Abstract
Background
Fulminant cardiac involvement in COVID-19 patients has been reported; the underlying suspected mechanisms include myocarditis, arrhythmia, and cardiac tamponade. In parallel, atrial fibrillation is common in the elderly population which is at particularly high risk for COVID-19 morbidity and mortality.
Case summary
A 72-year-old male SARS-CoV2-positive patient was admitted to the intensive care unit due to delirium and acute respiratory failure. Atrial fibrillation known from history was exacerbated, and made complex rate and rhythm control necessary. Progressive heart failure with haemodynamic deterioration and acute kidney injury with the need for continuous renal replacement therapy were further aggravated by pericardial tamponade.
Discussion
Treatment of acute heart failure in COVID-19 patients with a cytokine storm complicated by tachycardic atrial fibrillation should include adequate rate or rhythm control, and potentially immunomodulation.
Keywords: COVID-19, Atrial fibrillation, Multiorgan failure, Cardiac tamponade, Case report
Learning points
Atrial fibrillation might pose an additional risk factor for unfavourable outcome in COVID-19 patients.
Consider continuous cardio-selective beta-blockers in COVID-19 patients with supraventricular, non-compensatory tachycardia.
Introduction
Coronavirus disease (COVID)-19 is an emerging pandemic manifesting from asymptomatic infection to acute respiratory distress syndrome (ARDS) and multiorgan failure.1 Various phenotypes have been described, including a procoagulatory state, acute kidney injury (AKI), or hyperinflammatory syndromes such as a cytokine storm.2,3 Myocardial involvement is a common finding in critically ill patients, the aetiology being coronary microvascular ischaemia, stress cardiomyopathy, or sometimes viral myocarditis.4 We report on an elderly male COVID-19 patient presenting with ARDS and fulminant heart failure aggravated by atrial fibrillation (AF) with fatal outcome.
Timeline
| Day | Events |
|---|---|
| –6 to 0 | Patient suffering from fever, fatigue, and delirium tested positive for SARS-CoV2; home quarantine |
| 1 | Worsening of symptoms, subclinical hypoxaemia, ICU admission, and intubation; haemodynamically unstable, requiring catecholamine support; intermittent tachycardic atrial fibrillation |
| 2–3 | Continuous renal replacement therapy with immunoadsorption; clinically stable under ARDS-adapted ventilation, catecholamine support, and landiolol |
| 4 | Immunoadsorption stopped due to manufacturer’s demands |
| 5 | Haemodynamic deterioration and intermittent tachycardic atrial fibrillation in spite of exhausted therapeutic options |
| 6 | Pericardial tamponade successfully drained |
| 7–8 | Deteriorating haemodynamics |
| 9 | Death from multiorgan failure |
Case presentation
After having developed fever and fatigue, a 72-year-old male patient (body mass index 29.2) was diagnosed with COVID-19 and put in quarantine at home. Clinical worsening resulted in delirium. After 6 days, emergency medical services found the patient severely hypoxic (SpO2 65%) despite his not complaining about dyspnoea. Oxygen was administered and the patient was transported to a designated COVID-19 pulmonary intensive care unit (ICU).
History revealed a non-insulin-dependent diabetes mellitus type 2 (recent Hba1c 6.4%), aortic dissection type B (stable over time in various CTs), persistent AF, a smoking history (cessation 20 years ago), and chronic obstructive sleep apnoea syndrome (no therapy). Chronic medication consisted of apixaban (5 mg twice daily), gabapentin (150 mg twice daily), bisoprolol (5 mg twice daily), and metformin (500 mg twice daily), and did not include angiotensin-converting enzyme inhibitors or angiotensin receptor blockers.
