Biophys Acta Mol Basis Dis 2020;1866(4):165260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Mansfield A, Inness EL, Mcilroy WE. Stroke Handb Clin Neurol 2018;159:205–28. [DOI] [PubMed] [Google Scholar]
- [5].Tyson SF, Sadeghi-Demneh E, Nester CJ. The effects of transcutaneous electrical nerve stimulation on strength, proprioception, balance and mobility in people with stroke: a randomized controlled cross-over trial. Clin Rehabil 2013;27:785–91. [DOI] [PubMed] [Google Scholar]
- [6].Fishbein P, Hutzler Y, Ratmansky M, et al. A Preliminary study of dual-task training using virtual reality: influence on walking and balance in chronic poststroke survivors. J Stroke Cerebrovasc Dis 2019;28:104343. [DOI] [PubMed] [Google Scholar]
- [7].Celestino ML, van Emmerik R, Barela JA, et al. Intralimb gait coordination of individuals with stroke using vector coding. Hum Mov Sci 2019;68:102522. [DOI] [PubMed] [Google Scholar]
- [8].Kwan MS, Hassett LM, Ada L, et al. Relationship between lower limb coordination and walking speed after stroke: an observational study. Braz J Phys Ther 2019;23:527–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Regan E, Middleton A, Stewart JC, et al. The six-minute walk test as a fall risk screening tool in community programs for persons with stroke: a cross-sectional analysis. Top Stroke Rehabil 2019;17:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Joshi S, Vij JS, Singh SK. Medical science retrowalking: a new concept in physiotherapy and rehabilitation. Int J Sci Res 2015;4:152–6. [Google Scholar]
- [11].Sedhom MG. Backward walking training improves knee proprioception in non-athletic males. Int J Physiother 2017;4:33–7. [Google Scholar]
- [12].Shen M, Che S, Ye D, et al. Effects of backward walking on knee proprioception after ACL reconstruction. Physiother Theory Pract 2019;21:1–8. [DOI] [PubMed] [Google Scholar]
- [13].Alghadir AH, Anwer S, Sarkar B, et al. Effect of 6-week retro or forward walking program on pain, functional disability, quadriceps muscle strength, and performance in individuals with knee osteoarthritis: a randomized controlled trial (retro-walking trial). BMC Musculoskelet Disord 2019;20:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Rashij M, Rai HR, Sivapriya R, et al. Resisted backward walking to improve gait synergism in children with hemiparetic cerebral palsy. Indian J Physiother Occup Ther 2017;11:74–8. [Google Scholar]
- [15].Wnuk B, Walusiak M, Durma AJ, et al. Effects of physiotherapy including various forms of gait exercises on a treadmill on functional efficiency in the elderly at risk of falling. Physiotherapy 2010;18:3–9. [Google Scholar]
- [16].DeMark L. Backward walking and its application in geriatric patients. Adv Gerontol 2018;31:428–32. [PubMed] [Google Scholar]
- [17].Hawkins KA, Balasubramanian CK, Vistamehr A, et al. Assessment of backward walking unmasks mobility impairments in post-stroke community ambulators. Top Stroke Rehabil 2019;26:382–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].DeMark L, Fox EJ, Spigel PM, et al. Clinical application of backward walking training to improve walking function, balance, and fall-risk in acute stroke: a case series. Top Stroke Rehabil 2019;26:497–502. [DOI] [PubMed] [Google Scholar]
- [19].Wang J, Xu J, An R. Effectiveness of backward walking training on balance performance: a systematic review and meta-analysis. Gait Posture 2019;68:466–75. [DOI] [PubMed] [Google Scholar]
- [20].Wang J, Yuan W, An R. Effectiveness of backward walking training on spatial-temporal gait characteristics: a systematic review and meta-analysis. Hum Mov Sci 2018;60:57–71. [DOI] [PubMed] [Google Scholar]
- [21].Elnahhas AM, Elshennawy S, Aly MG. Effects of backward gait training on balance, gross motor function, and gait in children with cerebral palsy: a systematic review. Clin Rehabil 2019;33:3–12. [DOI] [PubMed] [Google Scholar]
- [22].Denissen S, Staring W, Kunkel D, et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev 2019;10:CD008728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Balasukumaran T, Olivier B, Ntsiea MV. The effectiveness of backward walking as a treatment for people with gait impairments: a systematic review and meta-analysis. Clin Rehabil 2019;33:171–82. [DOI] [PubMed] [Google Scholar]
- [24].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8:336–41. [DOI] [PubMed] [Google Scholar]
- [25].Higgins JP, Altman DG, Gotzscbe PC, et al. The Cochrane Collaboration’ s tool for assessing risk of bias in randomised trials. BMJ 2011;343:889–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Caldeira PC, Soto AML, de Aguiar MCF, et al. Tumor depth of invasion and prognosis of early-stage oral squamous cell carcinoma: a meta-analysis. Oral Dis 2019;Online, doi:10.1111/odi.13194. [DOI] [PubMed] [Google Scholar]
- [27].Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, et al. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 2006;11:193–206. [DOI] [PubMed] [Google Scholar]
