Abstract
Epidemiology of the US coronavirus disease 2019 (COVID-19) outbreak focuses on individuals’ biology and behaviors, despite centrality of occupational environments in the viral spread. This demonstrates collusion between epidemiology and racial capitalism because it obscures structural influences, absolving industries of responsibility for worker safety. In an empirical example, we analyzed economic implications of race-based metrics widely used in occupational epidemiology. In the United States, White adults have better average lung function and worse hearing than Black adults. Impaired lung function and impaired hearing are both criteria for workers’ compensation claims, which are ultimately paid by industry. Compensation for respiratory injury is determined using a race-specific algorithm. For hearing, there is no race adjustment. Selective use of race-specific algorithms for workers’ compensation reduces industries’ liability for worker health, illustrating racial capitalism operating within public health. Widespread and unexamined belief in inherent physiological inferiority of Black Americans perpetuates systems that limit industry payouts for workplace injuries. We see a parallel in the epidemiology of COVID-19 disparities. We tell stories of industries implicated in the outbreak and review how they exemplify racial capitalism. We call on public health professionals to critically evaluate who is served and neglected by data analysis and to center structural determinants of health in etiological evaluation.
Keywords: capitalism, COVID-19, health disparities, occupational health, racism, work
Abbreviations
- COVID-19
coronavirus disease 2019
- NHANES
National Health and Nutrition Examination Survey
- NIOSH
National Institute of Occupational Safety and Health
- PPE
personal protective equipment
- SARS-CoV-2
severe acute respiratory syndrome coronavirus-2
Editors note: The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the American Journal of Epidemiology.
From the criminal complaint against Derek Chauvin by the State of Minnesota, Hennepin County, May 29, 2020 (1):
Mr. Floyd is over six feet tall and weighs more than 200 pounds…. Floyd had underlying health conditions including coronary heart disease and hypertensive heart disease. The combined effects of Mr. Floyd being restrained by police, his underlying health conditions and any potential intoxicants in his system likely contributed to his death.
On Twitter, Benjamin Crump wrote, “Independent medical examiners determined #GeorgeFloyd’s death was due to asphyxia from sustained forceful pressure.” From his full statement (2):
[T]he manner of Mr. Floyd’s death was caused by asphyxia due to neck and back compression…. Sustained pressure on the right side of Mr. Floyd’s carotid artery impeded blood flow to the brain, and weight on his back impeded his ability to breathe…. “[H]e would be alive today if not from the pressure applied to his neck by fired officer Derek Chauvin and the strain on his body from two additional officers kneeling on him,” said lead attorney Crump.
The racialized use of individual-level risk factors is starkly evident in the aftermath of George Floyd’s recent murder. We see how scientific evidence is used to attribute risk to Floyd’s individual biology, in the form of the now familiar racial refrain of “underlying health conditions,” as well as risky behavior on the part of the deceased, whose physiological response to physical violence is presumed to have involved “potential intoxicants,” shifting the cause of death away from police violence. The same racialized narrative is prominent in the medical literature on coronavirus disease 2019 (COVID-19). The attribution of increased acquisition risk to individual-level etiologies—including higher rates of comorbidities and sociocultural differences such as health-seeking behavior and intergenerational cohabitation (3)—overshadows differential transmission related to structural factors (4), in particular, work environments. In this commentary, we tell stories about illness and work. We argue that the most salient commonality among workplace settings most responsible for the spread of COVID-19 are the racial and ethnic demographics of their work forces and clienteles. We further argue that the greatly amplified transmission risk occurring in these settings is not because of an inherent vulnerability of Black, Brown, or immigrant workers. Rather, a system of racial capitalism that preceded the pandemic structurally concentrates exposures and exacerbates COVID-19 risk for these worker populations, through replication of historical inequities and state-supported corporate neglect of worker protection (5, 6). Moreover, we argue that epidemiology as a discipline has selectively produced and promoted quantitative findings to justify and further this system of racial capitalism. The inequities evident in the ongoing COVID-19 pandemic offer an opportunity to redress our role in producing racially disparate health outcomes.
RACIAL CAPITALISM, THE INVERSE HAZARD LAW, AND THE COOPTING OF EPIDEMIOLOGY
Pirtle recently proposed in the journal Health Education & Behavior that “Racial capitalism is a fundamental cause of the racial and socioeconomic inequities (within COVID-19 in the United States)….” (6, p. 1) “Racial capitalism,” a term coined by Cedric Robinson (7), refers to the centrality of race in structuring social and labor hierarchies in capitalist economies. This system ensures “a vulnerable supply of low-wage workers” through “dual-wage systems, racially-exclusive labor unions, racialized divisions of labor, share-cropping, and related practices” (8, p. 528). Consistent with the theory of racial capitalism, Black and Latinx individuals are overrepresented in the low-paying jobs deemed “essential” in the President’s “Coronavirus Guidelines for America” issued during the first months of the US COVID-19 outbreak (9–11). Therefore, Black and Latinx people are disproportionately likely to work in jobs in which they are compelled to risk exposure to COVID-19. We and others argue that this elevated occupational risk is a major driver of the disproportionately high rates of COVID-19 infection, hospitalization, and mortality experienced by Black, Indigenous, and Latinx Americans (6, 12–14). For instance, the COVID-19 mortality rate among both Black and Latinx patients is over twice that of White patients in New York City (15). Many Indigenous populations share structural barriers to health experienced by Black and Latinx communities (e.g., job precarity) (12), but there is limited available data on COVID-19 within Indigenous Nations. While the infection rate in the Diné (Navajo People’s) Nation is nearly the highest per capita, US federal support has been minimal for Indigenous Nations, and COVID-19 outcomes specific to Indigenous Nations are largely excluded from US reports (12).
