Abstract
Gallbladder wall thickening (GBWT) is rarely reported in children with acute Epstein-Barr virus (EBV) infection. We present a child with EBV infection who was found on point-of-care ultrasound to have GBWT without signs of cholecystitis that subsequently resolved without intervention. We expect the proliferation of mobile and handheld sonography to increase the number of bedside examinations in febrile children. This, in turn, will increase the incidence of GBWT found in patients with EBV infection and without right upper quadrant pain. Prospective study is needed to define the incidence of GBWT in children with EBV infection.
Keywords: hepatitis and other GI infections, hepatitis other, infection (gastroenterology), radiology
Background
The majority of primary Epstein-Barr virus (EBV) infections are asymptomatic. Due to its high prevalence worldwide, EBV remains a major cause of morbidity in children and young adults. The typical clinical manifestation is infectious mononucleosis, characterised by fever, tonsillitis and lymphadenopathy.1 Hepatitis, usually mild and asymptomatic, appears in approximately 90% of acute EBV infection.1
Gallbladder wall thickening (GBWT) and acute acalculous cholecystitis (AAC) are rarely reported in children with acute EBV infection.2–6 We present a child with EBV infection who was found on point-of-care ultrasound (POCUS) to have GBWT.
Case presentation
A 2-year-old child presented to the paediatric emergency department with a chief complaint of bilateral periorbital swelling. Her previous medical history was unremarkable—she was born at term and had been otherwise healthy and developed normally. She was of Jewish ethnicity. She was living with her parents and sibling, had no sick contacts or significant family history.
On presentation, she was afebrile and mildly tachycardic to 130 beats per minute. Oxygen saturation was 99% in room air. She was well appearing and comfortable, with a faint, blanching, maculopapular rash on chest, abdomen and lower extremities. She had a full, non-tender abdomen with splenomegaly, enlarged bilateral submandibular nodes, mild oropharyngeal erythema and oedema to the face and lower legs.
Initial evaluation included complete blood count (CBC) significant for mild normocytic anaemia, a normal leucocyte count (9200/mm3 (normal range 5–13 K/mm3)) with a lymphocytic (61.8%) and monocytic (22%) differential and C reactive protein mildly elevated at 1.55 mg/dL (normal range <0.5 mg/dL). Urinalysis, erythrocyte sedimentation rate and basic chemistries were unremarkable. Liver enzymes were elevated (alanine transaminase 122 U/L (normal range 0–55 U/L), aspartate aminotransferase 110 U/L (normal range 5–34 U/L), alkaline phosphatase 312 U/L (normal range 62–288 U/L)), while gamma-glutamyl transferase and bilirubin were normal. Chest X-ray was unremarkable.
POCUS of the abdomen was performed to evaluate elevated liver enzymes and periorbital oedema. Both E-FAST and hepatobiliary windows were reviewed. GBWT to a wall thickness of 1 cm was noted (figures 1 and 2). Fanning through the gallbladder showed an absence of stones or polyps (video 1). There was no tenderness on the sonographic examination.
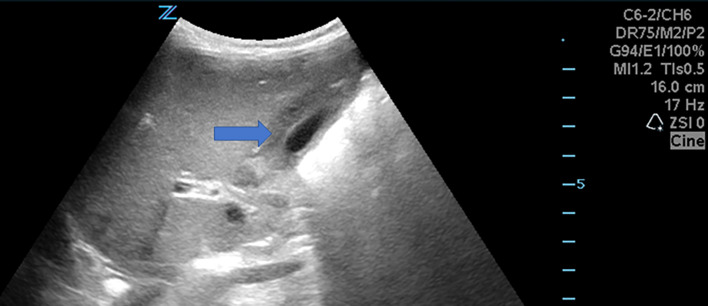
Figure 1.
Gallbladder wall thickness of about a centimetre, as indicated by the arrow. To the left of the gallbladder is the liver.
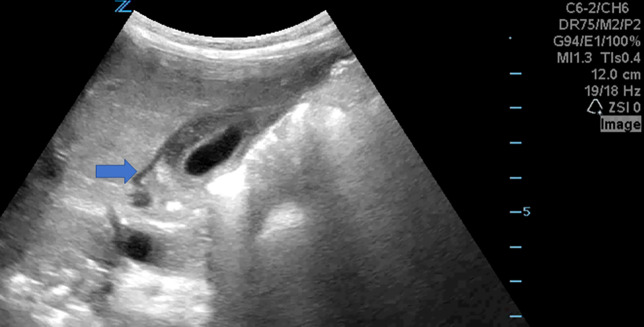
Figure 2.
A small amount of free fluid around the gallbladder, as indicated by the arrow.
video 1.
Learning points.
Gallbladder wall thickening (GBWT) and acute acalculous cholecystitis (AAC) may be part of the clinical picture of acute Epstein-Barr virus (EBV) infection, especially in females.
Many cases of EBV-related GBWT may be undiagnosed.
In the absence of signs of cholecystitis, GBWT per se should not prompt surgical consultation or intervention in patients with acute EBV.