- [28].Rajiv Gandhi University of Health Science, Baglary S. Effects of backward walking training in stroke patients. 2013. [Google Scholar]
- [29].Choi HS, Jeon SB. Effect of backward walking training on balance capability and gait performance in patients with stroke. J Digital Convergence 2015;13:367–73. [Google Scholar]
- [30].Kim CY, Lee JS, Kim HD. Comparison of the effect of lateral and backward walking training on walking function in patients with poststroke hemiplegia: a pilot randomized controlled trial. Am J Phys Med Rehabil 2017;96:61–7. [DOI] [PubMed] [Google Scholar]
- [31].Kim K, Lee S, Lee K. Effects of progressive body weight support treadmill forward and backward walking training on stroke patients’ affected side lower extremity's walking ability. J Phys Ther Sci 2014;26:1923–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Kim KH, Lee KB, Bae YH, et al. Effects of progressive backward body weight suppoted treadmill training on gait ability in chronic stroke patients: a randomized controlled trial. Technol Health Care 2017;25:867–76. [DOI] [PubMed] [Google Scholar]
- [33].Lee BH, Jeong JG, Kim CK. Effects of backward walking training in the gait ability and foot pressure of hemiplegia patients. Journal of the Korea academia-industrial cooperation society 2014;15:7259–65. [Google Scholar]
- [34].Rose DK, DeMark L, Fox EJ, et al. A backward walking training program to improve balance and mobility in acute stroke: a pilot randomized controlled trial. J Neurol Phys Ther 2018;42:12–21. [DOI] [PubMed] [Google Scholar]
- [35].Takami A, Wakayama S. Effects of partial body weight support while training acute stroke patients to walk backwards on a treadmill: a controlled clinical trial using randomized allocation. J Phys Ther Sci 2010;22:177–87. [Google Scholar]
- [36].Weng CS, Wang J, Pan XY, et al. Effectiveness of backward walking treadmill training in lower extremity function after stroke. Zhonghua Yi Xue Za Zhi 2006;86:2635–8. [PubMed] [Google Scholar]
- [37].Yang YR, Yen JG, Wang RY, et al. Gait outcomes after additional backward walking training in patients with stroke: a randomized controlled trial. Clin Rehabil 2005;19:264–73. [DOI] [PubMed] [Google Scholar]
- [38].Hoogkamer W, Meyns P, Duysens J. Steps forward in understanding backward gait: from basic circuits to rehabilitation. Exerc Sport Sci Rev 2014;42:23–9. [DOI] [PubMed] [Google Scholar]
- [39].Joshi S, Singh SK, Vij JS. Effect of retrowalking, a non-pharmacological treatment on pain, disability, balance and gait in knee osteoarthritis: a randomized controlled trial. Indian Journal of Public Health Research & Development 2019;10:214–9. [Google Scholar]
- [40].Zhang X, Zhang Y, Gao X, et al. Investigating the role of backward walking therapy in alleviating plantar pressure of patients with diabetic peripheral neuropathy. Arch Phys Med Rehabil 2014;95:832–9. [DOI] [PubMed] [Google Scholar]
- [41].Grobbelaar R, Venter R, Welman KE. Backward compared to forward over ground gait retraining have additional benefits for gait in individuals with mild to moderate Parkinson's disease: a randomized controlled trial. Gait Posture 2017;58:294–9. [DOI] [PubMed] [Google Scholar]
- [42].Cappellini G, Sylos-Labini F, MacLellan MJ, et al. Backward walking highlights gait asymmetries in children with cerebral palsy. J Neurophysiol 2018;119:1153–65. [DOI] [PubMed] [Google Scholar]
- [43].Dufek J, House A, Mangus B, et al. Backward walking: a possible active exercise for low back pain reduction and enhanced function in athletes. J Exerc Physiol Online 2011;14:17–26. [Google Scholar]
- [44].Thomas KS, Hammond M, Magal M. Graded forward and backward walking at a matched intensity on cardiorespiratory responses and postural control. Gait Posture 2018;65:20–5. [DOI] [PubMed] [Google Scholar]
- [45].Chaloupka EC, Kang J, Mastrangelo MA, et al. Cardiorespiratory and metabolic responses during forward and backward walking. J Orthop Sports Phys Ther 1997;25:302–6. [DOI] [PubMed] [Google Scholar]
- [46].Wallis JA, Webster KE, Levinger P, et al. A walking program for people with severe knee osteoarthritis did not reduce pain but may have benefits for cardiovascular health: a phase II randomised controlled trial. Osteoarthr Cartil 2017;25:1969–79. [DOI] [PubMed] [Google Scholar]
- [47].Manisha R, Tushar P, Anjumol V. Efficacy of backward walking on patients with osteoarthritis of knee on quadriceps strength, pain and physical functions. Indian J Physiother Occup Ther Int J 2014;8:192–6. [Google Scholar]
- [48].Louie DR, Eng JJ. Berg Balance Scale score at admission can predict walking suitable for community ambulation at discharge from inpatient stroke rehabilitation. J Rehabil Med 2018;50:37–44. [DOI] [PubMed] [Google Scholar]
- [49].Jeon YJ, Kim GM. Comparison of the berg balance scale and fullerton advanced balance scale to predict falls in community-dwelling adults. J Phys Ther Sci 2017;29:232–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