However, there are high-exposure jobs in which workers do not experience elevated risk of COVID-19 or severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection. For instance, medical doctors have infection rates similar to the general public despite high levels of exposure to the SARS-CoV-2 virus in their workplaces (16). This paradoxical finding is consistent with Krieger et al.’s (17) Inverse Hazard Law. The Inverse Hazard Law states that hazards accumulate inversely with power and resources in US workplaces. In the case of COVID-19, adequate personal protective equipment (PPE) greatly reduces risk of being infected with SARS-CoV-2 (18). As described later in this commentary, workers in high-status, high-wage jobs with predominantly White workforces, such as physicians, experience lower risk of SARS-CoV-2 infection (19) than other workers in similarly high-exposure work settings. Jobs that are structured around the supply of low-wage workers of color who do not have the power and resources to demand workplace protections or leave the high-hazard jobs are the ones among whom COVID-19 risk is especially high because adequate PPE is not provided in high-exposure jobs.
How does epidemiology support the interests of racial capitalism? In her scholarship on the history of race and medicine, Dorothy Roberts describes how focusing on “underlying” health conditions and behavioral risk factors allows society “both to ignore how disease is caused by political inequality and to justify an unequal system by pointing to the inherent racial difference that disease supposedly reveals” (20, p. 85). Under racial capitalism, attention is drawn away from workplace hazards by arguing that workers are inherently at high risk of ill health due to their own racial and behavioral susceptibilities, masking and justifying how labor is structured to concentrate risky, low-wage work among non-White or otherwise marginalized workforces. Contemporary, “mainstream” epidemiology’s technocratic focus on individual-level biological and behavioral risk factors (21–23) readily supplies data used to justify high levels of ill health observed among of low-wage workers. In particular, “mainstream” epidemiology colludes with racial capitalism by producing disproportionately more work documenting individual-level susceptibility than it does investigating more plausible alternative workplace-level explanations for workforce disparities (22). Moreover, as we demonstrate in the empirical case study below, much of “mainstream” work in epidemiology is structurally racist in that it serves to reinforce and, post hoc, justify pervasive narratives of biological and cultural inferiority of Black and Brown people (24).
CASE STUDY: RACIALIZED METRICS IN WORKERS’ COMPENSATION CLAIMS
The collusion of epidemiology with racial capitalism is particularly insidious because racial capitalism can leverage statistical methodology that is perceived as objective to hide even obviously racist distributions of health (25, 26). Below we present an example from occupational health that demonstrates how epidemiologic data is strategically used to downplay the effects of occupational exposures on poor health and thus minimize financial exposure of the corresponding industries.
Lung function and hearing loss are metrics commonly monitored in manufacturing industries due to Occupational Safety and Health Administration regulations (27, 28). These metrics are proxies of health impacts of hazardous work environments in manufacturing settings (29). Moreover, lung impairment and hearing loss are frequent grounds for workers’ compensation claims (30). Workers’ compensation is a legal process in which workers file claims in relation to illness and injury resulting from job tasks and exposures. Compensation is paid by industry when the court rules in favor of the worker (30). Therefore, strategies that minimize identification of worker injuries directly benefit the owners of and investors in the businesses employing those workers.
The epidemiologic literature on lung function and hearing
In the United States, on average, Black adults tend to have worse lung function but better hearing than White adults (31, 32). Seminal epidemiologic analyses of the National Health and Nutrition Examination Survey (NHANES) III (1988–1994) concluded that lung function among “African-Americans” is 12%–15% lower than among “Caucasians” (31). The epidemiologic data indicate the opposite for hearing. Numerous US cohort studies have concluded that Black adults tend to have better hearing than White adults (and women tend to have better hearing than men) (32–35). Epidemiologic studies suggest that the minimum noise levels must be 25%–45% louder to be detected by White Americans compared with Black Americans (34, 36).
Workers’ compensation for lung and hearing impairment
Workers qualify for compensation only when they reach a set level of impairment. For lung function, workers are typically eligible for compensation when their lung capacity performance is lower than 90% of their predicted lung capacity. The predicted values are based on age, sex, height, and race (37, 38) and come from equations by Hankinson et al. (31) based on their epidemiologic studies of NHANES III data. The equations set expected lung capacity for Black adults 15% lower than that for White adults. In other words, Black workers must experience 15% worse lung function than White workers to qualify for workers’ compensation.
In contrast to lung function, no race-based decrement is applied to hearing loss disability thresholds. If workers can show that their impaired hearing is not attributable to any degenerative or genetic disorder, they are eligible for compensation of 70 weeks’ pay for 1 impaired ear and 150 weeks’ pay for 2 ears being impaired (37). In spite of the epidemiologic evidence demonstrating better hearing for Black adults versus White adults and for women than men, workers are evaluated using only their observed hearing test results (32–35). Hearing loss disability qualifications are made based on the average of decibel thresholds a worker demonstrates, regardless of a worker’s race or sex.
Empirical simulation: workers’ compensation awards with and without race “corrections”
We examined the effects of this selective application of epidemiologic data on workers’ compensation claim payouts. For lung function, we used a demonstration database of deidentified Black and White workers provided with the National Institute of Occupational Safety and Health (NIOSH)’s Spirometry Longitudinal Data Analysis Software (39). The workers are representative of workers from occupational settings with high exposure to particulate matter (39). For hearing, we used data from the 2005–2006 NHANES, which is representative of the US Black and White adult populations during a similar time period to the NIOSH data. We restricted the sample to respondents aged 20–65 years who reported “ever having job exposure to loud noise” (40). We estimated the percentage of workers who met the respective thresholds for a disability claim under 2 conditions: the current standard and a counterfactual scenario in which race adjustments were (hearing) or were not (lung function) used. For the counterfactual hearing-loss condition, we applied a conservative 25% decrement to White workers, based on age-adjusted population estimates (34, 36). For the counterfactual lung function condition, we eliminated the race correction from the predicted lung function equation.
