Abstract
Background
The coronavirus disease 2019 [COVID-19] pandemic is affecting lives worldwide. The influence of inflammatory bowel disease [IBD] medication and IBD itself on COVID-19 is controversial. Additionally, IBD-focused guidance is scarce.
Objective
Our aims were to determine COVID-19 prevalence/exposure, perception and information sources, medication compliance, patient behaviour and physician contact among patients with IBD compared with non-IBD controls.
Methods
A cross-sectional anonymous survey of patients with IBD [N = 415] at one university IBD clinic and one gastroenterology practice, matched 4:1 with control participants [N = 116], was performed.
Results
Patients with IBD had a high fear of infection. This was more pronounced in patients taking immunosuppressants and it extended to hospitals, private practices and public places, such as supermarkets. IBD patients reported leaving their homes less frequently than their peers without IBD. A total of 90% of patients with IBD reported washing their hands more frequently. Patients taking immunosuppressants were concerned about interactions between medication and COVID-19, whereas patients taking 5-aminosalicylates were not. Nonetheless, 96.4% of patients adhered to continuing their medication. Patients sought guidance primarily from television and internet news sites. Video consultations were found to be a suitable solution for a subset of patients who are young, have a high level of fear and leave their home less frequently than their peers, whereas overall acceptance of video consultations was limited.
Conclusion
Patients with IBD are significantly more affected by the COVID-19 pandemic than their non-IBD peers, but they continue to adhere to their medication regimens. IBD-focused COVID-19 information should be actively conveyed.
Keywords: Inflammatory bowel disease, COVID-19, patient behaviour
1. Introduction
The coronavirus disease 19 [COVID-19], a new form of severe acute respiratory syndrome [SARS], is caused by the novel coronavirus SARS-CoV-2. On 12 March 2020, after an unprecedented worldwide spread following its outbreak in China in December 2019, SARS-CoV-2 was announced as a global pandemic by the World Health Organization [WHO].1 It infected more than 5 million people in the subsequent weeks and has become a substantial threat to public health and society, worldwide. Governments around the world have responded with surges in new public policies, and one-third of the world’s population has now been subjected to social restrictions ranging from bans on public assembly to complete lockdowns.2
Symptoms of COVID-19 comprise fever, aches, dry cough and shortness of breath; however, life-threatening conditions, ranging from respiratory failure to multi-organ dysfunction, may also result. Increasing evidence indicates that older and immunocompromised patients, as well as patients with existing comorbidities, are at higher risk of more complicated or even lethal courses of COVID-19.3
Although there is no evidence to date of higher susceptibility of patients with IBD to COVID-19,4 IBD medications may pose a threat. IBD treatments often rely on immunosuppressive therapy regimens to induce and maintain clinical remission. Opinions differ as to whether these medications should be continued or discontinued, owing to their potential to cause infectious complications; 5 however, in cytokine storm-driven inflammation immunosuppressive therapies might possibly have a protective effect.6 Moreover, experimental evidence suggests that commonly used IBD treatments may have lung protective effects.7
WHO guidance for behaviour during the COVID-19 pandemic includes basic protective measures, such as frequent hand washing; social distancing; avoiding touching of the eyes, nose and mouth; respiratory hygiene; seeking medical care early in the case of respiratory symptoms; and remaining informed.8 However, IBD-specific guidance for patients is lacking.
In our daily outpatient practice visits, there is notable uncertainty among patients with IBD regarding the influence of their disease and medication on COVID-19 disease. To date, there is a lack of data regarding how this uncertainty translates into the daily lives of our patients.
We assessed the COVID-19 prevalence/exposure, perception and information sources, patient behaviour, physician contact and medication compliance among patients with IBD in April 2020, by using a cross-sectional anonymous survey, and we compared the results with those from a non-IBD control cohort.
2. Methods
2.1. Patient recruitment
Patients from the IBD outpatient clinic of Jena University Hospital [Jena, Germany] and an IBD-specialized gastroenterology practice in Leipzig, Germany, were identified. A total of 715 patients with IBD were asked to complete the survey. Recruitment occurred between April 2 and 17, 2020.