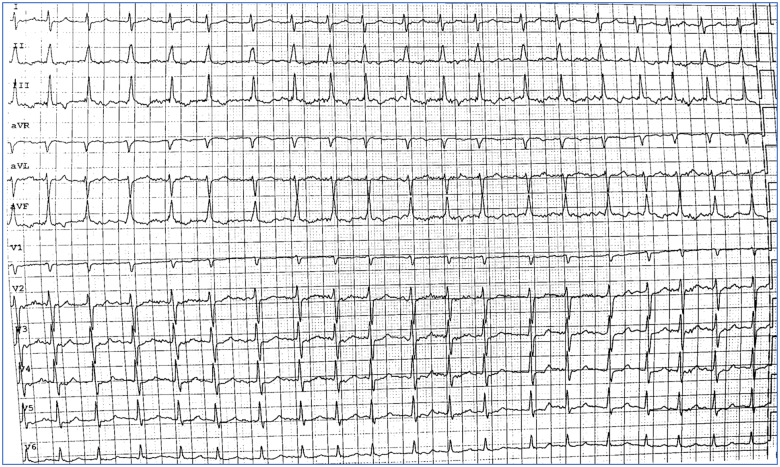
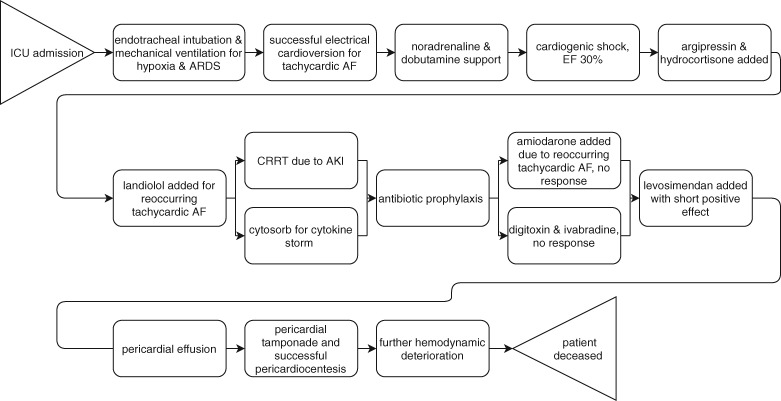
Upon arrival, the patient was normotensive with an irregular heart rhythm, appearing exhausted and perspiring, but not subjectively dyspnoeic. Auscultation revealed bilateral medium to coarse crackle sounds. He was intubated due to severe hypoxaemia [Horovitz index 111, positive end-expiratory pressure (PEEP) 18 cmH2O, pressure control max. 32 cmH2O, FiO2 80%]. Sufficient oxygenation and normocapnia (pO2 89 mmHg, pCO2 45 mmHg) were achieved. Tachycardic AF up to 180 b.p.m. (Figure 1) was successfully electrically cardioverted. However, bedside echocardiography showed globally reduced left ventricular systolic function (LVSF) and ejection fraction (EF, 30%), necessitating noradrenaline and dobutamine support (initial dosages 0.32 μg/kg/min and 6.67 μg/kg/min, respectively). Pulse contour cardiac output monitoring was established (initial values: cardiac index 1.6 L/min/m2, cardiac function index 2.2 L/min, global end-diastolic volume index 791 mL/m2, pulse pressure variation 14%, extra-vasal lung water index 35.3 mL/kg, pulmonary–vascular permeability index 7.2) to guide further treatment, including careful volume resuscitation, argipressin (1.8 IU/h), hydrocortisone (8 mg/h), and continuous landiolol (initial dose 8 μg/kg/min) for control of reoccurring tachycardic AF.
Figure 1.
Electrocardiogram (25 mm/s) with atrial fibrillation as described in the text.