Figure 1 shows Black workers’ and White workers’ distributions of lung capacity and hearing as they would be measured to evaluate compensation. The solid curves are the conditions currently in practice: race-specific equations for lung function and the race-neutral absolute threshold for hearing. The dashed lines are the counterfactual conditions: elimination of race “correction” for lung function and addition of White decrement “correction” for hearing. The vertical lines show the thresholds for initial compensation. Those workers to the left of the line would be eligible for compensation.
Figure 1.
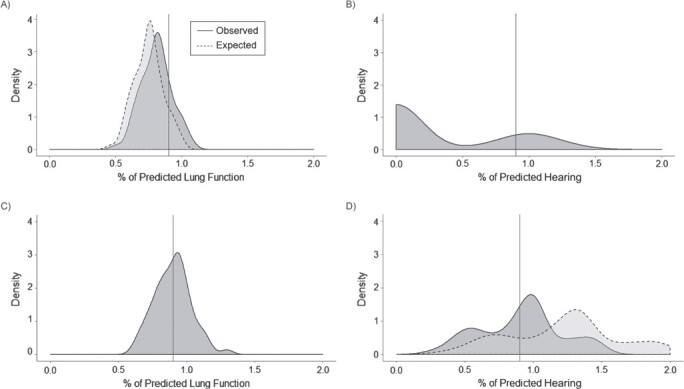
Distributions of percent of predicted lung function (National Institute of Occupational Safety and Health Spirometry Longitudinal Data, 1999) and hearing (National Health and Nutrition Examination Survey, 2005–2006) under race-based correction conditions among Black and White workers, United States. A) Distributions of lung capacity among Black workers; B) distributions of hearing among Black workers. C) Distributions of lung capacity among White workers. D) Distributions of hearing among White workers. These distributions represent how they would be measured to evaluate compensation. The solid curves are the conditions currently in practice: race-specific equations for lung function and the race-neutral absolute threshold for hearing. The dashed lines are the counterfactual conditions: elimination of race “correction” for lung function and addition of White decrement “correction” for hearing. The vertical lines show the thresholds for initial compensation. Those workers to the left of the line would be eligible for compensation.
Using the current algorithms for predicted lung function, 60% of White workers and 81% of Black workers qualify for compensation. When applying an algorithm to Black workers that is not race corrected, 94% of the Black workers would qualify for compensation. Using the current, not race-corrected, algorithm for predicted hearing, 43% of white workers and 70% of Black workers would qualify for compensation. When imposing a race-specific adjustment for White workers, only 38% of White workers would qualify.
Discussion of empirical case study
In all 4 scenarios in Figure 1, Black workers exhibit greater impairment than White workers. Even in the case of hearing, where Black Americans generally have less impairment than their White counterparts (32), Black workers fare worse in the end. The hearing finding is evidence in favor of the theory of racial capitalism and the Inverse Hazard Law: Greater exposure to noise hazards or lack of workplace protections could explain why Black workers experience much greater hearing loss despite better hearing in the general population.
Our analysis of workers’ compensation claims makes explicit one mechanism by which racial capitalism enriches industries. In the counterfactual scenario of no Black lung-function correction but a White hearing correction, industry would owe 31% more in workers’ compensation payouts (this calculation is based on applying the average payout associated with each workers’ compensation award in a typical state (30)). Of course, applying a Black race correction to lung function and a White race correction to hearing would theoretically reduce industry payouts even more. So why are race corrections for lung function uncontested, standard practice in occupational regulations and occupational epidemiology research (37, 41) while race corrections for hearing are not? First, as shown by the 31% statistic above, the Black race correction is more profitable to industry than a White race correction. Under racial capitalism, Black workers experience more work-related health damage because they are concentrated in riskier, less protected jobs. Therefore, “corrections” that understate the extent of their damaged health will be disproportionately more valuable to industry than corrections that understate workplace impacts on less-exposed populations. Second, consistent applications of race corrections would undermine the narrative of inherent Black biological inferiority that helps make racial capitalism so profitable. Exposing the fact that Black workers in high-noise jobs experience more hearing impairment even though a race correction is applied to account for the typically worse hearing of White adults makes more obvious the likelihood that the greater hearing damage observed among Black workers is actually because of the workplace setting. That logical connection in turn suggests that other health harms disproportionately experienced by Black workers are also because of the organization of work.
We end this section with a note about epidemiology’s complicity with racial capitalism in regard to damage to hearing and lung function. As we’ve described above, the field of epidemiology has published and promoted the use of race-“corrected” equations for lung function (where Black adults tend to perform worse) but not for hearing (where Black adults tend to perform better). Moreover, smoking status, a strong predictor of lung capacity, is not included in the lung function reference equations: Hankinson et al. (31) restricted their NHANES III analysis to “lifelong nonsmoking subjects.” Because Whites in the United States are more likely to smoke and with more intensity (42), exclusion of smoking from the equations likely overstates the “predicted” lung function of White workers, making them even more disproportionately likely and other workers relatively less likely to qualify for workers’ compensation based on impaired lung function. Whatever the intentions of these analytical and dissemination decisions, the overall impact of this body of epidemiologic research is to reinforce a narrative of Black workers’ biological inferiority, increasing the financial gains that industries can reap by using racial capitalism as an organizational strategy.
RACIAL CAPITALISM IS DRIVING WORKPLACE TRANSMISSION OF SARS-COV-2
Next we briefly discuss key industries implicated in the spread of the SARS-CoV-2 virus in the United States. We group the work settings by the demographic compositions of the workers or the clientele served. Applying theories of racial capitalism and Inverse Hazard Law, we argue that the risks associated with these workplaces are highly patterned by race/ethnicity and immigrant status.