The survey was paper-based and focused on demographic data [age, sex, educational status and profession], pre-existing medical conditions, current IBD therapy and subjective clinical disease activity, influenza vaccination status and smoking status. Patients were asked to select their most important information sources for behavioural guidance during the COVID-19 pandemic from among nine options. Eight statements concerning the coronavirus were rated on a five-point Likert-scale. Nine closed-ended questions regarding coronavirus infection status, exposure, personal protective equipment, hand hygiene, IBD medication adherence and physician contact were answered [Supplementary Material 1].
To compare opinions, concerns and behaviour, mostly healthy non-IBD participants were asked to complete a similar survey [control group]. This group consisted of healthy family members of patients with IBD [n = 75] and relatives/acquaintances of healthcare workers [n = 41].
The study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee [2020-1733-Reg]. All participants provided written informed consent before inclusion into the study.
2.2. Statistical analysis
Statistical analysis was performed in SPSS 23 [IBM] and PRISM 6 [GraphPad Software]. Statistical differences between groups were analysed with the non-parametric Mann–Whitney U-test for continuous data or Fisher’s exact test for discrete data. To analyse correlations between variables, Spearman’s correlation was used. Results with p < 0.05 in two-sided tests were considered statistically significant.
3. Results
A total of 715 patients with IBD were contacted by mail or during outpatient visits: 535 at Jena University Hospital and 180 in Leipzig. A total of 415 patients with IBD [response rate = 58.2%] and 116 non-IBD participants completed the survey, thus resulting in a 4:1 ratio of patients with IBD to controls. A similar distribution in the IBD and control groups regarding sex [approximately 55% of participants were female] and age [IBD median 45 years vs controls 48 years] was observed. Tobacco use was lower in the IBD group [IBD 15.7% vs 25.9% in the control group] [Table 1].
Table 1.
Participant demographics and characteristics
| IBD, N = 415 | Controls, N = 116 | ||
|---|---|---|---|
| Age, years, mean [min; max] | 45 [18; 82] | 48 [18;82] | |
| Age under 60 years, n [%] | 341 [82.2%] | 87 [75.0%] | |
| Sex | Female, n [%] | 227 [54.7%] | 66 [56.9%] |
| Education, n [%] | Junior high school [Hauptschule] | 43 [10.4%] | 10 [8.7%] |
| Secondary school [Realschule] | 185 [44.6%] | 47 [40.9%] | |
| High school | 53 [12.8%] | 19 [16.5%] | |
| College degree | 125 [30.1%] | 38 [33.0%] | |
| Smoker | Yes, n [%] | 65 [15.7%] | 30 [25.9%] |
| Influenza vaccination | Yes, n [%] | 175 [42.2%] | 52 [44.8%] |
| Comorbidities | |||
| Lung disease, n [%] | Asthma | 32 [7.7%] | 4 [3.4%] |
| COPD | 8 [1.9%] | 0 | |
| Other | 4 [1.0%] | 1 [0.9%] | |
| Cardiac disease, n [%] | Coronary heart disease | 13 [3.1%] | 4 [3.4%] |
| Arterial hypertension | 73 [17.6%] | 21 [18.1%] | |
| Other | 4 [1.0%] | 2 [1.7%] | |
| Liver disease, n [%] | Primary sclerosing cholangitis | 11 [2.7%] | 2 [1.7%] |
| Liver cirrhosis | 2 [0.5%] | 1 [0.9%] | |
| NAFLD | 32 [7.7%] | 2 [1.7%] | |
| Autoimmune hepatitis | 1 [0.2%] | 0 | |
| Primary biliary cholangitis | 1 [0.2%] | 1 [0.9%] | |
| Other | 0 | 2 [1.7%] | |
| Diabetes, n [%] | 23 [5.5%] | 9 [7.8%] | |
| Kidney disease, n [%] | 5 [1.2%] | 1 [0.9%] | |
| Rheumatological disease, n [%] | 29 [7.0%] | 0 | |
| Malignancy, n [%] | 8 [1.9%] | 1 [0.9%] | |
| Organ transplantation, n [%] | 2 [0.5%] | 0 | |
| Other comorbidities | 67 [16.1%] | 9 [7.8%] | |
| Number of comorbidities | 0 | 208 [50.1%] | 73 [62.9%] |
| 1 | 131 [31.6%] | 31 [26.7%] | |
| 2 | 50 [12.0%] | 10 [8.6%] | |
| 3 | 19 [4.6%] | 1 [0.9%] | |
| 4 | 5 [1.2%] | 1 [0.9%] | |
| 5 | 1 [0.2%] | 0 | |
| 7 | 1 [0.2%] | 0 |
COPD, chronic obstructive pulmonary disease; NAFLD, non-alcoholic fatty liver disease.