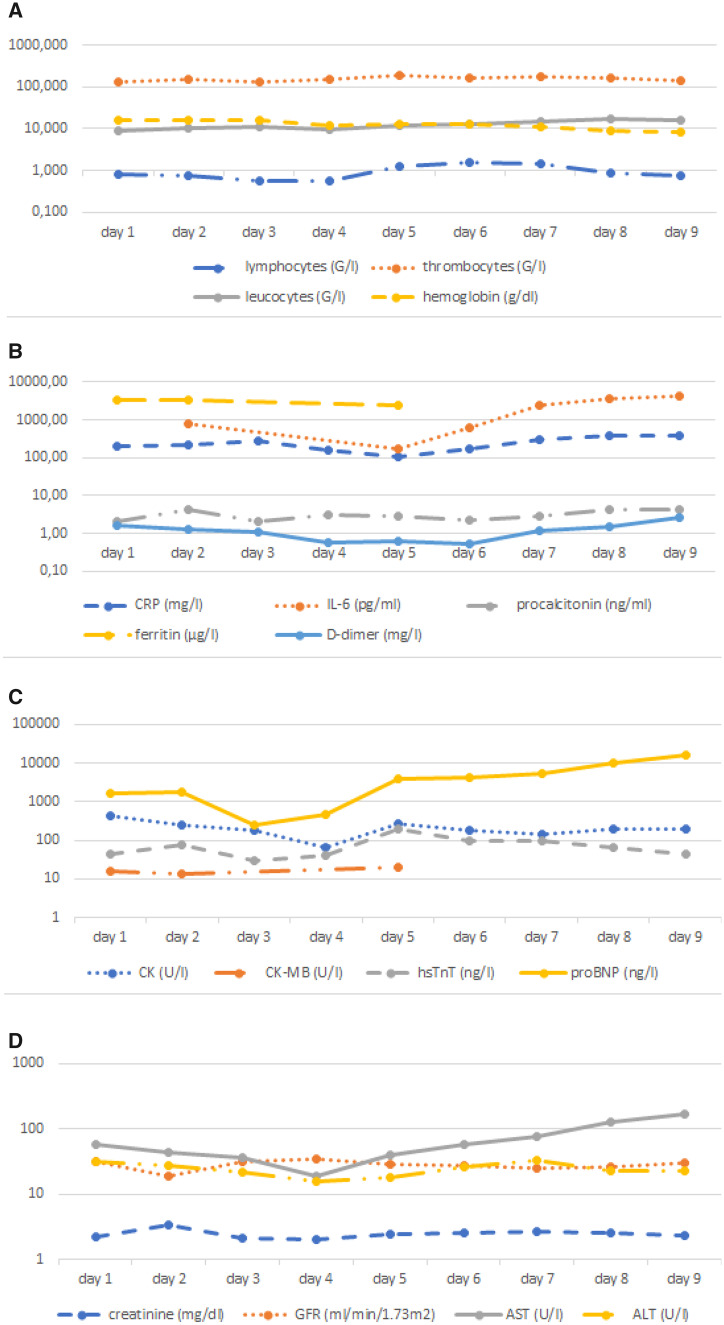
A chest X-ray showed bilateral consolidations compatible with ARDS (Figure 2). Laboratory results showed AKI. Continuous renal replacement therapy (CRRT) was established and upgraded with an immunoadsorbant filter (Cytosorb®) for 48 h to counteract a suspected cytokine storm mirrored by rising interleukin-6 (IL-6) levels. The initial pro-brain natriuretic peptide (BNP) was 1612 ng/L, ultimately reaching 10-fold levels. High sensitivity troponin T (hs-TnT) values were undulant during the entire stay, with maximum levels of 200 ng/L. For the development of laboratory values over time, see Figure 3. Due to organizational reasons and potential cardiac side effects, it was chosen not to administer experimental therapeutics such as hydroxychloroquine, tocilizumab, or antiviral agents.
Figure 2.
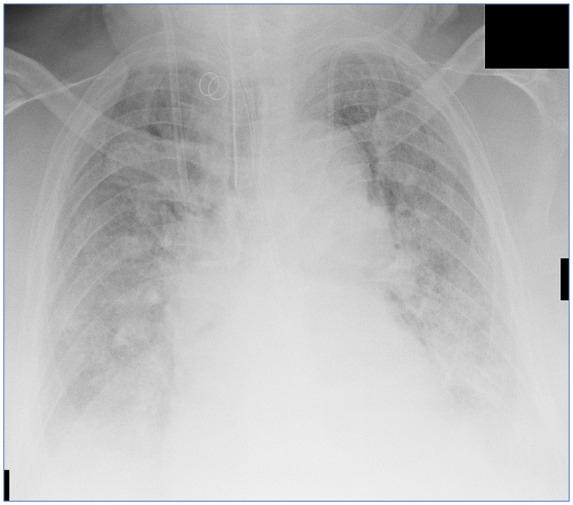
Chest X-ray showing bilateral consolidations as in acute respiratory distress syndrome as described in the text.