Meat packing and agricultural workers
From farmworkers to meat packers to supermarket-chain employees and food-delivery workers, the extreme vulnerability of labor forces across the food-production system demonstrates that while industrial agriculture work is considered essential, the workers themselves are treated as expendable (14). Moreover, the concentration of US industrial agriculture in the South and the lack of workplace protections for the predominantly Black and Latinx workforces reflect the ongoing legacies of plantation slavery (5). In meat packing, where congregate work is standard and several major outbreaks are occurring (43), the worker population is 35% Latinx despite Latinx workers making up only 18% of the national workforce (10). Further, 34% of this industry’s workers are non-White versus 22% of the national workforce. Industry generates perverse incentive structures with regard to testing within facilities by denying sufficient sick leave support (5). While the Centers for Disease Control and Prevention recommends employer-initiated interventions to prevent transmission (43), company leadership engages in territorial stigmatization (44) by blaming high rates of SARS-CoV-2 infection on community transmission and worker behaviors (45). Not only does this narrative minimize public awareness of the extent of disease spread, but it also erases worker visibility and facilitates management misconduct in mitigating outbreaks.
Construction workers
The construction industry employs nearly 7 million workers, with an estimated 14% of construction workers being undocumented, although this is likely an underestimate. Austin, Texas, is home to an estimated 50,000 construction workers, about 50% of whom are undocumented and more than 50% of whom make below poverty-level wages (46–48). Despite early orders by local government declaring construction workers “nonessential” and subject to stay-at-home orders (49), and despite an epidemiologic study identifying significant risk of hospitalization for COVID-19 if construction workers were to resume work (50), under the influence of building and real-estate industries the state governor quickly intervened with a statewide order deeming all construction work as “essential” (51). By early April it was clear that construction workers, Latinx workers in particular, were falling sick and being hospitalized for COVID-19 at disproportionately higher rates than the general public (51–53). The majority of cluster cases in Austin were linked to construction work sites, and surveillance testing for coronavirus among construction workers yielded a positive rate of approximately 3.5 times the average rate at drive-through surveillance sites (54). The flawed dominant narrative blames workers in this industry by attributing high disease transmission to multigenerational households, inadequate personal hygiene, and poor health literacy (55). However, despite citywide requirements for construction employers to support strict physical-distancing guidelines and personal hygiene recommendations, no oversight mechanism exists and workers report ongoing lack of access to personal protective equipment (56).
Health-care workers
The health-care workforce providing for patients with COVID-19, in general, experiences the highest risk of contracting the virus (57). Disaggregation of this sector reveals disparities in disease risk that mirror the race and gender disparities that epidemiologists and sociologists have documented for decades (58). While even high-status physicians, who are most likely to be White men, face potential job loss if they speak out about lack of PPE (59), workers in lower-prestige and lower-paid jobs within the health-care system are experiencing the greatest burden of COVID-19 (60, 61). These jobs include custodial staff, nurses, and domestic care providers—positions disproportionately filled by women of color (10). Several structural factors increase these workers’ vulnerability to the disease, including the need to work multiple jobs because of low wages (potentially at different facilities with high exposure potential), consistent job precarity, and limited ability to provide their own PPE (5, 6) in the context of inadequate employer and governmental protections despite their extreme vulnerability.
Nursing homes and assisted-living facilities
On June 4, 2020, after persistent pressure from activists, families, public health professionals, and journalists, the Centers for Medicare and Medicaid Services posted the first set of COVID-19 nursing home data. These data showed that, as of May 31, 2020, there were 95,000 confirmed cases and close to 32,000 deaths in the 88% of Medicare and Medicaid nursing homes reporting—accounting for about 5% of confirmed cases and a third of the deaths in the United States (62). Mergers, acquisitions, and takeovers have consolidated about 67% of US nursing-home beds within for-profit facilities that are increasingly owned by large corporate providers (63). The staffing ratio of high-skilled and higher-paid professionals (e.g., registered nurses and licensed practical nurses) to less-skilled and lower-paid professionals (e.g., certified nursing assistants) has decreased drastically (64, 65). In fact, certified nursing assistants now provide close to 80% of caregiving duties in nursing homes, resulting in a cost-savings for owners who reduce the registered-nurse and licensed-practical-nurse staff (65).
The demographic characteristics and precarity of nursing assistants reflects historical continuities in the racialized and gendered labor of caregiving (66). Certified nursing assistants are disproportionately women of color, and disproportionately Black; 20% are born outside of the United States, and just under half have no formal educational training beyond high school (67). They serve predominantly US-born White residents at low wages (median hourly wage, $11.87) (67). They are injured on the job 3.5 times more often that an average worker in the United States (67). Due to precarious and/or part-time contracts, approximately 20% are uninsured, even while potentially working at multiple nursing homes to make ends meet. Within the context of the COVID-19 pandemic, nursing home staff have not been provided appropriate levels of PPE, information about COVID-19 cases within facilities, access to testing, or data about risk overall (68–70). Nursing-home employees have reported retaliation and job loss because of complaints of lack of PPE and inappropriate work conditions throughout the COVID-19 pandemic (69).
Moreover, the nursing homes primarily supported by Medicare and Medicaid are less resourced with sufficient PPE, cleaning materials, and appropriate staffing levels, leading to gaps in care and hygiene, as well as minimal client interaction with skilled staff (71). Even after controlling for funding sources, location, size, and a range of other factors, nursing homes are racially/ethnically segregated, with those facilities occupied mostly by marginalized populations having the worst conditions; nursing homes with primarily Black and Latinx residents have consistently poorer quality, more violations, and disproportionate burden of infectious disease (70).
Carceral facilities: jails, prisons, and detention centers
Carceral facilities differ from the other workplaces described above in that a predominantly White workforce oversees a disproportionately Black and Latinx population (72). We include these facilities here because jails, prisons, and Immigration and Customs Enforcement detention centers are major sites of SARS-CoV-2 transmission (73–75). Further, narratives employed by facility management to refuse COVID-19-related worker requests mirror strategies employed under racial capitalism in the work settings described above. Management’s narratives emphasize the innate susceptibility of Black and Latinx prisoners to COVID-19 morbidity and negative racialized behaviors. For instance, 2 press releases from the US Department of Justice Federal Bureau of Prisons reported deaths of inmates Patrick Jones and Nicholas Rodriguez on March 28, 2020, and April 1, 2020, respectively. One sentence was nearly identical: “… Mr. [Jones|Rodriguez], who had long-term, pre-existing medical conditions which the [Centers for Disease Control and Prevention] lists as risk factors for developing more severe COVID-19 disease, was pronounced dead by hospital staff.” The next sentences list the age, sex, and charges (both drug-related) of which the men had been convicted (76, p.1).