Patients with IBD had more comorbidities than participants in the control group. Approximately half of the surveyed IBD population had at least one comorbidity (n = 207 [49.9%]), in contrast to only 37% of the controls (n = 43 [37.1%]).
3.1. IBD characteristics and medication
The participants in the IBD group showed a nearly even distribution between Crohn’s disease [51.8%] and ulcerative colitis [46.3%]. Five patients [1.2%] had IBD unclassified [IBDU], and the disease type was not further specified by three patients [Table 2]. Clinical disease activity was assessed subjectively by the patients. A total of 56.1% of patients stated that they were in complete clinical remission, 30.6% had mild symptoms, 12% had chronically active disease and 0.5% were in a flare-up.
Table 2.
IBD patient characteristics
| n [%] | ||
|---|---|---|
| Type of IBD | Not specified | 3 [0.7%] |
| Crohn’s disease | 215 [51.8%] | |
| Ulcerative colitis | 192 [46.3%] | |
| IBDU | 5 [1.2%] | |
| Clinical activity of IBD | Remission | 233 [56.1%] |
| Mildly active | 127 [30.6%] | |
| Chronically active | 50 [12.0%] | |
| Flare | 2 [0.5%] | |
| IBD medication | ||
| Corticosteroids | 54 [13.0%] | |
| Mesalazine/sulfasalazine | 143 [34.5%] | |
| Anti-TNF | 99 [23.9%] | |
| Ustekinumab | 46 [11.1%] | |
| Vedolizumab | 49 [11.8%] | |
| JAK inhibitors | 14 [3.4%] | |
| Immunomodulators [azathioprine, 6-MP, MTX] | 70 [16.9%] | |
| Calcineurin inhibitors | 4 [1.0%] | |
| Other immunosuppression | 4 [1.0%] | |
| Total number of immunosuppressants | 0 | 149 [35.9%] |
| 1 | 212 [51.1%] | |
| 2 | 48 [11.6%] | |
| 3 | 6 [1.4%] |
IBDU, IBD unclassified; JAK, Janus kinase; MTX, methotrexate; Anti-TNF, anti-tumour necrosis factor alpha therapy; Other immunosuppression: guselkumab, eculizumab, chemotherapy for colon cancer, leflunomide.
The most common medication was 5-aminosalicylates, which were taken by one-third of the patients with IBD [34.5%], and this was followed by anti-tumour necrosis factor alpha [anti-TNF] therapy [25.5%]. However, biological agents together composed the largest group of IBD medication [46.8%]. Combination treatment with more than one immunosuppressant was used in 13% of the patients with IBD. Only 15.3% of patients in the IBD cohort were not taking any IBD therapy [Table 2].