Figure 3.
Laboratory values over time. (A) Blood count; (B) immune response; (C) cardiac markers; (D) renal and hepatic values. ALT = alanine aminotransferase; AST = aspartate aminotransferase; BNP = brain natriuretic peptide; CK = creatine kinase; CRP = C-reactive protein; GFR = glomerular filtration rate; hsTnT = high sensitivity troponin-T; IL-6 = interleukin-6.
More frequent tachycardic AF episodes did not respond to electrical cardioversion, escalation of landiolol (up to 40 μg/kg/min without effect of further escalation), or addition of amiodarone (300 mg in 30 min and 38 mg/h over 24 h thereafter). Also, digitoxin (0.25 mg daily) and ivabradine (5 mg twice daily)—initially showing promising results—ultimately proved ineffective. Progressing heart failure seemed to be mainly dependent on tachycardic AF. Levosimendan (10 μg/kg/min for 10 min and 0.2 μg/kg/min for 24 h thereafter) led to a transient positive effect that only lasted ∼24 h. In echocardiographic controls, pericardial effusion (circumference, 2–3 cm, Figure 4) developed in 48 h, leading to pericardial tamponade that was successfully drained (a SARS-CoV-2 test from the fluid was negative). After pericardiocentesis, haemodynamics improved only transiently, and LVSF/EF deteriorated rapidly. At this stage, an ultima ratio treatment option would have been veno-arterial extracorporeal membrane oxygenation (VA-ECMO). However, existing literature surrounding the role of VA-ECMO in the treatment of COVID-19-associated cardiogenic shock is scarce. Due to the multiple comorbidities, resource availability, and the perceived risk–benefit ratio, a decision against ECMO was made. In a multidisciplinary way, a do not resuscitate order was agreed on. Nine days after ICU admission, the patient died from multiorgan failure. Figure 5 gives an overview of the entire case.
Figure 4.
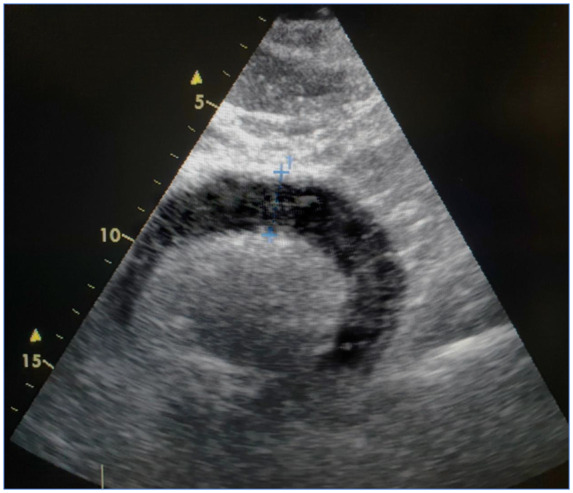
Pericardial tamponade seen in the subxiphoidal echocardiographic view.
Figure 5.
Overview of the case presentation. AF = atrial fibrillation; ARDS = acute respiratory distress syndrome; CRRT = continuous renal replacement therapy; EF = ejection fraction; ICU = intensive care unit.
Discussion
Cardiac (co-)injury has already been duly noted as a crucial possible COVID-19 characteristic: most reports include perimyocarditis and de novo or aggravated heart failure.5 Pericardial effusion or tamponade appear in up to 5% of cases.6–8 In our patient, perimyocarditis and pericardial effusion might have been triggered by the underlying mechanisms ranging from potential direct viral invasion of the myocardium9 and angiotensine-converting enzyme 2 signal pathways to a cytokine storm.2,5,10 With extreme levels of IL-6, a state of virally driven hyperinflammation can be suspected in our case. In the final disease stage, the reported patient was positive for secondary haemophagocytic lymphohistiocytosis (sHLH) as suggested by Mehta et al.2,11 After discontinuation of immunoadsorption, IL-6 values exacerbated, strengthening this theory. In future similar cases, the IL-6 antibody tocilizumab could be a therapeutic option, if available.