People who are incarcerated in US facilities are at high risk of being infected with SARS-CoV-2, not because of preexisting medical conditions or crimes they may have committed. The incarcerated face a high risk of being infected because of crowded, enclosed spaces; limited access to protective equipment, including masks; limited access to SARS-CoV-2 testing and humane isolation spaces; and limited access to basic hygiene supplies, such as soap and hot water (75). However, the staff of carceral facilities have also complained about elevated infection risks (74, 75). In federal facilities, workers have asked for more tests, more PPE, hazard pay, and extended leave when exposed to infection or because of their own health conditions or conditions of family members. Each of these requests comes with financial costs, and they have often been met with resistance by the Bureau of Prisons and other managers of carceral facilities (73, 74). COVID-19 deaths of inmates reflect the extent and seriousness of SARS-CoV-2 transmission in carceral facilities. Statements that focus on the susceptibility of Black inmates such as Jones to COVID-19 death distract from the facility conditions that escalate SARS-CoV-2 transmission—facility conditions that workers partially share. True worker protection would require a rethinking and restructuring of carceral facilities and systems entirely.
HOW SHOULD PUBLIC HEALTH ADDRESS RACIAL CAPITALISM?
In this commentary, we argue that the role of workplaces in SARS-CoV-2 transmission illustrates how racial capitalism operates. We observe a concentration of SARS-CoV-2 exposure among low-wage and essential-worker populations who are disproportionately racial and ethnic minorities and immigrants. In nursing homes, the sector associated with a third of US COVID-19 mortality (62), workers are predominantly women of color and low-wage employees, who lack appropriate PPE. Our analysis also reflects Krieger et al.’s Inverse Hazard Law (17). Even within high-exposure workforces, we observe stratification with regard to providing PPE. An increasing number of deaths among nurses (77) and nonclinical hospital staff (78) are attributable to inadequate provision of PPE, notably more common than among their physician counterparts, who have greater protections. Finally, across all occupational settings, narratives of innate susceptibility (20), territorial stigmatization (44), and individual behavioral explanations (6) abdicate corporate responsibility and associated government policies to provide safe environments, adequate PPE, paid sick leave, and SARS-CoV-2 testing. These narratives instead impose blame on workers for the hazards they experience at work.
We recognize that the disparities in incidence and mortality related to COVID-19 stem from centuries of US industrial development that depends on structural racism to thrive (7). Our analyses have salience beyond the scope of this outbreak. As with all diseases for which workplace environment is a root cause, the most marginalized workers with the least power and resources (e.g., people who are undocumented residents, incarcerated, people of color, women, or lesbian, gay, bisexual, transgender, or queer) are least likely to have access to testing for infectious diseases and most likely to be missed in cohort enumeration (17). During the COVID-19 outbreak, public health institutions are not collecting and/or suppressing complete testing, workplace, and demographic information (12, 79). Despite—or perhaps because of—underlying risks, decision-makers have been reluctant to release data regarding COVID-19 cases, deaths, and hospitalizations associated with nursing homes, with some going as far as insinuating it was “bad for business” (80, 81). At minimum, all COVID-19 researchers in the United States should routinely collect data on occupation and stratify data summaries by race, ethnicity, and gender whenever possible. At the least, we must strive toward a field of inquiry in which political influence does not compromise public health practice. We urge COVID-19 researchers and public health professionals more broadly to engage with occupational hazards as root causes of diseases and disparities.
One of epidemiology’s founding legends is John Snow’s removal of the Broad Street pump (82). Would we be talking reverentially about John Snow if he’d done a study of individual-level risk factors for cholera death among those admitted to the regional hospital? Ford and Airhihenbuwa’s (83) Public Health Critical Race praxis calls on public health professionals to question the ways in which we recreate racism through our study designs, information collection, research questions, and data-analysis methods. By ignoring and misrepresenting root causes of poor health among workers, we absolve industries and government leaders of their responsibility for equitable health protection. In the midst of the COVID-19 crisis, we have an opportunity to critically evaluate our methods and take measurable steps toward promoting social justice and health equity.
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (Elizabeth S. McClure, Whitney R. Robinson); Carolina Population Center, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (Elizabeth S. McClure, Whitney R. Robinson); Department of African and African Diaspora Studies, University of Texas at Austin, Austin, Texas (Pavithra Vasudevan); Center for Women’s and Gender Studies, University of Texas at Austin, Austin, Texas (Pavithra Vasudevan); Jay Weiss Institute for Health Equity, Sylvester Comprehensive Cancer Center, Miller School of Medicine, University of Miami, Miami, Florida (Zinzi Bailey); and Department of Internal Medicine, Dell Medical School, University of Texas at Austin, Austin, Texas (Snehal Patel).
This work was funded by the National Institutes of Health (grants T32 ES007018 and T32 HD007168).
We acknowledge the Concerned Citizens of West Badin for inspiring this initial inquiry, as well as #BlackEpiMatters (https://twitter.com/hashtag/blackepimatters), the attendees of the Spirit of 1848 caucus sessions of the 2019 American Public Health Association Meeting, and the Carolina Population Center Interdisciplinary Seminar for their thoughtful feedback in the early stages of this study.
Conflicts of interest: none declared.