3.2. Perception of the coronavirus pandemic
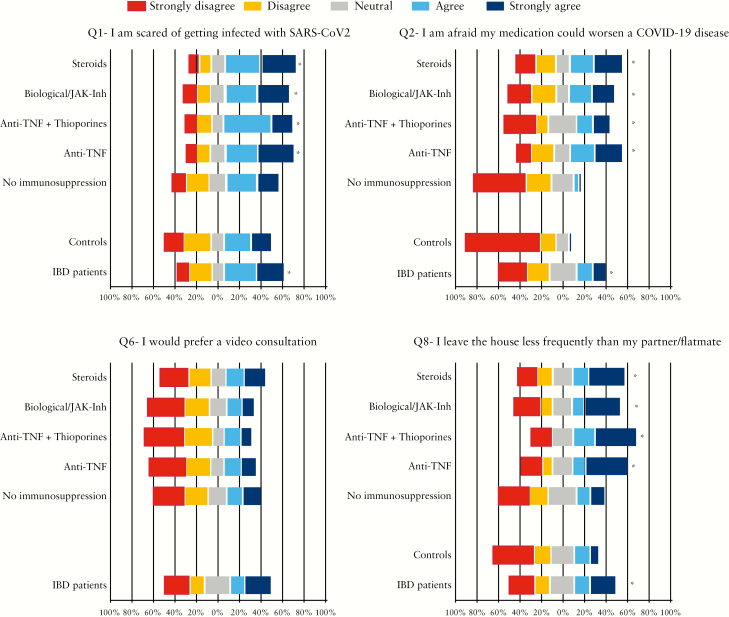
Patients with IBD were more afraid of being infected with SARS-CoV-2 (question 1 [Q1]) than participants in the control group [‘agree’ vs ‘neutral’, statistically significant, p = 0.009] [Supplementary Table 1]. This fear was more pronounced in patients taking immunosuppressants [Figure 1]. Patients with IBD were afraid of contracting SARS-CoV-2 in three different external environments: hospitals [Q3], private practice [Q4] and supermarkets [Q5] [all median ‘agree’]. In contrast, the control group did not fear these environments as much: they rated their fear of private practices [p = 0.062] or supermarkets as ‘neutral’ [p = 0.65] and they ‘disagreed’ with being afraid of being infected in hospitals [p = 0.03].
Figure 1.
Subgroup analysis of different IBD medications for Likert-scale questions 1, 2, 6 and 8. Q6 = I would prefer a video consultation over a face-to-face consultation. For questions 1, 2 and 8 all subgroups were compared to the control group. The top five bars represent subgroups of patients from the IBD group taking different medications, and the bottom two bars represent all controls and all patients with IBD [Q1, Q2, Q8] or all patients with IBD Q6. No immunosuppression = 5-aminosalicylates or no medication [Mann–Whitney U-test, *p < 0.05].
Participants in both groups ‘agreed’ that they ‘leave the house less frequently than before the coronavirus pandemic’ [Q7]. However, the control group leaned more towards a ‘neutral’ sentiment [statistically significant, p = 0.037]. Moreover, 38.2% of patients with IBD [controls 23%] indicated that they leave the house less frequently than their partners/flatmates [Q8] [statistically significant, p < 0.001].
Patients with IBD were more concerned about the negative effects of their medication on COVID-19 disease than controls [Q2]. A subgroup analysis of Q2 for medication type showed that patients taking biological agents or Janus kinase inhibitors, combination therapy [anti-TNF and thiopurines] or corticosteroids were more afraid of their medications’ effects [Figure 1]. A total of 44.1% of patients taking one, and 57.7% taking two, immunosuppressants agreed or strongly agreed with fearing a negative effect [data not shown], whereas the concern among patients with IBD taking 5-aminosalicylates or no medication was statistically not different from that of the control group [both ‘strongly disagree’].
When patients with IBD were asked whether they would prefer a video consultation over an in-person consultation [Q6], the median response was ‘disagree’. To further examine this result, we used Spearman’s correlation. Patients who had a high fear of contracting SARS-CoV-2 [weak positive correlation r = 0.293, p = 0.01], who feared a negative influence of their medication on COVID-19 [weak positive correlation, r = 0.298, p = 0.01] and who reported leaving the house less frequently [moderate positive correlation, r = 0.312, p = 0.01] were more likely to prefer a video consultation over a face-to-face appointment. Furthermore, we observed a strong age correlation: only 46.5% of patients under the age of 40 years preferred for the appointment to be in-person [r = −0.894, p = 0.015]. No correlation was seen between preference for video consultations and the number of comorbidities, number of immunosuppressants, education level, IBD clinical disease activity, IBD disease type or sex.