The possibility that a true AAC could develop during primary EBV infection should be considered.
She was admitted to the hospital for further evaluation. On hospital day 1, she developed a fever to 40.1°C. Further laboratory evaluation revealed normal anti-streptolysin O and viral hepatitis serologies. Epstein-Barr viral capsid antigen (VCA) IgG and IgM were both positive, with Epstein-Barr nuclear antigen (EBNA) IgG negative. Cytomegalovirus (CMV) IgG and IgM (confirmed on Vitek Immunodiagnostic Assay System (VIDAS) platform) were positive, but CMV IgG avidity index was high borderline (0.6), indicating active EBV infection and past CMV infection with probable cross-reactive IgM. She received only antifebrile treatment and was discharged home after a 48-hour hospitalisation.
Her clinical presentation and serologies were consistent with acute EBV infection. At no point, prior to or during hospitalisation did she complain of abdominal pain.
Outcome and follow-up
Outpatient abdominal ultrasound 6 weeks after discharge showed continued splenomegaly and a normal gallbladder. Repeat liver function tests at that point had normalised.
Discussion
Wall thickness is assessed through the anterior wall of the gallbladder to avoid the acoustic enhancement artefact that obscures the posterior wall.7 Normal wall thickness is 3 mm— figure 1 shows significant wall thickness in our patient as indicated by the arrow. Figure 2 shows a small amount of pericholecystic fluid, as indicated by the arrow.
Distension and thickening of the gallbladder in the absence of cholelithiasis and in the clinical setting of right upper quadrant pain is described as AAC. AAC is a well-recognised but poorly defined diagnosis which occurs in a wide variety of clinical situations, such as trauma, major surgery, burns, sepsis, systemic vasculitis, nephrotic syndrome, specific infections and others.8–10 Inflammatory symptoms (right upper quadrant abdominal pain or positive Murphy sign) are characteristic of AAC, while distension of gallbladder without inflammation is generally referred to as gallbladder hydrops.8 Diagnostic ultrasound imaging criteria for AAC include wall thickening as per above, biliary sludge, hydrops (gallbladder distension) and pericholecystic fluid.11 AAC from viral illness is rare in children but has been described in viral hepatitis, primary CMV infection, EBV infection2–6 and human herpes virus type 6 infection.12–14
GBWT not described as AAC has been found in a number of conditions. In a series of 67 children with GBWT, only 4 were found to have EBV.15 In a literature review by Hamdy in 2014, 14 paediatric patients (≤18 years) with primary EBV infection with gallbladder involvement were summarised.9 In this series, eight were classified as having AAC, while four were noted to have ‘gallbladder thickening’ and two were classified as having hydrops of the gallbladder.9 Branco reports on a 16-year old with EBV infection and AAC that presented as mild right upper quadrant pain.4 Lagona et al described a similar case of AAC due to EBV in a 4-year-old girl who presented with cholestatic jaundice, prolonged fever and severe abdominal pain.3 Thus, AAC and GBWT may lie on opposite ends of a spectrum of illness.
GBWT, as a function of fluid retention, has been shown to be a marker of severity in Dengue infection.16 Similarly, Yamada studied 39 adults with mononucleosis and found a positive correlation between extent of GBWT (present in 15% of their cohort) and lower levels of serum protein and albumin, as well as with a longer hospitalisation.17 Barlow et al also suggested that in EBV infection, GBWT may reflect the severity of cholestatic hepatitis.6 Thus, location on the spectrum between GBWT and AAC may be indicative of severity of EBV infection. Additional ultrasonographic findings such as distention and pericholecystic fluid may rise further suspicion for AAC. Regardless of terminology, prompt diagnosis of the condition is important to avoid unnecessary procedures and antibiotic treatment.
While both AAC and GBWT are rare in EBV infection, the literature reports almost exclusively on EBV-related AAC. A retrospective cohort study from Seoul showed that GBWT is more common in the setting of primary EBV than previously reported.18 GBWT in the setting of EBV infection has never been found incidentally on POCUS. At no point did our patient have a clinical picture of acute cholecystitis—she did not complain of abdominal pain nor was she jaundiced, and she had normal CBC and inflammatory markers. In the pre-POCUS era, her clinical picture would likely have precluded radiologist-performed sonography as described in the case series cited above. Thus, we postulate that GBWT is underdiagnosed in patients with infectious mononucleosis.
Interestingly, the patient in our case, as in the most of the previously published cases, is female. Similarly, in a literature review by Agergaard, 26 of 27 patients with AAC in both adult and paediatric EBV infections were females.5 The reason for the predominance of female cases, as well the exact pathophysiology of the condition requires further study.
In conclusion, we present a case of a child who presented with EBV infection and was found incidentally on POCUS to have GBWT. Many cases of EBV-related GBWT may be undiagnosed. We expect the proliferation of mobile and handheld sonography to increase the number of bedside examinations and, in turn, the number of cases of GBWT found in patients with EBV infection without right upper quadrant pain. Prospective study is needed to define the incidence of GBWT in children with EBV infection.