REFERENCES
- 1. State of Minnesota Judicial Branch . 27-CR-20-12646: State vs. Derek Chauvin. St Paul, MN: State of Minnesota Judicial Branch; 2020. http://www.mncourts.gov/media/StateofMinnesotavDerekChauvin. Accessed August 12, 2020. [Google Scholar]
- 2. Crump B. Independent medical examiners determined #GeorgeFloyd’s death was due to asphyxia from sustained forceful pressure. Full statement: https://t.co/cIbWu8ssWX. https://twitter.com/attorneycrump/status/1267540974244442112. Posted June 1, 2020. Accessed June 2, 2020.
- 3. Pareek M, Bangash MN, Pareek N, et al. Ethnicity and COVID-19: an urgent public health research priority. Lancet. 2020;395(10234):1421–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bailey ZD, Moon JR. Racism and the political economy of COVID-19: will we continue to resurrect the past? [published online ahead of print May 28, 2005. J Health Polit Policy Law. (doi: 10.1215/03616878-8641481). [DOI] [PubMed] [Google Scholar]
- 5. Freshour C, Williams B. Abolition in the time of covid-19. Antipode. https://antipodeonline.org/2020/04/09/abolition-in-the-time-of-covid-19/. Accessed May 18, 2020. [Google Scholar]
- 6. Laster Pirtle WN. Racial capitalism: a fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Health Educ Behav. 2020;47(4):504–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robinson CJ. Black Marxism: the Making of the Black Radical Tradition. Chapel Hill, NC: University of North Carolina Press; 2000. [Google Scholar]
- 8. Pulido L. Geographies of race and ethnicity II: environmental racism, racial capitalism and state-sanctioned violence. Prog Hum Geogr. 2017;41(4):524–533. [Google Scholar]
- 9. Poteat T, Millett G, Nelson LE, et al. Understanding COVID-19 risks and vulnerabilities among Black communities in America: the lethal force of syndemics. Ann Epidemiol. 2020;47:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. U.S. Bureau of Labor Statistics . Employed persons by detailed industry, sex, race, and Hispanic or Latino ethnicity. https://www.bls.gov/cps/cpsaat18.htm. Accessed May 20, 2020.
- 11. Office of the White House . Coronavirus guidelines for America. https://www.whitehouse.gov/briefings-statements/coronavirus-guidelines-america/. Accessed June 2, 2020.
- 12. Godin M. Indigenous groups are taking on governments over coronavirus failures. https://time.com/5808257/indigenous-communities-coronavirus-impact/. Accessed June 2, 2020.
- 13. Gennetian LA, Johnson MS. Work-based risks to Latino workers and their families from COVID-19. https://econofact.org/work-based-risks-to-latino-workers-and-their-families-from-covid-19. Accessed June 13, 2020.
- 14. Alkon AH, Bowen S, Kato Y, et al. Unequally vulnerable: a food justice approach to racial disparities in COVID-19 cases. Agric Hum Values. 2020;37:535–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention . COVID-19 in racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html. Accessed June 2, 2020.
- 16. Kaplan R. Physicians’ risk from COVID-19: a reassuring statistic. https://www.medpagetoday.com/infectiousdisease/covid19/85902. Accessed June 2, 2020.
- 17. Krieger N, Chen JT, Waterman PD, et al. The inverse hazard law: blood pressure, sexual harassment, racial discrimination, workplace abuse and occupational exposures in US low-income black, white and Latino workers. Soc Sci Med. 2008;67(12):1970–1981. [DOI] [PubMed] [Google Scholar]
- 18. World Health Organization . Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim guidance. https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf. Accessed June 13, 2020.
- 19. Association of American Medical Colleges . Percentage of all active physicians by race/ethnicity, 2018. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018. Accessed June 13, 2020.
- 20. Roberts DE. Fatal Invention: How Science, Politics, and Big Business Re-create Race in the Twenty-first Century. New York, NY: New Press; 2011. [Google Scholar]
- 21. Wing S. Limits of epidemiology. Med Global Survival. 1994;1(2):74–86. [Google Scholar]
- 22. Krieger N. Epidemiology and the People’s Health. New York, NY: Oxford University Press; 2011. [Google Scholar]
- 23. Hoffman KM, Trawalter S, Axt JR, et al. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci. 2016;113(16):4296–4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bailey ZD, Krieger N, Agénor M, et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. [DOI] [PubMed] [Google Scholar]
- 25. Zuberi T, Bonilla-Silva E. White Logic, White Methods: Racism and Methodology. Lanham, Maryland: Rowman & Littlefield Publishers, Inc; 2008. [Google Scholar]
- 26. Kendi IX. How to Be an Antiracist. New York, NY: Random House Publishing Group; 2019. [Google Scholar]
- 27. Occupational Safety and Health Administration . Safety and health topics | occupational noise exposure. https://www.osha.gov/SLTC/noisehearingconservation/. Accessed January 7, 2020.
- 28. Occupational Safety and Health Administration . Pulmonary function testing training requirements and spirometer transmission of disease. https://www.osha.gov/laws-regs/standardinterpretations/1993-06-17-0. Accessed January 7, 2020.
- 29. Kongerud J, Grønnesby JK, Magnus P. Respiratory symptoms and lung function of aluminum potroom workers. Scand J Work Environ Health. 1990;16(4):270–277. [DOI] [PubMed] [Google Scholar]
- 30. Sengupta I, Reno VP, Burton J, et al. Workers’ compensation: benefits, coverage, and costs, 2010. https://papers.ssrn.com/abstract=2131336. Accessed January 7, 2020.