3.3. Coronavirus exposure and behaviour/coping mechanisms
Of all 531 participants in this survey, there was one reported case of SARS-CoV-2 infection in the control group [0.9% of the control group population]. Exposure to SARS-CoV-2-infected patients was more frequent in the control group (11 participants [10.5%] vs 7 [1.7%] in the IBD group [statistically significant, p < 0.001]) [Table 3].
Table 3.
Results of closed-ended questions and statements concerning coronavirus exposition and behaviour/coping strategy. Significant differences are shown in bold type [Fisher’s exact test, p < 0.05]
| IBD, N = 415 | Controls, N = 116 | p | ||
|---|---|---|---|---|
| ‘I was infected with SARS-CoV-2’ | Yes, % | 0% | 0.9% | 0.216 |
| ‘I had exposure to a SARS-CoV-2-infected person’ | Yes, % | 1.7% | 10.5% | <0.001 |
| ‘I reduced my medication on my own account’ | Yes, % | 3.8% | 0% | n.a. |
| ‘I wear personal protective equipment when leaving the house’ | Yes, % | 34.5% | 50.9% | 0.002 |
| If yes, ‘Did you handcraft your facemask?’ | Yes, % | 38.6% | 36.2% | 0.872 |
| ‘I wash my hands more frequently’ | Yes, % | 91.8% | 90.4% | 0.705 |
| ‘I tried to contact my physician’ | Yes, % | 25.6% | 15.9% | 0.033 |
| If yes, ‘Family physician or gastroenterologist?’ | ||||
| Family physician, % | 53.3% | 100% | ||
| Gastroenterologist, % | 46.7% | 0% | ||
| If yes, ‘Could you reach the physician?’ | Yes, % | 90.0% | 93.3% |
Of the 398 patients, 15 [3.8%] in the IBD group but no individuals in the control group reported having reduced their medication on their own account. The discontinued medications were mesalazine [n = 6], anti-TNF therapy (n = 4 [golimumab = 1, adalimumab = 3]), methotrexate, prednisolone, budesonide, allopurinol and insulin [each n = 1]. Nine out of 10 participants stated that they wash their hands more frequently than they did before the coronavirus pandemic [91.8% IBD, 90.4% controls]. Unexpectedly, 50.9% of the control group stated that they wear personal protective equipment, as compared with only 34.5% of the patients with IBD [statistically significant, p = 0.002]. Among those wearing personal protective equipment, one-third [38.6% IBD, 36.2% controls] stated that they had handcrafted the equipment.
A total of 25.6% of the IBD population in this study had attempted to contact a physician to obtain information about the coronavirus [control group = 15.9%]. Half [53.3%] of the patients with IBD had contacted their family physicians, and only 46.7% had tried to consult with their gastroenterologists. Consultation was successful 90% of the time in both groups [90% IBD, 93.3% controls].
3.4. Sources of information
The most important source of information to guide behaviour during the COVID-19 pandemic among patients with IBD was the public media [Supplementary Table 2]. Television [62.9%] and internet news sites [62.7%] were the most frequently named sources. The German public health institute for infectious diseases [Robert Koch Institute] was the third most important information source for both IBD [34.2%] and non-IBD participants [29.3%]. A total of 17.3% of patients with IBD listed physicians as an important source for information. Of note, IBD-centred information sources were not a major source of advice during the coronavirus pandemic among patients with IBD. The largest German IBD self-help organization, Deutsche Morbus Crohn/Colitis ulcerosa Vereinigung [DCCV], and IBD internet forums were respectively the third least and least frequently mentioned sources of advice in the IBD group.