Footnotes
Contributors: ES recorded the image and cared for the child in the emergency room. AG cared for the child in the ward. Both authors wrote key sections of the manuscript, involved in revision and approved the final manuscript. Both authors approved this revised draft.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Johannsen EC, Kaye KM. Epstein-Barr Virus (Infectious Mononucleosis, Epstein-BarrVirus–Associated Malignant Diseases, and Other Diseases) In: Bennett J, Blaser J, eds Mandell, Douglas, and Bennett's principles and practice of infectious diseases, 2020: 1872–90. [Google Scholar]
- 2.Poddighe D, Cagnoli G, Mastricci N, et al. Acute acalculous cholecystitis associated with severe EBV hepatitis in an immunocompetent child. Case Rep Child Meml Hosp Chic 2014;2014:bcr2013201166 10.1136/bcr-2013-201166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lagona E, Sharifi F, Voutsioti A, et al. Epstein-Barr virus infectious mononucleosis associated with acute acalculous cholecystitis. Infection 2007;35:118–9. 10.1007/s15010-007-6115-y [DOI] [PubMed] [Google Scholar]
- 4.Branco L, Vieira M, Couto C, et al. Acute acalculous cholecystitis by Epstein-Barr virus infection: a rare association. Infect Dis Rep 2015;7:6184. 10.4081/idr.2015.6184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agergaard J, Larsen CS. Acute acalculous cholecystitis in a patient with primary Epstein-Barr virus infection: a case report and literature review. Int J Infect Dis 2015;35:67–72. 10.1016/j.ijid.2015.04.004 [DOI] [PubMed] [Google Scholar]
- 6.Barlow G, Kilding R, Green ST. Epstein-Barr virus infection mimicking extrahepatic biliary obstruction. J R Soc Med 2000;93:316–8. 10.1177/014107680009300612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsung JW, Raio CC, Ramirez-Schrempp D, et al. Point-Of-Care ultrasound diagnosis of pediatric cholecystitis in the ED. Am J Emerg Med 2010;28:338–42. 10.1016/j.ajem.2008.12.003 [DOI] [PubMed] [Google Scholar]
- 8.Fishman DS, Gilger MA. Diseases of the Gallbladder In: Wyllie RMD, Hyams J, MMD K, eds Pediatric gastrointestinal and liver disease, 2016: 977–89e6. [Google Scholar]
- 9.Hamdy RF, Stein RE, Larru B, et al. Gallbladder wall thickening in an adolescent with acute mononucleosis: a case report and brief review of the literature. J Pediatric Infect Dis Soc 2015;4:267–71. 10.1093/jpids/piu023 [DOI] [PubMed] [Google Scholar]
- 10.Dinulos J, Mitchell DK, Egerton J, et al. Hydrops of the gallbladder associated with Epstein-Barr virus infection: a report of two cases and review of the literature. Pediatr Infect Dis J 1994;13:924–9. 10.1097/00006454-199410000-00014 [DOI] [PubMed] [Google Scholar]
- 11.Poddighe D, Sazonov V. Acute acalculous cholecystitis in children. World J Gastroenterol 2018;24:4870–9. 10.3748/wjg.v24.i43.4870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maudgal DP, Wansbrough-Jones MH, Joseph AE. Gallbladder abnormalities in acute infectious hepatitis. A prospective study. Dig Dis Sci 1984;29:257–60. 10.1007/BF01296260 [DOI] [PubMed] [Google Scholar]
- 13.Gora-Gebka M, Liberek A, Bako W, et al. Acute acalculous cholecystitis of viral etiology--a rare condition in children? J Pediatr Surg 2008;43:e25–7. 10.1016/j.jpedsurg.2007.10.073 [DOI] [PubMed] [Google Scholar]
- 14.Gomes MM, Antunes H, Lobo AL, et al. Acute Alithiasic cholecystitis and human herpes virus type-6 infection: first case. Case Rep Pediatr 2016;2016:9130673:4. 10.1155/2016/9130673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JH, No YE, Lee YJ, et al. Acalculous diffuse gallbladder wall thickening in children. Pediatr Gastroenterol Hepatol Nutr 2014;17:98–103. 10.5223/pghn.2014.17.2.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pothapregada S, Kullu P, Kamalakannan B, et al. Is ultrasound a useful tool to predict severe dengue infection? Indian J Pediatr 2016;83:500–4. 10.1007/s12098-015-2013-y [DOI] [PubMed] [Google Scholar]
- 17.Yamada K, Yamada H. Gallbladder wall thickening in mononucleosis syndromes. J Clin Ultrasound 2001;29:322–5. 10.1002/jcu.1042 [DOI] [PubMed] [Google Scholar]
- 18.Yi DY, Kim JY, Yang HR. Ultrasonographic gallbladder abnormality of primary Epstein-Barr virus infection in children and its influence on clinical outcome. Medicine 2015;94:e1120. 10.1097/MD.0000000000001120 [DOI] [PMC free article] [PubMed] [Google Scholar]