- 31. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159(1):179–187. [DOI] [PubMed] [Google Scholar]
- 32. Helzner EP, Cauley JA, Pratt SR, et al. Race and sex differences in age-related hearing loss: the health, aging and body composition study. J Am Geriatr Soc. 2005;53(12):2119–2127. [DOI] [PubMed] [Google Scholar]
- 33. Lin FR, Maas P, Chien W, et al. Association of skin color, race/ethnicity, and hearing loss among adults in the USA. J Assoc Res Otolaryngol. 2012;13(1):109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Agrawal Y, Platz EA, Niparko JK. Prevalence of hearing loss and differences by demographic characteristics among US adults: data from the National Health and Nutrition Examination Survey, 1999–2004. Arch Intern Med. 2008;168(14):1522–1530. [DOI] [PubMed] [Google Scholar]
- 35. Jerger J, Jerger S, Pepe P, et al. Race difference in susceptibility to noise-induced hearing loss. Am J Otol. 1986;7(6):425–429. [PubMed] [Google Scholar]
- 36. Agrawal Y, Niparko JK, Dobie RA. Estimating the effect of occupational noise exposure on hearing thresholds: the importance of adjusting for confounding variables. Ear Hear. 2010;31(2):234–237. [DOI] [PubMed] [Google Scholar]
- 37. Rondinelli R. AMA Guides to the Evaluation of Permanent Impairment. 6th ed. Chicago, IL: American Medical Association; 2007. [Google Scholar]
- 38. US Department of Labor . Division of Federal Employees' Compensation (DFEC): A.M.A. Guides to the Evaluation of Permanent Impairment, 6th Edition. https://www.dol.gov/owcp/dfec/AMAGuideEvalPermImpair6thEd.htm. Accessed January 9, 2020.
- 39. Centers for Disease Control and Prevention . SPIROLA software—NIOSH workplace safety and health topic. https://www.cdc.gov/niosh/topics/spirometry/spirola-software.html. Accessed February 14, 2020.
- 40. National Center for Health Statistics . National Health and Nutrition Examination Survey Data: audiometry data. https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/AUX1.htm#AUXU500L. Accessed February 19, 2020.
- 41. American Thoracic Society . Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991;144(5):1202–1218. [DOI] [PubMed] [Google Scholar]
- 42. Holford TR, Levy DT, Meza R. Comparison of smoking history patterns among African American and White cohorts in the United States born 1890 to 1990. Nicotine Tob Res. 2016;18(suppl_1):S16–S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dyal JW. COVID-19 among workers in meat and poultry processing facilities — 19 states, April 2020. MMWR Morb Mortal Wkly Rep. 2020;6946(18):557–561. [DOI] [PubMed] [Google Scholar]
- 44. Wacquant L, Slater T, Pereira VB. Territorial stigmatization in action. Environ Plan A. 2014;46(6):1270–1280. [Google Scholar]
- 45. Samaha A, Baker K. Smithfield Foods is blaming “living circumstances in certain cultures” for one of America’s largest COVID-19 clusters. Buzzfeed. https://www.buzzfeednews.com/article/albertsamaha/smithfield-foods-coronavirus-outbreak. Accessed May 20, 2020. [Google Scholar]
- 46. Torres R, Heyman R, Munoz S, et al. Building Austin, building justice: immigrant construction workers, precarious labor regimes and social citizenship. Geoforum. 2013;45:145–155. [Google Scholar]
- 47. Workers Defense Project . Building a better Texas: construction working conditions in the Lone Star State. https://www.workersdefense.org/construction-working-conditions-in-the-lone-star-state/. Accessed June 2, 2020.
- 48. Workers Defense Project . Build a better nation: a case for comprehensive immigration reform. https://www.workersdefense.org/immigration-report/. Accessed June 2, 2020.
- 49. State of Texas . Stay home—work safe order information. https://austintexas.gov/department/covid-19-information/stay-home-order. Accessed June 2, 2020.
- 50. Pasco R, Du Z, Wang X, et al. COVID-19 in Austin, Texas: epidemiological assessment of construction work. https://cid.utexas.edu/sites/default/files/cid/files/covid-19_austin_construction_workforce-meyers_ut-040520.pdf. Accessed June 2, 2020.
- 51. City of Austin, Texas . Work session of the Austin City Council, item B001—briefing on matters related to COVID-19. https://www.austintexas.gov/department/city-council/2020/20200519-wrk.htm. Accessed June 2, 2020.
- 52. Wilson M, Hawkins L. Coronavirus in Austin: virus clusters showing up in construction, other industries. Austin American-Statesman. https://www.statesman.com/news/20200519/coronavirus-in-austin-virus-clusters-showing-up-in-construction-other-industries. Accessed June 2, 2020. [Google Scholar]
- 53. Adeni H, Streicher B. Austin health officials seeing spike in COVID-19 cases among construction workers. KVUE. https://www.kvue.com/article/news/health/coronavirus/austin-covid-19-coronavirus-cases-construction-hotspots/269-844d3a4e-a2f1-49fc-b9f8-6bfda4921798. Accessed June 2, 2020. [Google Scholar]
- 54. Escott M. May 14: COVID-19: contact tracing & cluster investigation. https://dellmed.utexas.edu/virtual-town-hall-for-the-medical-community. Accessed June 2, 2020.
- 55. Olivo A, Lang MJ, Harden JD. Crowded housing and essential jobs: why so many Latinos are getting coronavirus. Washington Post. https://www.washingtonpost.com/local/latinos-coronavirus/2020/05/25/6b5c882a-946e-11ea-82b4-c8db161ff6e5_story.html. Accessed June 2, 2020. [Google Scholar]
- 56. McGlinchy A. Construction in Texas is “essential” during the pandemic. Workers worry their health is not. KUT. https://www.kut.org/post/construction-texas-essential-during-pandemic-workers-worry-their-health-not. Accessed June 2, 2020. [Google Scholar]
- 57. Douglas M, Katikireddi SV, Taulbut M, et al. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Aguirre BE, Wolinsky FD, Niederauer J, et al. Occupational prestige in the health care delivery system. J Health Soc Behav. 1989;30(3):315–329. [PubMed] [Google Scholar]
- 59. Carville O, Court E, Brown KV, et al. Hospitals tell doctors they’ll be fired if they speak out about lack of gear. Fortune. https://fortune.com/2020/03/31/coronavirus-shortages-hospitals-doctors-fired-face-masks-ppe/. Accessed June 5, 2020. [Google Scholar]
- 60. Lu M. These are the occupations with the highest COVID-19 risk. https://www.weforum.org/agenda/2020/04/occupations-highest-covid19-risk/. Accessed June 5, 2020.