4. Discussion
In this survey of more than 400 patients with IBD, we found that the fear of infection by SARS-CoV-2 was high and exceeded that in the non-IBD participants. This fear extended to hospitals and private practices as well as public places such as supermarkets. Therefore, the question arose as to whether the daily lives of patients with IBD might be influenced. Patients with IBD reported leaving their homes less frequently than they used to before the COVID-19 pandemic. This result was expected; however, this group of participants left the house even less frequently than their partners/flatmates in the same household. A total of 90% of participants said that they washed their hands more often than they did before and, therefore, followed the WHO recommendations. Paradoxically, this cautious behaviour did not translate into greater use of personal protective equipment, such as surgical masks, when leaving the home. This finding may be explained by the rapidly changing governmental COVID-19 protection policies. Alarmingly, only 42% of patients with IBD have had an influenza vaccination. Whereas SARS-CoV-2 vaccines will probably become available too late to affect the first wave of the COVID-19 pandemic,9 influenza vaccines are readily available and should be administered to avoid co-infection with COVID-19 and influenza.10
Another important finding of this study is that patients consider the possible effects of their medication on COVID-19. Patients taking 5-aminosalicylates were not afraid that their medication might worsen COVID-19, whereas patients taking immunosuppressants were concerned about negative effects. This concern increased with the total number of immunosuppressants taken. Moreover, in this group, perception of the COVID-19 pandemic was more negative, because the patients were more afraid of contracting SARS-CoV-2, and consequently left the house less frequently than patients not taking immunosuppressants. Thus, patients do factor the immunosuppressive potential of their medication into their decisions. Despite this fear, most patients remained compliant with their therapy. Only 3.8% of patients decreased their medication on their own account, which is in line with the results of a currently published online survey.11 This is a fairly low proportion, given that up to 50% medication incompliance rates have been reported in IBD.12 Five of the 15 treatments discontinued were anti-TNF agents. In light of the existing results from the Surveillance Epidemiology of Coronavirus [COVID-19] Under Research Exclusion—IBD [SECURE-IBD] registry, wherein 376 patients with IBD who were taking anti-TNF therapy and had COVID-19 had a mortality rate of only 1% [n = 3]; 13 thus, discontinuation is not supported by evidence. Moreover, one current hypothesis is that immunosuppressive treatment does not cause clinical worsening of COVID-19.14 TNFα is also overexpressed in severe respiratory distress syndrome.15 Therefore, treatment with anti-TNFs might be protective against both the severity of pulmonary disease and the recurrence of the intestinal disease in patients with IBD who are infected with COVID-19.
Normally patients with IBD do ask medical professionals for information regarding IBD diagnosis and medical therapy and ask their peers online for advice regarding daily problems and coping strategies.16,17 However, in the COVID-19 pandemic, we observed that patients with IBD primarily consulted television and internet news for guidance, whereas IBD support groups and physicians were of far lesser importance. We therefore recommend actively reaching out to patients with IBD [e.g. sending informative letters, e-mails and suggestions of reliable information sources] to provide IBD-relevant information and advice concerning the COVID-19 pandemic. IBD organizations do provide expert-based guidance for physicians regarding COVID-19.10 We should grant patients access to these sources by providing a patient-focused version.
Medical systems worldwide have been transformed to treat patients with COVID-19. Regular scheduled outpatient consultations have been reduced considerably.18 Furthermore, patients with IBD do perceive hospitals and private practices as possibly hazardous environments. However, one-quarter of the patients with IBD sought advice from a physician about the coronavirus. To avoid in-person meetings, new models for consultations have received increasing interest.19,20 An et al. counselled 318 patients with IBD by using the WeChat messenger service as well as phone calls during the SARS-CoV-2 outbreak in December 2019 in Wuhan province, with good success.21 We found a demand for video consultation among a subset of patients with high fear of contracting SARS-CoV-2, who prefer to stay at home and who are younger [<40 years]. However, overall, patients did prefer consultations in person. Not all clinical situations are appropriate for video consultations. General information and advice may be discussed over video. Acute problems of patients with IBD and/or immunosuppression who require physical examination, ultrasound and laboratory testing are not sufficiently feasible with current video consultation techniques, thus resulting in reduced acceptance.22
Despite the large sample size of IBD patients, high response rate and comparison to a non-IBD cohort, there are some limitations to this study. Over 100 control participants were surveyed, but the ratio of IBD to non-IBD subjects was about 4:1. Although this ratio is also being used for similar numbers of subjects in clinical trials,23 it does limit comparison of the two groups.