The arrhythmogenic effect of COVID-19 might still be under-reported and was noted in up to 17% of patients; the literature still lacks more precise differentiation.5 Importantly, the presence of AF together with inadequate rate control might have a negative impact on patients’ prognosis. With a large prevalence of AF in the general, and especially the elderly, population12 and the known connection of arrhythmic burden and viral disease,13 AF may influence mortality. While there may or may not be a direct causal relationship between AF and COVID-19, the often-needed extensive catecholamine support can either initiate or aggravate AF, therefore inducing a vicious circle of cardiac injury through tachyarrhythmogenic and adrenergic stress.4,5,10 A possible treatment add-on in this dilemma would be milrinone, a synthetic non-catecholamine phosphodiesterase type III inhibitor. When compared with dobutamine, milrinone is associated with less tachycardia and increases the cardiac index, but reduces arterial blood pressure and pulmonary vascular resistance (the reason why it is often combined with noradrenaline and vasopressin).14 Such an approach might represent an alternative in cardiogenic shock with a high ventricular rate.
Besides management of respiratory complications, comorbidities of COVID-19 patients are known to be important risk factors for worse outcome5—and AF should be recognized as one of them. In patients with tachyarrhythmia, short-acting cardioselective beta-blockers may be a good initial choice for heart rate control. Frequent reassessment of cardiac function by echocardiography will help to adapt treatment and to recognize complications in the course of the disease.
Conclusion
Treatment of acute heart failure in COVID-19 patients with a cytokine storm complicated by tachycardic AF should include adequate rate or rhythm control, and potentially immunomodulation.
Lead author biography

Sebastian Schnaubelt is a resident physician at the Emergency Department of the Medical University of Vienna, Austria. His research focuses on arrhythmia, angiology and cardiopulmonary resuscitation under the lead of Prof. Hans Domanovits and Prof. Michael Holzer.
Acknowledgements
We thank Professor Dr Anton Laggner, Professor Dr Sylvia Hartl, and the physician and nursing staff of the pulmonary ICU for their support.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient’s guardians in line with COPE guidance.
Conflicts of interest: none declared.
References
- 1. Weiss P, Murdoch DR.. Clinical course and mortality risk of severe COVID-19. Lancet 2020;395:1014–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ.. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395:1033–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B.. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chapman AR, Bularga A, Mills NL.. High-sensitivity cardiac troponin can be an ally in the fight against COVID-19. Circulation 2020;doi: 10.1161/CIRCULATIONAHA.120.047008. [DOI] [PubMed] [Google Scholar]
- 5. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B.. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hua A, O’Gallagher K, Sado D, Byrne J.. Life-threatening cardiac tamponade complicating myo-pericarditis in COVID-19. Eur Heart J 2020;doi: 10.1093/eurheartj/ehaa253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C.. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, Li C.. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol 2020;55:327–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, Sepe PA, Resasco T, Camporotondo R, Bruno R, Baldanti F, Paolucci S, Pelenghi S, Iotti GA, Mojoli F, Arbustini E.. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail 2020;doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. South AM, Diz D, Chappell MC.. COVID-19, ACE2, and the cardiovascular consequences. Am J Physiol Heart Circ Physiol 2020;318:H1084–H1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rizzo P, Vieceli Dalla Sega F, Fortini F, Marracino L, Rapezzi C, Ferrari R.. COVID-19 in the heart and the lungs: could we ‘Notch’ the inflammatory storm? Basic Res Cardiol 2020;115:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindriks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P.. ESC Scientific Document Group. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;37:2893–2962. [DOI] [PubMed] [Google Scholar]
- 13. Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C.. Cardiac and arrhythmic complications in Covid-19 patients. J Cardiovasc Electrophysiol 2020;31:1003–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ginwalla M, Tofovic DS.. Current status of inotropes in heart failure. Heart Fail Clin 2018;14:601–616. [DOI] [PubMed] [Google Scholar]