- 61. Pasquini M. Three New York City hospital workers died from coronavirus weeks after handing out masks. People Magazine. https://people.com/health/nyc-hospitals-workers-died-coronavirus-after-handing-out-masks/. Accessed June 5, 2020. [Google Scholar]
- 62. Centers for Medicare & Medicaid Services . COVID-19 nursing home data. https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/. Accessed June 5, 2020. [PubMed]
- 63. Ronald LA, McGregor MJ, Harrington C, et al. Observational evidence of for-profit delivery and inferior nursing home care: when is there enough evidence for policy change? PLoS Med. 2016;13(4):e1001995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hurtado DA, Sabbath EL, Ertel KA, et al. Racial disparities in job strain among American and immigrant long-term care workers. Int Nurs Rev. 2012;59(2):237–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Seblega BK, Zhang NJ, Unruh LY, et al. Changes in nursing home staffing levels, 1997 to 2007. Med Care Res Rev. 2010;67(2):232–246. [DOI] [PubMed] [Google Scholar]
- 66. Glenn EN. From servitude to service work: historical continuities in the racial division of paid reproductive labor. Signs. 1992;18(1):1–43. [Google Scholar]
- 67. PHI . U.S. nursing assistants employed in nursing homes: key facts (2019). https://phinational.org/resource/u-s-nursing-assistants-employed-in-nursing-homes-key-facts-2019/. Accessed June 5, 2020.
- 68. Tahir D, Cancryn A. Bad state data hides coronavirus threat as Trump pushes reopening. Politico. https://www.politico.com/news/2020/05/27/bad-state-coronavirus-data-trump-reopening-286143. Accessed June 5, 2020. [Google Scholar]
- 69. Khimm S. The forgotten front line: Nursing home workers say they face retaliation for reporting COVID-19 risks. NBC News. https://www.nbcnews.com/news/us-news/forgotten-front-line-nursing-home-workers-say-they-face-retaliation-n1209606. Accessed June 5, 2020. [Google Scholar]
- 70. Chidambaram P. State reporting of cases and deaths due to COVID-19 in long-term care facilities. https://www.kff.org/coronavirus-covid-19/issue-brief/state-reporting-of-cases-and-deaths-due-to-covid-19-in-long-term-care-facilities/. Accessed June 5, 2020.
- 71. Himmelstein KEW, Venkataramani AS. Economic vulnerability among US female health care workers: potential impact of a $15-per-hour minimum wage. Am J Public Health. 2019;109(2):198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Federal Bureau of Prisons . BOP statistics: staff ethnicity/race. https://www.bop.gov/about/statistics/statistics_staff_ethnicity_race.jsp. Accessed May 18, 2020.
- 73. Trevizo P. COVID-19 cases at one Texas immigration detention center soared in a matter of days. Now, town leaders want answers. ProPublica. https://www.propublica.org/article/covid-19-cases-at-one-texas-immigration-detention-center-soared-in-a-matter-of-days-now-town-leaders-want-answers. Accessed June 13, 2020. [Google Scholar]
- 74. Davidson J. Unions for prison, VA workers file “imminent danger” reports about coronavirus conditions. Washington Post. https://www.washingtonpost.com/politics/unions-for-prison-va-workers-file-imminent-danger-reports-about-coronavirus-conditions/2020/04/08/78962ea0-79e4-11ea-8cec-530b4044a458_story.html. Accessed June 13, 2020. [Google Scholar]
- 75. Reitman J. ‘Something is going to explode’: when coronavirus strikes a prison. New York Times. https://www.nytimes.com/2020/04/18/magazine/oakdale-federal-prison-coronavirus.html. Accessed June 13, 2020. [Google Scholar]
- 76. Federal Bureau of Prisons . BOP: COVID-19 update. https://www.bop.gov/coronavirus/index.jsp. Accessed June 13, 2020.
- 77. Sengupta S. A N.Y. nurse dies. Angry co-workers blame a lack of protective gear. New York Times. https://www.nytimes.com/2020/03/26/nyregion/nurse-dies-coronavirus-mount-sinai.html. Accessed June 15, 2020. [Google Scholar]
- 78. Hong N. 3 hospital workers gave out masks. Weeks later, they all were dead. New York Times. https://www.nytimes.com/2020/05/04/nyregion/coronavirus-ny-hospital-workers.html. Accessed June 15, 2020. [Google Scholar]
- 79. Allen G. Florida governor defends firing of top data scientist. National Public Radio. https://www.npr.org/sections/coronavirus-live-updates/2020/05/20/859741245/florida-governor-defends-firing-of-top-data-scientist. Accessed June 15, 2020. [Google Scholar]
- 80. McGlade C. Arizona: Revealing nursing homes with COVID-19 outbreaks would hurt businesses. New York Times. https://www.azcentral.com/story/news/local/arizona-health/2020/05/15/arizona-disclosing-nursing-homes-have-covid-19-would-hurt-business/5203600002/. Accessed June 5, 2020. [Google Scholar]
- 81. Roberts L. State won’t name nursing homes where seniors are dying because it’s .... bad publicity? AZCentral. https://www.azcentral.com/story/opinion/op-ed/laurieroberts/2020/05/17/state-admits-why-wont-name-nursing-homes-covid-19-bad-publicity/5210671002/. Accessed June 5, 2020. [Google Scholar]
- 82. Vinten-Johansen P, Brody H, Paneth N, et al. Cholera, Chloroform, and the Science of Medicine: A Life of John Snow. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 83. Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health. 2010;100(suppl 1):S30–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]