The control group had a similar demographic distribution [age, sex, education], but two-thirds of the participants were living in the same household as IBD patients. This could bias the results to a more cautious behaviour or attitude because of their more vulnerable IBD household member. Nevertheless, attitude and behaviour towards COVID-19 differed significantly between the control group and IBD patients. Furthermore, similar significant differences were also seen in a survey comparing liver transplant recipients with their household members during the COVID-19 pandemic.24
In our survey, the prevalence of exposure to infected individuals in the IBD group was 1.7% and no SARS-CoV-2 infection was reported in this group. The true prevalence of SARS-CoV-2 may be underestimated, given the report-based data acquisition and the possible underdiagnosis of COVID-19 due to asymptomatic patients or atypical symptoms such as smell/taste disorders or muscle aches, which were not recommended for testing in the early phase of the COVID-19 pandemic.
Most participants were from the state of Thuringia and Saxony, where the cumulative SARS-CoV-2 incidence is as low as 90/100 000 and 106/100 000, respectively [as of April 23, 2020].25 This geographical range might be a limitation of our study. Although the actual number of infections is lower than that in some other countries, media coverage regarding the global extent of the COVID-19 pandemic is universal in German media, and we found a considerable fear of infection among the surveyed population.
In conclusion, we observed that the COVID-19 pandemic influences the daily lives of our patients with IBD differently from non-IBD participants. The fear of SARS-CoV-2 infection was higher in patients with IBD than in those without IBD, and the former stay at home more frequently than their peers. Patients taking immunosuppressants were more concerned about becoming infected and about interactions between medications and COVID-19. However, overall medication non-adherence was very low. Patients with IBD sought guidance primarily from television and internet news. Therefore, these patients should be actively approached to convey IBD-relevant information. Video consultations are a suitable offer for a subset of patients who are younger, have a high fear of contracting coronavirus and leave the house less frequently than their peers; however, overall acceptance of video consultations was limited.
Supplementary Material
Acknowledgments
We thank Cornelia Nageler for survey data input.
Funding
No funding was sourced for this project.
Conflict of Interest
Dr. Teich reports personal fees from Abbvie, MSD, Takeda, Pfizer, Amgen, Falk Foundation, Janssen, grants and personal fees from Ferring Arzneimittel GmbH, outside the submitted work. The remaining authors have no conflicts of interest to declare.
Author Contributions
P.C.G., N.T., J.S. and A.S. designed the research; P.C.G., P.A.R., N.T. and A.S. performed the research; P.C.G. and P.A.R. analysed the data; P.C.G. wrote the manuscript; P.A.R., J.S., N.T. and A.S. critically revised the manuscript for important intellectual content. All authors gave final approval of the version to be submitted.
References
- 1. WHO Director-General’s opening remarks at the media briefing on covid-19 - 11 March 2020 https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Accessed April 10, 2020; 2020.
- 2. Weible CM, Nohrstedt D, Cairney P, et al.. Covid-19 and the policy sciences: Initial reactions and perspectives. Policy Sci 2020:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020. [DOI] [PubMed] [Google Scholar]
- 4. Monteleone G, Ardizzone S. Are patients with inflammatory bowel disease at increased risk for covid-19 infection? J Crohns Colitis 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Singh S, Facciorusso A, Dulai PS, Jairath V, Sandborn WJ. Comparative risk of serious infections with biologic and/or immunosuppressive therapy in patients with inflammatory bowel diseases: A systematic review and meta-analysis. Clin Gastroenterol Hepatol 2020;18:69–81 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Collins M, Soularue E, Marthey L, Carbonnel F. Management of patients with immune checkpoint inhibitor-induced enterocolitis: a systematic review. Clin Gastroenterol Hepatol 2020;18:1393–1403.e1. [DOI] [PubMed] [Google Scholar]
- 7. Zhang XY, Zhang C, Sun QY, et al.. Infliximab protects against pulmonary emphysema in smoking rats. Chin Med J (Engl) 2011;124:2502–6. [PubMed] [Google Scholar]
- 8. Coronavirus disease (covid-19) advice for the public https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Accessed April 22, 2020; 2020.
- 9. Amanat F, Krammer F. SARS-CoV-2 vaccines: status report. Immunity 2020;52:583–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Laurent Beaugerie CMFdA, Torsten Kucharzik 5th interview COVID-19 ECCO Taskforce 2020. https://ecco-ibd.eu/images/6_Publication/6_8_Surveys/5th_Interview_COVID-19_ECCO_Taskforce_published.pdf. Accessed April 24, 2020.
- 11. D’Amico F, Rahier JF, Leone S, Peyrin-Biroulet L, Danese S. Views of patients with inflammatory bowel disease on the covid-19 pandemic: A global survey. Lancet Gastroenterol Hepatol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lopez A, Billioud V, Peyrin-Biroulet C, Peyrin-Biroulet L. Adherence to anti-TNF therapy in inflammatory bowel diseases: a systematic review. Inflamm Bowel Dis 2013;19:1528–33. [DOI] [PubMed] [Google Scholar]
- 13. Brenner EJ, Ungaro R, Colombel JF, Kappelman MD. Secure-IBD database public data update https://covidibd.org/current-data/. Accessed May 30, 2020.
- 14. Tursi A, Angarano G, Monno L, et al.. COVID-19 infection in Crohn’s disease under treatment with adalimumab. Gut 2020;69:1364–5. [DOI] [PubMed] [Google Scholar]
- 15. Malaviya R, Laskin JD, Laskin DL. Anti-TNFα therapy in inflammatory lung diseases. Pharmacol Ther 2017;180:90–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cima RR, Anderson KJ, Larson DW, et al.. Internet use by patients in an inflammatory bowel disease specialty clinic. Inflamm Bowel Dis 2007;13:1266–70. [DOI] [PubMed] [Google Scholar]
- 17. Kuehn BM. Patients go online seeking support, practical advice on health conditions. JAMA 2011;305:1644–5. [DOI] [PubMed] [Google Scholar]
- 18. CMS releases recommendations on adult elective surgeries, non-essential medical, surgical, and dental procedures during COVID-19 response https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental. Accessed April 23, 2020.
- 19. Greenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid-19. BMJ 2020;368:m998. [DOI] [PubMed] [Google Scholar]
- 20. Chatterjee SS, Barikar C M, Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J Psychiatr 2020;51:102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. An P, Ji M, Ren H, et al.. Prevention of COVID-19 in patients with inflammatory bowel disease in Wuhan, China. Lancet Gastroenterol Hepatol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Greenhalgh T, Vijayaraghavan S, Wherton J, et al.. Virtual online consultations: advantages and limitations (VOCAL) study. BMJ Open 2016;6:e009388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sandborn WJ, Su C, Sands BE, et al.; OCTAVE Induction 1, OCTAVE Induction 2, and OCTAVE Sustain Investigators Tofacitinib as induction and maintenance therapy for ulcerative colitis. N Engl J Med 2017;376:1723–36. [DOI] [PubMed] [Google Scholar]
- 24. Reuken PA, Rauchfuss F, Albers S, et al.. Between fear and courage: Attitudes, beliefs, and behavior of liver transplantation recipients and waiting list candidates during the covid-19 pandemic. Am J Transplant in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Daily situation report of the Robert Koch Institute https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-04-23-en.pdf?__blob=publicationFile. Accessed April 23, 2020; 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.